The Operating Theatre Environment
A modern operating theatre incorporates the following design features:
 environmental controls of varying degrees of complexity, to reduce the risk of airborne infection
environmental controls of varying degrees of complexity, to reduce the risk of airborne infection
 services for surgical and anaesthetic equipment
services for surgical and anaesthetic equipment
 an operating table on which the patient may be placed in the position required for surgery
an operating table on which the patient may be placed in the position required for surgery
 artificial lighting appropriate for the requirements of both surgeon and anaesthetist
artificial lighting appropriate for the requirements of both surgeon and anaesthetist
THE OPERATING THEATRE SUITE
The main purpose of the operating theatre environment is to provide a safe environment for patients and staff. A key component of this is to minimize the risk of transmission of infection to the patient from the air, the building or the staff. The operating theatre suite contains four zones of increasing degree of cleanliness (Table 20.1).
TABLE 20.1
Zones of Cleanliness in the Operating Theatre Suite
Outer zone – hospital areas up to and including the reception area
Clean zone – the circulation area used by staff after they have changed, and the route taken by patients from the transfer bay to the anaesthetic room
Aseptic zone – scrub-up and gowning area, anaesthetic room, theatre preparation room, operation room, exit bay
Disposal zone – disposal area for waste products and soiled or used equipment and supplies
Anaesthetic Room
 The patient’s anxiety may be reduced by avoiding the sights and sounds of the operating theatre. This is of special importance in children.
The patient’s anxiety may be reduced by avoiding the sights and sounds of the operating theatre. This is of special importance in children.
 The equipment which may be necessary during induction of anaesthesia can be stored in an uncluttered manner, with each item readily available and its location obvious, in contrast to the cramped ‘cart’ which is usually employed to provide equipment and drugs when anaesthesia is induced in the operating theatre.
The equipment which may be necessary during induction of anaesthesia can be stored in an uncluttered manner, with each item readily available and its location obvious, in contrast to the cramped ‘cart’ which is usually employed to provide equipment and drugs when anaesthesia is induced in the operating theatre.
 Time is saved by inducing anaesthesia while surgery is being completed on another patient. This is useful particularly if preparation is prolonged, e.g. performance of local anaesthetic blocks or establishment of invasive cardiovascular monitoring, but is safe only if at least two anaesthetists and two trained assistants are present.
Time is saved by inducing anaesthesia while surgery is being completed on another patient. This is useful particularly if preparation is prolonged, e.g. performance of local anaesthetic blocks or establishment of invasive cardiovascular monitoring, but is safe only if at least two anaesthetists and two trained assistants are present.
However, there are several disadvantages.
 Anaesthetic and monitoring equipment must be duplicated, or moved to the operating theatre with the patient; this usually necessitates temporary disconnection from electrical or gas supplies.
Anaesthetic and monitoring equipment must be duplicated, or moved to the operating theatre with the patient; this usually necessitates temporary disconnection from electrical or gas supplies.
 Hazards are involved in transferring an unconscious patient from a trolley to the operating table.
Hazards are involved in transferring an unconscious patient from a trolley to the operating table.
 Construction and maintenance of anaesthetic rooms are expensive.
Construction and maintenance of anaesthetic rooms are expensive.
Safety in the Operating Theatre
Trailing electrical wires, gas supply hoses, ventilator tubing, intravenous tubing and monitoring cables represent a hazard to both staff and patients in the operating theatre. Staff may trip and suffer injury, and it is easy to disconnect the electrical supply to vital equipment. If the power to modern anaesthetic machines is disconnected, monitoring, ventilation and gas supplies may fail simultaneously. In addition, there may be a risk to staff from pollution of the atmosphere with anaesthetic gases and vapours, and of contracting infection, particularly human immunodeficiency virus (HIV) or hepatitis, from infected patients. Potential hazards in the operating theatre are shown in Table 20.2.
TABLE 20.2
Potential Hazards in the Operating Theatre
Electricity
Liquids
Gases and vapours
Temperature
Humidity
Fire
Cables and tubes
Electrical Safety
Although some mention is made of electrical hazards in the operating theatre in Chapter 14, a detailed description is beyond the scope of this book, and the reader is referred to the article by Boumphrey and Langton (2003) in the further reading list. The electrical supply to the operating theatre and all electrical equipment connected to the patient incorporate design features which minimize the risk of electrical currents being transmitted through the patient to earth.
Atmospheric Pollution
Nevertheless, it is sensible to minimize atmospheric pollution in the operating theatre, and hospital regulations in both western Europe and North America require the installation of anaesthetic gas-scavenging systems in all areas where anaesthesia is administered. In the USA, the National Institute of Occupational Safety and Hygiene (a federal regulatory body) dictates that environmental concentrations of anaesthetic gases should not exceed a value of 25 ppm of nitrous oxide and 2 ppm of volatile agent. In the UK, the Health and Safety Executive introduced maximum limits of exposure to anaesthetic agents in January 1996; these are shown in Table 20.3. Scavenging systems are described in Chapter 15.
TABLE 20.3
Maximum Levels of Exposure to Anaesthetic Agents in the Operating Theatre Suite Over an 8-h Time-Weighted Average Reference Period, as Laid Down in the UK by the Health and Safety Executive
| Agent | Maximum Concentration (ppm) |
| Nitrous oxide | 100 |
| Halothane | 10 |
| Enflurane | 50 |
| Isoflurane | 50 |
| Sevoflurane | 20* |
Infection
 Gloves must be worn during induction of anaesthesia, performance of venepuncture or insertion of any intravascular cannula, and during insertion or removal of airways and tracheal tubes; this should be a routine when dealing with any patient. A plastic apron, mask and eye protection should be worn if substantial spillage of blood is anticipated, e.g. during insertion of an arterial cannula. Gloves should normally be discarded on taking the patient into the operating theatre and a fresh pair donned when any of these procedures is carried out during or at the end of anaesthesia.
Gloves must be worn during induction of anaesthesia, performance of venepuncture or insertion of any intravascular cannula, and during insertion or removal of airways and tracheal tubes; this should be a routine when dealing with any patient. A plastic apron, mask and eye protection should be worn if substantial spillage of blood is anticipated, e.g. during insertion of an arterial cannula. Gloves should normally be discarded on taking the patient into the operating theatre and a fresh pair donned when any of these procedures is carried out during or at the end of anaesthesia.
 Equipment, notes and other articles must not be handled with contaminated gloves.
Equipment, notes and other articles must not be handled with contaminated gloves.
 Needles which have been in contact with the patient must not be resheathed or handed from one person to another.
Needles which have been in contact with the patient must not be resheathed or handed from one person to another.
 Cuts or abrasions on the anaesthetist’s hands should be covered with a waterproof dressing. An anaesthetist with considerable skin lesions, such as eczema, chapping or several scratches, is particularly at risk of being infected.
Cuts or abrasions on the anaesthetist’s hands should be covered with a waterproof dressing. An anaesthetist with considerable skin lesions, such as eczema, chapping or several scratches, is particularly at risk of being infected.
 If a needlestick injury or contamination of a cut or abrasion occurs, bleeding should be encouraged and the skin washed thoroughly with soap and water.
If a needlestick injury or contamination of a cut or abrasion occurs, bleeding should be encouraged and the skin washed thoroughly with soap and water.
 Advice should be obtained immediately from the hospital’s occupational health department if there is reason to believe that contamination has occurred. Post-exposure prophylaxis following potential HIV exposure should be started within one hour of injury.
Advice should be obtained immediately from the hospital’s occupational health department if there is reason to believe that contamination has occurred. Post-exposure prophylaxis following potential HIV exposure should be started within one hour of injury.
 Disposable equipment should be used where possible. Non-disposable equipment should be decontaminated with 2% glutaraldehyde, washed with soap and water and left in glutaraldehyde for a further 3 h. Contaminated floors and surfaces should be washed with 1% hypochlorite solution. Gloves must be worn.
Disposable equipment should be used where possible. Non-disposable equipment should be decontaminated with 2% glutaraldehyde, washed with soap and water and left in glutaraldehyde for a further 3 h. Contaminated floors and surfaces should be washed with 1% hypochlorite solution. Gloves must be worn.
Prevention of Hospital-Acquired Infection
 Washing hands with soap and water at the start of the day, after eating or drinking, visiting the toilet or if hands are visibly soiled.
Washing hands with soap and water at the start of the day, after eating or drinking, visiting the toilet or if hands are visibly soiled.
 Frequent hand hygiene with an appropriate agent (often antiseptic hand-gel) whenever there is the possibility of cross-contamination. Of particular relevance to the anaesthetist is the risk of transfer of organisms around the airway to intravascular devices.
Frequent hand hygiene with an appropriate agent (often antiseptic hand-gel) whenever there is the possibility of cross-contamination. Of particular relevance to the anaesthetist is the risk of transfer of organisms around the airway to intravascular devices.
 Washing/cleaning hands between patients – particularly after handover in recovery.
Washing/cleaning hands between patients – particularly after handover in recovery.
 Wet hands with water (if using soap and water)
Wet hands with water (if using soap and water)
 Apply enough soap and handwash or hand-gel to cover all hand surfaces
Apply enough soap and handwash or hand-gel to cover all hand surfaces
2. Right palm over the other hand with interlaced fingers and vice versa (back of hands)
3. Palm to palm with fingers interlaced (between the fingers)
4. Backs of fingers to opposing palms with fingers interlocked (backs of fingers)
5. Rotational rubbing of left thumb clasped in right palm and vice versa (thumbs)
6. Rotational rubbing, backwards and forwards with clasped fingers of right hand in left palm and vice versa (finger tips).
 Rinse hands with water (if relevant)
Rinse hands with water (if relevant)
Equipment Checks
Anaesthetic apparatus should be checked before the start of each operating session in a logical sequence as recommended in the AAGBI checklist shown in Tables 20.4 and 20.5. Further checks shown in Table 20.6 should be undertaken between cases. The primary intention of the check of the anaesthetic machine is to ensure that it is safe to use and to deliver gases under pressure without leaks. These checklists are available as laminated cards, intended to be attached to all anaesthetic machines in the UK and Ireland.
TABLE 20.4
The Association of Anaesthetists of Great Britain and Ireland Checklist for Pre-Session Checking of Anaesthetic Equipment
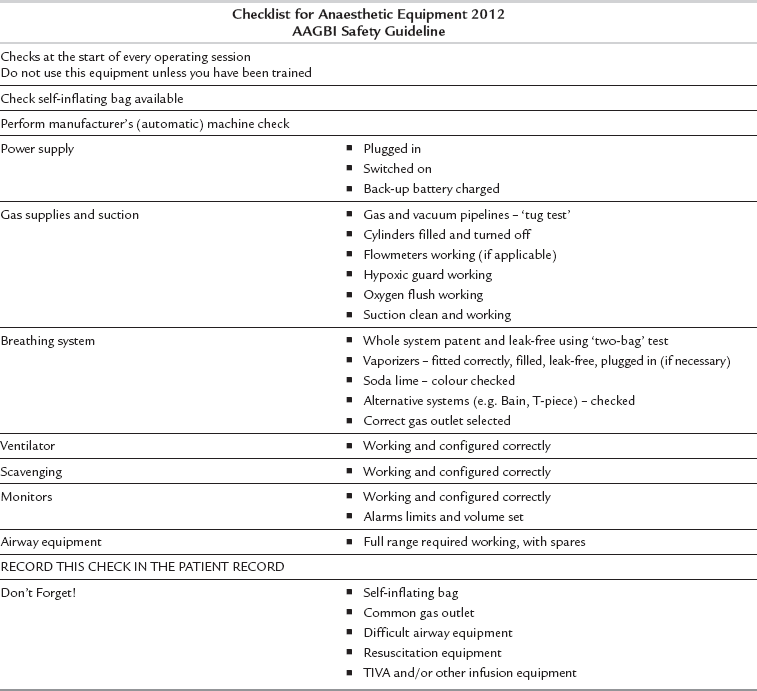
© The Association of Anaesthetists of Great Britain and Ireland 2012.
Adapted from Checking Anaesthetic Equipment 2012, with permission.
TABLE 20.5
The Association of Anaesthetists of Great Britain and Ireland ‘Two-Bag’ Test
THE TWO-BAG TEST
A two-bag test should be performed after the breathing system, vaporizers and ventilator have been checked individually
1. Attach the patient end of the breathing system (including angle piece and filter) to a test lung or bag.
2. Set the fresh gas flow rate to 5 L min− 1 and ventilate manually. Check that the whole breathing system is patent and that the unidirectional valves are moving. Check the function of the APL valve by squeezing both bags.
3. Turn on the ventilator to ventilate the test lung. Turn off the fresh gas flow, or reduce to a minimum. Open and close each vaporizer in turn. There should be no loss of volume in the system.
Adapted from Checking Anaesthetic Equipment 2012, with permission.
TABLE 20.6
The Association of Anaesthetists of Great Britain and Ireland Checklist for Checking Anaesthetic Equipment between Cases
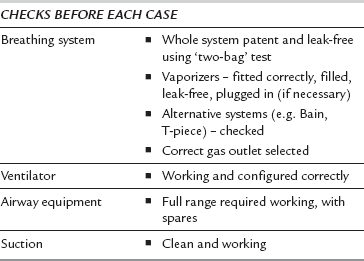
Adapted from Checking Anaesthetic Equipment 2012, with permission.
Breathing System and Vaporizers
All breathing systems which are to be used must be checked and a ‘two-bag test’ performed before use (Table 20.5). Breathing systems should be inspected visually for correct configuration and assembly. All connections within the system and to the anaesthetic machine should be checked to ensure that they are secured by ‘push and twist’. Ensure that there are no leaks or obstructions in the reservoir bags or breathing system and that they are not obstructed by foreign material. A pressure leak test (between 20 and 60 cmH2O) should be performed on the breathing system by occluding the patient end and compressing the reservoir bag.
All vaporizers must be turned off after they have been checked.
Two-Bag Test
A two-bag test should be performed after the breathing system, vaporizers and ventilator have been checked individually (see Table 20.5). Breathing systems should be protected with a test lung or bag when not in use to prevent intrusion of foreign bodies.
Total Intravenous Anaesthesia (TIVA)
The following recommendations have been made to minimize the risks of awareness during TIVA.
1. An anti-reflux/non-return valve should always be used on the intravenous fluid infusion line when administering TIVA to prevent accumulation of drug in the fluid infusion tubing.
2. Sites of intravenous infusions should be visible so that they can be monitored for disconnection, leaks or subcutaneous leakage.
3. The anaesthetist must know how to use, and to check, the equipment before use.
4. Hospitals should give preference to purchasing intravenous connectors and valves which are clearly labelled.
Recovery Room/Post-Anaesthesia Care Unit
Clinical aspects of recovery room care are discussed in Chapter 40.
Ancillary Staff
 Preparation and preliminary checking of equipment. It should be stressed that this does not absolve the anaesthetist from the responsibility of checking the equipment fully before an operating list is started.
Preparation and preliminary checking of equipment. It should be stressed that this does not absolve the anaesthetist from the responsibility of checking the equipment fully before an operating list is started.
 Alleviation of anxiety by reassurance and constant communication with the patient while awaiting anaesthesia.
Alleviation of anxiety by reassurance and constant communication with the patient while awaiting anaesthesia.
 Checking the correct identity of the patient and participating in the WHO checklist procedures. It is the responsibility of the surgeon to ensure that the appropriate procedure is undertaken on the correct patient, but the anaesthetist must also confirm the identity of the patient and, as far as is possible, confirm that the surgeon is performing the correct operation. This is one of the many reasons why the anaesthetist must see every patient preoperatively.
Checking the correct identity of the patient and participating in the WHO checklist procedures. It is the responsibility of the surgeon to ensure that the appropriate procedure is undertaken on the correct patient, but the anaesthetist must also confirm the identity of the patient and, as far as is possible, confirm that the surgeon is performing the correct operation. This is one of the many reasons why the anaesthetist must see every patient preoperatively.
 Preparation of intravenous infusions, cardiovascular monitoring transducers, etc.
Preparation of intravenous infusions, cardiovascular monitoring transducers, etc.
 Assistance during anaesthesia, particularly during induction, when special manoeuvres such as cricoid pressure may be required, and after transfer to the operating theatre to assist in re-establishment of monitoring.
Assistance during anaesthesia, particularly during induction, when special manoeuvres such as cricoid pressure may be required, and after transfer to the operating theatre to assist in re-establishment of monitoring.
 Assistance in positioning the patient for local or regional blocks.
Assistance in positioning the patient for local or regional blocks.
 Assistance in obtaining drugs or equipment if complications arise during anaesthesia.
Assistance in obtaining drugs or equipment if complications arise during anaesthesia.
 Assistance in the immediate postoperative period before the patient is transferred to the recovery room.
Assistance in the immediate postoperative period before the patient is transferred to the recovery room.
Physicians’ Assistants (Anaesthesia)
 be present in the theatre suite, must be easily contactable and must be available to attend within 2 min of being requested to attend by the PA(A)
be present in the theatre suite, must be easily contactable and must be available to attend within 2 min of being requested to attend by the PA(A)
 be present in the anaesthetic room/operating theatre during induction of anaesthesia
be present in the anaesthetic room/operating theatre during induction of anaesthesia
 regularly review the intraoperative anaesthetic management
regularly review the intraoperative anaesthetic management
 be present during emergence from anaesthesia until the patient has been handed over safely to the recovery room staff
be present during emergence from anaesthesia until the patient has been handed over safely to the recovery room staff
 remain in the theatre suite until control of airway reflexes has returned and artificial airway devices have been removed, or the ongoing care of the patient has been handed on to other appropriately qualified staff, e.g. in the intensive care unit.
remain in the theatre suite until control of airway reflexes has returned and artificial airway devices have been removed, or the ongoing care of the patient has been handed on to other appropriately qualified staff, e.g. in the intensive care unit.
Association of Anaesthetists of Great Britain and Ireland. Immediate postanaesthetic recovery. London: AAGBI, 2013.
Association of Anaesthetists of Great Britain and Ireland. Infection control and anaesthesia 2. London: AAGBI, 2008.
Association of Anaesthetists of Great Britain and Ireland. Checking anaesthetic equipment 2012. London: AAGBI, 2012.
Boumphrey, S., Langton, J.A. Electrical safety in the operating theatre. BJA CEPD Reviews. 2003;3:10.
Johnston I.D.A., Hunter A.R., eds. The design and utilization of operating theatres. London: Edward Arnold, 1984.
Royal College of Anaesthetists, 2011. PA(A) supervision and limitation of scope of practice (May 2011 revision). http://www.rcoa.ac.uk/node/1927
Spence, A.A. Environmental pollution by inhalation of anaesthetics. Br. J. Anaesth. 1987;59:96.
Taylor T.H., Major E., eds. Hazards and complications of anaesthesia, second ed., Edinburgh: Churchill Livingstone, 1994.








