The Operating Room Suite and Instrumentation
Many functional, uncluttered, and multidisciplinary systems are available to help organize an operating room suite. Most instruments can be placed on carts or booms, which can be moved to accommodate the surgical site (Figs. 114–1 and 114–2). An operating suite does not have to contain all commercially available instruments to function properly. The basic instruments that are required for safe laparoscopic surgery can be divided into three groups: the electronic cart, the laparoscopic instrument table, and the vaginal instrument table.
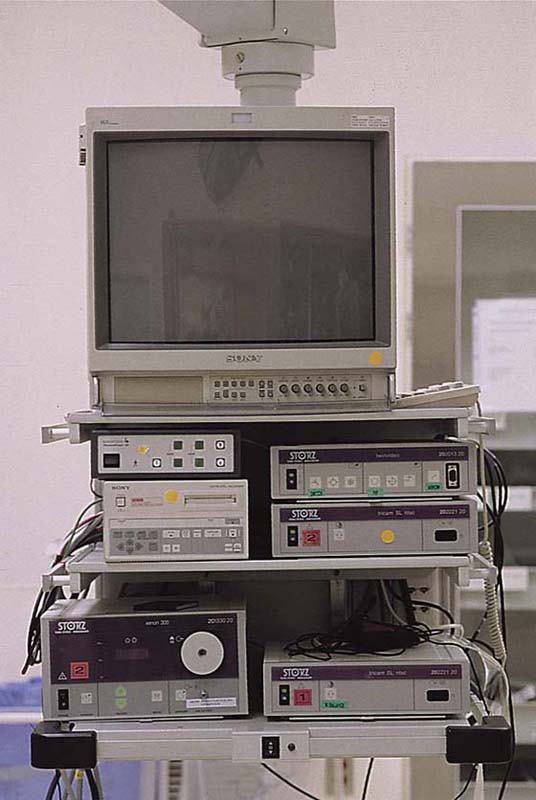
Electronic Cart
The following instruments are usually placed on the electronic cart (Fig. 114–3):
 Monitor
Monitor
 Light source
Light source
 Camera and camera control unit
Camera and camera control unit
 High-flow insufflator
High-flow insufflator
 Electrosurgical unit
Electrosurgical unit
 Image recording device
Image recording device
The monitor can be on the cart as shown. Recently, the flat screen monitors are separate units.
A three-chip camera will give higher resolution than a one-chip camera. This will be noticed only if the monitor has the same number of lines of resolution. A xenon light source (300W) gives better illumination and color duplication than a halogen (150W and 300W) one. All insufflators have flow and pressure controls. The pressure should always be set at less than 15 mm Hg. Higher settings are rarely needed and should be used for brief periods of time. High-flow insufflators will render small leaks less important. An electrosurgical unit that has both unipolar and bipolar systems should be used. The unipolar system should generate both nonmodulated (cutting) and modulated (coagulation) current. The bipolar instruments will have the source current on a prong of the forceps or scissors and the return electrode on the other prong. In the unipolar system, the instrument is the source of the current, and the return electrode is the grounding pad.
Surgical instruments that are used for laparoscopic procedures are usually kept on one or two separate tables, depending on whether the operation will have a vaginal component.
Laparoscopic Instrument Table
 Laparoscopes: three sizes (2/3, 5, and 10 mm) (Fig. 114–4)
Laparoscopes: three sizes (2/3, 5, and 10 mm) (Fig. 114–4)
 Light cables
Light cables
 Trocars (2, 5, and 10/12 mm) and Veress needle
Trocars (2, 5, and 10/12 mm) and Veress needle
 Graspers and dissectors
Graspers and dissectors
 Scissors
Scissors
 Needle holders, needle assist, and knot pushers
Needle holders, needle assist, and knot pushers
 Aspiration and injection instruments
Aspiration and injection instruments
 Bipolar forceps and cords
Bipolar forceps and cords
 Introducer for introducing a pretied suture
Introducer for introducing a pretied suture
The laparoscopes used in gynecology have a 0° deflection. You see what is straight ahead. Several sizes of laparoscopes are useful (see Fig. 114–4). The larger the diameter of the laparoscope, the greater is the brightness. A 10-mm laparoscope with a working channel will decrease the brightness. The decrease in luminosity will depend on the size of the working channel (3 to 8 mm). The authors use a 5- to 12-mm laparoscope for operative laparoscopy, a 5-mm laparoscope for diagnostic laparoscopy under general anesthesia, and a 2- to 3-mm laparoscope for diagnostic laparoscopy under conscious sedation. A 12-mm laparoscope is used for robotic surgery, but a 5-mm laparoscope is used for all other operative procedures, including single port surgery.
A variety of graspers are available, but we use the following:
 Allis graspers when a firm purchase is required, as when the ovarian cortex or the myometrium is grasped
Allis graspers when a firm purchase is required, as when the ovarian cortex or the myometrium is grasped
 Atraumatic graspers for grasping delicate tissues
Atraumatic graspers for grasping delicate tissues
 Soft bowel grasper for placing traction on the bowel
Soft bowel grasper for placing traction on the bowel
 Maryland dissector for blunt dissection or precise tissue grasping
Maryland dissector for blunt dissection or precise tissue grasping
All accessory instruments go down a 5-mm port. The scissors should be disposable because the reusable ones often are not sharp. An aspiration-suction device is mandatory for gynecologic laparoscopic surgery. The fluid bags should be warmed because hypothermia is a significant problem during prolonged surgery. The suction canisters and fluid bags are usually placed off to one side. The tips are reusable (5 and 10 mm), but the tubing and the handle are often disposable.
FIGURE 114–1 An operating room can be structured so that equipment does not take up an inordinate amount of space.
FIGURE 114–2 Operating room setup. Note that there are two booms. Each has a monitor, so that all physicians can view the surgical field from a comfortable position.
FIGURE 114–3 Equipment placed on a cart or boom (Bertchold Co, Charleston, South Carolina).
FIGURE 114–4 Laparoscope sizes.
Vaginal Instrument Table
 Open-sided speculum
Open-sided speculum
 Single-toothed tenaculum
Single-toothed tenaculum
 Foley catheter
Foley catheter
 Cervical dilators
Cervical dilators
 Uterine manipulators: Cohen cannula (Eder Instruments, Oak Creek, Wisconsin), RUMI manipulator (Cooper Medical, Oklahoma City, Oklahoma), Hulka uterine forceps (Rocket, Wolf, California)
Uterine manipulators: Cohen cannula (Eder Instruments, Oak Creek, Wisconsin), RUMI manipulator (Cooper Medical, Oklahoma City, Oklahoma), Hulka uterine forceps (Rocket, Wolf, California)
The vaginal table may have other instruments if there is a significant vaginal component, such as with laparoscopic hysterectomy.
A variety of other instruments or energy forms may be useful in specific cases. These are described in the appropriate chapters. We do not routinely use other energy forms such as an ultrasonic scalpel or a carbon dioxide (CO2) laser because they have never been shown to be safer or to cause less tissue injury or adhesion formation than electrosurgery.

 Mark D. Walters
Mark D. Walters