http://evolve.elsevier.com/McCuistion/pharmacology
In their everyday practice, nurses have many important tasks; however, drug administration is at the top of the list. It is estimated that about 40% of the nurse’s time is spent on drug administration, and knowledge of these drugs is essential to patient safety. If unsure about a patient’s medication, consult the health care provider for clarification.
Nurses are often the first line of defense against drug errors in patient care. Federal, state, and local authorities issue regulations and guidelines for practice, and each state has a nurse practice act that defines the scope and function under which the nurse practices. Health care institutions also have policies that help nurses follow federal and state guidelines and regulations.
This chapter focuses on the nursing process as it relates to pharmacology and the safe administration of patient drugs with a focus on patient- and family-centered care. Chapter 9 offers additional information on safety in pharmacotherapy.
 The Quality and Safety Education for Nurses (QSEN) initiatives guide nurses in the practice of safe, comprehensive care. QSEN offers competencies to provide structure and encourages professional development while advocating for safe patient care. QSEN equips nurses with competencies to improve the quality and safety of the health care system in which they work.
The Quality and Safety Education for Nurses (QSEN) initiatives guide nurses in the practice of safe, comprehensive care. QSEN offers competencies to provide structure and encourages professional development while advocating for safe patient care. QSEN equips nurses with competencies to improve the quality and safety of the health care system in which they work. The QSEN competencies are as follows:
The QSEN competencies are as follows:1. Patient- and family-centered care: Recognize the patient as the source of control and full partner in providing compassionate and coordinated care based on respect for patient preferences, values, and needs.
2. Collaboration and teamwork: Function effectively in nursing and inter-professional teams, fostering open communication, mutual respect, and shared decision-making to achieve quality patient care.
3. Evidence-based practice: Integrate best current evidence with clinical expertise and patient/family preferences and values for delivery of optimal health care. CustomWritings for help when in need of evidence that only writers qualified in the niche can provide.
4. Quality improvement: Continuously improve the quality and safety of health care systems by using data to monitor outcomes of care processes and improvement methods to design and test changes.
5. Safety: Minimize risk of harm to patients and providers through both system effectiveness and individual performance.
6. Informatics: Use information and technology to communicate, manage knowledge, mitigate error, and support decision making.
 QSEN competencies are integrated throughout the book and are highlighted in special features such as “Patient Safety” boxes and high-alert drug icons.
QSEN competencies are integrated throughout the book and are highlighted in special features such as “Patient Safety” boxes and high-alert drug icons.The Nursing Alliance for Quality Care (NAQC) is an organization that supports quality patient-centered health care. The NAQC in partnership with the American Nurses Association (ANA) has published guidelines that support the core principles of patient-centered quality care. These guidelines aim to foster “the patient relationship as the cornerstone of patient safety and quality.” The NAQC’s mission is to advance the highest quality, safety, and value of consumer-centered health care for all individual patients, their families, and their communities. NAQC believes it is the nurse’s role to cultivate successful patient and family engagement, and that fostering family engagement is an essential component in reducing drug errors. The nurse serves as a patient advocate by supporting the patient’s right to practice informed decision making and by maintaining patient-centered engagement in the health care setting. These guidelines include nurses at all levels of education and across all health care settings. Both QSEN and NAQC principles are fundamental to patient-centered practice and safety in pharmacotherapy.
Nursing Process: Patient-Centered Collaborative Care
The nursing process is a five-step decision-making approach that includes (1) assessment, (2) diagnosis, (3) planning, (4) implementation, and (5) evaluation. The purpose of the nursing process is to identify, diagnose, and treat human responses to health and illness. The nursing process is the essential core of practice for nurses. It supports the nurse in prioritizing the safe, timely delivery of drug administration. The nursing process is continuous and moves back and forth between the various steps. Careful attention to each phase of the process promotes the patient’s success with the prescribed medication regimen. These steps are discussed as each relates to health teaching and drug therapy.
Assessment
During the assessment phase, the nurse is gathering information from the patient about the patient’s health and lifestyle. Assessment includes both subjective and objective data. Always perform a complete, systemic assessment of the patient’s body systems. In this assessment, the nurse asks the patient questions about the illness and about the drug regimen. The nurse can also get information from family members, health professionals, and the medical record. The assessment phase is paramount because the nurse will use the information gathered to form the basis of the patient’s plan of care, which includes drug administration. Careful attention to each phase of the nursing process encourages the patient’s success with the prescribed medication regimen.
Subjective Data
Subjective data include information provided verbally by the patient, family members, friends, or other sources. The patient must verbalize subjective data, which are imperceptible by the nurse’s senses. The nurse may ask open-ended questions that allow the patient to answer directly, such as “Please tell me about your current medications.” The nurse may help the patient explain or describe subjective data but must never speak for the patient. Subjective data comprise what the patient personally has to say about his or her medications, health problems, and lifestyle. Examples of pertinent information that the nurse can use to help solicit subjective data from the patient concerning medication administration include the following:
• Current health history, including family history
• Swallowing problems (dysphagia)
• Signs and symptoms of the patient’s illness verbalized by the patient
• Current concerns about the patient’s:
• Knowledge about medications and side effects
• Over-the-counter (OTC) remedies, nutritional supplements, herbal remedies, and contraceptives
• Knowledge of side effects to report to the physician
• Attitude and beliefs about taking medications
• Allergies
• Financial barriers
• Use of tobacco, alcohol, and caffeine
• Cultural dietary barriers
• The patient’s home safety needs
• Caregiver needs and support system
Enhancing the patient’s adherence to the drug therapy regimen is an essential component of health teaching. The patient’s attitudes and values about taking medication are important considerations when determining readiness to learn. Attitudes and values should be considered when planning interventions to support the patient’s decision to adopt healthy behaviors related to medications. In addition, the patient’s social support system should be emphasized. This special support system is unique to the individual and may be composed of persons who assist in preparing drugs, organizing pills, and ordering medications. A support system can alert a patient to side effects, encourage actions that promote medication compliance, and notify the health care provider if a problem arises.
Objective Data
Objective data are what the nurse directly observes about the patient’s health status. It involves collecting the patient’s health information by using the senses: seeing, hearing, smelling, and touching. Objective data collection provides additional information about the patient’s symptoms and also targets the organs most likely to be affected by drug therapy. For example, if a drug is nephrotoxic, the patient’s creatinine clearance should be assessed.
The following are examples of objective data concerning medication administration:
• Physical health assessment
• Laboratory and diagnostic test results
• Data from the physician’s notes (i.e., health history)
• Measurement of vital signs
• The patient’s body language
Nursing Diagnosis
A nursing diagnosis is made based on analysis of the assessment data, and it determines the type of care the patient will receive. When data show an abnormality during the assessment, it can serve as the defining characteristic of a problem to support the appropriate nursing diagnosis; and more than one applicable nursing diagnosis may be generated. The nurse formulates nursing diagnoses and uses them to guide the development of a care plan to provide patient-centered quality care.
Common nursing diagnoses related to drug therapy include the following:
• Pain, Acute or Chronic, related to surgery
• Confusion, Acute related to an adverse reaction to medication
• Health Maintenance, Ineffective related to not receiving recommended preventive care
• Knowledge, Deficient related to effects of anticoagulant medication
• Noncompliance related to forgetfulness
• Health Management, Ineffective related to lack of finances
Use of nursing diagnoses is beneficial to patient care because it facilitates the development of an individualized care plan for each patient. It is important to note that a nursing diagnosis is different from a medical diagnosis, which identifies a disease condition and the results of diagnostic tests and procedures.
To review the complete list of NANDA nursing diagnoses please see http://faculty.mu.edu.sa/public/uploads/1380604673.6151NANDA%202012.pdf.
Planning
During the planning phase, the nurse uses the data collected to set goals or expected outcomes and interventions. Goals or expected outcomes should address the problems in the patient’s nursing diagnosis. Goals are patient centered, describe the specific activity, and include a time frame for achievement and reevaluation. Planning includes the development of nursing interventions used to assist the patient in meeting goals. In order to develop patient-centered goals and outcomes, collaboration with the patient and/or family is necessary. Effective goal setting has the following qualities:
• The expected change is realistic, measurable, and includes reasonable deadlines.
• The goal is acceptable to both the patient and nurse.
• The goal is dependent on the patient’s decision-making ability.
• The goal is shared with other health care providers, including family or caregivers.
• The goal identifies components for evaluation.
Examples of well-written comprehensive goals include the following:
• The patient will independently administer the prescribed dose of 4 units of regular insulin by the end of the fourth session of instruction.
• The patient will prepare a 3-day medication recording sheet that correctly reflects the prescribed medication schedule by the end of the second session of instruction.
Implementation of Nursing Interventions
The implementation phase is the part of the nursing process in which the nurse provides education, drug administration, patient care, and other interventions necessary to assist the patient in accomplishing the established goals. In most practice settings, administration of drugs and assessment of the drug’s effectiveness are important nursing responsibilities. (See Chapter 9 for more information.)
Patient Teaching
It is important for the nurse to keep in mind factors that help promote patient learning. The patient must be ready to learn and must make an investment in learning. If the patient buys into wanting to practice good health principles, learning can be successful. The nurse and patient together must become fully engaged in the learning process. Timing is another important factor. What is the best time for the patient to learn? Is the patient a morning or night person? People seem to learn best if the time between the learning and use is short. The environment should be conducive to learning with a temperature that is comfortable and an environment that is quiet. It is important for the nurse to recognize that certain barriers to learning exist. Pain is an obstacle, and the patient’s teaching should be postponed until pain is relieved. Be mindful of language barriers. If the patient does not speak the same language as the nurse, an interpreter may be needed. The patient’s age may be another important obstacle. If the patient is young, or perhaps elderly and forgetful, a family member or significant other will need to be present.
Patient teaching is essential to the patient’s recovery. It allows the patient to become informed about his or her health problems and to participate in creating interventions that can lead to good health outcomes. It is within the scope and practice of the nurse to embrace patient education and to use health-teaching strategies.
Nurses have a primary role in teaching both patients and families about drug administration. It is important that all teachings be tailored to the patient’s educational level and that the patient trusts the nurse for learning to begin. When possible, it is always important to include a family member or friend in the teaching to provide support to the patient with reminders and encouragement; they can also detect possible side effects that may occur in the patient. The following are important principles to remember when teaching patients about their medications:
• General. Instruct the patient to take the drug as prescribed. Consistency in adhering to the prescribed drug regimen is important.
• Provide simple written instructions to the patient with the doctor and pharmacy names and telephone numbers.
• Instruct the patient to notify the health care provider if any of the following occur:
• The dose, frequency, or time of the drug is adjusted.
• A female patient becomes pregnant.
• An OTC medication or supplement is added.
• Side effects. Give the patient instructions that will help minimize any side effects (e.g., avoid direct sunlight with drugs that can cause photosensitivity or sunburn). Advise patients of any expected changes in the color of urine or stool, and counsel the patient who has dizziness caused by orthostatic hypotension to rise slowly from a sitting to a standing position.
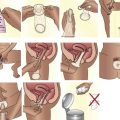
• Instruct the patient on drug administration according to the prescribed route: eye or nose instillation, subcutaneous injection, suppository, oral/mucosal (e.g., swish-and-swallow suspensions), and inhaled via a metered-dose inhaler with or without a spacer. Include a return demonstration in the instructions when appropriate.
• The use of drug cards is a helpful teaching tool (Box 8.1). Drug cards can be obtained from the health care provider or from the drug manufacturer. They are helpful components for teaching. Drug cards may include the name of the drug, the reason for taking the drug, the drug dosage, times to take the drug, possible side effects, possible adverse effects and when to notify the care provider, and specific things that should or should not be done while taking the medication (e.g., take with food, do not crush tablets).
• Diet. Advise the patient about foods to include in their diet and foods to avoid. Many foods interact with certain drugs. Depending on the nature of the interaction, certain foods have the ability to decrease drug absorption, increase the risk of drug toxicity, or create other problems that make them an important safety concern.
• Cultural considerations. The nurse must apply knowledge of cultural considerations to individualize a teaching plan (Box 8.2). A culturally sensitive nurse is alert to the patient’s cultural expectations. Begin by identifying your own cultural beliefs, practices, and values in order to keep them separate from those of the patient.
Additional suggestions include the following:
• Space instruction over several sessions if appropriate.
• Review community resources related to the patient’s nursing and medical diagnoses.
• Collaborate with the patient and family and other health care staff and agencies to mobilize resources to meet the patient’s needs.
• Identify patients at risk for noncompliance with the regimen. Alert the health care provider and pharmacist so they can develop a plan to minimize the number of drugs and the number of times drugs are administered.
• Evaluate the patient’s understanding of the medication regimen on a regular basis.
• Empower the patient to take responsibility for drug management.
• General points to remember and tips for successful patient education are presented in Box 8.3.
Many people take multiple drugs simultaneously several times each day, which presents a challenge to patients, their families, and nurses. This complex activity of taking several drugs can be segmented into several simple tasks that include the following:
• A recording sheet may be helpful. When the drug is administered, the patient or family member marks the sheet, which is designed to meet the patient’s individual needs. For example, the time can be noted by the patient, or it can be entered beforehand, with the patient marking the designated time the dose should be taken. A generic format follows:
• Alternatives to recording sheets are also available, and alarm reminder devices may be used.
Throughout the teaching plan, the nurse promotes patient independence (e.g., self-administering, safely storing, and ordering of the drug regimen). Always keep in mind patients’ goals and outcomes when teaching. Box 8.4 presents a checklist for health teaching in drug therapy.
Evaluation
In the evaluation phase of the nursing process, the nurse determines whether the goals and teaching objectives are being met. The nurse continues to use ongoing assessment data to evaluate the successful attainment of the patient’s objectives and goals. If the objectives and goals are not met, the nurse will revise the objectives, goals, and interventions to ensure success. If the objectives, goals, and interventions are met, the nurse will document the successful attainment in the nursing plan of care.
Critical Thinking Case Study
Mr. J.S. is a 66-year-old man who just arrived on the medical surgical unit following an appendectomy. He is complaining of pain. You are the nurse assigned to care for Mr. J.S.
1. What critical assessment data do you need to identify and collect?
2. Formulate a nursing diagnosis based on your assessment data.
3. Describe two nursing interventions to assist the patient.
4. What criteria would you use to evaluate the effectiveness of the nursing interventions?