3 The neurological examination
Cranial nerves
CN II (optic nerve)
This requires four separate tests: field, fundi, acuity and pupils.
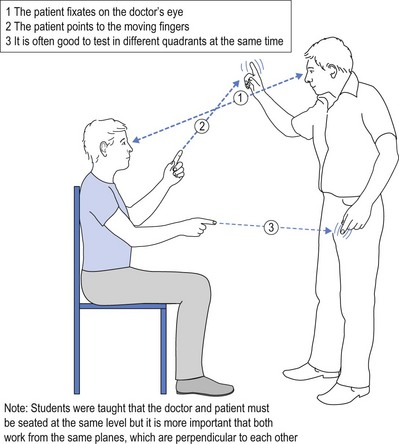
Fields are tested by confrontation, by standing in front of the patient and randomly wiggling fingers in each of the four quadrants of the visual fields (Fig 3.1).
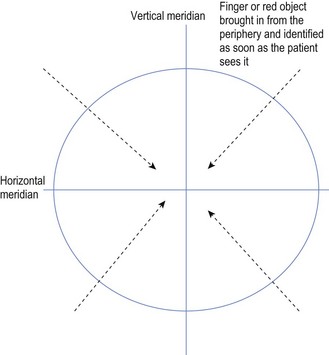
The patient is asked to point at the wiggling fingers, and at times it is worth wiggling fingers in more than one quadrant to encourage the patient to pay extra attention. If this test suggests abnormality, then each eye should be tested individually by covering the other eye. The crude test has the doctor wiggle the finger in each of the four quadrants of the visual field and the patient must identify the wiggling finger. More sophisticated testing has the doctor move the fingers in on the diagonal in each quadrant (see Fig 3.2).
The patient is asked to indicate as soon as the finger is seen, and the doctor compares this to their own perception of the finger to see if there is parity between doctor and patient. Use of a red object, such as a red pin, produces a more precise definition of the field of vision. The patient is asked to nominate when the pin is clearly perceived as red, thereby relying on colour vision, rather than a relatively large moving object. Loss of vision must respect the horizontal and vertical meridians to be anatomically sound (see Fig 3.2).
When the patient is uncooperative and will not point to the moving finger or object, an alternative method for testing visual fields is to use ‘menace’. Menace employs a motion as if the examiner is going to poke the patient in the eye, either with a fist or flattened hand, stopping just short of the point of contact. If the patient has preserved vision within the quadrant being tested, it is almost impossible for the patient to avoid blinking. This is an innate, self-protective reflex evoked by the patient seeing the menacing object, such as a fist, approach. Failure to blink in the face of such menace suggests blindness in the fields being tested. It is not absolute but it is very suggestive.
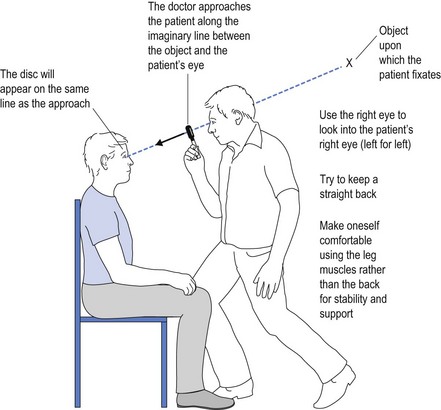
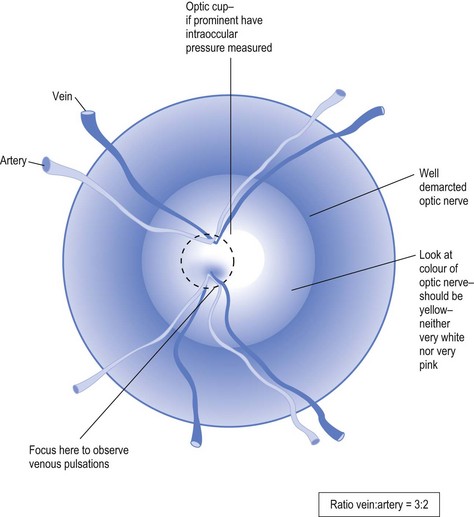
Fundi are tested using an ophthalmoscope. It is important to use the right eye to examine the right eye, to approach the patient from directly in front to avoid the forehead covering the line of vision of the other eye (the one not being examined) and to place the disc (that is, optic nerve) where it is most convenient to view it, rather than looking for it. The way to do this is to ask the patient to look at a convenient object that allows the examiner to approach using that line which follows an imaginary line drawn between the object and the eye (Fig 3.3).
The optic disc contains within it an internal ‘cup’. If this is very obvious it may simply be a variant of normal but it may also herald the first sign of glaucoma and, hence, if noted, should alert the examiner to seek measurement of intraocular pressure from either the optometrist or ophthalmologist.
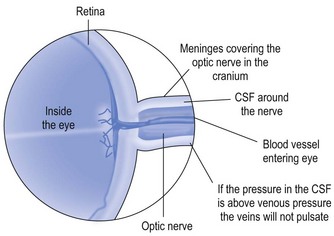
If the disc margins are ‘blurred’, this may reflect any number of normal conditions, such as medullated nerve fibres (fibres with myelin still in place) but it may also reflect papilloedema. Papilloedema is usually accompanied by haemorrhages and an angry looking disc (see Fig 3.6). Perhaps the first sign of papilloedema is a loss of venous pulsations, which can be seen in 90% of normal people. To seek out venous pulsations, the operator must identify the disc and focus upon it. The relative ratio of arteries to veins is 2 : 3, with the veins being the wider and darker vessels. The doctor selects the end of the vein before it disappears into the nerve, and focuses on that end. If venous pulsations are present then the vein will fill and empty while being observed. Alternatively, the vein may change from fatter to thinner in rhythmic fashion while pulsating. The presence of venous pulsations automatically excludes the presence of raised intracranial pressure but, as already stated, up to 10% of the normal population do not demonstrate such pulsations. Thus, absence of venous pulsations need not reflect raised intracranial pressure, while their presence excludes it (see Figs 3.4 and 3.5).
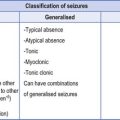
FIGURE 3.6 Papilloedema.
(Kliegman. Nelson Textbook of Pediatrics, 18th edn. 2007 Saunders; Figure 591-1 (a) Mild papilloedema. Blurred disc margins and venous congestion. (b) Moderate papilloedema. Disc oedematous and raised. Vessels buried within substance of nerve tissue. (c) Severe papilloedema. Haemorrhages are evident within disc (arrow), and there are microinfarcts (soft exudates) in the nerve fibre layer. (d) Macular star (arrow) with oedema residues distributed within the Henle layer of the macula.)
There are basically only four causes of ptosis:
Shining the light into the right pupil and shielding that light from the left eye should evoke constriction of both pupils. The right eye constricts because of direct response of the light onto the right optic nerve. The left pupil constricts because that message from the right CN II is transmitted consensually to the left pupil via CN III and parasympathetic fibres. Thus blindness in the right eye will prevent the process happening, and damage to the transmission via CN III, assuming functioning right eye, will result in no pupillary response on the left.
Having evoked the response from the right pupil, the shielded light is focused onto the left eye. This should result in a repetition of the above response. If the left eye is blind and does not constrict, then both pupils may dilate as a relaxation of the previous constriction. This does not imply the dilatation is evoked by the left eye, but rather that the left eye cannot perceive the light and does not prevent the dilatation consequent to the earlier constriction. This is known as the ‘swinging lantern sign’.
CN III, IV, VI (oculo-motor, trochlear and abduscens nerves)
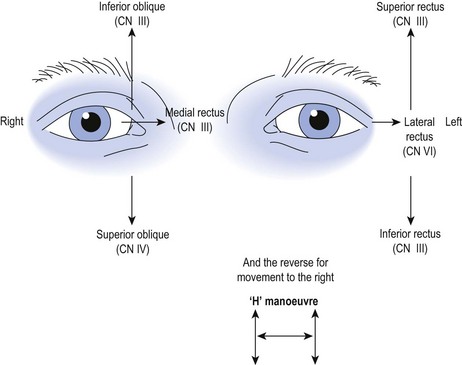
Eye movement is tested formally using an ‘H’ manoeuvre (see Fig 3.7).
Where there is loss of distant object, irrespective of which eye is covered, it is unlikely to be due to individual muscle or cranial nerve damage. While testing eye movement, the examiner should also look for nystagmus. As a simple rule of thumb, horizontal nystagmus suggests peripheral deficit and vertical nystagmus suggests central damage. This is not an absolute as cerebellar damage may cause horizontal nystagmus and drug toxicity may cause nystagmus in all directions.
A CN IV lesion is often overlooked. It innervates the superior oblique muscle of the eye, causing the eye to turn down and in (see Fig 3.7). It is not the only muscle doing this as CN III turns the eye in (medial rectus) and pulls the eye down (inferior rectus). Thus competing muscles may obscure a CN IV palsy presentation. What should alert the doctor is the patient who complains of diplopia and presents with the head held in a tilted position. The tilt is to overcome the diplopia. Remember that full adduction of the eye switches off most of the inferior rectus function (see Fig 3.7). Downward movement in this position is reliant on the superior oblique (innervated by CN IV). This two-step testing helps to identify the CN IV palsy on clinical testing.
CN VI abducts the eye on the horizontal plane. A CN VI palsy prevents the eye from full lateral movement. Such palsy allows there to be sclera between the iris and the margins of the palpebral fissure. If there is still ‘eye white’ lateral to the iris in the fully abducted eye, then a CN VI palsy should be considered. The CN VI has the longest, and hence most precarious, passage through the cranial vault. It follows that a partial CN VI palsy (incomplete abduction) may be a false localising sign of raised intracranial pressure. It should alert the GP to the possible need for repeat examination of the fundus, looking for papilloedema (see Figs 3.5 and 3.6), the first sign of which is loss of venous pulsations. It should also alert to the need for cerebral CT scanning looking for a space occupying lesion causing raised intracranial pressure. Unlike CN IV, where competing muscles produce some of the same eye movement functions, the competitors to the lateral rectus, the only muscle innervated by CN VI, is the medial rectus which adducts the eye. Hence a complete CN VI palsy will cause the eye to be turned in on the horizontal plane.
CN V (trigeminal nerve)
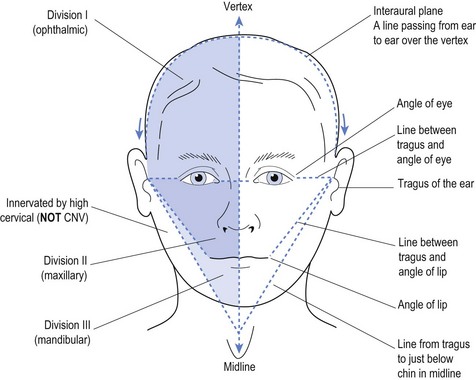
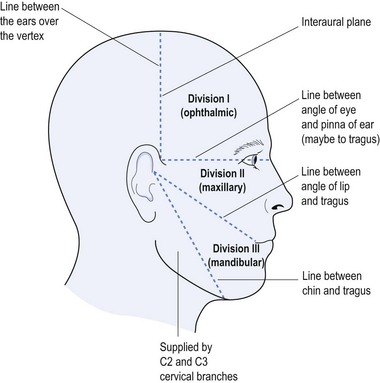
CN V is tested with respect to its three divisions, namely, first, ophthalmic branch, second, maxillary branch, and third, mandibular branch (Figs 3.8 and 3.9). It is important to note that sensory changes, which do not respect these anatomical demarcations, provide positive evidence of psychological, non-organic disease.
While motor testing of CN V is said to be important, motor function is rarely affected without sensory loss. Testing sensation with a motor response is performed via the corneal reflex, which is a useful way to test trigeminal sensation in the unconscious patient. It is not my chosen route, because if tested using cotton wool on the cornea, it is theoretically possible to leave a wisp of cotton wool on the cornea and thereby provoke a corneal ulcer. My chosen route, in unconscious patients, is to approach from the side with a rolled up tip of tissue and stimulate inside the nostril. This will usually evoke twitching of the nose due to an unpleasant sensory stimulation inside the nose. If the patient is conscious but uncooperative, it is best to stimulate surreptitiously so that the patient does not see the tissue approach, thereby evoking an unconscious response that truly reflects sensation of an unpleasant nature, rather than anticipation of that stimulus.
CN VIII (vestibular cochlear nerve)
Weber’s test involves placing the vibrating fork in the middle of the forehead. It should be perceived in the midline, at the place it is positioned. Should it be perceived lateralised to one ear, that implies either middle ear problems in that ear (enhanced conduction to that side) or neurosensory deafness in the opposite ear. If the patient has difficulty with the tuning fork placed in the midline of the forehead, the same test can be repeated by placing the same vibrating tuning fork at the vertex on the top of the head. Some patients find this easier to perceive.
CN IX, X, XI (hypoglossal, vagus and accessory nerves)
The accessory component of the CN XI is not really a cranial nerve but rather high cervical roots travelling up into the cranium and then out to supply the sternocleidomastoid muscles, which turn the head and elevators of the shoulders, the trapezius muscles. Pushing the chin against a hand will activate the sternocleidomastoid muscle opposite to the direction of the force; that is, pushing to the right with the chin will activate the left sternocleidomastoid muscle (and vice versa).
CN XII (glossopharyngeal nerve)
| Cranial nerve | Features |
|---|---|
| I | Sensation of smell—need to test with ‘soft’ scents as astringents may stimulate CN V endings in the nose |
| II |