Chapter 33
The Neurologic Examination
In many respects this chapter is a prologue to the experience of working directly with the patient. Now that many aspects of functional systems neurobiology have been mastered, the opportunity to apply this knowledge is at hand. The neurologic examination is an excellent example of how basic neuroscience can apply directly to events (both normal and abnormal) encountered in the clinical setting. After all, the neurologically compromised patient is simply a normal person whose nervous system is not functioning properly.
OVERVIEW
No other branch of medicine lends itself so well to the correlation of the signs and symptoms of disease with structure and function as does neurology. The neurologic diagnosis of the impaired patient is a deductive process and is reached by a synthesis of all of the details from the history, the examination, and laboratory studies. The neurologic examination is divided into four main segments: mental status, cranial nerves, motor and cerebellar, and sensory.
Figure 33-1 shows a sample set of tools necessary to perform a routine neurologic examination: visual acuity card and eye occluder, ophthalmoscope, dilating eye drops, flashlight, test tube with coffee to assess smell, disposable tongue blade, safety pin, tissue paper, and cotton-tipped applicator. Tuning forks, measuring tape, and reflex hammer as well as a quarter or a wooden cube for sensation testing should also be included.
Figure 33-1. Instruments used to conduct a general neurologic examination.
EVALUATION VERSUS EXAMINATION
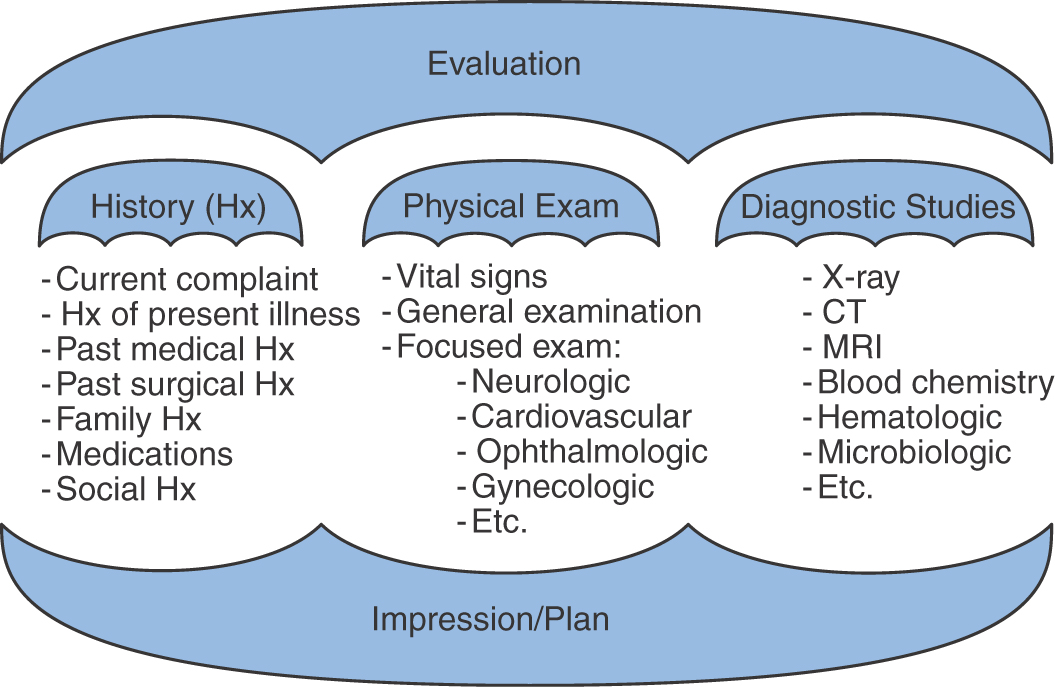
The evaluation and the examination of a patient are different but intimately integrated aspects of the patient-physician encounter. In general, the examination is a small umbrella under the larger umbrella of evaluation (Fig. 33-2).
Evaluation covers all the aspects related to a specific medical event (Fig. 33-2). It includes the current complaint, which is the main reason that the patient seeks medical attention at that time, and the history of present illness, which focuses on the details and circumstances surrounding the main complaint, such as time course (abrupt onset as opposed to slowly progressive), associated symptoms (pain, blurred vision, headache, inability to talk, and so on), and predisposing or concurrent factors (with exercise or physical activity, warm weather, or exposure to drugs). Remember that it is essential to obtain information from an observer, such as a family member or friend, to characterize many neurologic conditions (such as seizures, dementia, and loss of consciousness) when the patient may not be aware of the events. The past medical and surgical histories focus on learning facts about past illnesses; concurrent medical problems, such as arterial hypertension, diabetes mellitus, or history of cancer, may be pertinent to the new medical complaint. Surgical procedures that the patient may have had in the past are also important clues in the medical history. Family history is an essential part of the medical history and may explain the present medical issue. For example, some forms of hand tremors or strokes at an early age may be genetically determined. Social history inquires about the patient’s habits such as smoking, alcohol or illicit drug abuse, life style, and occupation. Medications that the patient is taking are also detailed in the history. Review of systems is a systematic general review of all systems, including cardiovascular, respiratory, genitourinary, and gastrointestinal.
Physical examination, or simply examination, is an important part of the more extensive evaluation of the patient (Fig. 33-2). In general, it includes the patient’s vital signs and a general examination by systems with a more focused examination of the system involved in the current medical problem. For example, if the patient complains of acute onset of chest pain and shortness of breath, a detailed cardiovascular examination is in order with a general examination of the abdomen and a brief neurologic examination. On the other hand, if a patient has sudden onset of weakness of the right side of the body and difficulty speaking, a detailed neurologic examination is called for.
Diagnostic studies (Fig. 33-2) may be ordered as a result of the overall evaluation of the patient to confirm a possible diagnostic hypothesis. For example, chemical, cytologic, and bacteriologic examination of cerebrospinal fluid can be done to confirm suspected meningitis, or computed tomography or magnetic resonance imaging of the brain can be ordered to confirm the localization of a stroke and to determine whether it is ischemic or hemorrhagic.
Finally, the impression (Fig. 33-2) of the evaluating physician of what and where the problem might be with recommendations on management and therapy indicated simply puts together the overall evaluation by the examiner and sets the immediate course of treatment and future health care plans for the patient.
MENTAL STATUS EXAMINATION
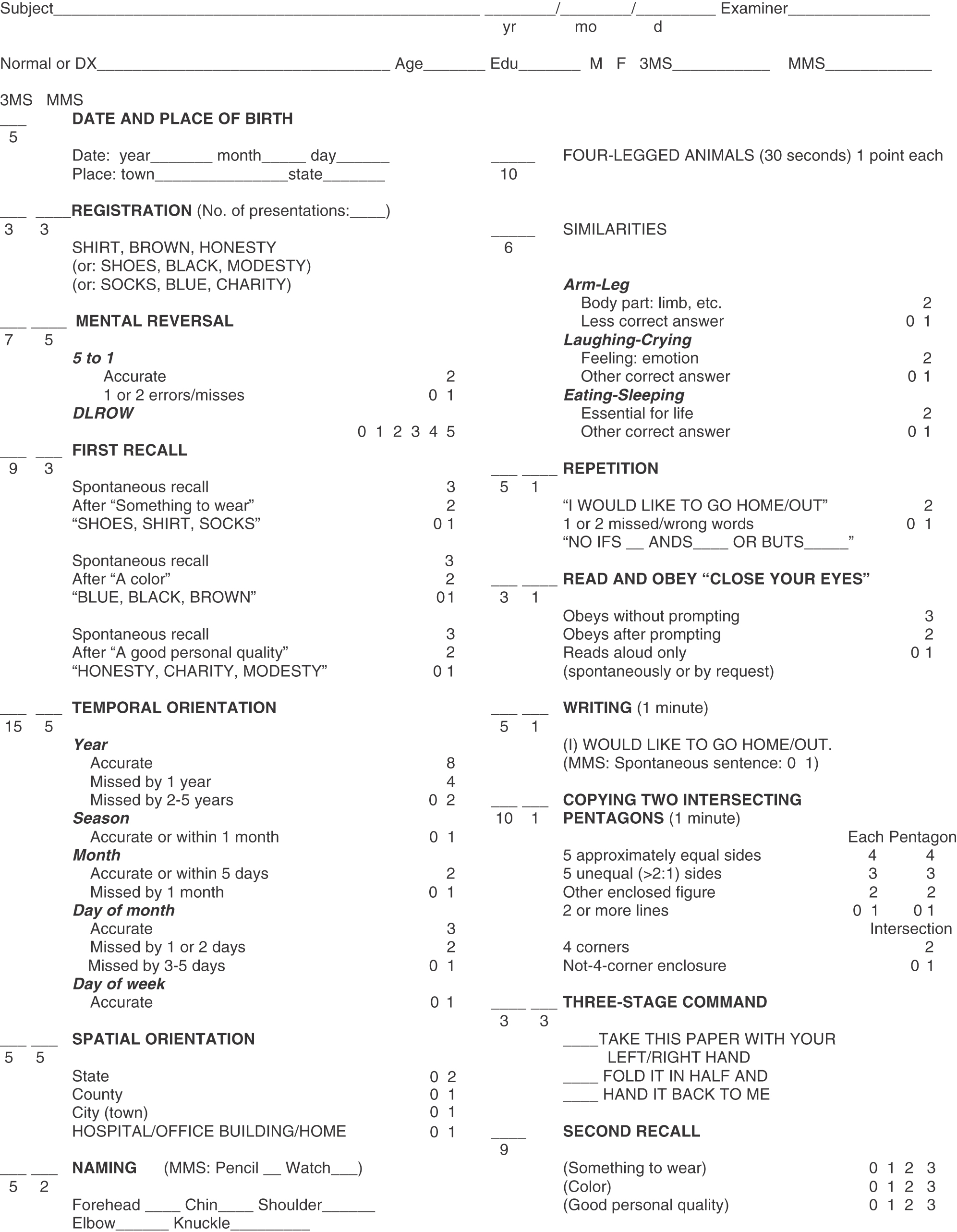
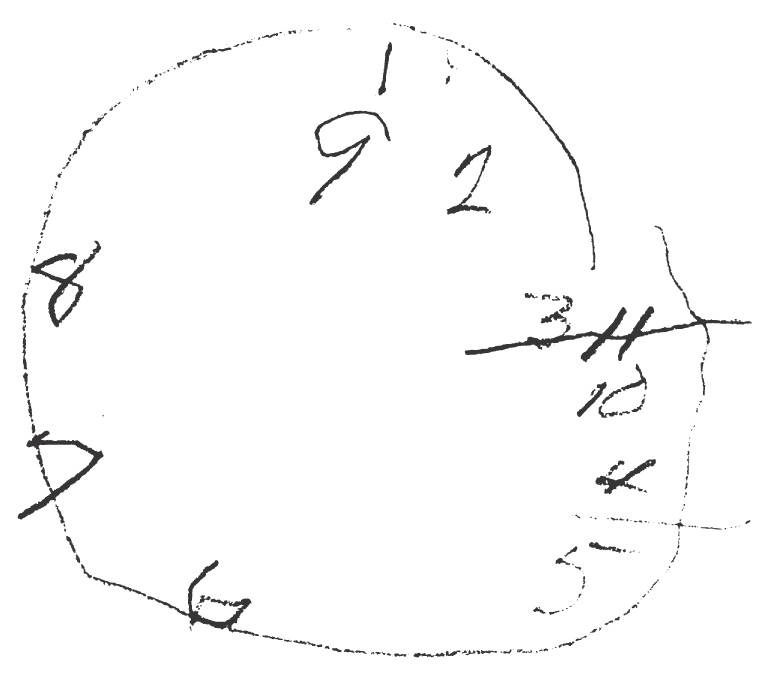
The mental status examination starts first with an assessment of the level of consciousness of the patient. Orientation to time, place, and person should also be documented. Memory of past events and short-term memory as well as the ability to calculate are also evaluated at this time. This basic examination is known as the Folstein Mini-Mental Status test (Fig. 33-3). Special tests of parietal lobe function include drawing a clock face (Fig. 33-4), bisecting a line, and copying a picture of a daisy or drawing a set of intersecting pentagons.
Figure 33-3. The Folstein Mini-Mental Status examination.
Figure 33-4. A clock face drawn by a patient with a parietal lobe lesion.
Speech disorders such as dysarthria are detectable in ordinary conversation and result from defects of articulation of the words secondary to tongue (cranial nerve XII), palate (cranial nerves IX and X), lips (cranial nerve VII), or pharyngeal muscle weakness or incoordination. Evidence of a speech disorder is usually pursued by asking the patient to repeat a difficult phrase like “Methodist Episcopal” or to repeat the sounds “puh-tuh-kuh” rapidly.
Language is the ability to use and to understand written and spoken speech and is a function of the cortical, thalamic, and basal nuclei language circuits located in the dominant cerebral hemisphere. Language is assessed by asking the patient to repeat words or phrases (“no ifs, ands, or buts”), to name simple objects (watch, finger, pen), to follow commands (touch your left shoulder, close your eyes, point to the ceiling), and to write a sentence and read it aloud.
Language abnormalities are called aphasias. There are two major types: nonfluent aphasia and fluent aphasia. In nonfluent aphasia, the patient has difficulty with verbal self-expression, producing the words only with great effort, but is able to understand and to follow commands appropriately. Nonfluent aphasia is also called an expressive or Broca aphasia; a lesion resulting in this type of deficit is found in the inferior frontal gyrus (sometimes called the Broca convolution) specifically involving the pars opercularis and the pars triangularis. In fluent aphasia, the patient has normal or even increased production of words, sometimes in long sentences with normal prosody (rhythm of speech); well-articulated but frequent neologisms (a series of meaningless words) give these sentences no content or meaning. In fluent aphasia, also called a receptive or Wernicke aphasia, neither the patient nor the examiner is able to understand the meaning of the patient’s speech. A lesion of the lateral aspect of the dominant hemisphere in the area of the supramarginal and angular gyri (and sometimes adjacent portions of the superior temporal lobe) may result in fluent aphasia.
CRANIAL NERVE FUNCTION TESTING
Cranial Nerve I
The olfactory nerve (cranial nerve I) is rarely tested because of the deleterious effects of smoking and sinus disease on the sense of smell in the general population. The nerve can be unilaterally damaged by trauma or a tumor of the skull base in the olfactory groove, such as an olfactory groove meningioma (see Fig. 7-9). Total loss of the ability to smell (anosmia) is always associated with the inability to taste food (ageusia) as well, a familiar example being the unappealing taste of food associated with the nasal congestion of a head cold. Dysgeusia is an unappealing or altered sense of taste, and parosmia is an altered or perverted perception of odors.
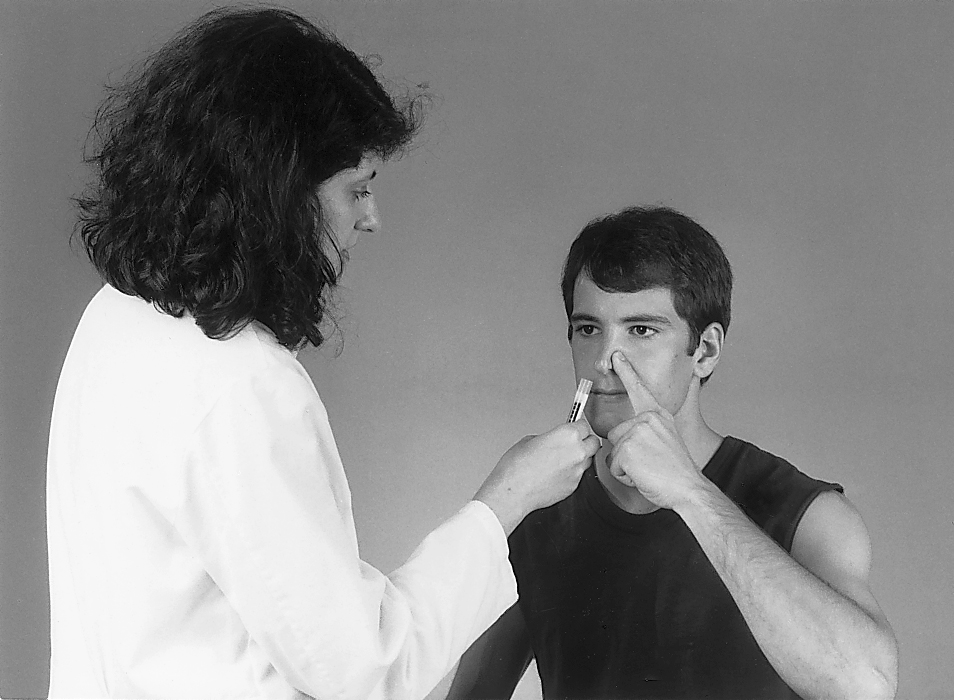
An olfactory stimulus should be nontrigeminal, that is, it should not tickle or irritate the inside of the nose (as does ammonia, for example), which is innervated by the trigeminal nerve. Commonly used substances are vanilla, coffee, and perfumed soap. With the patient’s eyes closed, occlude one nostril and bring a vial of the substance near the open nostril (Fig. 33-5). Ask the patient whether he or she smells something. The sensing of odor is more important than its identification. The process is then repeated for the other nostril.
Cranial Nerve II
The optic nerve (cranial nerve II) is tested by measurement of visual acuity (a measurement of the ability to detect fine detail and contrast in an image) and assessment of the extent of peripheral vision by examination of visual fields and by inspection of the retina and the optic nerve head with the ophthalmoscope. Visual acuity (also called visual resolution) is tested separately for each eye and should be recorded with use of the patient’s best spectacle correction and a hand-held visual acuity chart or a Snellen chart at 20 feet (Fig. 33-6). The number beside each line of letters indicates the number of feet at which the letters can be read by a person who has normal vision; thus, normally, the letters in the line designated 20 can be read at 20 feet, and the visual acuity is recorded as 20/20.
Figure 33-6. The hand-held visual acuity chart.
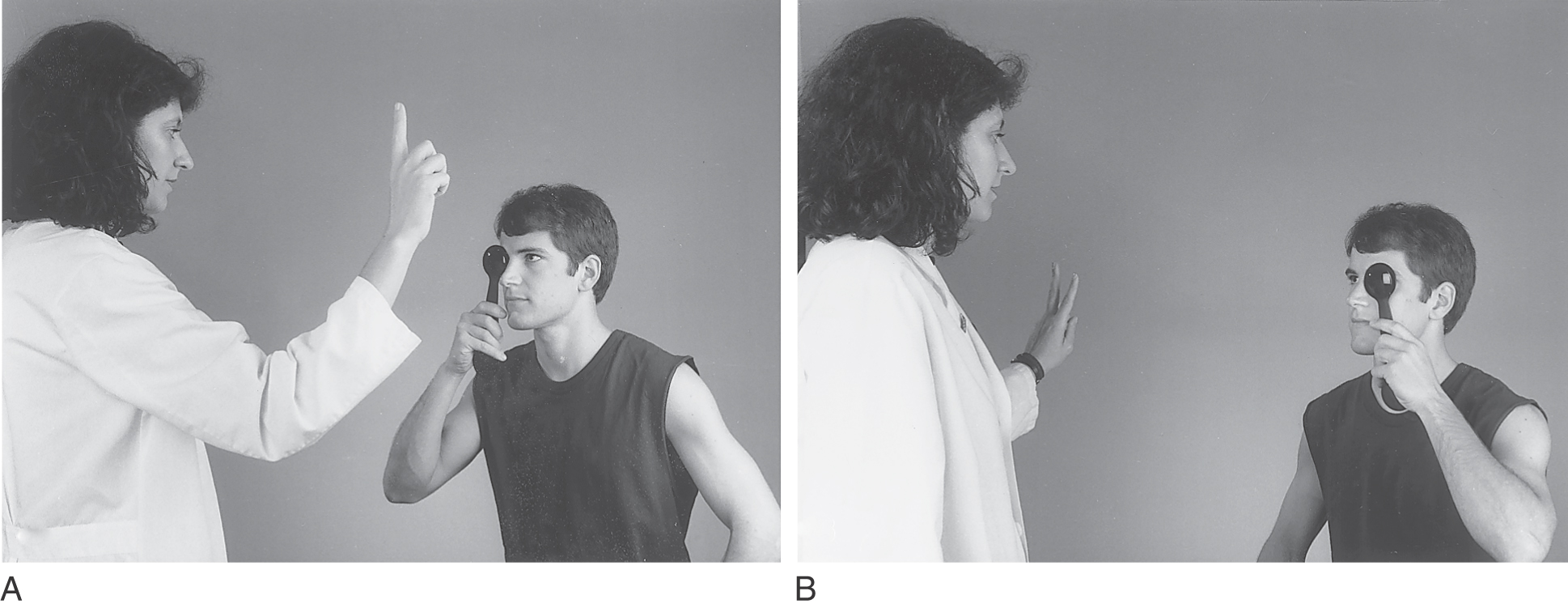
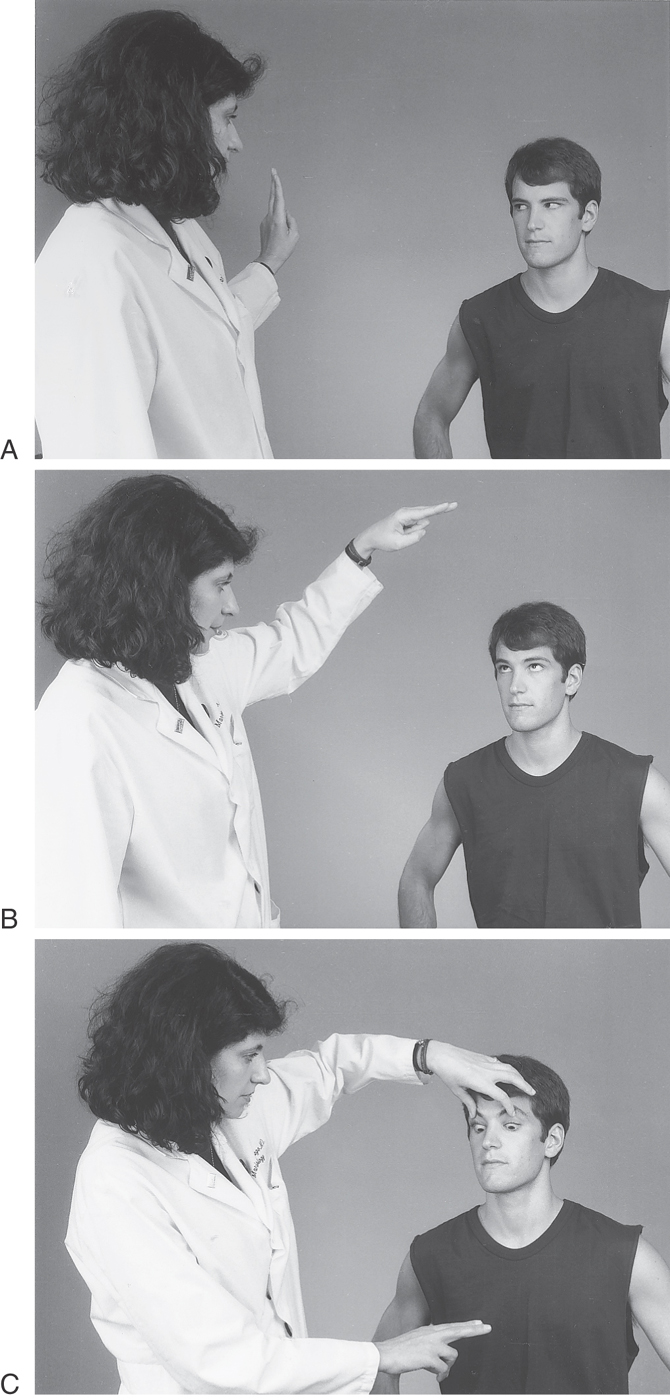
Examination of the visual fields is an important part of the ophthalmologic and neurologic examination. This procedure provides information about the entire visual pathway from the optic nerve to the occipital cortex. Because lesions interrupting various parts of the pathway cause specific types of defects in the visual field, it is frequently possible to determine the location of the lesion (see Chapter 20 for examples). There are several different methods for evaluation of the visual field. The most common method used by most neurologists at the bedside is the confrontation visual field examination. The examiner faces the patient being examined. The patient should cover one eye with the palm of the hand or with an eye occluder and fixate the gaze of the eye to be examined on the examiner’s nose. The examiner then presents a stimulus in each of the four quadrants—upper and lower nasal and upper and lower temporal—of the visual field; finger movement, rapid finger counting, or hand comparison may be used for this purpose (Fig. 33-7).
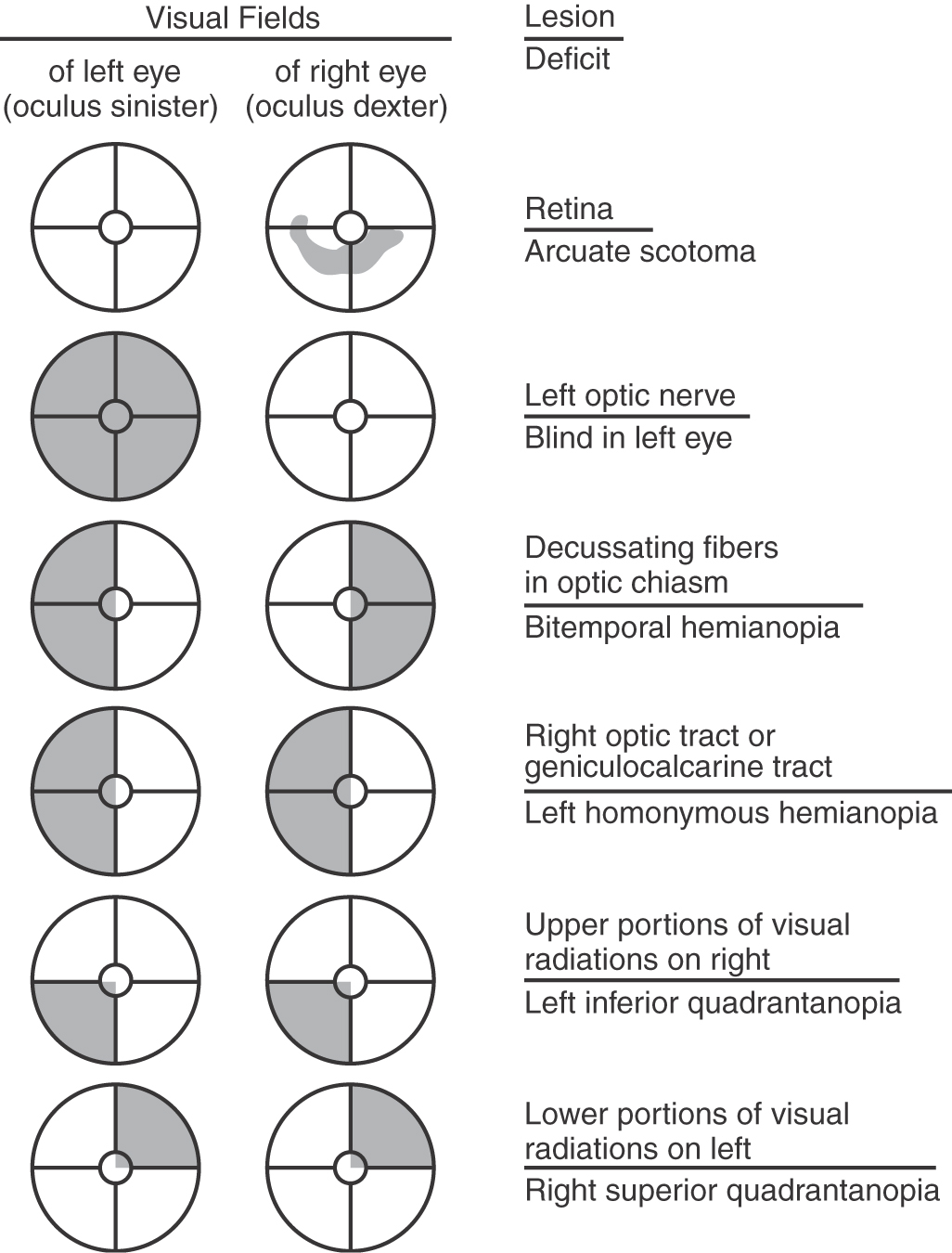
Lesions of the various structures collectively making up the visual pathway give rise to deficits that are characteristic of the specific portion of the pathway compromised. These lesions and corresponding deficits are considered in detail in Chapter 20 and are only summarized here (Fig. 33-8). A scotoma (Greek for “spot”) is a defect of the visual field surrounded by normal vision. A scotoma is most frequently the result of a lesion within the retina or the optic nerve but may also be seen in cases of stroke or tumor along the course of the visual pathway. It is perceived as an area within the field of vision where the patient cannot see. The blind spot is a physiologic scotoma that represents the position of the optic disc within the visual field (the optic disc has no rods, cones, or ganglion cells; see Chapter 20).
Figure 33-8. Representative visual field deficits as correlated with the name of the deficit and the location of the lesion. Also consult Chapter 20 for more information on the visual system.
Lesions of the visual pathway result in characteristic visual deficits. There are many variations to this theme, and only a few examples are illustrated in Figure 33-8 (for more detail on the visual system, consult Chapter 20). For example, loss of vision in half of the field in one eye is called hemianopia, and loss of vision in corresponding halves of the visual fields of both eyes is called right or left homonymous hemianopia, depending on which visual fields are lost. Loss of vision in the temporal halves of the visual fields of both eyes is called bitemporal hemianopia. The loss of a quadrant of the visual field, a homonymous quadrantanopia, is most commonly seen in lesions involving the white matter between the lateral geniculate body and the visual cortex, which is located on the superior and inferior banks of the calcarine sulcus in the occipital cortex.
The retinotopic organization is well preserved throughout the visual pathway. A careful examination of visual field deficits may be instrumental in precise localization of these lesions (Fig. 33-8).
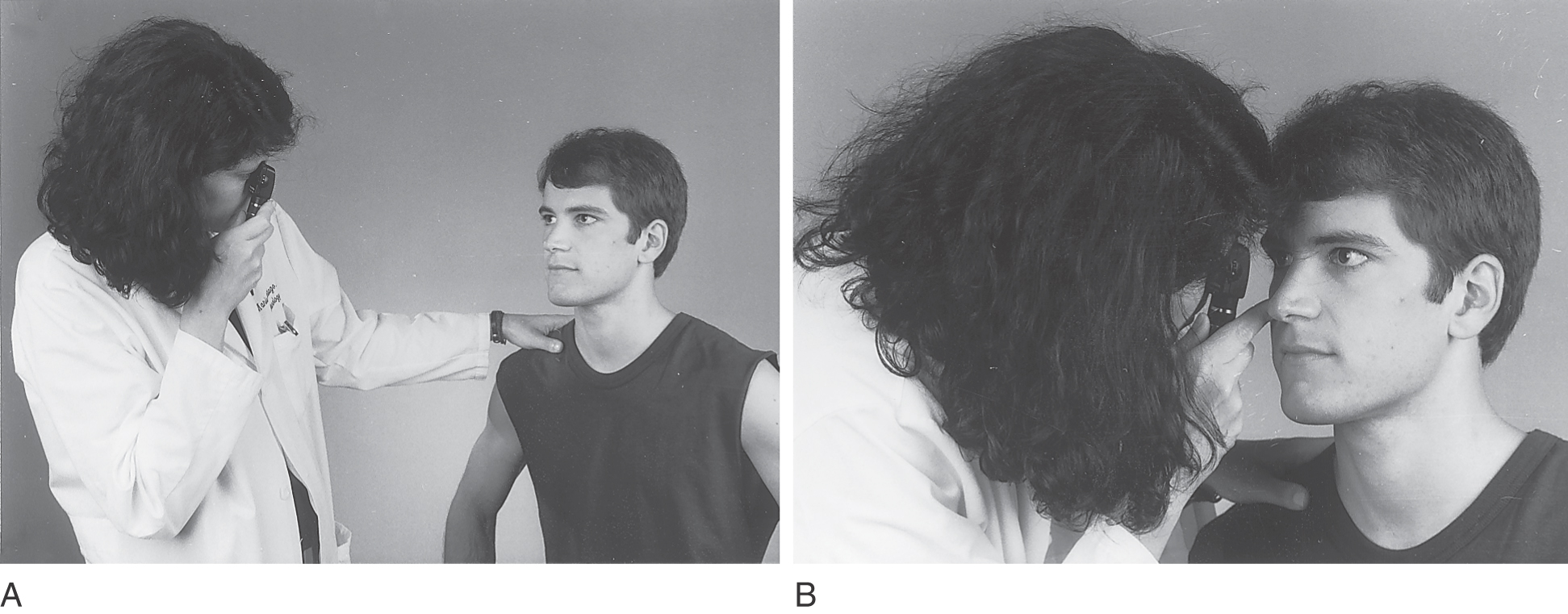
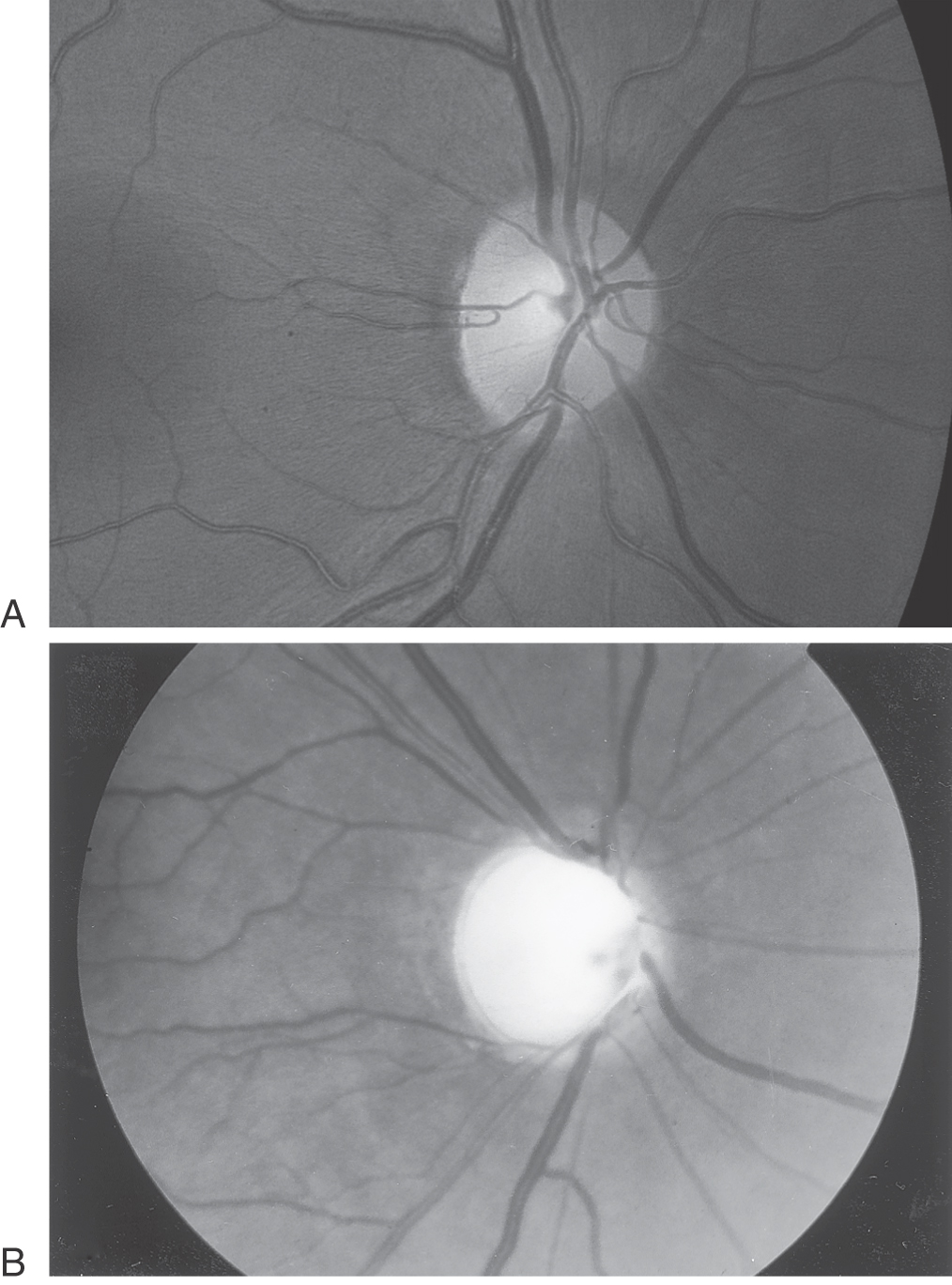
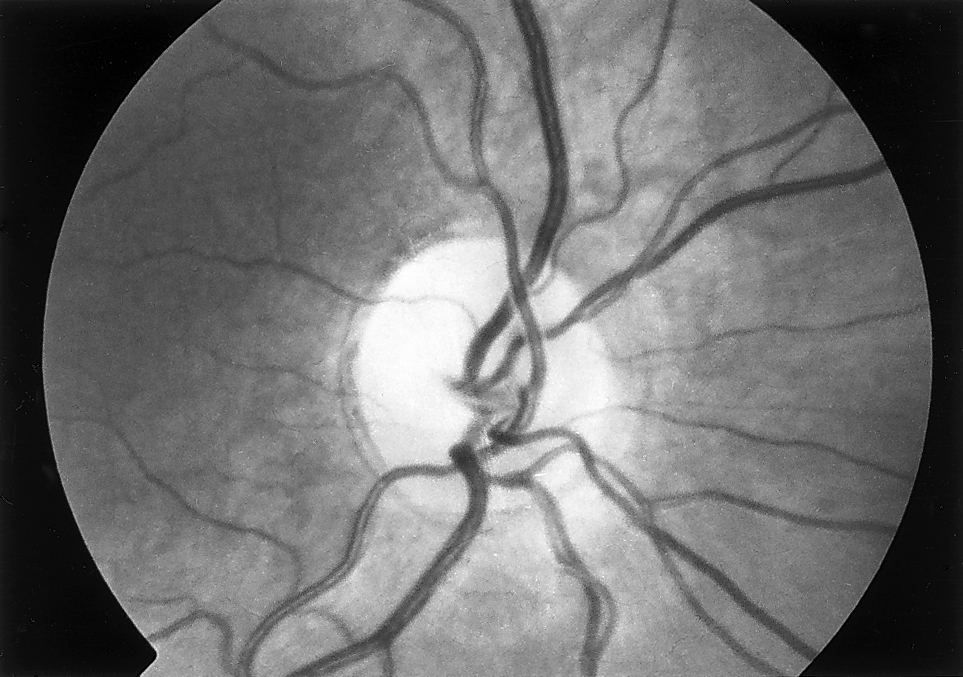
The appearance of the optic nerve head or the optic disc is examined with an ophthalmoscope (Fig. 33-9) while the patient looks at a distant object. To examine the patient’s right eye, the examiner holds the ophthalmoscope with the right hand and uses his or her own right eye; this technique is reversed for examination of the patient’s left eye. With the ophthalmoscope dial set on zero, the pupillary red reflex (the point at which the red retinal reflex is seen “glowing” in the pupil) is located from a distance of 2 or 3 feet (Fig. 33-9A). The examiner slowly approaches the patient’s eye as if viewing the eye through a keyhole. At the same time, plus or minus lenses, as needed, are dialed on the ophthalmoscope to focus on the patient’s retina. The optic disc is located by directing the ophthalmoscope slightly toward the nasal side of the patient’s retina (Fig. 33-9B). The appearance of the optic disc is important. It is normally round or slightly oval and of a yellow-red color, with clearly defined margins (Fig. 33-10A). Veins are darker and slightly larger in diameter than arterioles. The presence of the central cup, or excavation, and its size should be documented (Fig. 33-10B).
Figure 33-10. Normal optic disc (A) and an example of an abnormally enlarged central cup (B) in a patient with glaucoma.
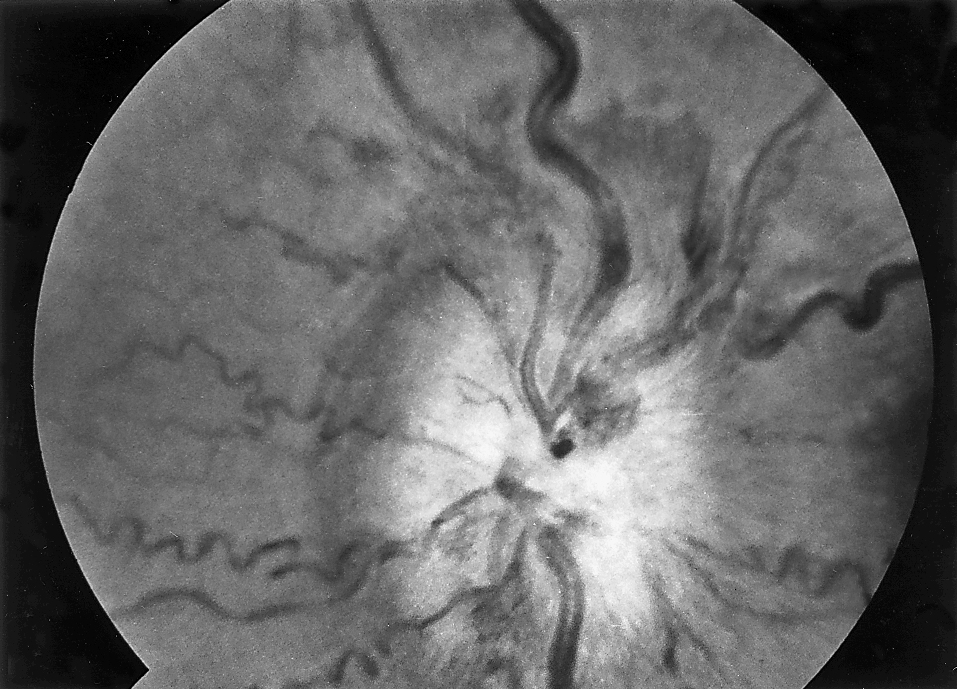
Papilledema, or swelling of the optic disc, is usually due to increased intracranial pressure, regardless of the cause of the pressure increase. Early signs of papilledema include disappearance of the normal cup, blurring of the disc margins, and arching and elevation of the vessels as they pass over the margin of the disc. As papilledema progresses, exudates and hemorrhages as well as tortuosity of the vessels appear (Fig. 33-11).
Figure 33-11. Papilledema with hemorrhages. Observe the tortuosity of vessels.
Optic atrophy may be primary or secondary. Primary optic atrophy results from different processes involving the optic nerve, such as retrobulbar optic nerve injury, compression by a tumor, or demyelination. Secondary optic atrophy is a consequence of chronic increased intracranial pressure, infarctions, or diseases such as syphilis (Fig. 33-12).
Figure 33-12. Optic atrophy. Note the pale appearance of the optic disc.
Cranial Nerves III, IV, and VI
The oculomotor, trochlear, and abducens nerves (cranial nerves III, IV, and VI) are usually examined as a group because they act together in controlling ocular muscles to ensure that the eyes remain parallel throughout their range of motion. A lesion affecting one or more of these nerves results in weakness of the corresponding muscles, manifested by diplopia or double vision. Ocular motility is tested by having the patient follow the examiner’s finger in upgaze and downgaze and from side to side (Fig. 33-13A–C).
The oculomotor nerve innervates the superior, medial, and inferior rectus muscles; the inferior oblique; and the constrictor of the pupil and the ciliary body as well as the levator of the eyelid (see Fig. 28-1). A complete lesion of the oculomotor nerve results in paralysis of the ipsilateral muscles innervated by the nerve and ptosis, pupillary dilation, and inability to look upward, downward, or inward. Aneurysms of the internal carotid artery or posterior communicating artery and pressure from herniation of the uncinate gyrus (uncus) in expanding lesions of the cerebral hemisphere are common causes of a peripheral complete third nerve palsy with pupillary involvement.
The trochlear nerve innervates the superior oblique muscle (see Fig. 28-1). When the fourth nerve is damaged, the affected ipsilateral eye is higher than the normal opposite eye, and it cannot be turned downward when the eye is rotated inward (adducted). The position of the globe (eyeball) is higher relative to the position of the other globe because the superior oblique muscle normally depresses the eyeball. When this muscle is weak or paralyzed, the eyeball will not depress normally relative to the other eye. Thus it is higher than the normal eye. It is important to recall that fibers arising in the trochlear nucleus cross the midline before exiting the brainstem to become the nerve. Consequently, the right nucleus innervates the left muscle, and the left nerve innervates the left muscle.
The abducens nerve controls the ipsilateral lateral rectus muscle, which makes the eye look outward (laterally). Defects in abduction (from a lesion of the sixth cranial nerve, for example) give the patient a “cross-eyed” appearance because the normal eye is oriented straight ahead and the affected eye is rotated slightly inward (medially) as a result of the unopposed action of the medial rectus muscle on that side.
Cranial Nerve V
The trigeminal nerve (cranial nerve V) is both motor and sensory. In sensory testing, its innervation includes the face up to the vertex of the scalp but spares the angle of the mandible (which is innervated by C3). The sensation from the oral and nasal cavities is transmitted through the trigeminal nerve, although these areas are not usually included in the routine neurologic examination (see Chapter 18).
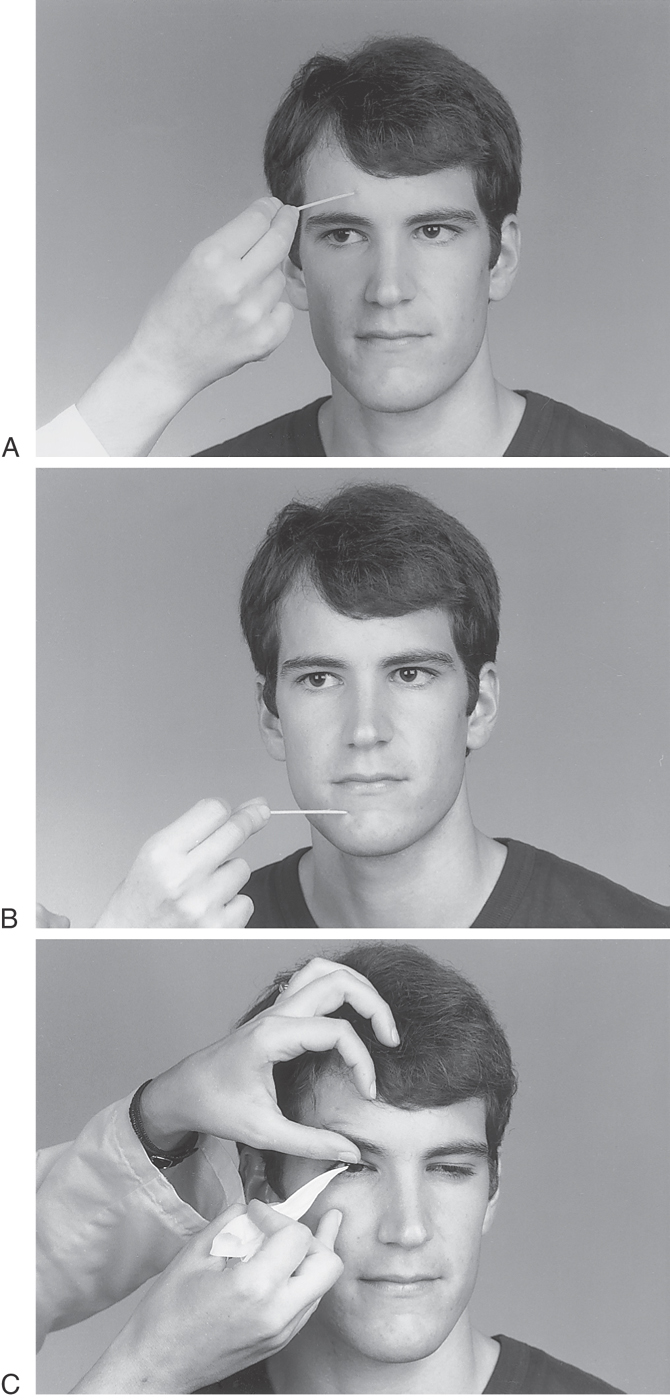
Pain and temperature should be tested in the three divisions of the fifth cranial nerve: the ophthalmic, the maxillary, and the mandibular (Fig. 33-14A, B; also see Fig. 18-4, Fig. 18-5, Fig. 18-14 and Fig. 18-15). The ophthalmic division innervates the scalp as far back as the vertex of the skull, forehead, cornea, conjunctiva, and skin of the side and tip of the nose. Corneal sensation is tested by gently touching the cornea with a cotton-tipped applicator or tissue paper while the patient looks in the other direction (Fig. 33-14C). This maneuver constitutes the afferent limb of the corneal reflex. The normal response is a rapid, partial or complete blinking movement of the eyelid elicited by the efferent limb of the corneal reflex via the facial nerve. The second trigeminal division, the maxillary nerve, conducts stimuli from the skin of the cheek, far lateral aspect of the nose, upper teeth, and jaw. The third division, the mandibular nerve, carries sensory and motor impulses. The sensory distribution is skin of the lower jaw, pinna of the ear, and lower teeth and gums as well as the side of the tongue.
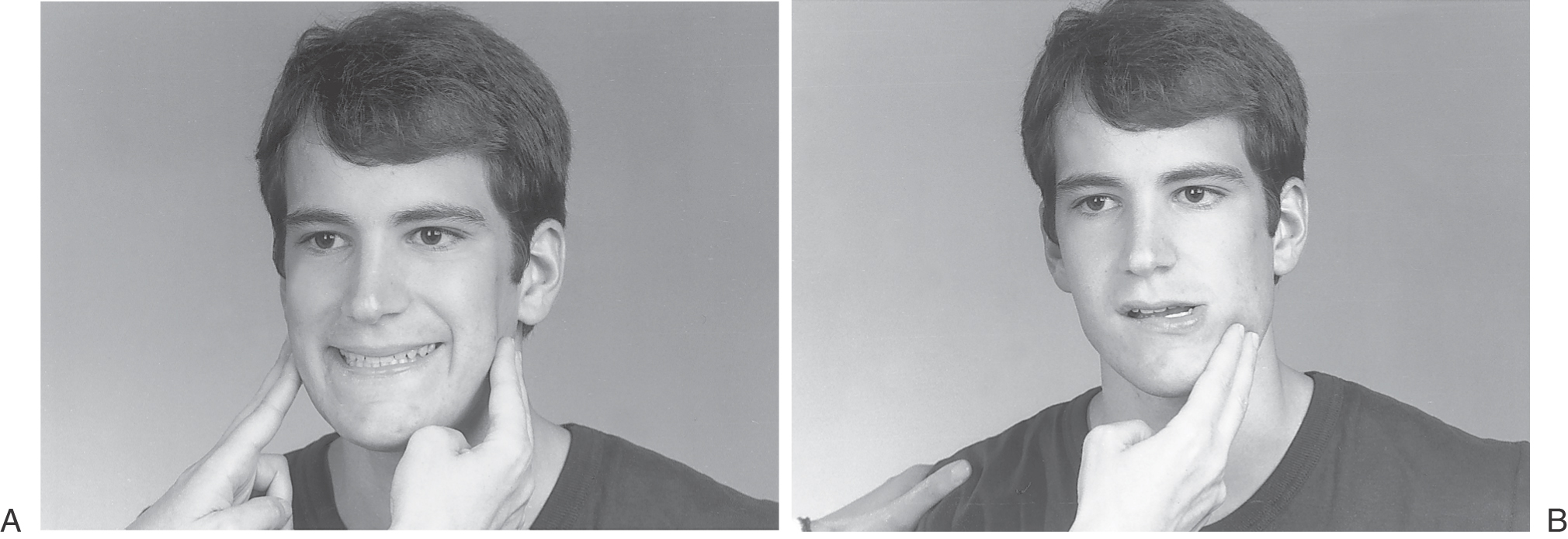
The motor fibers supply the muscles of mastication: the temporal, masseter, and pterygoid muscles. The temporal and masseter muscles are examined by having the patient close the jaws together while the examiner palpates these muscles (Fig. 33-15A). The pterygoid muscles are responsible for side-to-side movements of the jaw as well as aiding in closure of the jaw (Fig. 33-15B). A lesion of the motor fibers of the trigeminal nerve results in weakness of the masticatory muscles on that side and a slight deviation of the jaw toward the weak side, on jaw closing, because of the unopposed action of the healthy contralateral pterygoid muscles. The jaw jerk reflex is elicited by a gentle tap on the chin, with resultant closure of the jaw by the masticatory muscles. The afferent limb of this reflex is via receptors in the muscles of mastication that enter the brainstem on fibers of the mesencephalic tract, and the efferent limb is in response to collaterals of these fibers that bilaterally innervate the motor trigeminal muscles (also see Fig. 14-18).
Cranial Nerve VII
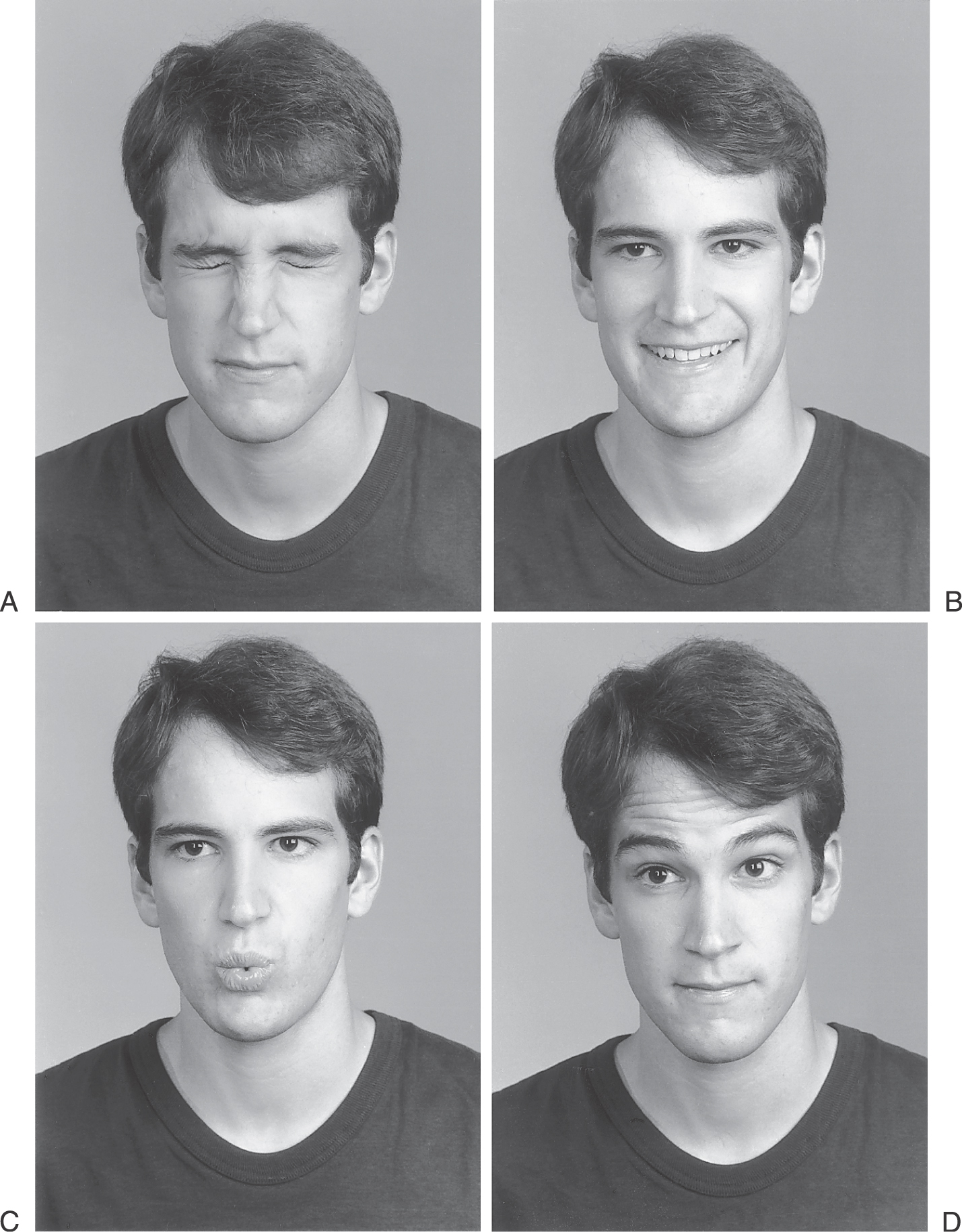
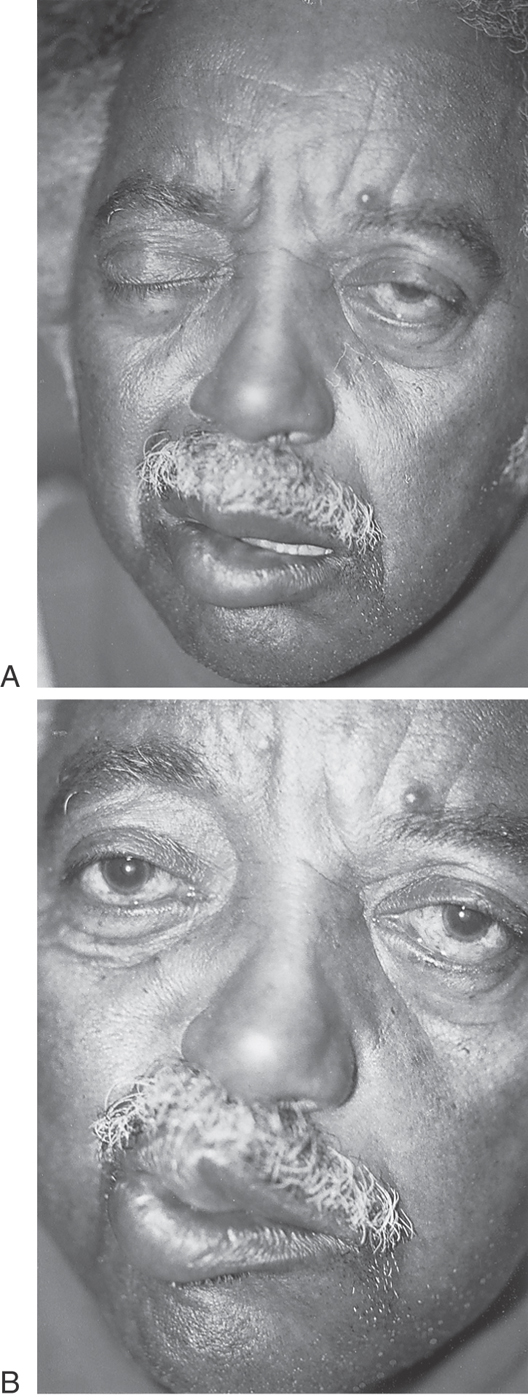
The facial nerve (cranial nerve VII) is a complex nerve with motor, sensory, and parasympathetic (visceromotor) fibers. The motor portion of the nerve innervates the muscles of facial expression and is tested by instructing the patient to wrinkle the forehead, to close the eyelids tightly, to smile or grimace showing the teeth, and to pucker (Fig. 33-16). There are two types of facial motor weakness, one with involvement of the upper motor neuron or corticonuclear pathways, and the other with involvement of the lower motor neuron or “peripheral” seventh nerve palsy. The “central” or upper motor neuron facial palsy is characterized by inability to retract the corner of the mouth; forehead function and eyelid closure remain unaffected for the most part. Lesions in the facial nucleus or the nerve proper will cause paralysis of half of the entire face, with inability to wrinkle the forehead or to close the eyelids and lips on the affected side (Fig. 33-17; also see Fig. 25-15).
Figure 33-17. A patient with a lesion of the facial nerve. The patient has difficulty closing his left eye (A; compare with Fig. 33-16A, B), and the left corner of his mouth droops, a defect that is especially evident when the patient attempts to purse his lips (B; compare with Fig. 33-16C).
The sensory portions of the seventh nerve originate from the taste buds in the anterior two thirds of the tongue and from the posterior wall of the external ear canal. Taste can be rarely examined by use of sugar, salt, or quinine solutions. The patient is instructed to protrude the tongue; the test substance is then applied with a cotton-tipped applicator on one side of the tongue. The patient must identify the test substance before drawing the tongue back into the mouth, where function of the posterior portion of the tongue or the contralateral side masks the result of the test. The facial nerve also carries parasympathetic fibers to the maxillary and lacrimal glands (see Chapter 14).
Cranial Nerve VIII
The eighth cranial nerve is made up of two divisions: cochlear, subserving the sense of hearing, and vestibular, subserving the sense of balance—hence its common name, the vestibulocochlear nerve.
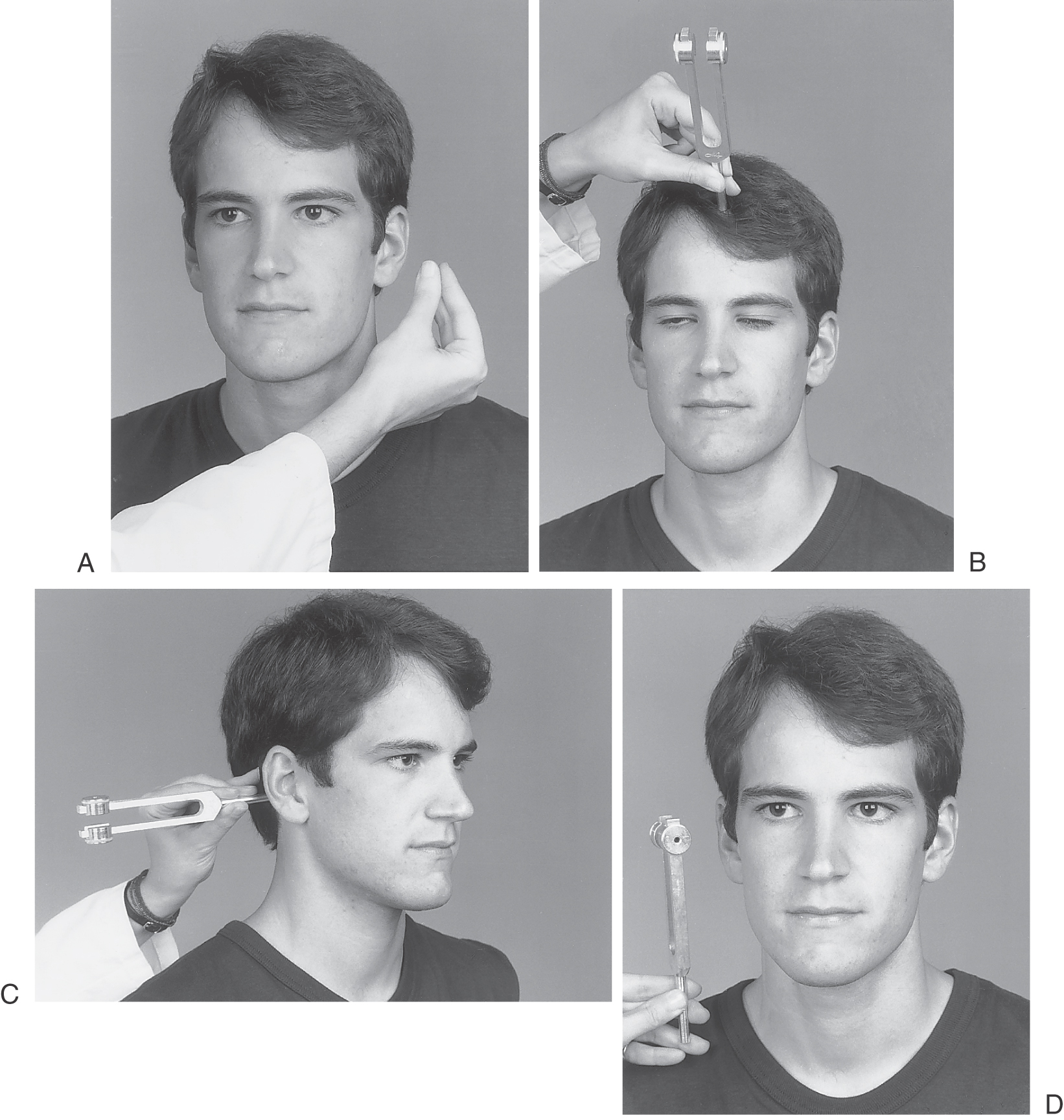
The cochlear division is usually tested by use of a tuning fork with a frequency of 256 vibrations per second to compare bone and air conduction (Fig. 33-18). This examination is known as the Rinne test. In the normal ear, air conduction is greater than bone conduction. The vibrating tuning fork is placed against the mastoid bone (Fig. 33-18C), and the patient is instructed to indicate when he or she no longer senses the vibration. The tuning fork is then placed near the external auditory canal (Fig. 33-18D), and the time for air conduction is estimated. With a normal test result, the time for air conduction is about twice that for bone conduction. Bone conduction will be louder in conductive hearing loss; both air and bone conduction are abnormal in neurogenic hearing loss. The Weber test is performed by placement of the tuning fork on the vertex of the skull (Fig. 33-18B); normally, the vibration is perceived equally in both ears. If there is disease of the middle ear or the external ear is blocked (conductive hearing loss), the vibration is lateralized to the affected side. If the cochlear nerve is involved on one side (neurogenic hearing loss), the sound is heard better on the opposite or the normal side.
The vestibular division of the acoustic nerve is assessed with use of rotational and caloric stimuli to produce changes in the endolymph current in the semicircular canals (see Chapter 22). Typically, patients with vestibular dysfunction complain of vertigo, nausea and vomiting, and difficulty with balance, especially with movement of the head. Vertigo may be perceived by the patient as movement of the environment around him or her (objective vertigo), or the patient perceives that he or she is moving and the environment remains still (subjective vertigo). Vertigo may be induced by visual input or by changes of the body space. The water caloric test, or Bárány test, is done by irrigation of the external auditory canal with 10 mL of cold water while the patient’s head is held at 30 degrees above the horizontal. The patient is then examined for horizontal nystagmus, with the slow component toward the side of the stimulus past the midline and the fast corrective phase of the nystagmus to the opposite side. The mnemonic COWS (cold—opposite/warm—same) refers to the direction of the fast phase of the nystagmus.
Cranial Nerves IX and X
The glossopharyngeal and vagus nerves (cranial nerves IX and X) are usually examined at the same time. Touching the posterior wall of the pharynx with a tongue depressor tests the general sensory fibers of the ninth nerve. The normal response is the prompt contraction of the pharyngeal muscles, including the stylopharyngeus muscle. Afferent information conducted on the ninth nerve and the resultant contraction of the stylopharyngeus muscle constitute the circuit of the gag reflex.
Vagus nerve dysfunction will result in ipsilateral paralysis of the palatal, pharyngeal, and laryngeal muscles. In such cases, the voice is hoarse (dysarthria) as a result of weakness of the vocal cord (and vocalis muscle) and speech has a nasal sound. In addition, the patient may experience difficulty in swallowing, or dysphagia, or may experience changes in heart rate, such as tachycardia. The soft palate should be observed while the patient says “ah.” Normally, the uvula remains in the midline, but in cases of weakness of the palate on one side, it is pulled toward the contralateral side because of the unopposed action of muscles on the healthy side (also see Fig. 25-16).
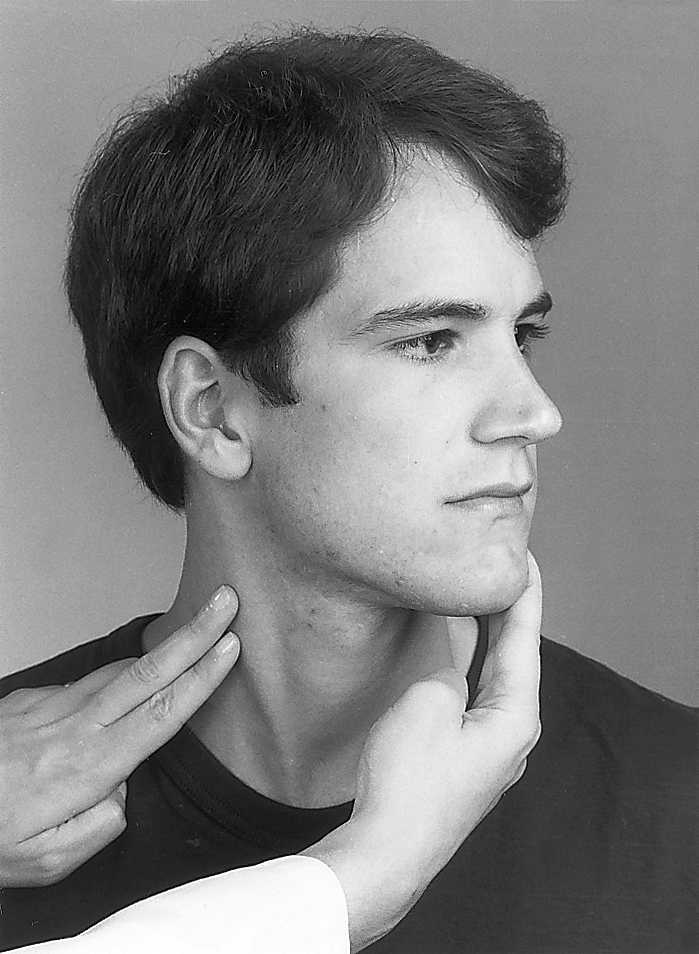
Cranial Nerve XI
The spinal accessory nerve (cranial nerve XI) innervates the ipsilateral sternocleidomastoid and trapezius muscles. It is examined by having the patient turn the head forcibly against the examiner’s hand away from the muscle being tested while the muscle is palpated (Fig. 33-19); contraction of the sternocleidomastoid muscle turns the head to the opposite side. The trapezius may be tested by asking the patient to shrug his or her shoulder while the examiner is gently pressing down on the shoulder. Damage to this nerve causes inability to shrug (elevate) the shoulder against resistance (weakness of the trapezius muscle), winging of the scapula on the side of the lesion, and inability to rotate the head away from the side of the weak sternocleidomastoid muscle (or toward the strong side).
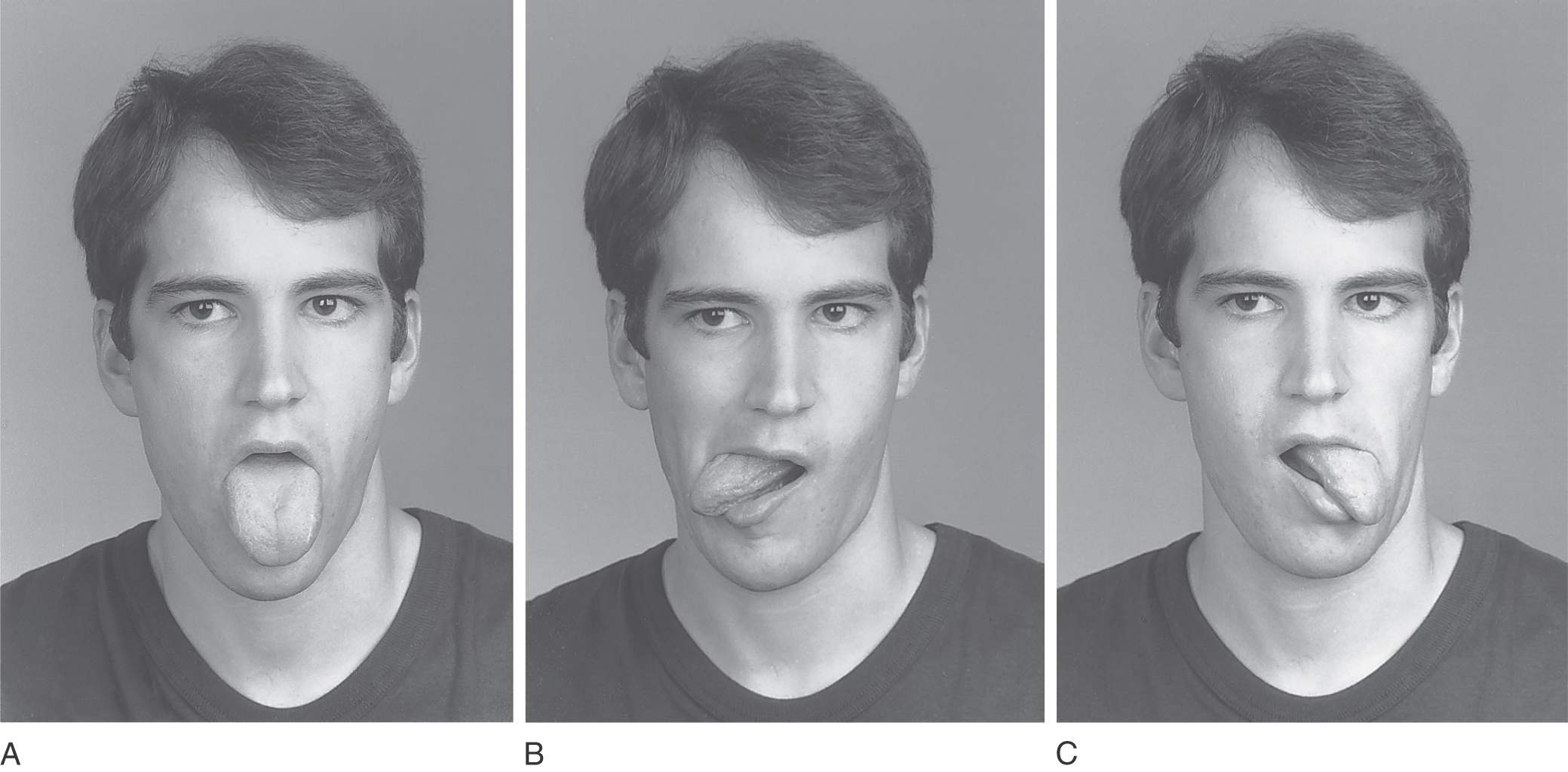
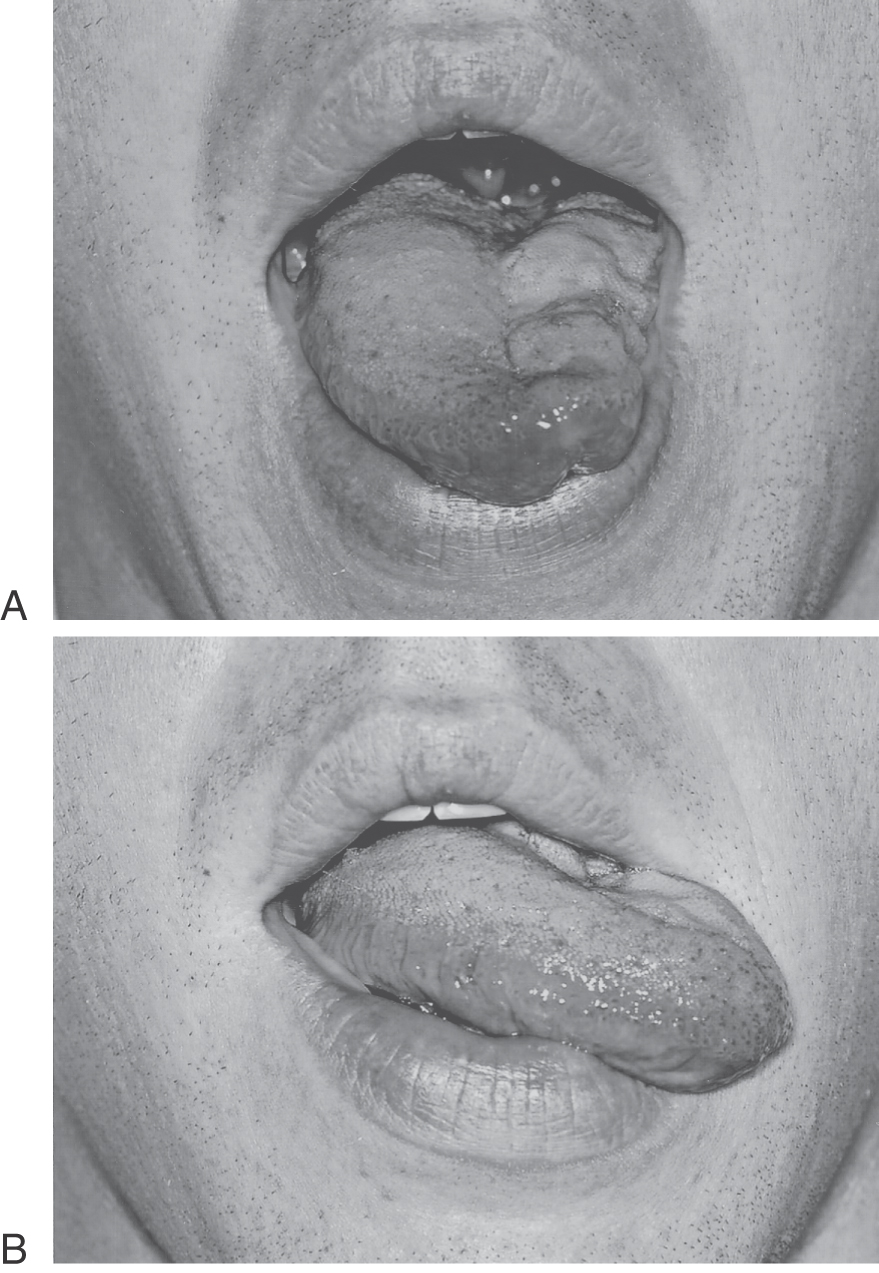
Cranial Nerve XII
The hypoglossal nerve (cranial nerve XII) supplies the extrinsic and intrinsic muscles of the tongue. For the integrity of the hypoglossal nerve to be tested, the patient is asked to protrude the tongue in the midline and to move it from side to side (Fig. 33-20). In the presence of a lesion of the hypoglossal nerve, the tongue is seen to deviate toward the side of the lesion, toward the weak half, on attempted protrusion (Fig. 33-21). This deficit is due to a paralysis of the genioglossus muscle.
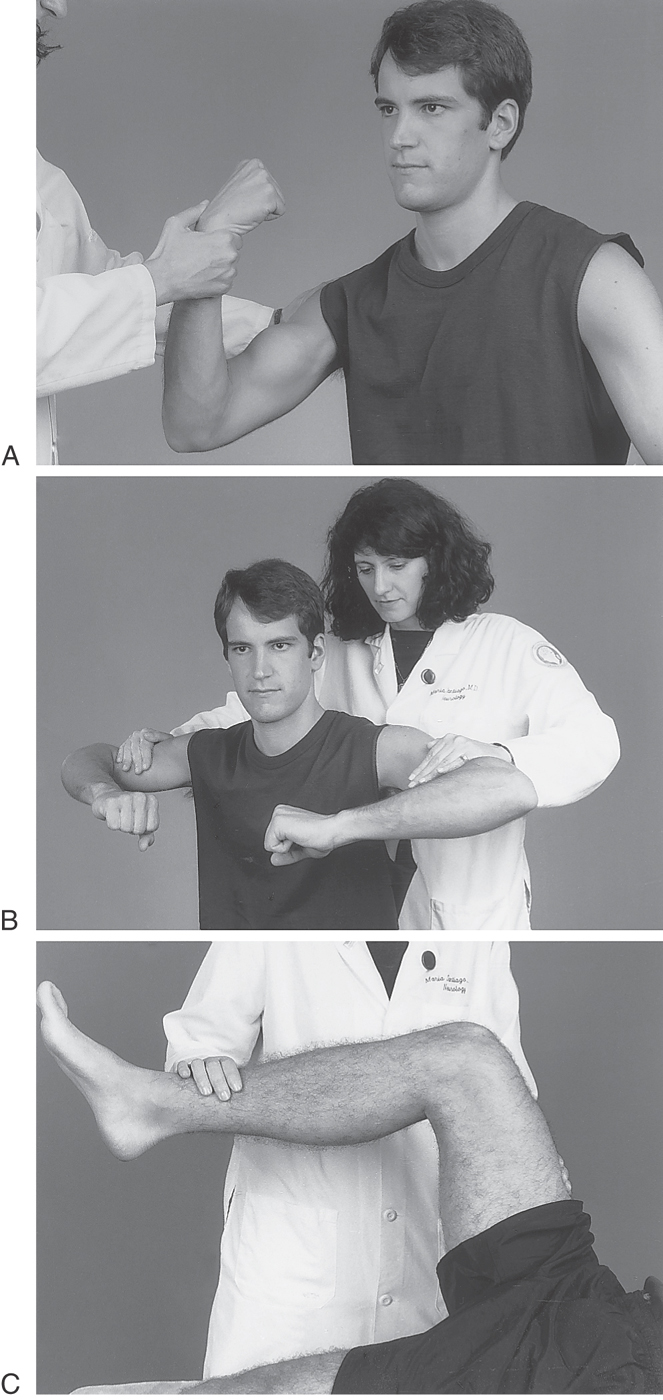
MOTOR EXAMINATION
The motor examination includes a consideration of muscle tone and strength. Tone examination requires that the patient be as relaxed as possible. The patient may respond to suggestions such as “Go loose” or “Let me do all the work and go floppy,” thereby permitting the examiner to move the patient’s limbs freely. Normally, a mild resistance to movement is noted during the whole range of motion. In hypertonicity, increased resistance is present in extensor and flexor muscles. Flexor resistance can range between very mild and so severe as to prevent passive movement. This increased tone is called lead pipe rigidity and is a feature of Parkinson disease (see Chapter 26).
Spasticity is a phasic change in muscle tone brought out by a rapid snap of the limb in extension or flexion. The spastic “catch” is an abrupt increase in the tone followed by a slow release, much as in the operation of the hydraulic hinge on the rear door of a hatchback automobile. Spasticity is seen with corticospinal tract lesions. Hypotonia is characterized by increased ease of passive movements, as exemplified by the pendular swing of a leg extended and released in the sitting position.
Muscle strength testing (Fig. 33-22) requires the patient’s cooperation. Results are usually graded as follows:
+0 = paralysis
+1 = minimal muscle contraction
+2 = muscle contracts but the patient is unable to lift the limb
+3 = able to hold the limb against gravity
+4 = able to hold against resistance but the examiner is able to overcome
+5 = not able to overcome resistance
The different muscle groups are examined in an organized fashion, proximal to distal in the upper and lower extremities, with documentation of the degree and pattern of strength or weakness observed (Fig. 33-22). A lesion in the cerebral hemisphere produces hemiparesis with weakness involving the face and upper and lower extremities on the contralateral side (see Chapter 25). A midthoracic (or slightly lower) lesion in the spinal cord may produce weakness in both lower extremities (paraplegia), with an associated sensory deficit and abnormal sphincter control. Weakness involving only one limb is called monoparesis; it is commonly but not invariably localized to a plexus or a peripheral nerve. A midcervical lesion of the spinal cord may result in quadriplegia (bilateral paralysis of both upper and lower extremities) with a corresponding sensory loss; if the lesion is at the C1 or C2 level, the patient may also experience difficulty in breathing without assistance. A lesion of one side of the spinal cord at midcervical levels may result in paralysis of the upper and lower extremities on that side; this deficit is a hemiplegia and is usually accompanied by characteristic sensory deficits (Brown-Séquard syndrome) (also see Fig. 25-13).
Muscle Stretch Reflexes
The muscle stretch reflexes are obtained in response to percussion of the tendons of major muscles (Fig. 33-23). The muscles are innervated by nerves from specific spinal cord levels. The afferent impulses are conducted to the spinal cord, or the brainstem, by the sensory fibers in the peripheral nerve and the corresponding posterior root or cranial nerve. The impulse then acts on the anterior horn cells of the cord (or motor cells of cranial nerves), and the action potential travels through the motor roots and peripheral nerve back to the muscle (see also Chapter 9). Normal reflexes indicate that the sensory-motor loop to and from the spinal cord (or brainstem) is intact.
Reflexes are modulated by down-coming inhibitory and excitatory influences from the cortical, vestibular, and reticular regions of the cerebral hemispheres and brainstem (see Chapter 24). When the inhibitory influences are damaged, the resulting reflex elicited by tapping a tendon may be brisk or hyperactive, called hyperreflexia. If the nerve leading to or from the muscle is injured, reflexes may be hypoactive (hyporeflexia) or absent (areflexia).
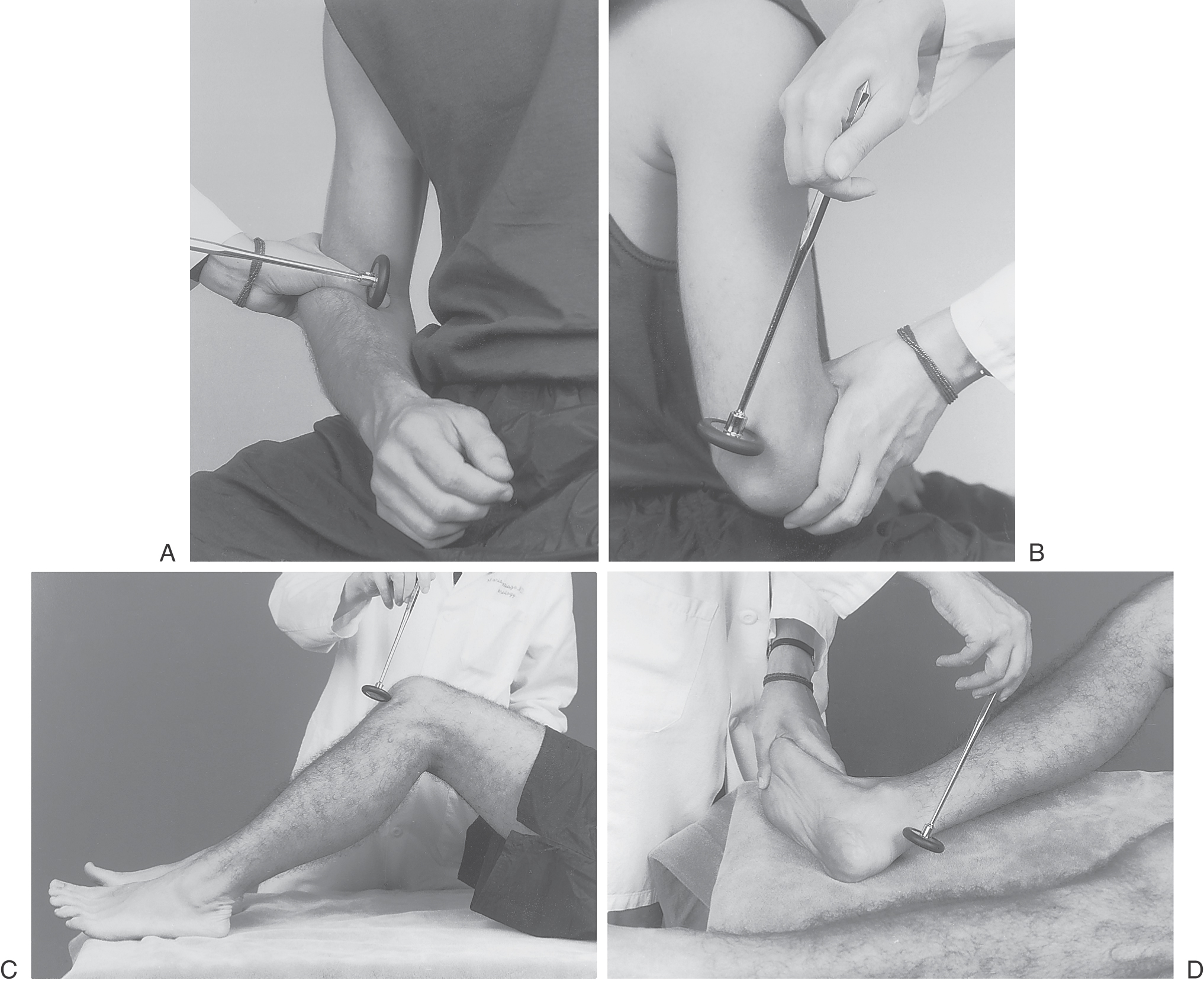
In the upper extremity, four reflexes are usually tested: the biceps reflex (Fig. 33-23A), mediated by C5-C6 through the musculocutaneous nerve; the triceps reflex (Fig. 33-23B), mediated by C7-C8 through the radial nerve; the brachioradialis reflex, mediated by C5-C6 through the radial nerve; and the finger flexor reflex, mediated by C7-C8 through the ulnar and median nerves. In the lower extremity, two reflexes are commonly tested: the quadriceps reflex, commonly called the patellar or knee jerk reflex, elicited by tapping the patellar tendon (Fig. 33-23C) and mediated by L2-L4 through the femoral nerve; and the Achilles reflex or ankle jerk reflex, mediated by S1 through the sciatic (tibial) nerve and elicited by tapping the tendon of the gastrocnemius muscle (Fig. 33-23D).
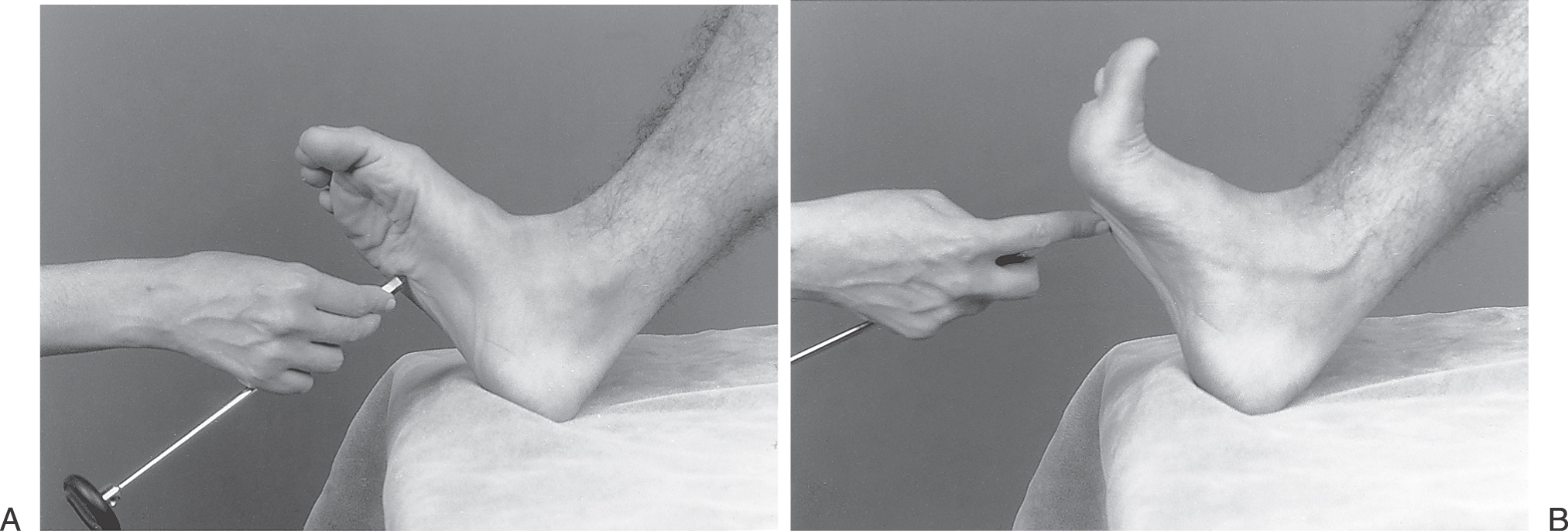
An example of a pathologic reflex is the Babinski sign, seen on stroking of the lateral border of the sole of the foot from the heel to the base of the great toe (Fig. 33-24). This reflex consists of dorsiflexion of the great toe, sometimes with fanning of the other toes (Fig. 33-24B). The normal response is flexion of all of the toes (Fig. 33-24A). In an adult, the Babinski sign indicates some type of abnormal process, whereas this sign may be present in a normal infant. The incomplete myelination seen in newborns or infants is the likely explanation of this latter observation.
Cerebellar Testing
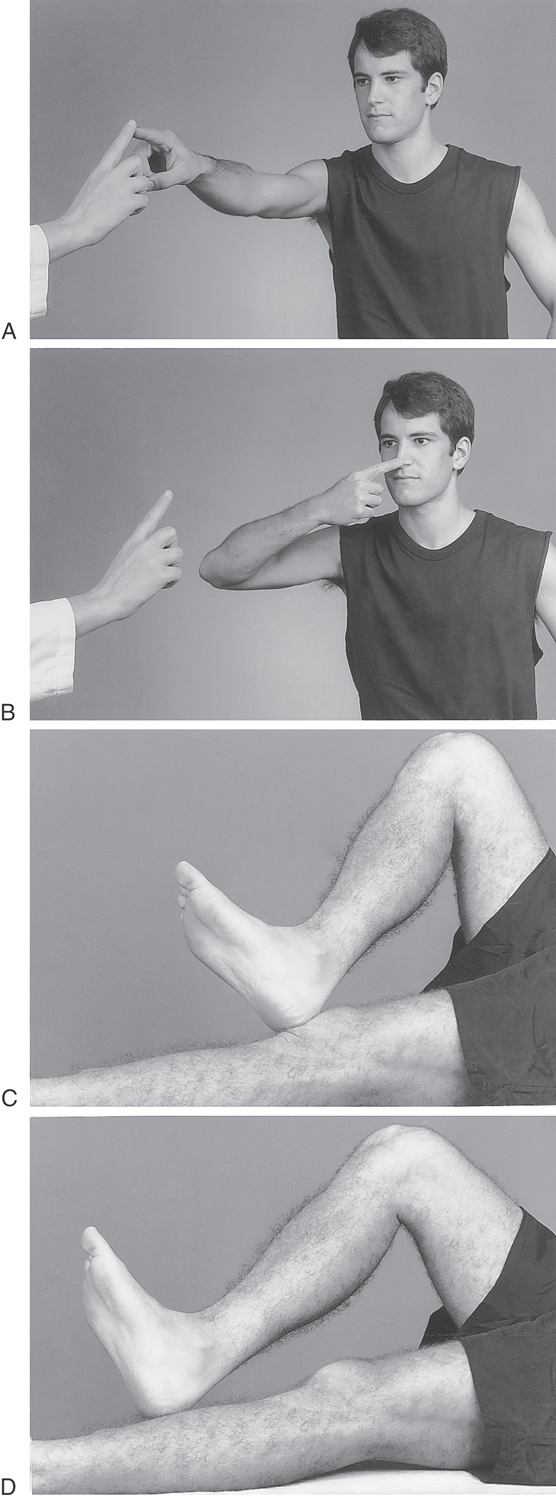
Cerebellar testing can be thought of as a mix of motor and sensory testing that assesses the accuracy of movement. In addition to normal cerebellar function, the patient must have normal strength, tone, and sensory input to carry out coordinated movements. It is important to compare coordination of one side of the body with the other. The cerebellum is usually tested by having the patient perform a finger-to-nose-to-finger maneuver (in which the patient touches alternately the examiner’s finger and then his or her own nose rapidly) (Fig. 33-25A, B); the heel-knee-shin maneuver (in which the patient puts the heel on the opposite knee and runs it down the shin) is performed to test the accuracy of appendicular movement (Fig. 33-25C, D). The inability to perform this maneuver is also called limb ataxia. These types of dysfunctions, largely relegated to the more distal parts of the body—the extremities—are indicative of damage to more lateral portions (the hemispheres) of the cerebellum (also see Fig. 27-20 and Fig. 27-21).
Truncal ataxia (titubation, from the Greek word meaning “to stagger”) is present when the patient exhibits unsteadiness while sitting, standing, or walking in tandem. This finding, in which primarily axial parts of the body are affected, is evidence of midline cerebellar dysfunction.
SENSORY EXAMINATION
Sensory testing is purely subjective; results obtained depend heavily on the patient’s accuracy and cooperation. The sensory examination is most conveniently divided into anterolateral system testing of pain and temperature sense and posterior column testing of vibration and position sense.
The standard method for evaluation of pain perception is to stimulate the skin with a pin and to ask the patient if the stimulus is perceived as sharp. Because the entire body surface cannot be evaluated, the examination must be guided by the nature and location of signs and symptoms, such as numbness or tingling in a specific distribution. Temperature sensation may also be tested by use of a cold metallic object or a small tube of warm water.
To test position sense, the examiner asks the patient to relax and, with the eyes closed, to indicate whether he or she feels the finger (or toe) moving up or down (Fig. 33-26). The Romberg test evaluates the sense of position of the legs and trunk when the visual information is blocked. While the patient stands with feet together and the eyes closed, the examiner looks for the presence of any sway or imbalance. These patients may be relatively steady during testing with eyes open but rapidly lose balance and sway or fall in any direction when visual compensation is eliminated by eye closure. Remember that ability to stand and to maintain balance is the result of vestibular, cerebellar, and peripheral nerve information, and patients with dysfunction of any of these systems may be unable to stand for Romberg testing. Vibration sense is tested with a 128-Hz tuning fork usually applied to the bone prominences of the terminal phalanges of the thumbs and great toes (Fig. 33-27). The patient is instructed to close the eyes and to indicate whether a “buzzing” sensation is experienced. Vibration changes may be seen in peripheral nerve disease and spinal cord problems. Selective loss of proprioception and vibration sense may localize the dysfunction to the posterior columns, as seen in patients with vitamin B12 deficiency or with syphilitic tabes dorsalis.
Figure 33-27. Test of vibratory sense. The tuning fork may be placed on the fingertip, tips of the toes, or bone prominences.
Cortical sensory function can be evaluated only if there is no loss of primary sensation. Testing is performed with use of familiar objects, such as a quarter, a wooden cube, or a plastic pen placed in the patient’s hand while the patient’s eyes are closed (Fig. 33-28). The patient is then asked to identify the objects. Stereognosis is the perception of the form and nature of an object. Two-point discrimination testing is also valuable; with the use of two pointed objects, the stimuli are applied at the same time, and the patient is asked whether one or two points are detected. Agnosia is a “percept stripped of its meaning.” Stereoagnosia is an inability to identify objects by touch (tactile agnosia) or by sight (visual agnosia), sounds or words (auditory agnosia), colors (color agnosia), or the location or position of an extremity (position agnosia). This type of deficit results from lesions in the cerebral hemisphere.
Sources and Additional Reading
Adams AC. Neurology in Primary Care. Philadelphia: FA Davis; 2000.
Aminoff MJ, Greenberg DA, Simon RP. Clinical Neurology. ed 3 Stamford, Ct: Appleton & Lange; 1996.
Caplan LR. Caplan’s Stroke: A Clinical Approach. ed 3 Boston: Butterworth Heinemann; 2000.
Donaghy M. Neurology. New York: Oxford University Press; 1997.
Haerer AF. DeJong’s The Neurologic Examination. ed 5 Philadelphia: JB Lippincott; 1992.
Hankey GJ, Wardlaw JM. Clinical Neurology. New York: Demos Medical Publishing; 2002.
Martin TJ, Corbett JJ. Neuro-Ophthalmology: The Requisites in Ophthalmology. St. Louis: Mosby; 2000.
Pryse-Phillips W. Companion to Clinical Neurology. ed 2 New York: Oxford University Press; 2003.
Rowland LP. Merritt’s Neurology. ed 10 Philadelphia: Lippincott Williams & Wilkins; 2000.
Victor M, Ropper AH. Adams and Victor’s Principles of Neurology. ed 7 New York: McGraw-Hill; 2001.