Chapter 31 The nervous system
How an Electrical Impulse is Generated
As previously discussed (see Chapter 19 ‘Pharmacodynamics: how drugs elicit a physiological effect’, p. 139), proteins span the cell membrane and can affect the rate of flow or direction of ions. These proteins are of two main types:
Both play in important role in conduction of a nerve impulse and muscle contraction.
Production of an Action Potential
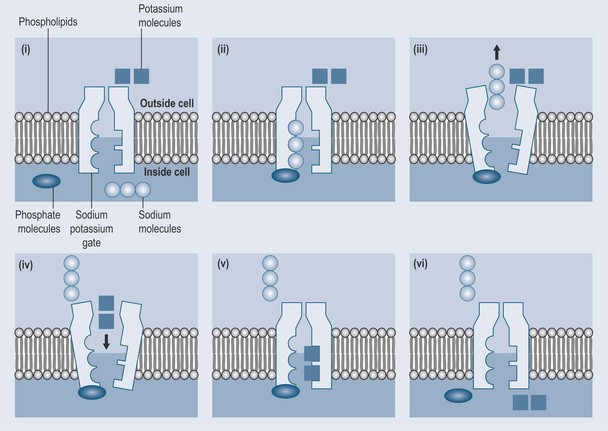
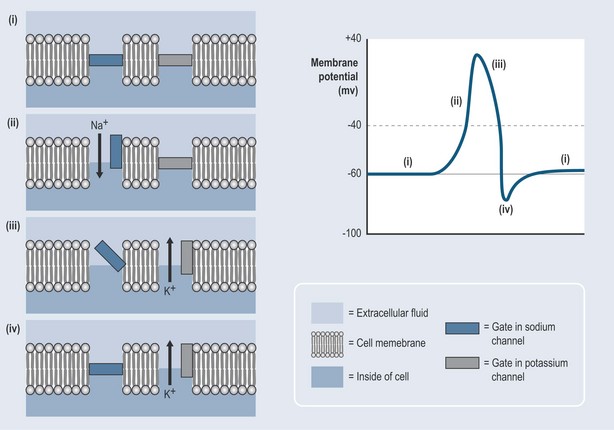
The sodium–potassium pump (Figure 31.1) is a form of active transport as both the sodium and potassium are moving against a gradient. It is responsible for maintaining an electrical balance across a cell membrane. The sodium–potassium pump actively pushes sodium molecules out of the cell and pumps potassium molecules in against a gradient. With each cycle, three Na+ ions are pumped out and two K+ ions are pumped in. The net result, as there are also negative ions such as Cl− (chlorine) present both inside and outside the cell, is a net negative charge inside the cell and a positive charge outside the cell. This means that there is a potential difference across the cell membrane, known as the resting potential. To produce an action potential (Figure 31.2):
Muscle Contraction
The actin filaments in the muscle cells are composed of three protein components:
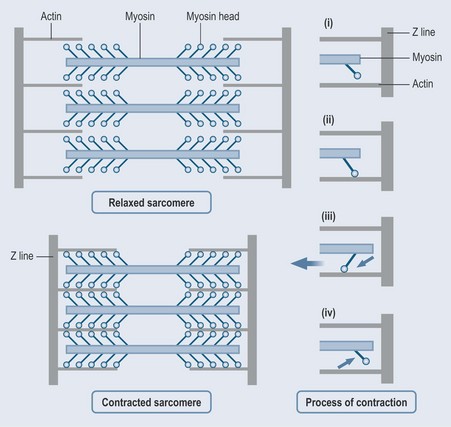
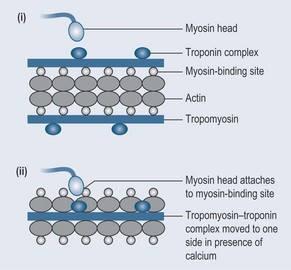
Figure 31.3 illustrates the process of muscle contraction. In (i) and (ii), the released calcium ions interact with the troponin units, making them change shape and allowing the tropomyosin to slide out of its groove to expose the actin myosin-binding sites and allow the cross-bridge components of the myosin to interact with the actin (Figure 31.4). Figure 31.3(iii) shows how this interaction results in the head of the myosin tilting towards the arm and dragging the actin filament with it (the power stroke). At the end of this power stroke (iv) the myosin head is cocked back. Adenosine triphosphate (ATP) is released and binds to the myosin head, releasing it from the actin filament. The myosin head swings back ready to attach again and take another power stroke. In this way, the filaments are walked past one another, or ‘ratcheted’. The cross-bridges are reputed to work independently, each one attaching, pulling along and detaching in a continuous cycle.
As the action potential passes, the calcium ions are pumped back into the sarcoplasmic reticulum and, as the calcium is removed from the muscle fibres, the muscle relaxes. The theory is that, the greater number of cross-bridges that are attached at one time, the greater the force of contraction. All this is very energy dependent; the power source is ATP (see Figure 12.3, p. 91).
The Autonomic Nervous System
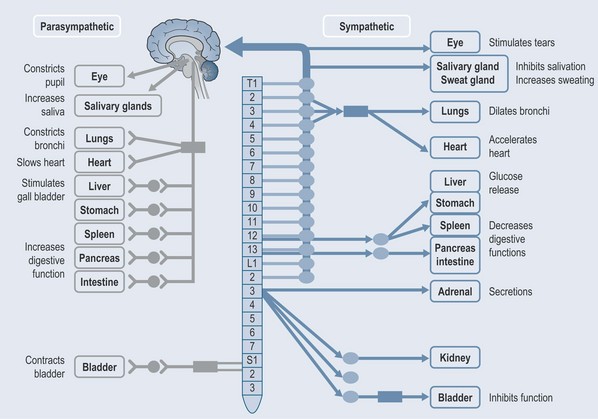
The sympathetic and parasympathetic nervous systems comprise the autonomic nervous system. The physical and chemical arrangement of each differs (Figure 31.5). Both systems use neurotransmitters.
Sympathetic Nervous System
This is arranged in two parts:
The sympathetic nervous system therefore involves two synapses, each with a different transmitter:
Parasympathetic Nervous System
Is also arranged in two parts:
Both synapses in the parasympathetic nervous system use acetylcholine.
Neurotransmitters
Pharmacology in the Central Nervous System
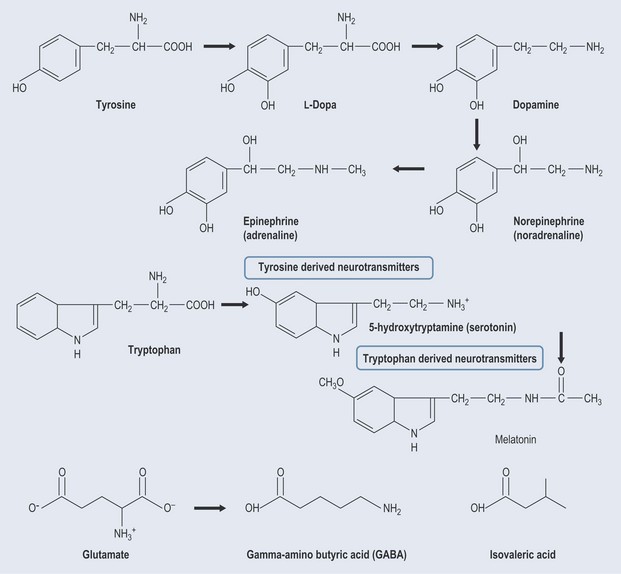
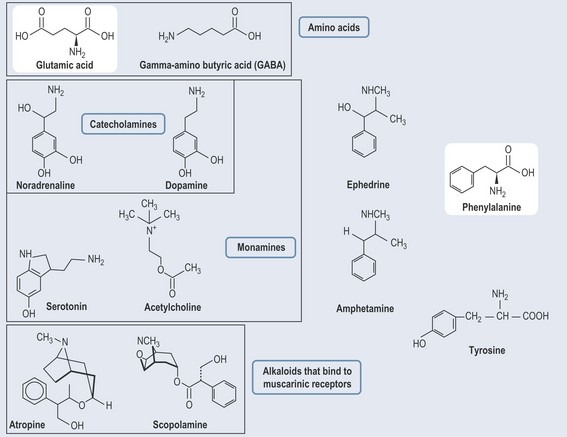
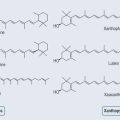
The function of the peripheral nervous system (PNS) is a great deal less compli-cated than that of the brain. The PNS utilizes acetylcholine and noradrenaline (norepinephrine) as its neurotransmitters; the brain has many more neurotransmitters because it is required to manage some very complicated functions, such as emotion. Not only are the transmitters in the central nervous system more diverse, but so are their actions:
Amino Acids
Peptides
Monoamines
• Dopamine
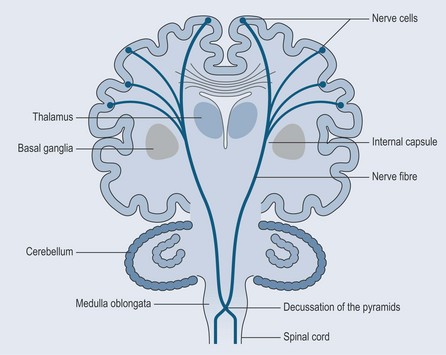
The basal ganglia (Figure 31.8) are a collection of nuclei embedded deep in the white matter of the cerebral cortex. The substantia nigra is a part of the basal ganglia. The ganglia are responsible, with the cerebellum, for organizing movement on a moment-to-moment basis (hence the problems associated with Parkinson’s disease).
• Serotonin (5-hydroxytryptamine (5-HT))
• Histamine
This potent agent is believed to be involved in the regulation of sleeping and waking states.
• Noradrenaline (Norepinephrine) and Adrenaline (Epinephrine)
There are four types of adrenoreceptor, alpha-1, alpha-2, beta-1 and beta-2:
Drugs enhancing adrenergic activity are used in asthma (adrenaline administrated in emergency) and heart failure. Interestingly monoamine oxidase inhibitors (MAOIs) and tricyclic antidepressants (TCAs; see Chapter 33 ‘Neurological disease’, p. 262) are thought to act by increasing synaptic noradrenaline (norepinephrine) in the CNS.
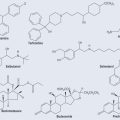
Ephedra spp. (Ma Huang)
Amphetamine (Figure 31.7) works in a similar way, to cause:
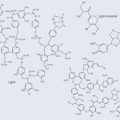
• Acetylcholine (Muscarinic and Nicotinic Receptors)
There are two types of acetylcholine receptor, which are named for the substances that block them: