6 The need for an outcome-based approach
What is outcome-based education (OBE)?
• The learning outcomes expected at the end of training and at the end of each phase of training to be clearly stated, explicit and communicated to all concerned including teachers, students and other stakeholders such as employers in the health service.
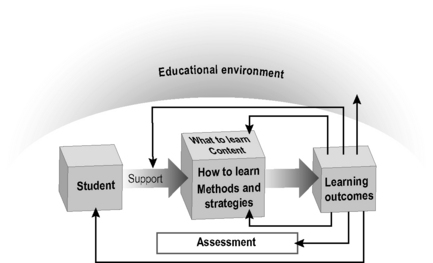
• Decisions about the curriculum, including the content, the educational strategies, the teaching methods and the assessment, to be based on the agreed learning outcomes. The learning outcomes define the process of what is taught, how it is taught and how it is assessed (Fig. 6.1).
• A collectively endorsed vision that reflects a commitment that students will succeed and that their achievement of the exit outcomes will be demonstrated before they leave the programme of training.
Why OBE has been adopted
OBE offers major advantages, some of which are obvious:
• OBE highlights the competencies to be achieved. What matters are the competencies and abilities achieved by doctors, including their knowledge, skills and attitudes, rather than how they were trained or how they acquired these competencies. This has been described as ‘education for capability’. In the analogy of buying a car, the customer is more interested in how the car performs, in its features and petrol consumption and in how easily it can be maintained rather than in the details of the car manufacturing process. As Thomas Fuller noted ‘A good archer is not known by his arrows but by his aim’.
• OBE is necessary given the rapid advances in medicine. Knowledge in the biomedical field is doubling every 18 months. It is no longer feasible, given this information explosion, to cover in the curriculum all aspects of a subject. While the amount of knowledge has greatly increased, the length of the undergraduate curriculum has remained the same at 4, 5 or 6 years’ duration. It is now more important than ever that we agree as teachers and advise our students about the core competencies and knowledge we expect them to master.
• OBE ensures consideration is given to important topics that otherwise might be neglected. Potentially important topics in the curriculum such as attitudes and professionalism, communication skills, health promotion, team working, patient safety and management of errors have in the past been neglected. OBE helps to ensure that careful consideration is given to these and other key topics.
• OBE emphasises accountability and transparency in medical education. To meet demands for greater accountability, quality assurance and transparency are features of medical education today. A clear statement of the learning outcomes achieved is required. An OBE approach to curriculum planning encourages a debate as to the purpose of medical education and what is required of a ‘good doctor’. This may include, in addition to the provision of quality care for individual patients, an element of social responsibility or accountability in medicine and the development of the doctor as a global citizen (Hodges 2009).
• OBE points students in the right direction. OBE provides a robust framework for the curriculum and can be thought of as the glue that holds the curriculum together. It is consistent with a move to a student-centred approach and provides students with a clearer idea of what is expected of them. Traditionally, when students embarked on their medical training it was more like a ‘magical mystery tour’. They lacked an understanding of what was expected of them at the different stages of their education. The provision of a clear set of learning outcomes empowers the students and engages them more actively with the curriculum.
• OBE provides the basis for the allocation of resources to providers. The contribution made by a course or subject to the overall learning outcomes can help to determine the allocation of time and resources to individual courses. In one medical school it was proposed that the duration of the obstetrics and gynaecology clerkship should be reduced significantly, given that competence in the delivery of a baby was no longer an undergraduate requirement. The proposal was quashed when the contributions of the clerkship to the school’s overall learning outcomes were considered. Among other things, the course offered students valuable opportunities at the antenatal classes to understand health promotion and to appreciate clinical audit at the child and mother mortality conferences.
• OBE ensures that the assessment is more valid. OBE has particular significance for student assessment and the approach helps to ensure greater validity of the assessment. OBE is consistent with the move to more performance-based assessment and facilitates an assessment-to-a-standard approach where it is the standards students achieve that are important and not the time they take to achieve them.
• OBE provides continuity across the continuum of medical education. There is a need to have a more seamless continuum between the different phases of undergraduate, postgraduate and continuing medical education. OBE, by making explicit the outcomes for each of the phases or stages of education, provides a vocabulary to discuss the continuum and helps to encourage continuity between the phases.
• OBE flags up problems in the curriculum. Increasing attention has been focused on curriculum evaluation. Learning outcomes provide a yardstick against which a curriculum can be judged. A failure to achieve the agreed outcomes almost certainly identifies a problem with the curriculum.
• OBE helps teachers to select the topics to be taught in a teaching session. Consideration of the expected learning outcomes guides a teacher as to topics to be covered in a teaching session. Although it may be tempting, teachers cannot simply address what is of interest to them. In the seventeenth century, the practice at Glasgow University was for teachers to do just that. They selected a book from their personal or the university’s collection that interested them and read it to students in the lecture hall. The senior university position of ‘reader’ exists even today although the role is very different. The concept of a planned ‘curriculum’ with clarity of the outcomes expected was developed in response to student protests.
• OBE enables curricula worldwide to be compared. It is possible to compare education programmes in different countries using statements of outcomes. The Bologna process is concerned with harmonisation, not necessarily uniformity, in the higher education sector in Europe, and the Tuning Project has as its aim the establishment of a learning outcome framework for primary medical degree qualifications in Europe.
Learning outcomes and instructional objectives
• Level and detail of specification. Instructional objectives were specified in great detail as a bottom-up approach. The book of instructional objectives published by the Southern Illinois Medical School, for example, extended to more than 400 pages. In contrast learning outcomes, as we will see in the next chapter, represent a top-down approach and are specified as broader domains. This approach is more user-friendly and can more easily be adopted by teachers and students in their day-to-day activities.
• Classification. Instructional objectives were classified into knowledge, skills and attitudes categories. This ignores the complexities of medicine and the interaction of all three domains in medical practice. The outcome domains described in Chapter 7 are more holistic and resonate more closely with the work of a doctor.
• Intent. The language of instructional ‘objectives’ suggests aims or aspirations. An outcome-based education requires the teacher to take responsibility for the student achieving the outcomes expected.
• Ownership of outcomes. Instructional objectives were presented as a teacher-centred activity. In contrast, the specification of learning outcomes and their impact on the curriculum involves a partnership of students and teachers and encourages ownership of the process by the different stakeholders.
Potential problems and limitations of OBE
• a lack of research base that demonstrates the effectiveness of implementing an outcome-based education model
• demands imposed on teachers in implementing OBE, in specifying learning outcomes and in relating the outcomes to teaching and learning experiences and the assessment
• limitations placed on learning and the imposition of a rigid model on curriculum developers and teachers – concerns that the teacher will simply become an ‘education technician’
• failure to address adequately in an outcome framework domains such as creativity, with the result that they will be ignored in an outcome-driven curriculum.
Reflect and react
1. Learning outcomes can help you in your role as a medical teacher. Think about which of the reasons described above for implementing an OBE approach are relevant to your own teaching.
2. Are there learning outcomes specified for the course or training programme for which you are responsible? If so, are you familiar with them?
Harden R.M., Crosby J.R., Davis M.H. Outcome-Based Education. AMEE Medical Education Guide No. 14 Part 2 An introduction to outcome-based education. Med. Teach.. 1999;21:7-14.
Harden R.M. Learning outcomes and instructional objectives: is there a difference. Med. Teach.. 2002;24:151-155.
Hodges B.D. Cracks and crevices: globalisation discourse and medical education. Med. Teach.. 2009;31:910-917.
Burke J., editor. Outcomes, Learning and the Curriculum. Implications for NVQs, GNVQs and other qualifications. London: The Falmer Press, 1995.
Carraccio C., Wolfsthal S.D., Englander R., et al. Shifting paradigms: from Flexner to competencies. Acad. Med.. 2002;77:361-367.
This article reviews the literature on competency-based education in medicine.
Morrison G., Goldfarb S., Lanken P.N. Team training of medical students in the 21st century: Would Flexner approve? Acad. Med.. 2010;85:254-259.
Spady W.G. Outcome-Based Education: Critical Issues and Answers. Arlington, Virginia: The American Association of School Administrators; 1994.