The metabolic response to injury
The problems faced by the traumatized individual are listed in Table 55.1. The metabolic response to injury (Fig 55.1) can be thought of as a protective physiological response designed to keep the individual alive until healing processes repair the damage that has been done. It is mediated by a complex series of neuroendocrine and cellular processes, all of which contribute to the overall goal – survival. The metabolic response to injury becomes clinically important only when the degree of injury is severe.
Table 55.1
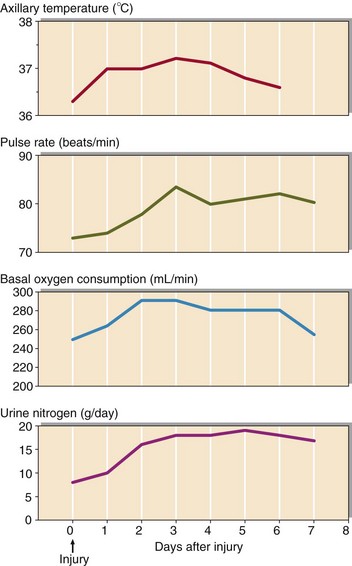
Fig 55.1 The changes in body temperature, pulse rate, oxygen consumption and urinary nitrogen excretion which accompany injury.
The phases of the metabolic response to injury
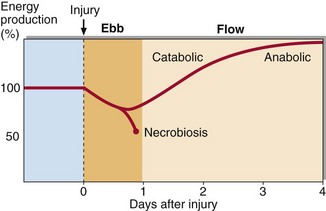
The metabolic response to injury has two phases, the ebb and the flow (Fig 55.2). The ebb phase is usually short and may correspond to clinical shock, resulting from reduced tissue perfusion. The physiological changes that occur here are designed to restore adequate vascular volume and maintain essential tissue perfusion. The severity of the ebb phase determines clinical outcome. If the ebb phase is mild or moderate, patients will have an uncomplicated transition to the flow phase. However, if severe, patients may develop the systemic inflammatory response syndrome (SIRS). The features of this are shown in Table 55.2. This is a complex pathophysiological state involving a vast array of inflammatory mediators and hormonal regulators, but the underlying mechanisms have yet to be clarified. No therapeutic strategies have been found to be helpful, perhaps because of our incomplete understanding of the SIRS. However, a proportion of patients will recover with intensive life support, including ventilation and dialysis.
Table 55.2
A number of biochemical parameters are deranged in this syndrome, because the normal homeostatic mechanisms are overridden by the stress response. A low level of albumin, zinc, iron and selenium are characteristic along with disordered hormonal regulation, e.g low T4, TSH and T3, and nearly all of these patients will develop SIAD (see p. 16).
The flow phase may last for days to weeks depending on the extent of the injury. In this phase, metabolism is altered to ensure that energy is available for dependent tissues at the expense of muscle and fat stores (Table 55.3).
Table 55.3
Biochemical changes in the metabolic response to injury
| Metabolic change | Consequence |
| Increased glycogenolysis | Leads to increased circulating blood glucose to be used as an energy substrate |
| Increased gluconeogenesis | Leads to increased circulating blood glucose to be used as an energy substrate |
| Increased lipolysis | Leads to increased free fatty acids which are used to provide energy and increased glycerol which may be converted to glucose |
| Increased proteolysis | Leads to increased amino acids which may be catabolized to provide energy or used for tissue synthesis and wound healing |
The acute phase protein response
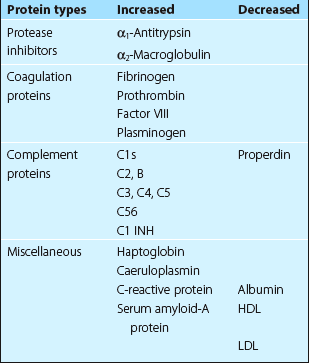
The acute phase protein response leads to greatly increased de novo synthesis (principally by the liver) of a number of plasma proteins along with a decrease in the plasma concentration of some others. This response is stimulated by the release of cytokines such as interleukin 1 and 6 and tumour necrosis factor, and raised concentrations of the hormones cortisol and glucagon. The major human acute phase proteins are listed in Table 55.4.
Clinical uses
 By measuring serum CRP. CRP concentrations change very rapidly and can be used to monitor changes on a daily basis (Fig 55.3).
By measuring serum CRP. CRP concentrations change very rapidly and can be used to monitor changes on a daily basis (Fig 55.3).
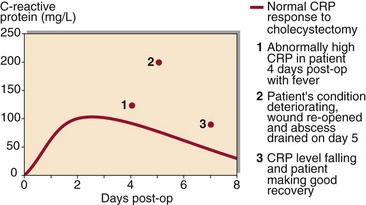
Fig 55.3 CRP concentrations in a patient who developed an occult abscess following abdominal surgery.
 By monitoring the erythrocyte sedimentation rate (ESR). This reflects fibrinogen and immunoglobulin concentration. ESR changes slowly, and is used to monitor the inflammatory process over weeks rather than days.
By monitoring the erythrocyte sedimentation rate (ESR). This reflects fibrinogen and immunoglobulin concentration. ESR changes slowly, and is used to monitor the inflammatory process over weeks rather than days.