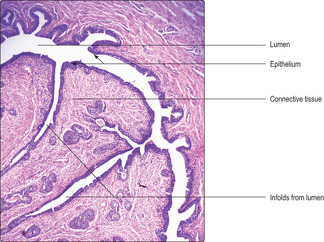
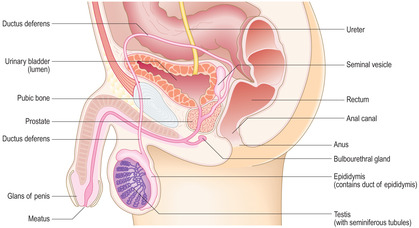
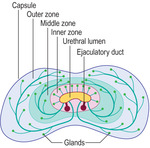
Benign prostatic hypertrophy This condition afflicts 30–40% of men over the age of 50years, and more than 95% of men over the age of 80years. As it is the inner zone of the gland that is affected, any enlargement can readily put pressure on the urethra and affect the ability to pass urine.
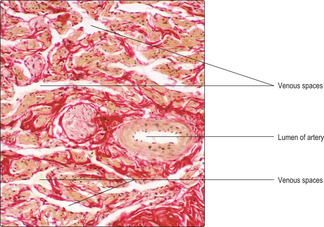
Prostate cancer Cancer of the prostate affects about 30% of males over the age of 75years, and in older men it is almost always present. However, in older men it is usually a very slow growing form of cancer and the individuals usually die from some other disease. In cancer of the prostate, it is usually the outer zone that is affected and, in its most aggressive form, it may spread via the bloodstream before any swelling compresses the urethra and inhibits micturition.
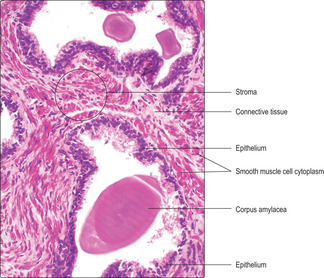
A diagnostic test used to indicate an increased risk of prostatic cancer is a blood test to measure the levels of circulating prostate-specific antigen (PSA). This glycoprotein is secreted by prostatic epithelial cells into the lumina of the glands and normally does not circulate in blood. If prostatic epithelial cells have spread beyond their basement membrane their secretions may circulate in blood. However, PSA may also be raised in patients with benign prostatic hypertrophy, so its usefulness as a diagnostic test is limited.