Chapter 4 The ligaments of the lumbar spine
Topographically, the ligaments of the lumbar spine may be classified into four groups:
1 Those ligaments that interconnect the vertebral bodies.
Ligaments of the vertebral bodies
Anuli fibrosi
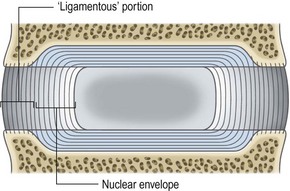
As described in Chapter 2, each anulus fibrosus consists of collagen fibres running from one vertebral body to the next and arranged in concentric lamellae. Furthermore, the deeper lamellae of collagen are continuous with the collagen fibres in the fibrocartilaginous vertebral endplates (see Ch. 2). By surrounding the nucleus pulposus, these inner layers of the anulus fibrosus constitute a capsule or envelope around the nucleus, whereupon it could be inferred that their principal function is to retain the nucleus pulposus (Fig. 4.1).
In contrast, the outer fibres of the anulus fibrosus are attached to the ring apophysis (see Ch. 2). For various reasons it is these fibres that could be inferred to be the principal ‘ligamentous’ portion of the anulus fibrosus. Foremost, like other ligaments they are attached to separate bones, and like other ligaments they consist largely of type I collagen, which is designed to resist tension (see Ch. 2). Such tension arises during rocking or twisting movements of the vertebral bodies. During these movements the peripheral edges of the vertebral bodies undergo more separation than their more central parts, and the tensile stresses applied to the peripheral anulus are greater than those applied to the inner anulus. In resisting these movements the peripheral fibres of the anulus fibrosus are subject to the same demands as conventional ligaments, and function accordingly.
As outlined in Chapter 2 and considered further in Chapter 8, the anulus fibrosus functions as a ligament in resisting distraction, bending, sliding and twisting movements of the intervertebral joint. Thus, the anulus fibrosus is called upon to function as a ligament whenever the lumbar spine moves. It is only during weight-bearing that it functions in concert with the nucleus pulposus.
Anterior longitudinal ligament
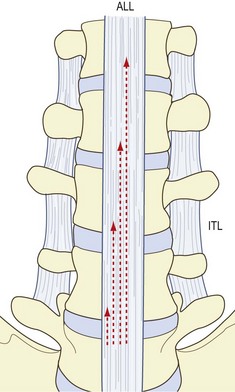
Conventional descriptions maintain that the anterior longitudinal ligament is a long band which covers the anterior aspects of the lumbar vertebral bodies and intervertebral discs (Fig. 4.2).1 Although well developed in the lumbar region, this ligament is not restricted to that region. Inferiorly it extends into the sacrum, and superiorly it continues into the thoracic and cervical regions to cover the anterior surface of the entire vertebral column.
Structurally, the anterior longitudinal ligament is said to consist of several sets of collagen fibres.1 There are short fibres that span each interbody joint, covering the intervertebral disc and attaching to the margins of the vertebral bodies (Figs. 4.2, 4.3). These fibres are inserted into the bone of the anterior surface of the vertebral bodies or into the overlying periosteum.2,3 Some early authors interpreted these fibres as being part of the anulus fibrosus,4 and there is a tendency in some contemporary circles to interpret these fibres as constituting a ‘disc capsule’. However, embryologically, their attachments are always associated with cortical bone, as are ligaments in general, whereas the anulus fibrosus proper is attached to the vertebral endplate.2 Even those fibres of the adult anulus that attach to bone do so by being secondarily incorporated into the ring apophysis (Ch. 2), which is not cortical bone. Because of these developmental differences, the deep, short fibres of the anterior longitudinal ligament should not be considered to be part of the anulus fibrosus.
Because of its strictly longitudinal disposition, the anterior longitudinal ligament serves principally to resist vertical separation of the anterior ends of the vertebral bodies. In doing so, it functions during extension movements of the intervertebral joints and resists anterior bowing of the lumbar spine (see Ch. 5).
Posterior longitudinal ligament
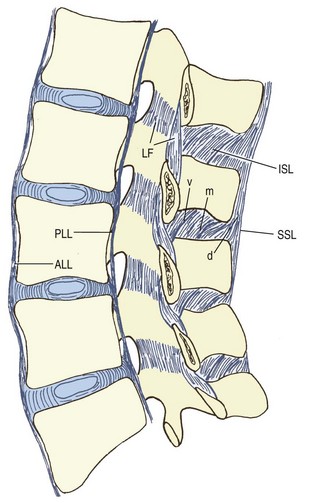
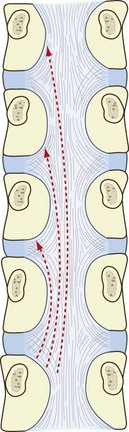
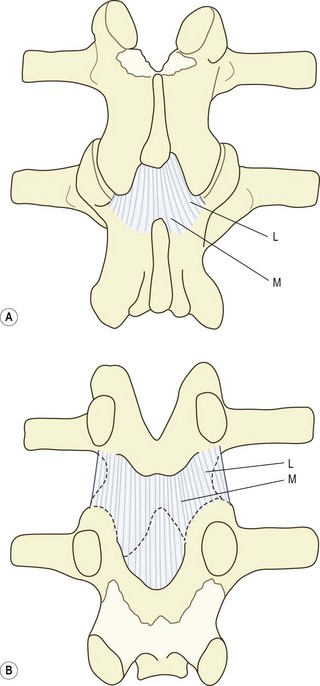
Like the anterior longitudinal ligament, the posterior longitudinal ligament is represented throughout the vertebral column. In the lumbar region, it forms a narrow band over the backs of the vertebral bodies but expands laterally over the backs of the intervertebral discs to give it a serrated, or saw-toothed, appearance (Fig. 4.4). Its fibres mesh with those of the anuli fibrosi but penetrate through the anuli to attach to the posterior margins of the vertebral bodies.3 The deepest and shortest fibres of the posterior longitudinal ligament span two intervertebral discs. Starting at the superior margin of one vertebra, they attach to the inferior margin of the vertebra two levels above, describing a curve concave laterally as they do so. Longer, more superficial fibres span three, four and even five vertebrae (see Figs 4.3 and 4.4).
Ligaments of the posterior elements
The named ligaments of the posterior elements are the ligamentum flavum, the interspinous ligaments, and the supraspinous ligaments. In some respects, the capsules of the zygapophysial joints act like ligaments to prevent certain movements, and in a functional sense they can be considered to be one of the ligaments of the posterior elements. Indeed, their biomechanical role in this regard is quite substantial (see Ch. 8). However, their identity as capsules of the zygapophysial joints is so clear that they have been described formally in that context.
Ligamentum flavum
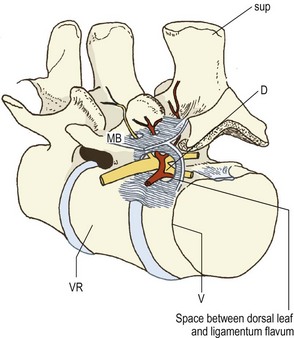
The ligamentum flavum is a short but thick ligament that joins the laminae of consecutive vertebrae. At each intersegmental level, the ligamentum flavum is a paired structure, being represented symmetrically on both left and right sides. On each side, the upper attachment of the ligament is to the lower half of the anterior surface of the lamina and the inferior aspect of the pedicle (Figs. 4.3, 4.5). Its smooth surface blends perfectly with the smooth surface of the upper half of the lamina. Traced inferiorly, on each side the ligament divides into a medial and lateral portion.5–7 The medial portion passes to the back of the next lower lamina and attaches to the rough area located on the upper quarter or so of the dorsal surface of that lamina (see Fig. 4.5). The lateral portion passes in front of the zygapophysial joint formed by the two vertebrae that the ligament connects. It attaches to the anterior aspects of the inferior and superior articular processes of that joint, and forms its anterior capsule. The most lateral fibres extend along the root of the superior articular process as far as the next lower pedicle to which they are attached.7
Histologically, the ligamentum flavum consists of 80% elastin and 20% collagen.7,8 Elastic fibres proper are found throughout the ligament but at its terminal ends the ligament contains modified fibres consisting of elastin and microtubules, and known as elaunin.8
As an elastic ligament, the ligamentum flavum differs from all the other ligaments of the lumbar spine. This difference has prompted speculation as to its implied unique function. Its elastic nature has been said to aid in restoring the flexed lumbar spine to its extended position, while its lateral division is said to serve to prevent the anterior capsule of the zygapophysial joint being nipped within the joint cavity during movement. While all of these suggestions are consistent with the elastic nature of the ligament, the importance of these functions for the mechanics of the lumbar spine is unknown. It is questionable whether the ligamentum flavum contributes significantly to producing extension,9 and no disabilities have been reported in patients in whom the ligamentum flavum has been excised, at single or even multiple levels. Biomechanical studies have revealed that the ligamentum flavum serves to pre-stress the intervertebral disc, exerting a disc pressure of about 0.70 kg cm−2,10 but the biological significance of this effect remains obscure.
Interspinous ligaments
The interspinous ligaments connect adjacent spinous processes. The collagen fibres of these ligaments are arranged in a particular manner, with three parts being identified (see Fig. 4.3).11 The ventral part consists of fibres passing posterocranially from the dorsal aspect of the ligamentum flavum to the anterior half of the lower border of the spinous process above. The middle part forms the main component of the ligament, and consists of fibres that run from the anterior half of the upper border of one spinous process to the posterior half of the lower border of the spinous process above. The dorsal part consists of fibres from the posterior half of the upper border of the lower spinous process which pass behind the posterior border of the upper spinous process, to form the supraspinous ligament. Anteriorly, the interspinous ligament is a paired structure, the ligaments on each side being separated by a slit-like midline cavity filled with fat. This cavity is not present more posteriorly.
Histologically, the ligament consists essentially of collagen fibres, but elastic fibres occur with increasing density in the ventral part of the ligament, towards its junction with the ligamentum flavum.8,12
The fibres of the interspinous ligament are poorly disposed to resist separation of the spinous processes; they run almost perpendicularly to the direction of separation of the spinous processes. Indeed, X-ray diffraction studies have indicated a greater dispersal of fibre orientation than that indicated by dissection, with many fibres running roughly parallel to the spinous processes13 instead of between them. Accordingly, contrary to traditional wisdom in this regard, the interspinous ligaments can offer little resistance to forward bending movements of the lumbar spine.13
Supraspinous ligament
The supraspinous ligament lies in the midline. It runs posterior to the posterior edges of the lumbar spinous processes, to which it is attached, and bridges the interspinous spaces (see Fig. 4.3). The ligament is well developed only in the upper lumbar region; its lower limit varies. It terminates at the L3 spinous process in about 22% of individuals, and at L4 in 73%; it bridges the L4–5 interspace in only 5% of individuals, and is regularly lacking at L5–S1.11,14
Upon close inspection, the nature of the supraspinous ligament as a ligament can be questioned. It consists of three parts: a superficial; a middle; and a deep layer.14 The superficial layer is subcutaneous and consists of longitudinally running collagen fibres that span three to four successive spinous processes. It varies considerably in size from a few extremely thin fibrous bundles to a robust band, 5–6 mm wide and 3–4 mm thick, with most individuals exhibiting intermediate forms.14
The middle layer is about 1 mm thick and consists of intertwining tendinous fibres of the dorsal layer of thoracolumbar fascia and the aponeurosis of longissimus thoracis (see Ch. 9).
The deep layer consists of very strong, tendinous fibres derived from the aponeurosis of longissimus thoracis. As these tendons pass to their insertions on the lumbar spinous processes, they are aggregated in a parallel fashion, creating a semblance of a supraspinous ligament, but they are clearly identifiable as tendons. The deepest of these tendons arch ventrally and caudally to reach the upper border of a spinous process, thereby constituting the dorsal part of the interspinous ligament at that level. The deep layer of the supraspinous ligament is reinforced by tendinous fibres of the multifidus muscle (see Ch. 9).
It is therefore evident that the supraspinous ligament consists largely of tendinous fibres derived from the back muscles and so is not truly a ligament. Only the superficial layer lacks any continuity with muscle, and this layer is not present at lower lumbar levels. Lying in the subcutaneous plane, dorsal to the other two layers and therefore displaced from the spinous processes, the superficial layer may be rejected as a true ligament and is more readily interpreted as a very variable condensation of the deep or membranous layer of superficial fascia that anchors the midline skin to the thoracolumbar fascia. It affords little resistance to separation of the spinous processes.13
Iliolumbar ligament
An early description, provided by professional anatomists with an eye for detail, accorded five parts to the ligament (Fig. 4.6).15
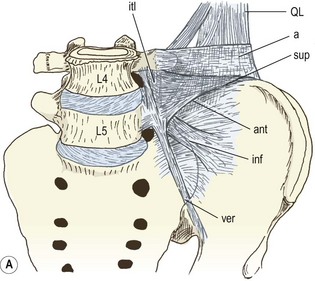
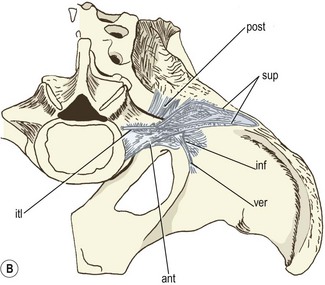
Figure 4.6 The left iliolumbar ligament. (Based on Shellshear and Macintosh 1949.15) (A) Front view. (B) Top view. a, anterior layer of thoracolumbar fascia; ant, anterior iliolumbar ligament; inf, inferior iliolumbar ligament; itl, intertransverse ligament; post, posterior iliolumbar ligament; QL, quadratus lumborum; sup, superior iliolumbar ligament; ver, vertical iliolumbar ligament.
A modern study confirmed the presence of anterior and posterior parts of the iliolumbar ligament, but denied a superior part and did not comment on the inferior and vertical parts.16 These differences can be resolved.
Another study confirmed the incidence and attachments of the anterior, dorsal and inferior bands, but added a further part.17 This was called the sacroiliac part. Its fibres passed between the sacrum and ilium, below the L5 transverse process, and blended superiorly with the lowest fibres of the anterior part.
Notwithstanding the details of its parts, the existence of the iliolumbar ligament has been questioned. One study has found it to be present only in adults. In neonates and children it was represented by a bundle of muscle.18 The interpretation offered was that this muscle is gradually replaced by ligamentous tissue. Replacement starts near the transverse process and spreads towards the ilium. The structure is substantially ligamentous by the third decade, although some muscle fibres persist. From the fifth decade the ligament contains no muscle but exhibits hyaline degeneration. From the sixth decade the ligament exhibits fatty infiltration, hyalinisation, myxoid degeneration and calcification. The identity of the muscles that form the iliolumbar ligament is discussed in Chapter 9.
In contrast, another study unequivocally denied the absence of an iliolumbar ligament in fetuses.19 It found the ligament to be present by 11.5 weeks of gestation. How this difference should be resolved is not clear. What may be critical are data from older fetuses and new data from infants. The embryological study was not able to examine fetuses older than 16.5 weeks, which leaves a gap between that age and infancy. The only reported data in that age range stipulate that the ligament was muscular.18
Regardless of what its structure may or may not be in children and adolescents, in the mature adult the iliolumbar ligament forms a strong bond between the L5 vertebra and the ilium, with different parts subserving different functions. As a whole, the ligament is disposed to prevent forward sliding of the L5 vertebra on the sacrum, and the relevance of this function is explored in Chapter 5. It also resists twisting, and forward, backward and lateral bending of the L5 vertebra.20,21 Forward bending is resisted by the posterior band of the ligament, while lateral bending is resisted by its anterior band.22
False ligaments
Intertransverse ligaments
The so-called intertransverse ligaments (see Fig. 4.2) have a complicated structure that can be interpreted in various ways. They consist of sheets of connective tissue extending from the upper border of one transverse process to the lower border of the transverse process above. Unlike other ligaments, they lack a distinct border medially or laterally, and their collagen fibres are not as densely packed, nor are they as regularly orientated as the fibres of true ligaments. Rather, their appearance is more like that of a membrane.3 The medial and lateral continuations of these membranes suggest that rather than being true ligaments, these structures form part of a complex fascial system that serves to separate or demarcate certain paravertebral compartments. Indeed, the only ‘true’ ligament recognised in this area is the ligament of Bourgery which connects the base of a transverse process to the mamillary process below.3
In the intertransverse spaces, the intertransverse ligaments form a septum that divides the anterior musculature of the lumbar spine from the posterior musculature, and embryologically the ligaments arise from the tissue that separates the epaxial and hypaxial musculature (see Ch. 12). Laterally, the intertransverse ligaments can be interpreted as dividing into two layers: an anterior layer, otherwise known as the anterior layer of thoracolumbar fascia, which covers the front of the quadratus lumborum muscle and a posterior layer which blends with the aponeurosis of the transversus abdominis to form the middle layer of thoracolumbar fascia (see Ch. 9).
Towards the medial end of each intertransverse space, the intertransverse ligament splits into two leaves (Fig. 4.7).23 The dorsal leaf continues medially to attach to the lateral margin of the lamina of the vertebra that lies opposite the intertransverse space. Inferiorly, it blends with the capsule of the adjacent zygapophysial joint. The ventral leaf curves forwards and extends forward over the lateral surface of the vertebral bodies until it eventually blends with the lateral margins of the anterior longitudinal ligament. In covering the lateral aspect of the vertebral column, it forms a membranous sheet that closes the outer end of the intervertebral foramen. This part of the leaf is marked by two perforations which transmit structures into and out of the intervertebral foramen. The superior opening transmits the nerve branches to the psoas muscle. The inferior opening transmits the ventral ramus of the spinal nerve and the spinal branches of the lumbar arteries and veins.
Transforaminal ligaments
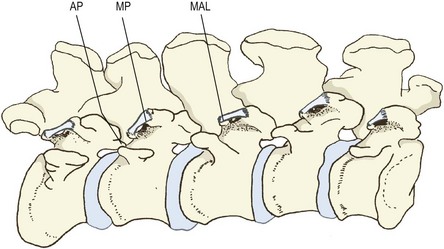
The transforaminal ligaments are narrow bands of collagen fibres that traverse the outer end of the intervertebral foramen. Five types of such bands have been described, according to their specific attachments (Fig. 4.8):24
• The superior corporotransverse ligaments connect the lower posterolateral corner of a vertebral body with the accessory process of the transverse process of the same vertebra.
• The inferior corporotransverse ligaments connect the lower posterolateral corner of a vertebral body with the transverse process below.
• The superior transforaminal ligaments bridge the inferior vertebral notches, and the inferior transforaminal ligaments bridge superior vertebral notches.
• The midtransforaminal ligaments run from the posterolateral corner of an anulus fibrosus to the zygapophysial joint capsule and ligamentum flavum behind.
Figure 4.8 The transforaminal ligaments. (Based on Golub and Silverman 1969.24) (A) Superior and inferior corporotransverse ligaments. (B) Superior transforaminal ligament. (C) Middle transforaminal ligament. (D) Inferior transforaminal ligament.
Transforaminal ligaments are not always present. The overall incidence of all types is around 47%, with the superior corporotransverse being the most common type (27%).24 For two reasons, they are not strictly ligaments. Firstly, their structure resembles bands of fascia more than ligaments proper. Secondly, except for the inferior corporotransverse ligament, they do not connect two separate bones, and the midtransforaminal variety is not connected to any bones. Accordingly, they are more correctly interpreted as bands of fascia, and in view of their location it is most likely that they represent thickenings in the ventral leaf of the intertransverse ligament.
Mamillo-accessory ligament
A tight bundle of collagen fibres of variable thickness bridges the tips of the ipsilateral mamillary and accessory processes of each lumbar vertebra (Fig. 4.9). This structure has been called the mamillo-accessory ligament25 but it is not a true ligament because it connects two points on the same bone. Moreover, its cord-like structure resembles a tendon more than a ligament, and indeed it has been interpreted as representing a tendon of the semispinalis musculature in the lumbar region.25 The ligament may be ossified, converting the mamillo-accessory notch into a bony foramen. The prevalence of this change was found in one study to be 10% at the L5 level,25 while in another study it was 28% at L5, 10% at L4 and 3% at L3.26
The ligament has no biomechanical significance, but its significance lies in the fact that it covers the medial branch of the dorsal ramus of the spinal nerve as it runs through the mamillo-accessory notch. Furthermore, when the ligament is ossified, the foramen it forms can be an apparent anomaly evident on CT scans.27 Ossification of the ligament, however, is a normal phenomenon without any pathological significance. It has been suggested that the ligament may be a site of entrapment of the nerve beneath it,28 but this has not been verified clinically.
1 Williams PL, editor. Gray’s Anatomy, 38th ed, Edinburgh: Churchill Livingstone, 1995.
2 Francois RJ. Ligament insertions into the human lumbar vertebral body. Acta Anat. 1975;91:467-480.
3 Vallois HV. Arthologie. In: Nicolas A, editor. Poirier and Charpy’s Traité d’Anatomie Humaine, Vol 1. Paris: Masson; 1926.
4 Coventry MB, Ghormley RK, Kernohan JW. The intervertebral disc: its microscopic anatomy and pathology. Part I. Anatomy, development and physiology. J Bone Joint Surg. 1945;27:105-112.
5 Naffziger HC, Inman V, Saunders JB, de CM. Lesions of the intervertebral disc and ligamenta flava. Surg Gynecol Obstet. 1938;66:288-299.
6 Ramsey RH. The anatomy of the ligamenta flava. Clin Orthop. 1966;44:129-140.
7 Yong-Hing K, Reilly J, Kirkaldy-Willis WH. The ligamentum flavum. Spine. 1976;1:226-234.
8 Yahia LH, Garzon S, Strykowski H, et al. Ultrastructure of the human interspinous ligament and ligamentum flavum: a preliminary study. Spine. 1990;15:262-268.
9 Twomey LT, Taylor JR. Sagittal movements of the human lumbar vertebral column: a quantitative study of the role of the posterior vertebral elements. Arch Phys Med Rehab. 1983;64:322-325.
10 Nachemson AL, Evans JH. Some mechanical properties of the third human lumbar interlaminar ligament (ligamentum flavum). J Biomech. 1968;1:211-220.
11 Heylings DJA. Supraspinous and interspinous ligaments of the human spine. J Anat. 1978;125:127-131.
12 Yahia LH, Drouin G, Maurais G, et al. Etude de la structure microscopique des ligaments postérieurs du rachis lombaire. Int Orthop. 1989;13:207-216.
13 Hukins DWL, Kirby MC, Sikoryn TA, et al. Comparison of structure, mechanical properties, and functions of lumbar spinal ligaments. Spine. 1990;15:787-795.
14 Rissanen PM. The surgical anatomy and pathology of the supraspinous and interspinous ligaments of the lumbar spine with special reference to ligament ruptures. Acta Orthop Scand. 1960;46(suppl.):1-100.
15 Shellshear JL, Macintosh NWG. The transverse process of the fifth lumbar vertebra. In: Shellshear JL, Macintosh NWG, editors. Surveys of Anatomical Fields. Sydney: Grahame; 1949:21-32. Ch. 3
16 Hanson P, Sonesson B. The anatomy of the iliolumbar ligament. Arch Phys Med Rehab. 1994;75:1245-1246.
17 Pool-Goudzwaard AL, Kleinrensink GJ, Snijders CJ, et al. The sacroiliac part of the iliolumbar ligament. J Anat. 2001;199:457-463.
18 Luk KDK, Ho HC, Leong JCY. The iliolumbar ligament. A study of its anatomy, development and clinical significance. J Bone Joint Surg. 1986;68B:197-200.
19 Uhtoff HK. Prenatal development of the iliolumbar ligament. J Bone Joint Surg. 1993;75B:93-95.
20 Chow DHK, Luk KDK, Leong JCY, et al. Torsional stability of the lumbosacral junction: significance of the iliolumbar ligament. Spine. 1989;14:611-615.
21 Yamamoto I, Panjabi MM, Oxland TR, et al. The role of the iliolumbar ligament in the lumbosacral junction. Spine. 1990;15:1138-1141.
22 Leong JCY, Luk KDK, Chow DHK, et al. The biomechanical functions of the iliolumbar ligament in maintaining stability of the lumbosacral junction. Spine. 1987;12:669-674.
23 Lewin T, Moffet B, Viidik A. The morphology of the lumbar synovial intervertebral joints. Acta Morphol Neerlando-Scand. 1962;4:299-319.
24 Golub BS, Silverman B. Transforaminal ligaments of the lumbar spine. J Bone Joint Surg. 1969;51A:947-956.
25 Bogduk N. The lumbar mamillo-accessory ligament. Its anatomical and neurosurgical significance. Spine. 1981;6:162-167.
26 Ninghsia Medical College. Anatomical observations on lumbar nerve posterior rami. Chin Med J. 1978;4:492-496.
27 Beers GJ, Carter AP, McNary WF. Vertical foramina in the lumbosacral region: CT appearance. Am J Roentgenol. 1984;143:1027-1029.
28 Bradley KC. The anatomy of backache. Aust NZ J Surg. 1974;44:227-232.