TOPIC 8 The labour ward
Fetal well-being: Antenatal investigations
Test: Cardiotocograph (CTG)
How it is done
A cardiotocograph simultaneously records both the fetal heart rate (FHR) and uterine contractions.
Interpretation
Physiological principles
Definitions
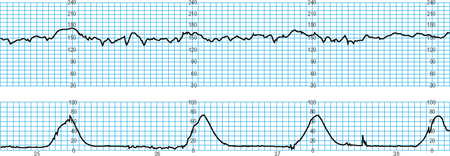
Bradycardia
A baseline heart rate of less than 110 bpm (Fig. 8.2). A profound and sustained decrease in FHR is indicative of fetal distress.
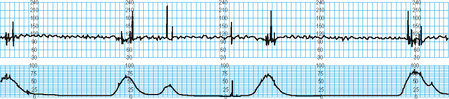
Baseline variability
This is the minor fluctuation in baseline fetal heart rate. It is measured by estimating the difference in beats per minute between the highest peak and lowest trough of fluctuation in a 1-minute segment of the trace. The normal baseline variability is >5 bpm between contractions. Decreased or absent variability (Fig. 8.3) reflects decreased fetal central nervous system activity (associated with fetal sleep cycles or maternal drug administration, e.g. opioid, magnesium, benzodiazepines). However sustained reduction in variability may indicate fetal hypoxaemia/acidosis.
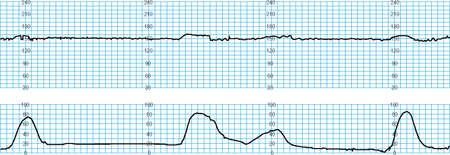
Accelerations
This is defined as a transient increase in heart rate >15 bpm for at least 15 seconds. Accelerations are normal indicating fetal responsiveness. Two accelerations in 20 minutes is considered a reactive trace. The absence of accelerations with an otherwise normal CTG is of uncertain significance.
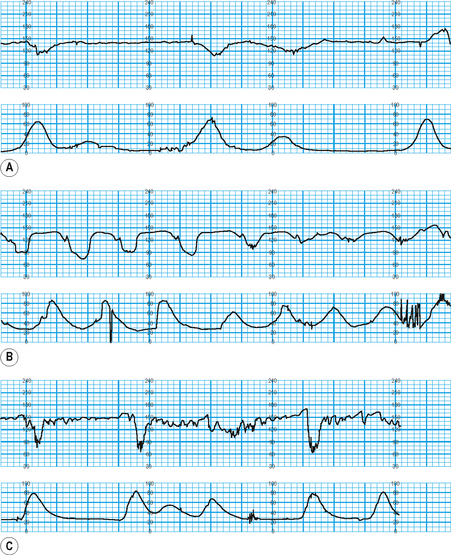
Decelerations
These may either be normal or pathological:
Normal values, abnormalities and management principles
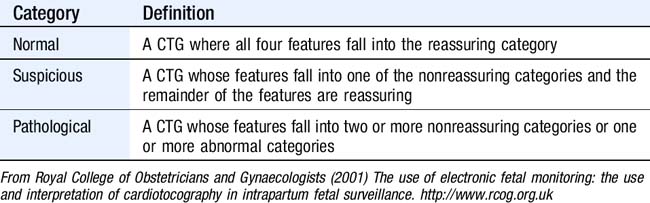
| Category | Definition |
|---|---|
| Normal | A CTG where all four features fall into the reassuring category |
| Suspicious | A CTG whose features fall into one of the nonreassuring categories and the remainder of the features are reassuring |
| Pathological | A CTG whose features fall into two or more nonreassuring categories or one or more abnormal categories |
From Royal College of Obstetricians and Gynaecologists (2001) The use of electronic fetal monitoring: the use and interpretation of cardiotocography in intrapartum fetal surveillance. http://www.rcog.org.uk
Table 8.3 Categorization of fetal heart rate (FHR) features (Table 2.3 RCOG guidelines)
Management principles
Limitations and complications
Test: Fetal scalp blood sampling
Interpretation
Fetal well-being: Postnatal investigations
Test: Cord blood sampling
Indications
How it is done
Management principles
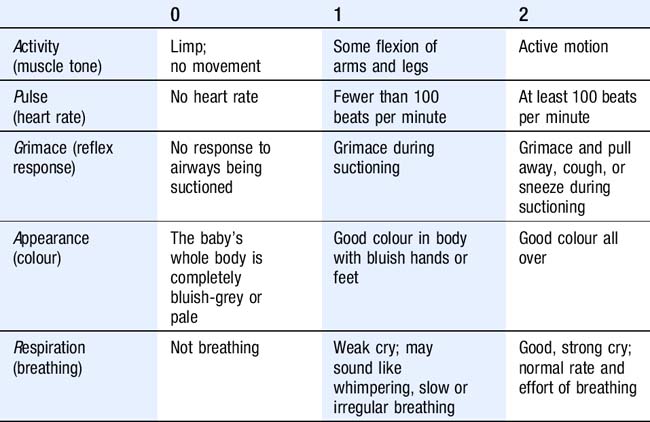
Test: APGAR scoring
How it is done
Abnormalities and management principles
Management principles
Maternal well-being
Test: Antenatal tests in the UK
Test: Blood tests during pregnancy
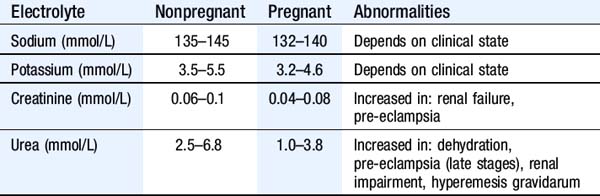
Renal function tests
Interpretation
Table 8.6 shows renal function values in pregnant and non-pregnant women.