6 THE KNEE
Applied Anatomy
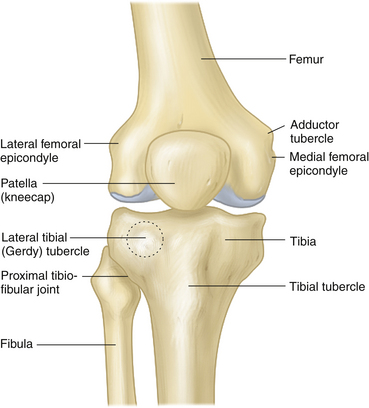
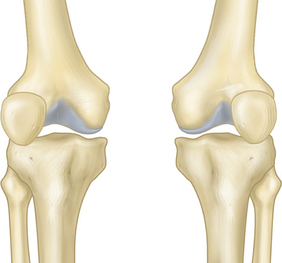
The knee is the largest synovial joint in the body. The knee joint is inherently unstable, because it is not constrained by the shape of its articulating bones. It consists of two tibiofemoral and one patellofemoral compartment. The tibiofemoral articulation is a condylar joint, whereas the patellofemoral articulation is a gliding joint (Figure 6-1). The proximal tibiofibular joint is a plain synovial articulation between the lateral tibial condyle and the fibular head. The tibiofibular joint capsule is much thicker anteriorly and is reinforced by the anterior and posterior tibiofibular ligaments. Slight movements occur at the joint with lower-limb rotation and with activities involving the ankle. The capsules and synovia of the knee and the proximal tibiofibular joints intercommunicate in about 10% of adults.
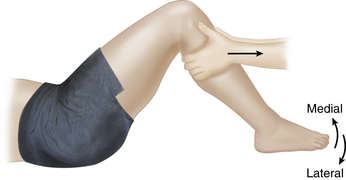
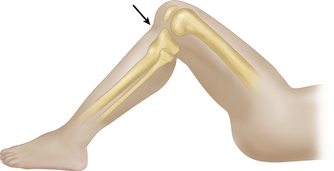
LOWER LIMB ALIGNMENT, PATELLOFEMORAL ARTICULATION, AND PATELLAR TRACKING
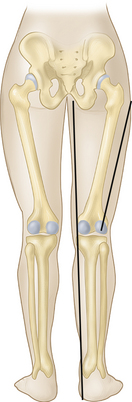
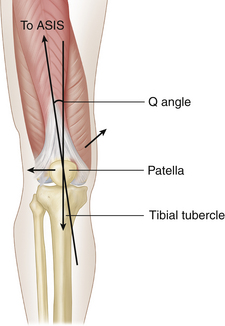
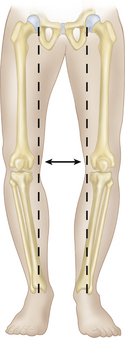
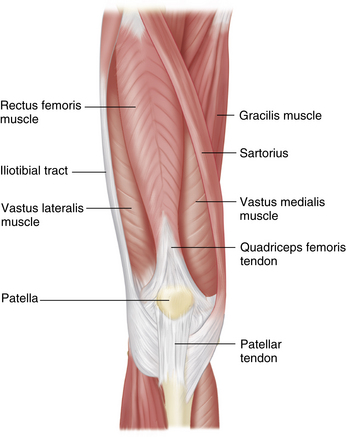
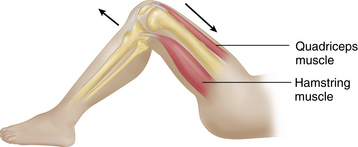
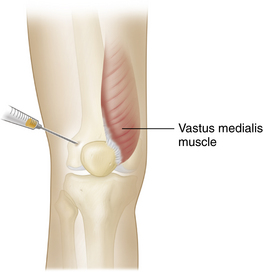
Normally, the center of the femoral head, the center of the knee joint, and the center of the ankle joint are aligned in the coronal plane (Figure 6-2). The adductor muscle mass normally produces the appearance of a relatively straight medial border from top to bottom in the lower extremity (Figure 6-3). Because the femoral neck offsets the femoral shaft away from the hip joint, the femoral shaft must meet the tibia at an angle (see Figure 6-2). This relationship has significant implications for the biomechanical functioning of the patellofemoral articulation. As the force of the quadriceps muscle contraction is transmitted through the tibial tubercle, at an angle to the quadriceps muscle pull, the patella experiences a laterally directed force. This force is resisted dynamically by the vastus medialis muscle (Figure 6-4), which is attached more distally to the patella than the vastus lateralis. The lateral femoral condyle projects more anteriorly than the medial condyle does, and this also helps to counteract lateral dislocation of the patella when the quadriceps contracts (see Figure 6-6A). The angle formed between the quadriceps muscle pull and the tibial shaft, known as the quadriceps angle or Q angle in a supine patient (see Figure 6-4), is normally between 8° and 14° in males and somewhat higher in females, although measurement error may be up to 5°, and there is disagreement regarding the upper limits of normal. The Q angle is measured between a line from the anterior superior iliac spine (ASIS) to the patellar midpoint and a line from the tibial tubercle through the patellar midpoint (see Figure 6-4). Weakness of the vastus medialis or a large Q angle is often associated with patellofemoral symptoms.
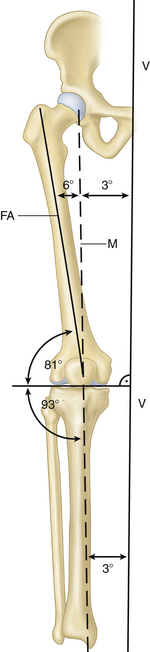
FIGURE 6-2 LOWER-LIMB ALIGNMENT.
(From Gross J, Fetto J, and Rosen E., eds.: Musculoskeletal Examination, 2nd ed. Malden, MA: Blackwell Publishing Company, 2002, page 293.)
When a person is standing erect, the knee is normally locked in extension, and no sustained quadriceps muscle contraction is required. Moreover, in full knee extension, the tibia rotates externally with respect to the femur, the so-called screw-home mechanism (Figure 6-5). Overextension and overrotation of the knee are prevented by the anterior cruciate, collateral, and oblique popliteal ligaments; an unexpected blow to the back of the knee causes the knee to buckle.
The knee is considered to be in the close-packed position during full extension, when the capsule and ligaments are maximally taut and the articular surfaces are compressed and maximally congruent. The open-packed position occurs when the knee is flexed. The three lower-extremity joints—hip, knee, and ankle—can be considered a kinetic chain. Open-chain movements occur when the femur is relatively stable and the tibia moves freely, whereas closed-chain movements involve femoral movement over a fixed tibia. Open- and closed-chain movements can result in different types of sports injuries.
KNEE LIGAMENTS AND SUPPORTING STRUCTURES
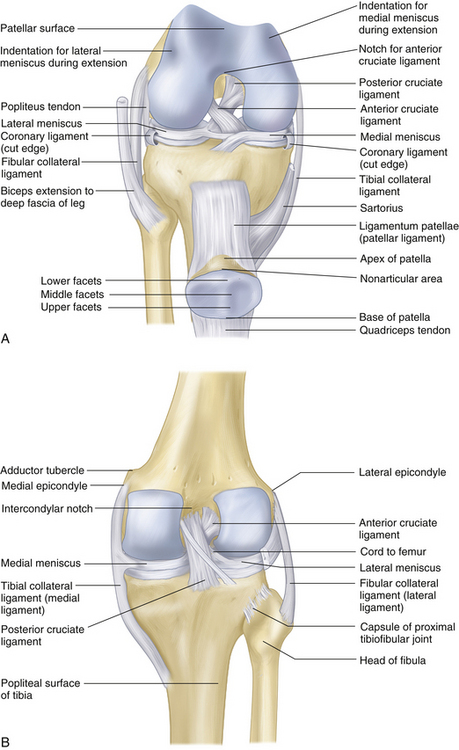
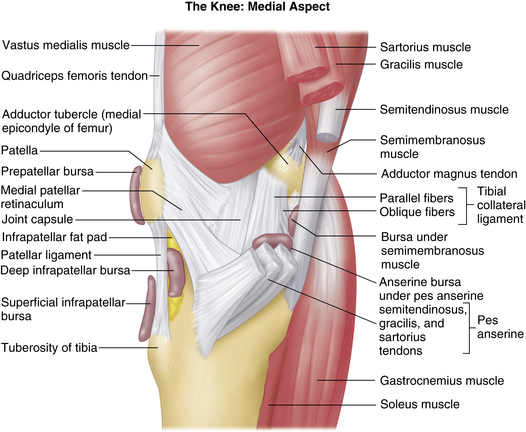
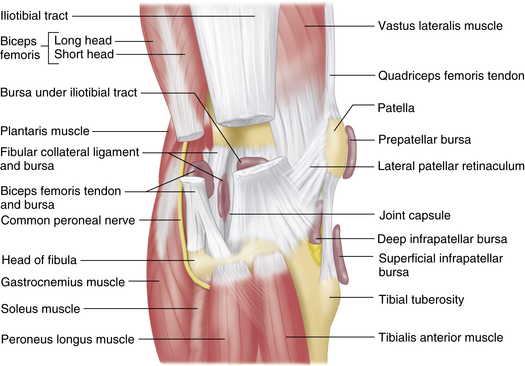
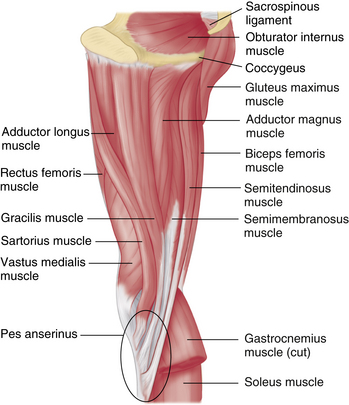
Although the main ligamentous structures about the knee (Figure 6-6) may be injured in isolation, knee-joint injuries often involve multiple ligaments, the joint capsule, and muscle insertions that act as static and dynamic knee-stabilizing structures (see Figure 6-5). In particular, the collateral and cruciate ligaments, posteromedial and posterolateral capsule, posterior oblique ligament, arcuate popliteus muscle complex, pes anserinus tendons, and iliotibial band represent the main static knee stabilizers (Figure 6-7). The hamstrings and quadriceps muscles serve as dynamic knee stabilizers by resisting anterior and posterior translation of the tibia on the femur, respectively. The fused tendons of the rectus femoris and vastis femoris (quadriceps tendon) insert into the upper patella, but some superficial fibers extend distally over the anterior patella to join the ligamentum patellae. Thinner bands from the sides of the patella attach to the anterior border of the tibial condyles to form the medial and lateral patellar retinacula. The gastrocnemius muscles make a more minor contribution to joint stability. The fabella, a sesamoid bone within the tendon of the lateral head of the gastrocnemius muscle, is present in approximately 10% to 20% of normal individuals. The fabella articulates on its anterior aspect with the posterior aspect of the lateral femoral condyle.
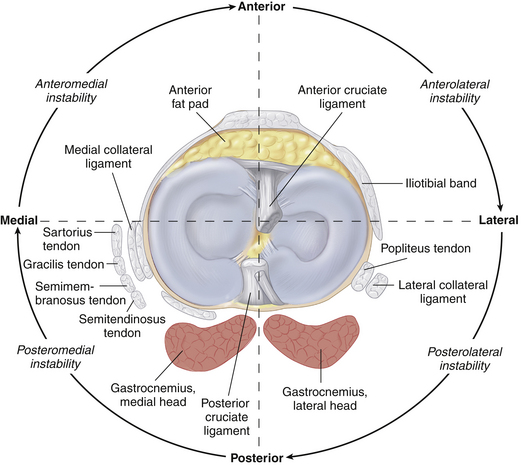
FIGURE 6-7 STABILIZING LIGAMENTS AND MUSCLES OF THE KNEE.
(From Gross J, Fetto J, and Rosen E, eds. Musculoskeletal Examination, 2nd ed. Malden, MA: Blackwell Publishing Company, 2002, page 369.)
Medial Collateral Ligament (MCL)
The medial (tibial) collateral ligament (MCL) consists of a deep and a superficial band. It attaches proximally to the medial femoral epicondyle immediately below the adductor tubercle and inserts distally into the medial tibial condyle (deep band) and into the medial surface of the tibia (superficial band or long band). The long, superficial band attaches to the tibia as a large fascial extension 7 to 10 cm below the joint line, deep to the pes anserinus tendons (Figure 6-8). The deep ligament band has attachments to the peripheral margin of the medial meniscus.
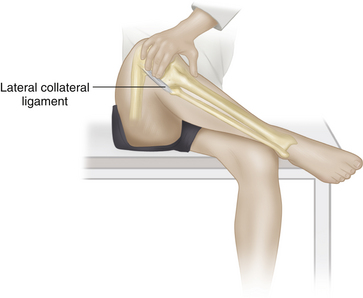
Lateral Collateral Ligament (LCL)
The relatively small-diameter lateral (fibular) collateral ligament extends from the lateral femoral epicondyle proximally to attach onto the fibular head distally (Figure 6-9).
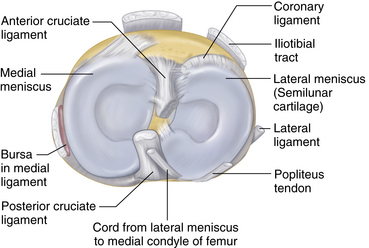
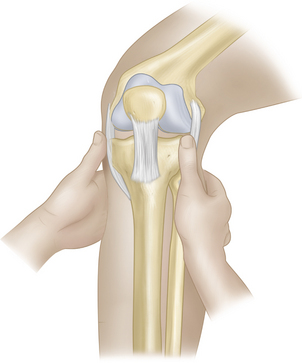
Anterior Cruciate Ligament (ACL)
The anterior and posterior cruciate ligaments, so named for the position of their attachment to the tibia, are situated centrally between the two tibiofemoral articulations (Figure 6-10). The cruciates provide a strong mechanical tie between the femur and the tibia, providing the main resistance to sagittal displacement; they also assist the collateral ligaments in resisting lateral bending of the joint. The anterior cruciate ligament (ACL) provides strong resistance to anterior displacement and excessive internal rotation of the tibia on the femur. The ACL attaches distally on the tibia in a relatively large expanse just in front of and lateral to the tibial spine (intercondylar eminence). It spirals upward and laterally to attach onto the posteromedial corner of the lateral femoral condyle, posterior to the longitudinal axis of the femur. The ACL twists around the posterior cruciate ligament (PCL) with internal rotation of the tibia on the femur, and it may be injured either with excessive anterior translation of the tibia on the femur or with excessive internal tibial rotation. The ACL has been described as consisting of three distinct bundles; although this is a somewhat oversimplified representation of the ligament in vivo, it is nonetheless useful when dealing with partial ACL tears. The anteromedial fibers are taut in flexion, whereas the larger, posterolateral fibers are tight in extension. The intermediate fibers remain relatively taut throughout knee range of motion.
Posterior Cruciate Ligament (PCL)
The tibial attachment of the PCL is extraarticular, extending down the back of the tibial plateau over 1 or 1.5 cm distal to the joint line (see Figure 6-6) and blending with the posterior horn of the lateral meniscus. On the femoral side, the ligament attaches onto the anterolateral aspect of the medial femoral condyle in the intercondylar notch on the opposite side of, and anterior to, the ACL (see Figure 6-10). The anterior fibers of the PCL are taut in flexion, whereas the posterior fibers are taut in extension.
THE MENISCI
The menisci are semilunar structures, with a triangular cross-sectional geometry, that are situated around the periphery of the medial and lateral knee joint compartments (see Figure 6-10). They are composed of fibrocartilage and are attached to the edge of the medial and lateral tibial plateau beneath the femoral condyles. The peripheral border of the medial meniscus is firmly attached to the medial capsule in the deep portion of the MCL, whereas the free surface is invested by synovial membrane. The menisci cover about two thirds of the articular surface of the tibia. The menisci allow controlled rotatory movements during knee flexion and extension, and they attenuate forces during axial loading by increasing the contact surface area between the femur and the tibia (shock absorption). By deepening and improving joint congruity, the menisci also help to stabilize the knee. The menisci may have a role in joint nutrition by helping to distribute synovial fluid evenly to the surrounding articular cartilage of the femoral condyles.
Medial Meniscus
The medial meniscus is C-shaped and has a larger radius than the lateral meniscus. The anterior horn of the medial meniscus is firmly attached to the tibia, just anterior to the ACL attachment. The posterior horn attaches adjacent to the PCL.
KNEE BURSAE
There are several bursae around the knee joint. These usually are not palpable unless they are inflamed (bursitis). The important ones are the following (see Figures 6-8 and 6-9):
Knee Movements
The knee is not a true hinge joint, because the axis of movement is not a fixed one. Instead, the axis shifts forward during extension and backward during flexion. Also, the commencement of flexion and the end of extension are accompanied by rotatory movements. Therefore, movements of the knee from full flexion to full extension consist of three components: 1) a simple rolling movement of the tibia on the femur; 2) a gliding movement of the tibia on the femur superimposed on rolling, in which the axis of movement through the medial and lateral femoral condyle gradually shifts forward during extension (opposite to what occurs during flexion); and 3) a rotatory movement at the end of extension, consisting of external rotation of the tibia on the femur through contraction of the biceps femoris and tensor fascia lata. This rotary movement is referred to as the locking movement of the joint or the screw-home movement. At the commencement of knee flexion, the converse occurs: the tibia internally rotates on the femur through contraction of the popliteus, semitendinosus, sartorius, gracilis, and semimembranosus, thereby “unlocking” the joint.
The screw-home position on full extension contributes significantly to knee stability, particularly when standing erect. It allows the patient to maintain knee extension over prolonged periods of standing without relying on continuous quadriceps contraction; therefore, it is an energy-conserving mechanism. The presence of a knee flexion deformity abrogates this stabilizing mechanism, causing quadriceps muscle fatigue.
Common Knee Disorders and Clinical Evaluation
KNEE PAIN
Heat and Redness
Swelling, heat, and redness are all signs of inflammation in the knee joint or periarticular tissues.
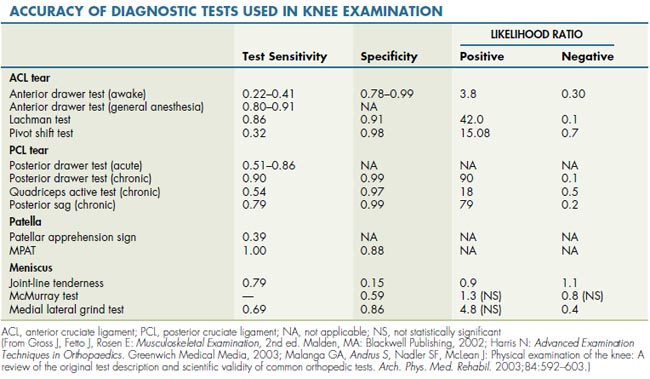
LIGAMENTOUS INJURY
In the acutely injured patient, the Lachman test is particularly useful, because it has both a high positive and a high negative predictive value for ACL injury diagnosis (Table 6-1). The pivot shift test is very useful, if it is positive; but injuries can be missed, especially in the acute situation, when a patient is apprehensive and in muscle spasm. The anterior drawer test is less accurate than the Lachman test. For the diagnosis of PCL injuries, the posterior sag, posterior drawer, and quadriceps active tests are all useful, especially for diagnosis of chronic injuries (see Table 6-1). Isolated ligament ruptures are relatively rare, and combined injuries with capsular tears, tibial plateau fractures, or meniscal injuries are more common.
MENISCUS INJURY
A history of an injury with subsequent locking, clunking, and localized pain to the joint line is a classic for a meniscus tear. The accuracy of physical examination maneuvers in correctly diagnosing meniscus pathology is low according to the published literature (see Table 6-1). Unquestionably, the evaluation of meniscus pathology requires attention to detail and skill that can be acquired only with experience. Careful application of the meniscus tests described earlier, in conjunction with a detailed history, should allow the examiner to limit the use of magnetic resonance imaging (MRI) studies to those cases in which significant uncertainty remains after the clinical evaluation. An acutely injured knee may be exceedingly difficult to examine for a meniscus injury. For example, it is impossible to perform a McMurray test unless the knee can be flexed to at least 90°. A repeat examination 1 or 2 weeks after the acute injury is often very helpful in establishing the correct diagnosis.
CONSIDERATIONS IN PATIENTS AFTER TOTAL KNEE REPLACEMENT
Neurovascular Pain and Dysfunction
The common peroneal nerve is particularly at risk for injury when a preoperative fixed valgus deformity is corrected at the time of knee replacement, resulting in lengthening of the lateral side of the knee and stretching of the peroneal nerve. Complaints of pain and paresthesia should be evaluated with a complete neurological examination. The most obvious motor abnormality with complete loss of common peroneal nerve function is a dense foot drop.
Physical Examination
INSPECTION
The integrity of the extensor mechanism of the knee can be tested by asking the supine patient to raise the leg off the examining table. In the absence of severe pain, inability to raise the heel off the table suggests hip joint pathology or loss of extensor function due to quadriceps weakness, rupture of the quadriceps tendon, fracture of the patella, or rupture of the patellar tendon. An individual with a large knee-joint effusion or a meniscus tear may not be able to fully extend the knee. In the frontal view, the patella should lie in between the two femoral epicondyles and in the same plane as the center of the femoral head and the center of the ankle joint.
Genu Varum and Genu Valgum
Normally, the center of the knee joint lies on a line that connects the center of the hip and the center of the ankle joint (see Figure 6-2). In an individual with genu varum, or bowleg deformity, the center of the knee joint falls lateral to the axis connecting the centers of the hip and ankle joints (Figure 6-11). Although accurate assessment of bony alignment requires radiographic imaging, a patient with more than 3 cm of space between the medial femoral condyles when standing with the feet together probably has genu varum. Conversely, genu valgum, or knock-knee deformity, occurs when the center of the knee joint is medial to the biomechanical axis of the lower extremity (Figure 6-12). Clinically, an individual with more than 3 cm between the medial malleoli likely has genu valgum. Inspection for varus or valgus misalignment is best performed with the knee in a weight-bearing (standing) position.
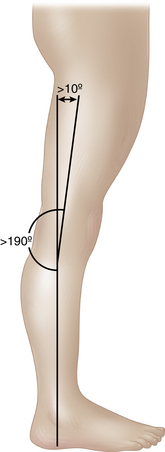
Genu Recurvatum and Genu Procurvatum
When the knee is examined from the side, the patient should be able to fully straighten it. A few degrees of hyperextension can be normal, especially in patients with generalized ligamentous laxity; but more than 10° of hyperextension, or genu recurvatum (“back knees”), generally indicates pathology such as hypermobility syndrome or a cruciate ligament laxity or injury (Figure 6-13). A fixed flexion deformity (genu procurvatum) or the inability to achieve full extension is always pathological and may be caused by arthritis, a large joint effusion, or a mechanical block to extension resulting from a meniscus tear or loose body.
Squinting and Frogeye Patellae
Squinting patellae, patellae that are facing toward each other when the patient walks toward the examiner with feet pointing forward, suggest an internal rotational deformity of the femur or an external rotational deformity of the tibia (Figure 6-14). External femoral rotation or internal tibial rotation gives the appearance of patellae that face away from each other (frogeye patellae; Figure 6-15).
PALPATION AND SPECIFIC MANEUVERS
Is the Knee Joint Inflamed?
The normal knee should be slightly cooler to the touch than the adjacent anterior thigh, which is surrounded by a well-perfused muscle layer. A knee that feels as warm as or warmer than the thigh is likely to be inflamed. Other signs of knee synovitis include redness, swelling, and a joint effusion. Synovitis of the knee is characterized by synovial thickening and diffuse joint-line tenderness, both along the medial and lateral compartments. The synovium is best palpated along the joint line with the knee 90° flexed. Normally, the synovial membrane is quite thin and difficult to palpate. Chronic synovitis, caused by rheumatoid or other inflammatory arthritis, is often associated with significant synovial thickening, with more soft tissue intervening between the palpating thumbs and the joint line (Figure 6-16).
Is There Fluid in the Knee Joint?
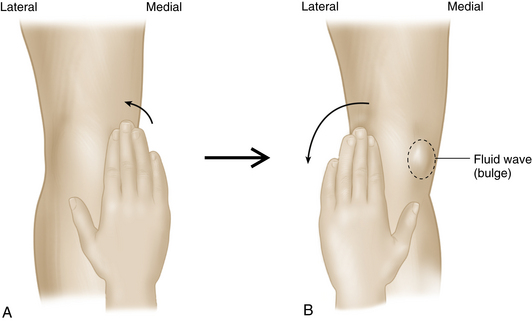
Bulge sign. In the brush, stroke, or wipe test, fluid is pushed up into the suprapatellar pouch by sliding the hand from the distal aspect to the proximal along the medial aspect of the knee joint with the patient in the supine position and the knee relaxed in extension. The fluid is then milked back down by sliding the hand from the superior aspect to the inferior along the lateral aspect of the knee (Figure 6-17). A medial fluid bulge indicates free fluid within the knee joint (bulge sign). The test can be used to demonstrate small to moderate effusions (less than 30 mL), but it may be difficult to detect a bulge with a large or tense effusion, because in this situation, the fluid cannot be milked out of one compartment and into the other.
Balloon test or cross-fluctuance test. The examiner places one hand over the suprapatellar pouch and the thumb and fingers of the other hand on the medial and lateral sides of the joint line, just distal to the margins of the patella. By pressing down with one hand and then the other, the examiner may feel cross-fluctuance of the fluid under the hands (Figure 6-18). The balloon test is particularly useful for patients in whom the patellar tap (Figure 6-19) is difficult to perform due to a large, tense effusion or the presence of a fixed knee-flexion deformity.
Is There Pathology Involving Soft Tissues?
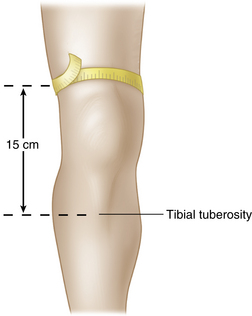
Quadriceps muscle and tendon. Disuse atrophy of the quadriceps muscle, especially the vastus medialis component, is a common finding in patients with knee pathology. The vastus medialis is palpated for its bulk and firmness bilaterally, with the knee in extension, during voluntary contraction of the muscle. Normally, the underlying femur bone cannot be palpated through the vastus medialis muscle without the application of extraordinary pressure. The girth of the quadriceps is measured and compared bilaterally by tape measure at a defined distance (approximately 15 cm above the tibial tubercle) with the knee in extension and the muscle contracted (Figure 6-20). The vastus medialis obliquus (VMO) contributes to both medial stability of the patella and the screw-home movement of the tibia on the femur in the last 10° of extension.
The quadriceps tendon is palpated for tenderness, defects, or swelling along the central tendinous portion and over the insertion into the proximal patellar pole. The medial and lateral patellar insertions of the vastus medialis and vastus lateralis, respectively, in association with the patellar retinacula, should also be palpated if pathology in the extensor mechanism is being considered (Figure 6-21).
Infrapatellar ligament (patellar tendon). Because this structure connects two bones, it is sometimes referred to as the infrapatellar ligament. Others consider the patella to be a large sesamoid bone and therefore refer to the structure as the patellar tendon. The infrapatellar ligament is palpated for tenderness, swelling, or defects along its length, from the inferior pole of the patella to its insertion into the tibial tubercle. The infrapatellar fat pad is situated immediately posterior to the patellar tendon at the level of the joint line. It can be readily palpated by curling the fingers around the tendon from either side (see Figure 6-8).
Pes anserinus. The pes anserinus—the conjoint tendon of the sartorius, gracilis, and semitendinosus muscles—inserts into the medial surface of the proximal tibia about 5 cm below the joint line and at the same level as the tibial tuberosity (see Figure 6-8). It is best palpated during resisted knee flexion of less than 90° (Figure 6-22). The fingers are placed around the medial aspect of the knee, just above the joint line. The two sharp, cordlike structures are the gracilis (more anterior and lateral) and the semitendinosus (more posterior and medial). Between these two structures, the bulky semimembranosus tendon (not part of the pes anserinus) can be palpated. More proximally, the semimembranosus muscle bulk is evident medial to the semitendinosus tendon. The fleshy bulk anterior to the gracilis tendon is the sartorius muscle.
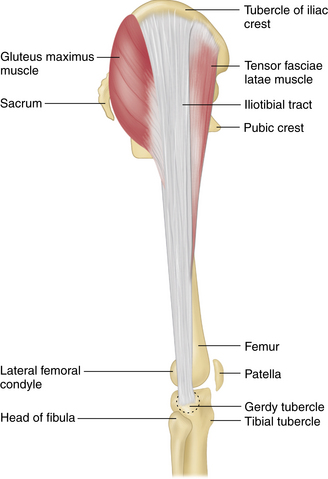
Iliotibial tract. The iliotibial tract is attached proximally to the iliac crest. The tensor fascia lata muscle inserts into it anteriorly, and the bulk of the gluteus maximus muscle inserts into it posteriorly (Figure 6-23). Distally, the iliotibial band attaches to the Gerdy tubercle on the anterolateral aspect of the proximal tibia. A band from the iliotibial tract also attaches to the lateral upper patella (superior patellar retinaculum). It is easy to palpate the iliotibial band distally by moving the fingers from the posterior to anterior aspect, just anterior to the biceps femoris tendon, while the knee is flexed 30° with an ipsilateral single-leg stance or during resisted abduction of the hip (see Figure 6-23).
Is the Iliotibial Band Inflamed?
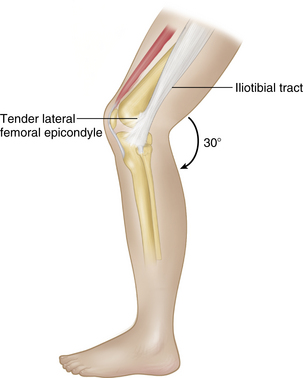
A tight iliotibial band can be associated with iliotibial band syndrome, inflammation of the band as it crosses over the lateral femoral epicondyle. This can be assessed with the Ober test (described in Chapter 5) and by one of the following two tests.
Renne test. The iliotibial band is directly over the lateral femoral epicondyle when the knee is in approximately 30° of flexion. The patient stands with the knee extended, and the examiner’s fingers are placed over the lateral femoral epicondyle. The patient is then asked to slowly flex the knee down into a squatting position (Figure 6-24). Pain at the epicondyle at about 30° of knee flexion is suggestive of iliotibial band friction syndrome.
Semimembranosus. The biceps femoris, the semimembranosus, and the semitendinosus together make up the hamstring muscles. The semimembranosus muscle can be palpated between the gracilis and semitendinosus tendons during resisted knee flexion in the supine or prone position. The bulky part of the muscle is medial to the semitendinosus proximally, but distally the tendon comes to lie deep to the pes anserinus as the tendon inserts more proximally onto the posteromedial tibial plateau (see Figure 6-22). It can be difficult to distinguish between semimembranosus tendinitis and posteromedial joint-line tenderness caused by meniscus pathology.
Knee bursae. A bursa is a potential space with very little fluid that facilitates movement of adjacent soft tissues. It is usually not palpable unless bursitis with fluid distension has developed. Bursae are compressible but may be quite firm to palpation. Chronic bursitis may lead to loculation of the bursa, making it difficult to aspirate. There are at least 14 bursae about the knee joint, but some are more commonly associated with clinical problems. For example, a popliteal cyst (Baker cyst) is readily visible and palpable with the patient standing. It is located between the medial gastrocnemius insertion and the semimembranosus tendon. This cyst typically arises due to chronic knee-joint inflammation with persistent joint fluid that enters into and distends the semimembranosus bursae. The popliteal cyst usually maintains a connection with the knee joint, which is why aspiration usually results in recurrence unless the underlying joint pathology is also addressed. The prepatellar bursa lies between the patella and the overlying skin. The deep infrapatellar bursa, which lies distal to the infrapatellar fat pad, separates the patellar tendon from the proximal tibia. The superficial infrapatellar bursa is situated more superficially, between the patellar tendon and the overlying skin. Medially the pes anserine bursa separates the tendons of the sartorius, gracilis, and semitendinosus from the underlying tibia.
Synovial membrane. The synovial membrane can be palpated for tenderness and synovial swelling (thickening) in a similar fashion. The thumbs of both hands palpate the medial and lateral joint lines, with the fingers placed behind the knee for counterpressure (see Figure 6-16).
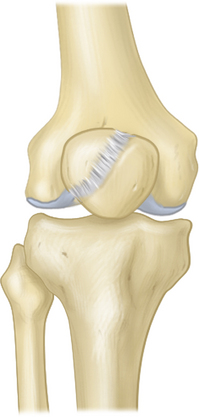
Is There Pathology Involving Bony Structures?
Patellar pathology and tests. The patella is readily palpable in the supine patient. The main body may be tender to palpation with traumatic contusions or fractures. Occasionally there is a bipartite patella, with a groove between the superolateral portion and the main patellar fragment (Figure 6-25). This can be a variant of normal. If it is associated with tenderness to palpation, swelling, or crepitus, a patellar fracture must be ruled out. Unless the patient has ligamentous laxity, the undersurface of the patella is difficult to palpate. The lateral facet can best be palpated for retropatellar tenderness or defects by sliding the patella laterally with the knee relaxed and extended. The medial surface can be palpated if the patella can be flipped up to face the examiner medially. The margins of the trochlear groove of the femur can be palpated with the knee flexed and the patella displaced to either side.
The patella is subject to lateral displacement during flexion and extension because the femur meets the tibia at an angle (see Figure 6-2). Because the quadriceps pulls along the femur, and the patellar tendon is anchored along the proximal tibia, this angle tends to force the patella laterally during active extension with muscle contraction. The vastus medialis resists this lateral translation, and the distal femoral anatomic groove further prevents patellar displacement. Normally the distance between the tibial tubercle and the lower pole of the patella is approximately the same distance as the distance from the lower to the upper pole of the patella (the patellar length). A high riding patella (patella alta) is one in which the length from the tendon to the lower patellar pole is greater than the patellar height, causing the patella to lie above the deep part of the femoral groove. In this position the patella is more prone to lateral displacement. Patella baja denotes a low-lying patella. The Q angle represents the relationship between the quadriceps muscle line of pull through the patella onto the tibial tubercle. As noted previously, a large Q angle has significant implications for patellar stability and may be associated with a patellofemoral syndrome (pain in the anterior aspect of the knee related to the extensor mechanism). The combination of generalized ligamentous laxity, a large Q angle, and a high-riding patella places the individual at high risk for the development of patellofemoral syndrome.
Chondromalacia patellae is a pathological diagnosis of cartilage damage or softening. It may be associated with the clinical entity of patellofemoral syndrome, but the two terms are not synonymous. The line of quadriceps muscle pull is approximated by drawing a line from the anterior superior iliac spine (see Chapter 5) to the center of the patella in a supine patient with the hips and knees fully extended. The angle between this line and a line from the center of the patella to the tibial tubercle constitutes the Q angle (see Figure 6-4).
Patellar Tests
Patellofemoral grinding test (Clarke sign). With the patient supine, the knee extended, and the leg relaxed, the patella is pushed distally in the trochlear groove by the examiner. The patient is then asked to tighten the quadriceps while the examiner palpates, compresses, and resists proximal movement of the patella. Normally, patellar movements are smooth and painless; but in patients with patellofemoral osteoarthritis or patellar contusion, the movements are rough and painful. The maneuver can be very painful, even in normal subjects. The patellar grinding test is neither sensitive nor specific and adds little useful information.
Is There a Pathological Plica Causing Anterior Knee Pain?
Medial femoral condyle and epicondyle. The medial femoral condyle can be palpated in the flexed knee medial to the patellar ligament, from the joint line distally to the proximal extent of the condyle medial to the patella. Full knee flexion is required to palpate the inferior part of the condyle. The proximal part can best be palpated with the knee in extension and the patella displaced laterally. The medial femoral epicondyle is readily palpable a few centimeters above the joint, the most prominent medial bony landmark of the distal femur, where the MCL attaches proximally (see Figure 6-5).
Lateral femoral condyle and epicondyle. The lateral femoral condyle is less prominent than the medial condyle but can be palpated in an analogous manner. The lateral epicondyle is easily identified as the most prominent lateral bony landmark on the distal femur, where the fibular collateral ligament is attached proximally (see Figure 6-5). Either epicondyle may be tender if it is inflamed (epicondylitis). Inflammation of the iliotibial band may cause tenderness in this area, which can be differentiated from epicondylitis using Ober, Renne, and Noble tests as described earlier.
Medial tibial plateau. Beginning from the joint line adjacent to the medial side of the patellar ligament, the fingers are moved medially to palpate the prominent medial tibial plateau (see Figure 6-16). The posterior muscular attachments prevent bony palpation of the posteromedial plateau in most patients. Osteoarthritis may lead to osteophyte formation around the knee joint, which may be readily palpable as enlargements that may or may not be tender.
Lateral tibial plateau. The joint line and plateau are palpated beginning at the lateral margin of the patellar ligament and moving laterally along the lateral tibial plateau (see Figure 6-16). As on the posteromedial side, the posterolateral plateau is difficult to palpate because of the muscular and tendinous structures overlying it.
Lateral tibial (Gerdy) tubercle. The iliotibial tract inserts into the Gerdy tubercle just below the joint line, between the fibular head laterally and the patellar ligament medially (see Figure 6-1). It is quite distinct in some individuals.
Medial and Lateral Collateral Ligament Palpation
When palpating the MCL, it may be difficult to differentiate meniscal tenderness in the medial joint line from MCL tenderness, given the intimate relationship between these two structures (see Figures 6-6 and 6-9). It is important to assess the entire extent of the ligament by slowly moving from the medial femoral epicondyle down to the tibial insertion point. The area of maximal tenderness should be sought. Maximal tenderness over the ligament, away from the joint line, is less likely to be related to meniscus pathology.
The LCL is easily isolated by placing the leg into the figure-four position. The ligament can then be palpated as it runs from the lateral femoral epicondyle to the fibular head. It is situated anterior to the biceps femoris tendon distally (Figure 6-26).
Joint Stability
In most slightly flexed, normal knees, some laxity allows a few degrees of angulation in varus/valgus testing and a few millimeters of glide in the anteroposterior plane. When examining a patient with an acute injury, laxity may be difficult to detect due to muscle spasm. The patient should be made as comfortable as possible to facilitate muscle relaxation, especially of the hamstring and quadriceps muscles.
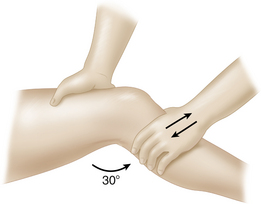
Medial stability. The MCL and the posteromedial capsule provide the major static medial support to the knee joint. At 30° of flexion, the MCL is isolated, whereas the posteromedial capsule and cruciate ligaments contribute to the resistance of valgus force in full-knee extension. The medial joint line is palpated while the leg is supported. With the knee at 30° of flexion, a valgus force is applied by the examiner’s arms (Figure 6-27). Joint opening and the patient’s pain response during valgus stressing of the joint are noted. Repeating the test with the knee in full extension evaluates both the MCL and the posterior capsule. If there is laxity in both flexion and full extension, both structures, and possibly one or more cruciate ligaments, are torn. If there is laxity only at 30° of flexion, the posterior capsule is intact.
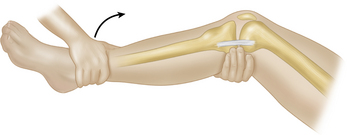
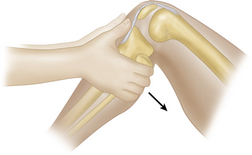
Lachman test. After an acute injury, hamstring spasm will prevent the examiner from appreciating laxity of the ACL with the knee in flexion. Moreover, it may be difficult for the patient to flex the knee due to pain. A Lachman test can be performed supine or prone with the knee in a comfortable position of slight flexion (about 30°). The femur is stabilized with one hand, while the other is used to pull the proximal tibia forward. It is important for the patient to try to relax the hamstring muscles during this test, but it is less critical; the hamstrings are at a mechanical disadvantage, because the examiner’s force is being applied roughly perpendicular to the muscle line of pull (Figure 6-28).
Anterior drawer test. The anterior drawer test is performed with the knee flexed 90° and the hip flexed 45°. The passive anterior drawer test involves placing the examiner’s fingers up the proximal tibia and fibula into the hamstrings, to make sure that these are relaxed. An anterior force is then applied to the proximal tibia, in an attempt to displace it forward on the femur, while the foot is stabilized on the examination table (Figure 6-29). Hamstring spasm can yield a false-negative result. The active anterior drawer test can be performed with the knee in the same position. It involves stabilizing the foot and asking the patient to contract the quadriceps to try to extend the leg against resistance. The quadriceps muscles pull the tibia forward if the ACL is disrupted. The active anterior drawer test is unlikely to yield useful information in an acutely painful injury because of quadriceps inhibition due to pain.
Anteromedial and Anterolateral Rotatory Instability
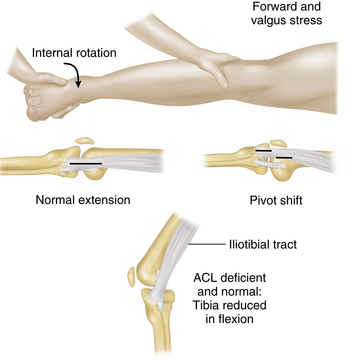
Pivot shift (MacIntosh) test and jerk test of Hughston. The pivot shift test (MacIntosh test) is a test for anterolateral rotatory instability caused by both an anterior cruciate tear and a posterolateral capsular tear. With the knee in full extension, the tibia internally rotated, and a valgus force applied, the tibia and the fibular head will sublux forward on the femur laterally in the presence of a complete ACL tear combined with a posterolateral capsule tear. As the knee joint is flexed beyond 30° to 40°, the iliotibial band comes to lie posterior to the lateral femoral epicondyle, and the tibia is seen to jump backward into position due to traction from the iliotibial band and other secondary restraints pulling the tibia back into place (Figure 6-30). The degree of instability is increased with hip abduction, because it relaxes the iliotibial tract. With severe disruption of the posterolateral corner of the knee joint, the tibia may jam up against the femoral condyle and not reduce until the valgus stress is relaxed, allowing further knee flexion. In the presence of medial joint instability, the pivot shift test cannot be performed, because the essential medial fulcrum is lost. After the tibia is reduced with flexion, the examiner can extend the knee again, while maintaining the valgus and internal rotation force at the knee. The tibia is seen and felt to jerk anteriorly, as it displaces once more at about 30°. This maneuver is sometimes called the jerk test of Hughston. It is less sensitive than the pivot shift test.
Slocum test. ACL disruptions are commonly associated with anterior rotatory instability because of disruption of both the ACL and the posteromedial capsule (anteromedial rotatory instability) or the posterolateral capsule (anterolateral rotatory instability). Testing for posterior capsular injury with the Slocum test involves performing the anterior drawer test with the hip flexed 45° and the knee flexed 90° with the tibia either in external rotation, to tighten the posteromedial capsule, or in internal rotation, to evaluate the integrity of the posterolateral capsule (Figure 6-31). The tibia should be rotated no more than 15° to 20° to avoid excessive tightening of multiple secondary restraints that might lead to a false-negative test. If the capsule is intact, the drawer should be greater in the neutral position than when the capsule is tightened in internal or external rotation. Anterolateral rotatory instability exists if the amount of anterior laxity in internal rotation is similar to that of the anterior drawer test done in the neutral position. Anteromedial rotatory instability exists if the amount of anterior laxity in external rotation is similar to that of the anterior drawer test done in the neutral position (see Figure 6-31).
Posterior Stability
Posterior sag (gravity drawer test) and quadriceps active test. Normally, the tibial plateau is visible and palpable in front of the medial and lateral femoral condyles with the knee in 90° of flexion. With the patient supine, the hip flexed 45°, and the knee flexed 90°, the tibia will sag backward due to gravity if the PCL is incompetent (Figure 6-32). When looking for posterior sag, care should be taken to position the tibia in neutral rotation to avoid involving the secondary restraints of the knee, which could lead to a false-negative test. The examiner can look for a posterior sag of the tibia by lifting the patient’s heel until the hip and knee are in 90° of flexion, taking into consideration the neutral position of the tibia in relation to the femur. A sagging tibia can be lifted forward to the neutral position. Alternatively, the patient may be asked to contract the quadriceps muscle to lift the tibia forward to the neutral position. This maneuver is sometimes referred to as the quadriceps active test (Figure 6-33). Care should be taken to avoid misinterpreting the anterior translation observed as a positive active anterior drawer sign (see the earlier discussion of the anterior drawer sign), which indicates disruption of the ACL. The key is to note whether the tibia begins in a posteriorly displaced position (PCL rupture with posterior sag due to gravity) or in a normal position (normal or ACL rupture) before the anterior translation is noted, and whether it lies in a normal position (PCL rupture reduced by quadriceps) or in an anteriorly displaced position (ACL rupture) when the quadriceps muscle is actively pulling the tibia forward.
Posterior drawer test. The posterior drawer test can be performed actively and passively, as with the anterior drawer test, except that the force is directed posteriorly. Comparison is always made with the normal side. As with the anterior drawer test, the knee is flexed 90° with the tibia in neutral rotation. With the fingers palpating the tibial plateau and femoral condyles anteriorly to assess their relative position, the proximal tibia is pulled forward until the tibia is in the normal relationship to the femur (tibial plateau palpable about 1 cm in front of the femoral condyles). A posteriorly directed force is then applied to the proximal tibia, and the degree of posterior translation is noted. Translation of the tibial plateau to a position posterior to the femoral condyles indicates complete disruption of the PCL (Figure 6-34). In practice, the anterior and posterior drawer tests are usually performed at the same time.
Posteromedial and Posterolateral Rotatory Instability
PCL disruptions are commonly associated with posterior rotatory instability because of concomitant disruption of the posteromedial capsule (posteromedial rotatory instability) or, more commonly, the posterolateral capsule (posterolateral rotatory instability). Although these rotatory tests are analogous to those discussed earlier for anterior rotatory instability, the junior clinician may be confused by the fact that the opposite tibial rotation is required to test the posterolateral (or posteromedial) corner. Consideration of the force to be applied will remind the examiner of the correct rotation for each test: If anterior stability is to be tested, by applying an anteriorly directed force, external rotation of the tibia will slacken the posterolateral structures and tighten up the posteromedial structures. If posterior stability is to be tested, by applying a posteriorly directed force, external tibial rotation will tighten up the posterolateral structures and slacken the posteromedial ones once the force is applied.
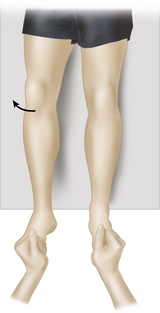
Tibial external rotation (dial) test. Disruption of the posterolateral corner of the knee results in excessive external tibial rotation. With the patient in the prone position, and the knees in 30° of flexion, both feet are passively externally rotated by lifting the great toes (Figure 6-35). More than 10° of excess external rotation indicates the presence of a torn posterolateral knee capsule and surrounding structures. The test should then be repeated with 90° of knee flexion. An isolated posterolateral capsular injury is associated with less side-to-side difference in rotation at 90°, because the intact PCL provides stability in 90° of knee flexion. If the posterolateral capsular injury is associated with a PCL disruption, the test will be equally or more positive with the knee flexed 90°, compared with 30° of flexion. A negative test in 30° of flexion implies that no significant injury is present to the posterolateral corner, and the 90° test is not required.
External rotation recurvatum test. With the patient in the supine position, the legs are lifted off the examining table by the great toes. The amount of external tibial rotation and knee recurvatum are noted. Excessive lateral rotation is indicative of a posterolateral capsular injury. Excessive rotation combined with recurvatum suggests a combined injury to the posterolateral corner of the knee and one or more of the cruciate ligaments. The examiner should be aware that external rotation may give the appearance of genu varum (Figure 6-36).
Medial and Lateral Meniscus Palpation
Palpation along the medial and lateral joint lines is performed with the patient in the supine or sitting position with the knee flexed 90° and the muscles relaxed. Palpation proceeds from the patellar ligament anteriorly to the biceps femoris tendon laterally and the semitendinosus medially. The posterior horn of the meniscus is easier to palpate with the patient prone. The posterior horn of the lateral meniscus is palpated posteromedial to the biceps femoris tendon, and the posterior horn of the medial meniscus can be palpated posterolateral to the semimembranosus tendon.
Meniscal Tests
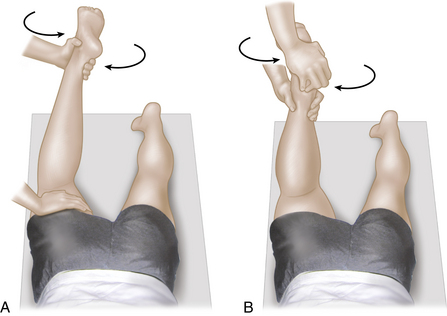
McMurray test. The basic premise of the McMurray test is that meniscus tears are trapped during certain knee movements, with resultant pain and clunking. The test is easy to demonstrate but difficult to describe. It can be properly performed only if the patient has a reasonably full and relatively pain-free range of motion. The knee is flexed to 90°, and an external rotation and varus force are applied to the joint. The applied forces are maintained while the knee is flexed smoothly to a position of maximum flexion, and then the force is smoothly changed from a varus and external rotation force to an internal rotation and valgus force while the knee is extended from the fully flexed position. The process is then reversed and is usually repeated several times in smooth succession, until the examiner is satisfied that the entire range has been thoroughly assessed. It may be helpful to consider that the heel describes a large “U,” with the toes always pointing toward the center of the “U.” During the test, the fingers of the examiner’s free hand are placed along the medial and lateral joint lines to palpate any abnormal snapping or clicking that might be caused by meniscus pathology. A positive test is indicated by pain in association with a clunk, as the torn meniscus fragment is manipulated between the femur and tibia. It is possible to trap a meniscus fragment and cause the knee to lock completely. Although it is generally thought that the medial meniscus is assessed during the valgus and internal rotation position of the tibia, and the lateral meniscus during the opposite phase of the test, this is probably an oversimplification. The area of pain and clunking is more reliable in pointing out the location of pathology in conjunction with other signs and symptoms (Figure 6-37).
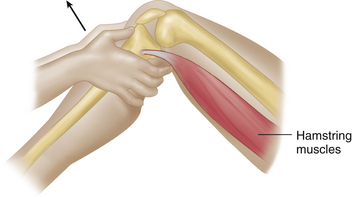
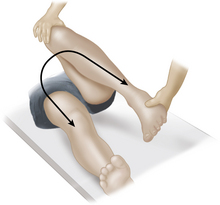
Apley distraction and grinding (compression) tests. Joint-line tenderness can be associated with meniscus or collateral ligament injury. The concept behind the Apley test is that ligaments usually are painful when stressed in distraction, whereas pain involving the meniscus is felt with compression. With the patient in the prone position, the knee flexed 90°, and the femur stabilized with one hand, distraction is applied with the other hand by pulling upward on the ankle while rotating medially and laterally. A varus and valgus force may also be applied to further delineate whether the MCL or the LCL might be the source of pain (Apley distraction test). Once the distraction portion of the test has been completed, compression is applied to alternately grind the medial and lateral meniscus between the tibia and femur, with gentle varus and valgus force applied, while internally and externally rotating and compressing the ankle downward (Apley grinding or compression test; Figure 6-38).
KNEE RANGE OF MOVEMENT
Flexion, Extension, and Rotation
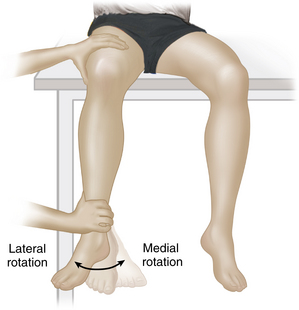
Tibial rotation on the femur is best tested with the patient in the sitting position and the lower leg over the edge of the examining table. The patient is asked to internally rotate the lower leg and then to externally rotate it. Normally, approximately 30° internal rotation and 20° external rotation are possible. Passive manipulation is again used after the limit of active range has been observed (Figure 6-39). Normally, in full extension the tibia externally rotates on the femur into a stable position (the screw-home mechanism).
Knee Aspiration and Joint Injection
ARTHROCENTESIS OF THE KNEE JOINT
As a subcutaneous joint, the knee is relatively easy to aspirate through a medial retropatellar, lateral retropatellar, suprapatellar, or anterior approach. With the knee in extension, fluid accumulates in the suprapatellar pouch, where it can be aspirated. The knee should be placed into a comfortable position of extension before beginning. It is important that the patient be relaxed and not actively contracting the quadriceps muscle. Medially, the bulk of the medial quadriceps should be avoided, because transmuscular needle insertion is painful and can cause excessive bleeding and bruising. For the medial retropatellar approach, the needle is inserted below the vastus medialis bulk, between the medial femoral condyle and the midpoint of the patella. Directing the needle cephalad safely places it into the suprapatellar pouch with minimal risk of injuring the patellar or femoral cartilage. Many clinicians prefer the lateral retropatellar approach, because there is no muscle bulk to contend with: A 21 gauge needle is inserted laterally at the junction of the middle and upper thirds of the patella, midway between the patella and the femoral condyle. If a large effusion is present, the needle is directed medially at 90° to the femur to access the suprapatellar pouch. If there is less fluid, the needle may need to be directed inferiorly and medially to enter the patellofemoral joint before fluid is encountered (Figure 6-40). Care should be taken to minimize trauma to the cartilage of the patella and femoral condyle by advancing the needle gently between the bone surfaces and redirecting it carefully if bone is encountered before fluid can be aspirated.
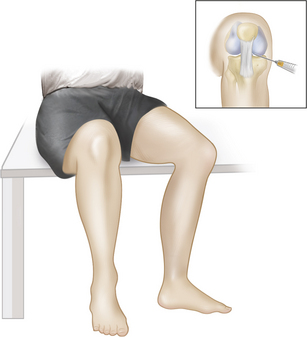
A suprapatellar approach is indicated if there is a very large effusion expanding the suprapatellar pouch. The needle is introduced into the suprapatellar pouch, above and just lateral to the patella. In the anterior approach, direct access to the medial or lateral tibiofemoral joint can be obtained with the patient in a seated position and the knee flexed 90°, preferably with the leg hanging over the end of the examining table to distract the joint by gravity as much as possible. The needle is inserted about one finger’s breadth above the joint line and one finger’s breadth lateral or medial to the patellar ligament. The needle is directed posteriorly and parallel to the line of the tibial plateau toward the midline, aiming for an imaginary point between the inferior aspects of the femoral condyles (Figure 6-41). The anterior approach is particularly indicated for patients with fixed knee-flexion deformity.
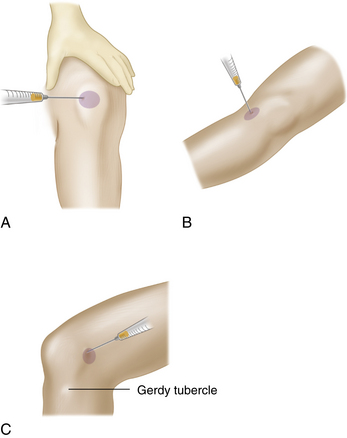
BURSAL ASPIRATION
The prepatellar, deep infrapatellar, and anserine bursae can be aspirated and injected by placing the needle into the area of maximal fluctuance (Figure 6-42). Chronic bursitis can result in bursal loculation, which may preclude complete aspiration of fluid. The prepatellar bursa is injected at the center of maximal fluctuance, usually over the lower part of the patella, with the needle at a 30° angle (see Figure 6-42A). The deep infrapatellar bursa can be entered through a medial or lateral approach deep to the patellar ligament, proximal to its insertion into the tibial tuberosity. The anserine bursa is located over the anteromedial surface of the proximal tibia at the level of the tibial tuberosity. The needle is inserted into the area of maximal tenderness and fluctuance (see Figure 6-42B). A swollen popliteal bursa (cyst) is almost always caused by knee effusion with a communicating, fluid-distended medial gastrocnemius-semimembranosus bursa. Appropriate management consists of joint aspiration and treatment of the underlying knee pathology; direct aspiration or injection of a popliteal cyst is not recommended.
Ahmad C.S., McCarthy M., Gomez J.A., Stein B.E.S. The moving patellar apprehension test for lateral patellar instability. Am. J. Sports Med. 2009;37:791-796.
Barton T.M., Torg J.S., Das M. Posterior cruciate ligament insufficiency: A review of the literature. Sports Med. 1984;16:419-430.
Gross J., Fetto J., Rosen E. Musculoskeletal Examination, second ed. Malden, MA: Blackwell Publishing; 2002.
Harris N. Advanced Examination Techniques in Orthopaedics. Greenwich Medical Media; 2003.
Magee D.J. Orthopedic Physical Assessment, fourth ed. Philadelphia: WB Saunders; 2002.
Malanga G.A., Andrus S., Nadler S.F., McLean J. Physical examination of the knee: A review of the original test description and scientific validity of common orthopedic tests. Arch. Phys. Med. Rehabil. 2003;84:592-603.
Scholten R.J., Opstelten W., van der Plas C.G., et al. Accuracy of physical diagnostic tests for assessing ruptures of the anterior cruciate ligament: A meta-analysis. J. Fam. Pract. 2003;52:689-694.
Solomon D.H., Simel D.L., Bates D.W., et al. Does this patient have a torn meniscus or ligament of the knee? Value of the physical examination. J. Am. Med. Assoc. 2001;286:1610-1620.