Chapter 11. The knee
SUMMARY
This chapter presents the anatomy of the knee relating to commonly encountered lesions. The commentary which follows explores the relevant points of history, aiding diagnosis, and the suggested method of objective examination adheres to the principles of selective tension. The lesions, their treatment and management are then discussed.
ANATOMY
Inert structures
The lower end of the femur consists of two large femoral condyles which articulate with, and transfer weight to, corresponding surfaces on the tibial condyles at the tibio-femoral joint. The two femoral condyles are separated posteriorly and inferiorly by the intercondylar notch or fossa. The anterior aspect of the femur bears an articular surface for the patella to form the patellofemoral joint.
The lateral femoral epicondyle gives attachment to the proximal end of the lateral (fibular) collateral ligament. Below this lies a smooth groove which contains the tendon of popliteus in full flexion of the knee. The medial femoral condyle displays a prominent adductor tubercle on the medial supracondylar line and just below this the medial epicondyle gives origin to the medial (tibial)collateral ligament. Posteriorly, the heads of gastrocnemius originate from the femoral condyles.
The tibia has an expanded upper end which overhangs the shaft posteriorly. The upper weight-bearing surface bears two shallow tibial condyles divided by the intercondylar area. Below the posterolateral tibial condyle lies an oval facet for articulation with the head of the fibula at the superior (proximal) tibiofibular joint. Anteriorly lies the prominent tibial tuberosity which gives insertion to the infrapatellar tendon (ligamentum patellae). Gerdy’s tubercle lies anterolaterally and marks the insertion of the iliotibial tract (Kapandji 1987, Burks 1990).
The upper end of the fibula is expanded to form the head, which articulates with the tibia on its superomedial side, at the superior tibiofibular joint. The apex of the head of the fibula gives attachment to the lateral collateral ligament and the biceps femoris tendon. The common peroneal nerve winds round the neck of the fibula.
The patella, the largest sesamoid bone in the body, lies within the quadriceps tendon and articulates with the lower end of the femur at the patellofemoral joint. It is a flat triangular-shaped bone with its base uppermost and apex pointing inferiorly (see Fig. 11.3). It has anterior and posterior surfaces and upper, medial and lateral borders. Its anterior surface shows vertical ridges produced by fibres of the quadriceps which pass over it. This surface is separated from the skin by a synovial-lined potential space, the subcutaneous prepatellar bursa. It contains minimal fluid and is only obvious when inflamed (Pope & Winston-Salem 1996).
Rectus femoris and vastus intermedius insert into the base of the patella, and the roughened posterior aspect of the apex gives attachment to the proximal end of the infrapatellar tendon (ligamentum patellae). A subcutaneous superficial infrapatellar bursa lies between the infrapatellar tendon and the skin; a deep infrapatellar bursa lies deep to the distal portion of the infrapatellar tendon and the underlying tibia and has no communication with the knee joint (LaPrade 1998). It is located by palpation on the lateral side of the infrapatellar tendon in extension, just proximal to the tibial tubercle; a point of access for injection (LaPrade 1998). Several fat pads are interposed between the knee joint capsule and synovial lining. The infrapatellar fat pad of Hoffa lies between the infrapatellar tendon and the knee joint and may be subjected to trauma or impingement (Jacobson et al 1997).
The vastus medialis and lateralis muscles send tendinous insertions to the medial and lateral borders of the patella in the form of quadriceps expansions (or the patella retinacula). The lateral expansion receives a distinct extension from the iliotibial tract and the quadriceps expansions together are responsible for transverse stability of the patella. The medial quadriceps expansion blends with the anterior fibres of the medial collateral ligament (Fig. 11.3).
The posterior articulating surface of the patella is covered with thick articular cartilage which is divided by a vertical ridge into medial and lateral articular facets for articulation with the femur, with an ‘odd’ facet on the medial side.
The knee joint consists of the tibiofemoral, patellofemoral and superior tibiofibular joints. The former two articulations exist within the same capsule but each has a different function:
• Tibiofemoral joint: involved in weight-bearing activities
• Patellofemoral joint: the joint of the extensor mechanism of the knee
The tibiofemoral joint is a synovial hinge joint between the convex condyles of the femur and the slightly concave articular surfaces of the tibia. Mobility is not normally compatible with stability in a joint, but the incongruent joint surfaces of the knee make it a mobile joint, while the shape of the articular surfaces and the interaction of muscles, tendons and strong ligaments all contribute to stability.
Two semilunar cartilages, the menisci, deepen the tibial articulating surface and contribute to the congruency of the joint. The menisci facilitate load transmission, shock absorption, lubrication and stability (Bessette 1992, Bikkina et al 2005). The peripheral rim of each meniscus is attached to deep fibres of the capsule which secure it to the edge of the tibial condyles. These deep capsular fibres are known as the coronary ligaments ( corona, Latin=crown) or meniscotibial ligaments (Fig. 11.1). They are difficult to separate from the adjacent capsule and collateral ligament and attach several millimetres below the articular cartilage (Bikkina et al 2005). They are strong, but lax enough to allow axial rotation to occur at the meniscotibial surface. The lateral coronary ligaments are longer than the medial to allow for the greater excursion of the lateral meniscus (Burks 1990).
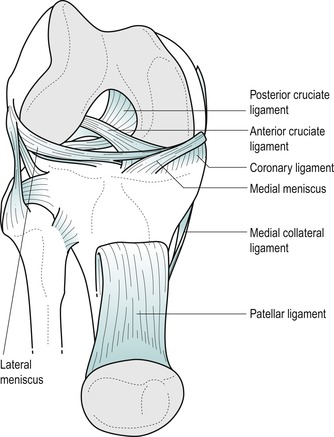 |
| Figure 11.1
Anterior view of the knee with patella reflected showing Coronary (meniscotibial) ligaments.
|
The menisci are composed of collagen fibres. The superficial collagen fibres are oriented radially and the deep fibres are circumferential (Bessette 1992). The orientation of the collagen fibres facilitates dispersion of compressive loads by the circumferential fibres and resistance to longitudinal stresses by the radial fibres; the fibre orientation at the surface of the meniscus is a random meshwork thought to be important for distributing shear stress (Greis et al 2002). Injury usually involves rotational strains and may result in longitudinal or transverse splitting of the fibrocartilage, or separation of the thinner inner part of the meniscus from the thicker outer portion, forming a ‘bucket handle’ lesion.
The medial meniscus is the larger of the two and is almost semicircular in shape. Its periphery has a definite attachment to the deep part of the medial collateral ligament, which forms part of the fibrous capsule of the knee joint. The lateral meniscus is almost circular but it is separated from the capsule of the knee joint at its periphery by the tendon of popliteus, to which it is attached. Posteriorly, the lateral meniscus contributes a ligamentous slip to the posterior cruciate ligament, known as the posterior meniscofemoral ligament.
The fibrous capsule of the knee joint is strongly supplemented by expansions from the tendons that cross it, plus ligamentous thickenings and independent ligamentous reinforcements. The medial collateral ligament, in particular, provides a strong integral reinforcement of the capsule, attaching also to the medial meniscus. The anterior capsule is reinforced by the quadriceps expansions and an extension from the iliotibial band. Independent ligaments such as the lateral collateral ligament and cruciates also have a strong stabilizing effect on the joint.
The cylindrical fibrous capsule is invaginated posteriorly and lined with synovial membrane. The synovium is reflected upwards anteriorly under the quadriceps, approximately three fingers’ breadth, to form the suprapatellar bursa. The articularis genu muscle connects vastus intermedius and the upper part of the suprapatellar bursa, maintaining the bursal cavity during extension of the knee. Plicae (folds of synovium that protrude inwards) exist in the knee joint and may be responsible for symptoms. Three are usually recognized: the superior plica, thought to be an embryological remnant of the division between the suprapatellar bursa and the joint; the inferior plica, located in the intercondylar notch anterior to the anterior cruciate ligament; and a medial plica, a vertical fold, varying from a small ridge to a cord-like structure adjacent to the medial border of the patella (Boles & Martin 2001).
As well as the bursae associated with the patella and patellar tendon as described above, numerous bursae are associated with the knee, facilitating the function of the tendons which are running more or less parallel to the bones, to exert a lengthwise pull across the joint (Palastanga et al 2006). Posteriorly, a bursa sits under each head of origin of gastrocnemius. Laterally, bursae lie either side of the lateral collateral ligament, cushioning it from biceps femoris and popliteus, as well as between popliteus and the lateral femoral condyle. Medially, the pes anserine bursa sits between the distal medial collateral ligament and the tendons of sartorius, gracilis and semitendinosus, known collectively as the pes anserinus. The semimembranosus bursa lies between the tendon of semimembranosus and the medial tibial condyle of the tibia and a variable number of small bursae lie deep to the medial collateral ligament.
The ligaments of the knee provide a dynamic guide during movement and act as a passive restraint to abnormal translations (Barrack & Skinner 1990). Each ligament is oriented in a direction to produce stability, and force is dissipated at the insertion by a gradual transition from ligament, to fibrocartilage, to bone (Woo et al 1990).
The medial collateral ligament is a strong, broad, flat band lying posteriorly over the medial joint line. The posteromedial position of the medial collateral ligament means that its anterior border may be palpated running perpendicular to and approximately halfway along the medial joint line, the ligament itself lying roughly two and a half fingers’ width behind this point. Passing from the medial femoral epicondyle just distal to the adductor tubercle, it descends vertically across the joint line and runs forwards to its attachment on the medial condyle and shaft of the upper tibia approximately 5 cm below the joint line, posterior to the pes anserinus insertion. As the ligament crosses over the knee joint its anterior fibres blend with fibres of the medial patellar retinaculum (El-Dieb et al 2002). It is the primary static stabilizer of the medial aspect of the knee joint and is assisted by the quadriceps expansions and the tendons of sartorius, gracilis and semitendinosus, which cross over its lower part, and from which it is separated by the pes anserine bursa.
The medial collateral ligament is composed of superficial and deep layers. The superficial part of the ligament, often referred to as the tibial collateral ligament, consists of fibres which pass directly from the femur to the tibia (Staron et al 1994, Schweitzer et al 1995). These fibres are relatively strong and provide 80% of the resistance to valgus force (Schenck & Heckman 1993). Under the superficial medial collateral ligament the capsule is thickened to form the deep medial collateral ligament which is firmly anchored to the medial meniscus (Pope & Winston-Salem 1996). This part of the ligament is relatively weaker. The capsule is further thickened by superior fibres, the meniscofemoral ligaments, which attach the meniscus to the femur, and inferior fibres, the meniscotibial ligaments, more commonly known as the coronary ligaments, which attach the meniscus to the tibia (Burks 1990, Staron et al 1994).
The primary stabilizing role of the medial collateral ligament is to support the medial aspect of the knee joint preventing excessive valgus movement. Its secondary stabilizing role is in preventing lateral rotation of the tibia, anterior translation of the tibia on the femur and hyperextension of the knee. Most of the ligament is taut in full extension preventing hyperextension, but it also remains taut throughout flexion (Pope & Winston-Salem 1996). Mechanisms of injury commonly include a rotation stress to the knee and the ligament is often injured together with the anterior cruciate ligament and medial meniscus. Valgus injuries occur through direct impact to the lateral aspect of the knee.
The lateral collateral ligament in isolation is a shorter, cord-like ligament separated from the capsule of the knee joint by the tendon of popliteus. It is approximately 5 cm long and roughly the size of half a pencil (Evans 1986, Palastanga et al 2006). It runs from the lateral femoral epicondyle to the head of the fibula where it blends with the insertion of biceps femoris to form a conjoined tendon which is an important lateral stabilizer.
However, the lateral collateral ligament may be more complex than that. Anatomically it is closely related to the underlying iliotibial band which is similar in width and direction to the medial collateral ligament and may indeed provide dynamic stability to the lateral aspect of the knee joint. Posteriorly the lateral collateral ligament has a relationship with the arcuate popliteal ligament and the popliteus tendon (Pope & Winston-Salem 1996). Its primary stabilizing role is to restrain varus movement, supporting the lateral aspect of the knee (Burks 1990), with a secondary stabilizing role in controlling posterior drawer and lateral rotation of the tibia. Injuries to the lateral collateral ligament complex are not as common as those to the medial aspect, but, if they do occur, they are more disabling and difficult to diagnose. Mechanisms of injury include a varus force applied to the knee in flexion and/or medial rotation, an unusual position for the knee accounting for the relative rarity of this injury (El-Dieb et al 2002).
The cruciate ligaments are strong intracapsular, but extrasynovial, ligaments said to be about as thick as a pencil (Evans 1986, Bowditch 2001). They are called cruciate ( crux, Latin=cross) because of the way they cross in the intercondylar fossa and are named anterior or posterior by their tibial attachments (see Figure 11.1 and Figure 11.2). Their primary stabilizing role is to resist anterior and posterior translation of the tibia under the femur. Their secondary stabilizing function is to act as internal collateral ligaments controlling varus, valgus and rotation (Schenck & Heckman 1993).
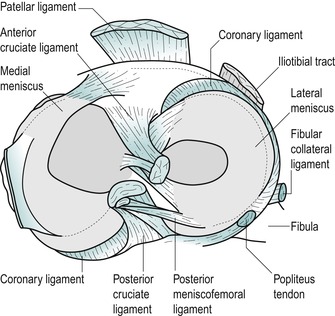 |
| Figure 11.2
Cruciate ligament attachments on the tibial plateau.
|
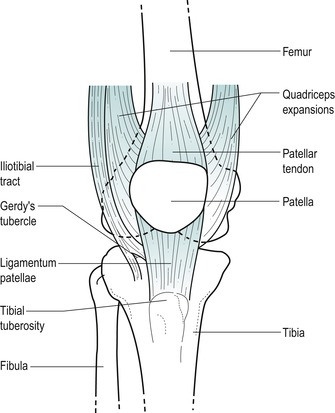 |
| Figure 11.3
Anterior aspect of the knee.
|
The anterior cruciate ligament passes from the anterior tibial intercondylar area upwards, posteriorly and laterally, twisting as it goes, to attach to the posteromedial aspect of the lateral femoral condyle. Anatomically it can be divided into two parts: an anteromedial band which is taut in flexion and a posterolateral band which is taut in extension. Functionally, the ligament has a stabilizing effect throughout the range of movement (Katz & Fingeroth 1986, Perko et al 1992). Its primary stabilizing role resists anterior translation and medial rotation of the tibia on the femur. A secondary stabilizing role relates it to the collateral ligaments in resisting valgus, varus and hyperextension stresses (Evans 1986). A study by Butler et al (1980) showed the anterior cruciate ligament to provide 86% of the total resisting force to anterior translation, with other ligaments and capsular structures making up the remaining secondary restraint (Katz & Fingeroth 1986). The most common mechanism of injury to the anterior cruciate ligament is lateral rotation combined with a valgus force applied to the fixed tibia. Less common mechanisms may include hyperextension, medial rotation in full extension or anterior translation produced by direct injury to the calf. Most tears occur within the ligament itself, with 20% involving either bony attachment (El-Dieb et al 2002). Complete ruptures of the anterior cruciate ligament most commonly result in disruption of all fibres and synovial coverings leading to a haemarth-rosis. With partial tears the synovial envelope may not be disrupted, leading to a contained haematoma without a haemarthrosis (Bowditch 2001).
The posterior cruciate ligament passes upwards, anteriorly and medially from the posterior intercondylar area, to attach to the anterolateral aspect of the medial femoral condyle. The ligament is said to be twice as strong and less oblique than the anterior cruciate ligament and its close relationship to the centre of rotation of the knee joint makes it a principal stabilizer (Palastanga et al 2006). As well as controlling posterior translation of the tibia on the femur, it seems to have a role in producing and restraining rotation of the tibia, since posterior translation occurs with concomitant lateral rotation of the tibia. Injury to the posterior cruciate ligament is not as common as to its anterior partner. Forced posterior translation of the tibia on the flexed knee, the typical ‘dashboard’ injury, is the most common mechanism of injury, but it may also be injured in forced hyperextension (El-Dieb et al 2002).
The main function of the knee joint is weight-bearing; therefore symptoms are usually produced on weight-bearing activities. During the gait cycle, the forces across the tibiofemoral joint amount to two to five times body weight according to position and activity. However, the forces may increase to 24 times body weight during activities such as jumping (Palastanga et al 2006).
The range of movement at the knee joint is greatest in the sagittal plane with an active range from 0° extension to 140° of flexion. Approximately 5–10° of passive extension is usually available and up to 160° of passive flexion, which is halted when the calf and hamstring muscles approximate and the heel reaches the buttock. During flexion and extension, the menisci stay with the tibia so that these movements occur as the femoral condyles roll and slide over the menisci.
Active and passive axial rotation occur with the knee joint in flexion and the range available is greatest at 90° of flexion. Active lateral rotation amounts to approximately 45° and medial rotation of 35°, with a little more movement in each direction available passively. During axial rotation, the menisci now stay with the femur and rotation occurs as the femoral condyles and menisci roll and glide over the tibial condyles. The coronary ligaments are lax enough to permit this movement.
A few degrees of automatic, involuntary rotation occurs to achieve the locked or unlocked positions of the knee. During the last 20° or so of knee extension, lateral rotation of the tibia on the femur occurs to produce the terminal ‘screw-home’ or ‘locking’ phase of the knee. This achieves the close packed position of the knee joint, where it is most stable, and rotation and accessory movements are impossible to perform on the normal extended knee. The knee is unlocked by the action of popliteus medially rotating the tibia on the femur.
The locking mechanism of the knee occurs because the medial femoral condyle is slightly longer than the lateral and the shape of the tibial condyles allows the lateral femoral condyle to glide more freely and over a greater distance than the medial. The ligaments around the knee contribute to stability in extension when most fibres are under tension.
The patellofemoral joint is the joint between the posterior aspect of the patella and the anterior surface of the femur. It is the joint of the extensor mechanism of the knee and therefore gives rise to symptoms on antigravity activities. The patella performs two important biomechanical functions at the knee (Nordin & Frankel 2001):
• It produces anterior displacement of the quadriceps tendon throughout movement, assisting knee extension by increasing the lever arm of the quadriceps muscle force.
• It increases the area of contact between the patellar tendon and the femur, distributing compressive forces over a wider area.
The articular cartilage on the back of the patella is said to be the thickest in the body, at 5–6 mm thick (Evans 1986). It is divided into areas for articulation with the medial and lateral femoral condyles in varying degrees of flexion and extension. The patella glides caudally approximately 7 cm and rotates as the knee moves from full extension to full flexion. The patella eventually sinks into the intercondylar groove in full knee flexion (Nordin & Frankel 2001).
Patellofemoral symptoms may arise from instability, maltracking, malalignment, biomechanical causes, subluxation and dislocation, which may lead to eventual chondromalacia patellae and osteoarthrosis of the joint. There is a tendency for the patella to slip laterally, particularly as the knee moves towards full extension, and this is counteracted by:
• The high lateral border of the patellar groove on the femur
• The active muscle pull of the oblique fibres of vastus medialis
• The medial quadriceps expansion.
The superior tibiofibular joint is a synovial plane joint between the lateral tibial condyle and the head of the fibula; it communicates with the knee joint in 10% of adults (Bozkurt et al 2003). The joint capsule is reinforced by anterior and posterior tibiofibular ligaments. Small accessory movements are possible at this joint which is mechanically linked to the inferior tibiofibular joint and dissipates torsional stress applied to the ankle. It is therefore influenced by movements at the ankle joint (Bozkurt et al 2003).
Contractile structures
The contractile structures at the knee consist of muscles which originate from the hip region and insert at the knee, or originate at the knee and insert below the ankle. The muscles will be described in relationship to the knee and the reader is referred to the chapters on the hip and ankle for further discussion of the muscle groups.
Quadriceps femoris (femoral nerve L2–L4) is composed of four muscles: rectus femoris, vastus lateralis, vastus medialis and vastus intermedius, uniting around the patella to form the infrapatellar tendon, which passes from the apex of the patella to insert into the tibial tuberosity.
Rectus femoris originates above the hip joint and inserts into the base of the patella (upper border) with fibres continued over and on each side of the patella contributing to the infrapatellar tendon.
Vastus lateralis passes down from the upper anterolateral femur to form a broad tendon which eventually tapers as it inserts into the lateral border of the patella as the lateral quadriceps expansion. Vastus lateralis contributes to the main quadriceps tendon, passing over the patella, as well as blending with fibres of the iliotibial tract to form a lateral extension and to support the anterolateral joint capsule.
Vastus medialis passes from the upper anteromedial femur downwards, to join the common quadriceps tendon and the medial border of the patella as the medial quadriceps expansion. The medial quadriceps expansion is a strong sheet of fibres on the anteromedial aspect of the knee with fibres continuing to run inferiorly and posteriorly to insert onto the tibia beside the fibres of the medial collateral ligament (Greenhill 1967). The lower fibres of the muscle, which continue to form the medial expansion, run more horizontally and have their origin from adductor magnus, with which they share a nerve supply. These fibres are commonly known as the vastus medialis obliquus (VMO). The VMO traditionally has a role in the ‘screwing home’ of the tibia in the final locking stage of knee extension (Greenhill 1967).
Vastus intermedius is the deepest part of the quadriceps and inserts with rectus femoris into the base of the patella as the suprapatellar tendon.
Quadriceps femoris is the main extensor muscle of the knee joint. Vastus medialis is believed to be particularly active during the later stages of knee extension, when it exerts a stabilizing force on the patella to prevent it slipping laterally. Although quiet in standing, the quadriceps femoris muscle contracts strongly in such activities as climbing.
The hamstrings (sciatic nerve L5, S1–S2), comprising biceps femoris, semimembranosus and semitendinosus, are responsible for flexion of the knee and medial and lateral rotation of the knee when flexed in the mid-position.
Biceps femoris inserts into the head of the fibula, splitting around the lateral collateral ligament as it does so, with which it forms a conjoined tendon. Semimembranosus has its main attachment into the posterior aspect of the medial tibial condyle, but sends slips on to blend with other structures to support the posteromedial capsule. Semitendinosus curves around the medial tibial condyle to the upper surface of the medial tibia together with sartorius and gracilis to form the pes anserine tendon complex. These tendons blend with the medial capsule, lending it some support. The pes anserine tendon complex is responsible for flexion of the knee and medial rotation of the tibia on the femur (Valley & Shermer 2000).
The iliotibial tract inserts into Gerdy’s tubercle on the anterolateral aspect of the upper tibia and blends with the lateral capsule and the lateral quadriceps expansion; functionally it is related to the lateral collateral ligament. Tensor fascia lata, acting with gluteus maximus, tightens the tract and assists extension of the knee.
Popliteus (tibial nerve L4–L5, S1) originates within the capsule of the knee joint as a tendon arising from the groove on the lateral aspect of the lateral femoral condyle. It separates the lateral collateral ligament from the fibrous capsule of the knee joint and, as it passes downwards, backwards and medially, it sends tendinous fibres to the posterior horn of the lateral meniscus. It forms a fleshy, triangular muscle belly and attaches to the posterior aspect of the tibia above the soleal line. Popliteus is the primary medial rotator of the knee, medially rotating the tibia on the femur and unlocking the knee joint from the close packed position. Some consider that, through its attachment to the lateral meniscus, it pulls the meniscus backwards during rotatory movements, possibly preventing it from being trapped (Safran & Fu 1995). Its complex attachment to the lateral meniscus, arcuate ligament, posterior capsule and lateral femoral condyle provides an appreciable role in dynamic stability, particularly in preventing forwards displacement of the femur on the tibia (Burks 1990, Safran & Fu 1995, El-Dieb et al 2002).
Gastrocnemius (tibial nerve S1–S2) arises by two heads from the posterior aspect of the medial and lateral femoral condyles and together with soleus and plantaris forms the triceps surae. As well as its action at the ankle, gastrocnemius is a strong flexor at the knee, but is unable to act strongly at both joints simultaneously.
A GUIDE TO SURFACE MARKING AND PALPATION
Anterior aspect (Fig. 11.3)
Locate the patella at the front of the knee and identify its base (upper border), apex (lower border), medial and lateral borders. With the knee extended and relaxed you should be able to shift the patella from side to side to palpate the insertion of the quadriceps expansions under the edge of each border. Tilt the base and apex to locate the suprapatellar and infrapatellar tendons respectively.
Follow the infrapatellar tendon down to its insertion onto the tibial tuberosity, which lies approximately 5 cm below the apex of the patella in the flexed knee.
Palpate and mark in the knee joint line with the knee in flexion. The anterior articular surface of each femoral condyle and the anterior articular margins of the tibia should be palpable at either side of the patella. Both can be followed round onto the medial and lateral aspects, but it is not possible to palpate the joint line posteriorly since it is covered by many musculotendinous structures.
With the knee joint flexed, the apex of the patella marks the approximate position of the joint line. In extension, the apex of the patella lies approximately one finger’s breadth above the joint line. This information may provide a useful guide if the joint is very swollen, making it difficult to palpate the joint line.
The quadriceps muscle forms the major anterior muscle bulk. On static contraction of this muscle, locate rectus femoris, which forms the central part of the muscle bulk. Vastus lateralis forms an obvious lateral muscle bulk, while vastus medialis terminates in oblique fibres which form part of the medial quadriceps expansion.
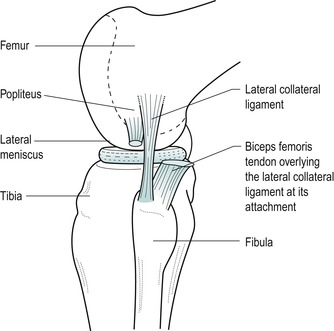
Lateral aspect (Fig. 11.4)
On the anterolateral surface of the tibia, approximately two-thirds of the way forward from the head of the fibula to the tibial tuberosity, palpate for Gerdy’s tubercle, which gives attachment to the iliotibial tract. The tract should be obvious as the quadriceps contracts.
 |
| Figure 11.4
Lateral aspect of the knee.
|
Palpate the head of the fibula just below the posterior part of the lateral condyle of the tibia where it forms the proximal tibiofibular joint. The common peroneal nerve can be rolled over the neck of the fibula.
Place the leg into the FABER position of flexion, abduction and external (lateral) rotation, and palpate the lateral aspect of the knee joint line. You should be able to roll the cord-like lateral collateral ligament under your fingers.
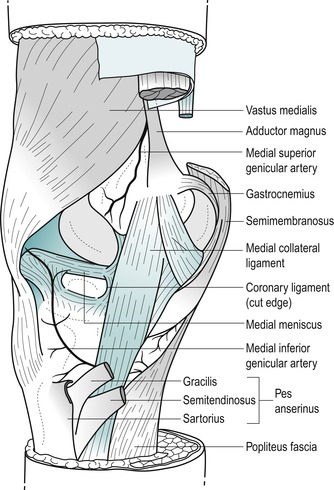
Medial aspect (Fig. 11.5)
Palpate the medial condyle of the femur and locate the prominent adductor tubercle on the upper part of the condyle. Deep palpation is necessary and the tubercle will feel tender to palpation.
 |
| Figure 11.5
Medial aspect of the knee.
|
Move directly distally from the adductor tubercle until you are over the joint line and see if you can identify, by palpation, the anterior edge of the medial collateral ligament. This ligament is approximately 8–10 cm long (Palastanga et al 2006) and two and a half fingers wide as it broadens to cross the joint line. Its anterior border may be palpated in most people and is usually in line with or just behind the central axis of the joint.
Visualize the position of the sartorius, gracilis and semitendinosus tendons (the pes anserine complex) as they cross the lower part of the medial collateral ligament to their insertion on the upper part of the medial tibia.
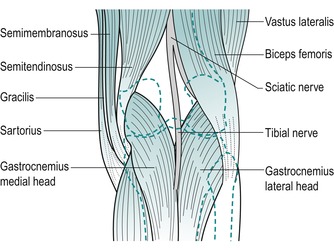
Posterior aspect (Fig. 11.6)
Resist knee flexion and palpate the hamstrings, which form the muscle bulk of the posterior thigh. The point at which the medial and lateral hamstrings separate can be identified, with biceps femoris forming the lateral wall of the popliteal fossa and semitendinosus lying on semimembranosus forming the medial wall.
 |
| Figure 11.6
Posterior aspect of the knee.
|
Biceps femoris can be followed down to its insertion onto the head of the fibula.
On the medial side of the popliteal fossa, semitendinosus can be felt as an obvious tendon. Medial to it is gracilis, made more prominent by adding resisted medial rotation. Deeper to this is semimembranosus, remaining more muscular as it blends into its aponeurotic attachment.
Posteriorly, locate the two heads of gastrocnemius as they originate above the knee joint from the medial and lateral femoral condyles.
COMMENTARY ON THE EXAMINATION
Observation
A general observation is made of the patient’s face and overall posture, but as the knee is a weight-bearing joint, particular attention is paid to the gait pattern. Note if an antalgic posture or gait has been adopted; a limp will be evident during gait if the patient has an abnormal stride length or is not weight-bearing evenly. Toeing in or out, together with abnormalities of foot posture, should also be noted.
History (subjective examination)
A detailed history is required at the knee since it gives important diagnostic clues, including typical injury patterns, which may be confirmed by clinical examination. It also assists in the identification of lesions which may be better suited for specialist referral.
The age, occupation, sports, hobbies and lifestyle of the patient are particularly relevant.
Some conditions affect certain age groups. Knee pain in children is commonly referred from the hip and it is necessary to carry out a thorough examination of both joints. Meniscal lesions are unusual in children and increase in incidence from adolescence onwards. A gradual onset of knee pain in adolescents may be related to patellofemoral joint syndromes or Osgood–Schlatter’s disease which presents as a localized pain felt over the tibial tuberosity due to traction apophysitis of the tibial tubercle.
The young adult, particularly male, may present with traumatic meniscal lesions associated with rotational injury during sporting activities (Greis et al 2002). Females tend to present with instability, subluxation or episodes of dislocation of the patella.
Rheumatoid arthritis may affect the knee and onset usually occurs between the ages of 30 and 40. Degenerative osteoarthrosis affects the older age group, but may occur earlier if predisposed by previous injury or through overuse in sporting activity. It is important to remember that osteoarthrosis can affect both the patellofemoral and tibiofemoral joints. Degenerative meniscal lesions occur more commonly in males in the fourth to sixth decades and can develop in association with degenerative joint disease (Greis et al 2002).
The lifestyle of the patient will reflect whether occupational or recreational activities are a contributing factor to their condition. Sport in particular may be responsible for traumatic incidents to the relatively unstable knee, especially in positions of flexion. Progressive microtrauma may be the result of incorrect training or overtraining, muscle imbalances or poor joint biomechanics.
The site of the pain indicates whether it is local or referred. Superficial structures tend to give local pain and point tenderness; therefore lesions of the medial collateral ligament, coronary ligaments or the tendinous insertions of the muscles around the knee give reasonably accurate localization of pain. Acutely inflamed lesions or deep lesions, such as of the tibiofemoral joint, menisci or cruciate ligaments, produce a vague, more widely felt, deep pain, with the patient unable to localize the lesion accurately.
The spread of pain generally indicates the severity of the lesion. While referred pain is expected distally to the site of the lesion, the knee as a central limb joint may also produce some proximal pain in the thigh. Pain referred from the hip or lumbar spine can be felt at the knee and both may need to be eliminated as a cause of pain.
Anterior knee pain is a description of the symptoms felt by the patient, although the term is often misused as a diagnosis. It usually indicates patellofemoral joint involvement, but must not be considered to be due to it exclusively. Chondromalacia patellae is a softening of articular cartilage that can be explored with magnetic resonance imaging (MRI) to establish the nature of the lesion. A bipartite patella is a normal asymptomatic variant which is often bilateral; it can occasionally become painful due to overuse or acute injury. The most common site for the lesion is the superolateral corner at the insertion of vastus lateralis. Stress fracture of the patella is a rare cause of anterior knee pain.
Several causes of anterior knee pain can be identified with MRI following anterior cruciate ligament reconstruction including contracture of the retropatellar fat pad and patellar tendon, fibrous hyperplasia or scarring in the peripatellar tissues and the so-called ‘Cyclops lesion’, with bone and/or fibrous tissue lying in front of the anterior cruciate ligament graft in the tibial tunnel (Llopis & Padrón 2007).
The anatomy at the knee makes the structures susceptible to direct and indirect trauma. The menisci and ligaments are often the sites of acute lesions, while the contractile structures are susceptible to overuse as well as acute trauma. The superior tibiofibular joint is mechanically linked to its inferior counterpart and influenced by mechanisms of injury at the foot and ankle.
The onset of the pain is extremely relevant to lesions at the knee. Trauma is a common precipitating cause and the sudden nature of the injury makes it easily recalled by the patient. A direct injury can cause muscular contusion and commonly involves the quadriceps. A direct blow to the patella, such as a fall on the flexed knee, may result in fracture, or may cause contusion of the periosteum or involvement of the prepatellar bursa. A direct blow to the anterior aspect of the upper tibia or, again, a fall on the flexed knee can injure the posterior cruciate ligament.
In contact sports such as rugby and football, the lateral side of the knee is vulnerable to impact, which may result in excessive valgus strain affecting the medial collateral ligament. Injury may be produced by excessive forces applied to the flexed knee while the foot is fixed, e.g. skiing injuries. The medial collateral ligament, anterior cruciate ligament and medial meniscus may be affected. The position of the coronary ligaments involves them in rotational injuries. Major ligamentous rupture, particularly of the anterior cruciate ligament, is usually accompanied by a ‘pop’ or tearing sound as the patient feels the ligament ‘go’ (Edwards & Villar 1993).
Hyperextension injuries can affect any of the ligaments, since all are taut in extension, but the anterior cruciate ligament and medial collateral ligament are most commonly affected. Recalling the exact onset of the injury, the forces involved and the position of the leg at the time of injury will give an idea of the likely anatomy involved in the lesion.
Muscle injuries are common around the knee, as the major muscle groups span two joints and may affect the origin, insertion or mid-belly. Strain results from eccentric contraction (attempting to contract when the muscle is on the stretch), when the muscle is unable to overcome the resistance. Explosive sprinting action affects the hamstrings and the quadriceps, and rectus femoris particularly may be affected by kicking against strong resistance. A direct blow to the quadriceps may cause severe haematoma. Patellar instability, subluxation or dislocation affects the medial quadriceps expansions, vastus medialis or the medial capsule.
Repetitive minor injury results in microtrauma, making the onset of the lesion difficult to recall, and the examiner will have to be aware of contributing factors such as overtraining, training errors, foot posture and faulty knee joint biomechanics. Lateral knee pain due to iliotibial band friction syndrome is common in long-distance runners. Infrapatellar tendinopathy is common in activities associated with jumping and the bursae can be inflamed if any structures passing over them are overused.
The duration of the symptoms will indicate the stage in the inflammatory process reached, or the recurrent nature of the condition. Different treatment approaches depend on the acute, subacute or chronic nature of a ligamentous sprain or muscle belly strain. Overuse lesions around the knee tend to be chronic in nature and are present for some considerable time before the patient seeks treatment.
Recurrent episodes of pain and swelling may be due to instability and derangement of the joint. Patellar subluxation, meniscal lesions or partial ligamentous tears may produce pain and joint effusion after use. Degenerative osteoarthrosis may be symptom-free until overuse triggers a synovitis with increased pain and swelling.
The symptoms and behaviour need to be considered. The behaviour of the pain and the symptoms described by the patient are very relevant to diagnosis at the knee. Immediate pain after injury indicates a severe lesion but pain developing or increasing slowly over several hours may indicate less serious pathology. The ability to continue with the sport or activity after the onset of pain is often indicative of minor ligamentous sprain, whereas major ligament disruption and muscle tears, meniscal lesions or cruciate rupture often result in the patient being totally incapacitated.
Total rupture of a ligament may produce severe pain at the time of injury but, following the initial injury, pain may not be a particular feature since the structure is totally disrupted. Partial ligamentous rupture continues to produce severe pain on movement.
The quality of the pain may indicate severity, but it is important to remember the subjective nature of pain. Aggravating factors can be activity, which indicates a mechanical or muscular lesion, or rest, which indicates a ligamentous lesion with an inflammatory component.
Postures such as prolonged sitting may affect the patellofemoral joint in particular. A pseudo-locking effect often occurs when the patient first gets up to weight-bear. This is not the same as true locking of the knee joint, but is a stiffness experienced by the patient which usually resolves after a few steps. It is thought to be due to excessive friction from changes in the articular cartilage of the patella. Walking, squatting and using stairs all aggravate patellofemoral conditions, particularly going downstairs, when the forces acting on this joint are increased to approximately three times body weight.
The tibiofemoral joint, as the weight-bearing joint, usually produces symptoms on weight-bearing activities, i.e. the stance phase of walking or running or prolonged standing. Pain produced on deep knee bends, rising from kneeling and rotational strains may indicate a meniscal lesion.
The other symptoms described by the patient give important clues to diagnosis. Swelling may be a symptom and it is important to know if it is constant or recurrent or provoked by activity. Swelling that usually occurs quickly within 2–6 h of injury is indicative of haemarthrosis. It can take up to 24 h to appear but this is not its normal presentation. The joint may feel warm to touch and the swelling may be tense. Structures responsible for a haemarthrosis are those with a good blood supply; the anterior cruciate ligament associated with torn synovium being the commonest cause of a haemarthrosis (Shaerf & Banerjee 2008).
Amiel et al (1990) quoted a study by Noyes in which over 70% of patients presenting with acute haemarthrosis of the knee had an acute tear of the anterior cruciate ligament. In children, however, haemarthrosis is more likely to be indicative of an osteochondral fracture than an anterior cruciate ligament injury (Baker 1992). The forces required for rupture of the posterior cruciate ligament are great and therefore the posterior capsule usually tears as well with blood escaping into the calf, where swelling and bruising may have been noticed by the patient.
Swelling which develops more slowly over 6–24 h is synovial in origin due to traumatic arthritis. Structures with a relatively poor blood supply tend to produce this traumatic arthritis, e.g. meniscal lesions, the deep part of the medial collateral ligament involving the capsule of the knee joint and subluxation or dislocation of the patella.
Activity may provoke swelling in conditions such as degenerative joint disease, chronic instability or internal derangement. This may be confirmed after the objective examination which may stir up the condition. Localized swelling may indicate bursitis, e.g. prepatellar bursitis, Baker’s cyst (synovial effusion into the gastrocnemius or semimembranosus bursa due to effusion in the knee joint) or meniscal cyst, which more commonly affects the lateral meniscus.
The presence of an effusion may affect the gait pattern and limit full extension. Reflex inhibition of the quadriceps muscle and an inability to lock the knee gives a feeling of insecurity on weight-bearing with the patient complaining of a sensation of ‘giving way’. Giving way on weight-bearing may also be due to a loose body or meniscal lesion; it is momentary and occurs together with a twinge of pain. Muscle imbalances, particularly involving VMO, may produce a feeling of apprehension as the knee feels as if it will give way. This may occur when weight-bearing after sitting for prolonged periods or walking downstairs.
True locking of the knee is indicative of a meniscal lesion and usually occurs in conjunction with a rotary component to the injury. It has a tendency to recur. The locking may resolve spontaneously over several hours or days or it may need to be manipulatively unlocked. Locking usually occurs at 10–40° short of full extension (Hartley 1995). Meniscal lesions occurring in isolation may present with acute pain and swelling and the patient may report locking or catching. Degenerative meniscal lesions occur in older patients who present with an atraumatic history, mild swelling, joint line pain and mechanical symptoms (Greis et al 2002). A ruptured anterior cruciate ligament can cause locking as the ligamentous flap catches between the joint surfaces. True locking must be distinguished from the pseudo-locking associated with the patellofemoral joint after prolonged sitting.
Provocation of pain on the stairs is important. The patellofemoral joint characteristically produces more pain on coming downstairs, due to the greater joint reaction force, although the pain may also have been provoked while walking upstairs.
Clicking, snapping or catching may be due to internal derangement. Patients often describe a ‘popping’ sensation on injury that can indicate cruciate ligament rupture. Grating and pain associated with crepitation are usually indicative of degenerative changes of the tibiofemoral joint, patellofemoral joint, or both.
To exclude symptoms arising from the lumbar spine, the patient should be questioned about paraesthesia and pain provoked by coughing or sneezing.
Other joint involvement should be explored to ascertain the possibility of inflammatory joint disease. Have there been any previous knee problems or knee surgery? Past medical history should exclude serious pathology, and questions about medications will highlight any contra-indications to treatment. If degenerative osteoarthrosis is considered a factor in the diagnosis, the patient can be questioned about significant weight gain. It has been suggested that obesity is a cause of osteoarthrosis in the knee (Felson et al 1988, Felson & Chaisson 1997). As well as past medical history, establish any ongoing conditions and treatment. Explore other previous or current musculoskeletal problems with previous episodes of the current complaint, any treatment given and the outcome of treatment.
Inspection
The knee should be fully extended in standing. If not, some compromise of the terminal screw home or locking mechanism exists, or an effusion with limited extension is present as part of the capsular pattern.
The knee should be inspected in both the weight-bearing and non-weight-bearing positions. In standing, the normal slight valgus tibiofemoral angle should be obvious.
The whole lower limb is inspected for leg length discrepancy and obvious bony deformity such as genu valgum, varum, recurvatum or ‘wind-swept’ knees (one varus, one valgus). The posture of the feet is important. Overpronation or a tight Achilles tendon may be related to the knee symptoms and a detailed biomechanical assessment is then required. Position of the pelvis and obvious spinal deformities may be important to note if relevant to symptoms.
The position, shape and size of the patellae are noted if relevant to the presenting symptoms. Patellar alignment is measured by the Q-angle – the angle between the line of the quadriceps muscle (anterior superior iliac spine to the midpoint of the patella) and the patellar tendon (midpoint of the patella to the tibial tuberosity). An angle of between 15 and 20° is considered normal for patellar alignment and tracking, and less or more than this can be considered to be a malalignment (Norris 2004). Congenital malformation of the patella, i.e. small or absent, may lead to instability and recurrent subluxation of the patella as a rare cause of knee pain (Bongers et al 2005).
Colour changes may be present, especially if the condition is acute, when the joint looks red due to inflammatory changes. Direct trauma may produce bruising and acute muscle lesions may show bruising, particularly in the quadriceps and hamstring muscles. Distal colour changes may be indicative of circulatory problems.
In standing, all muscle groups are inspected for wasting. The quadriceps wastes rapidly due to reflex inhibition if pain, swelling or degenerative change is present. In patellofemoral problems wasting of the oblique fibres of vastus medialis may be obvious.
Loss of the dimple on the medial aspect of the knee will indicate the presence of swelling, drawn out of the suprapatellar bursa by gravity. Minor swelling may not be obvious and may only be apparent on testing by palpation in the supine position.
State at rest
Before any movements are performed, the state at rest is established to provide a baseline for subsequent comparison.
Examination by selective tension (objective examination)
The suggested sequence for the objective examination will now be given, followed by a commentary including the reasoning in performing the movements and the significance of the possible findings. Comparison should always be made with the other side.
Supine lying
Eliminate the hip
• Passive hip flexion (Fig. 11.10)
 |
| Figure 11.10
Passive hip flexion.
|
• Passive hip medial rotation (Fig. 11.11)
 |
| Figure 11.11
Passive hip medial rotation.
|
• Passive hip lateral rotation (Fig. 11.12)
 |
| Figure 11.12
Passive hip lateral rotation.
|
• Passive knee flexion (Fig. 11.13)
 |
| Figure 11.13
Passive knee flexion.
|
• Passive knee extension, once for range (Fig. 11.14a), once for end-feel (Fig. 11.14b)
 |
| Figure 11.14
Passive knee extension: (a) for range and (b) for end-feel.
|
• Passive valgus stress (Fig. 11.15a, b)
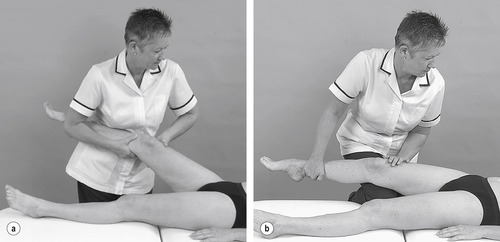 |
| Figure 11.15
Valgus stress (a) and (b) alternative position.
|
• Passive varus stress (Fig. 11.16)
 |
| Figure 11.16
Varus stress.
|
• Passive lateral rotation (Fig. 11.17a)
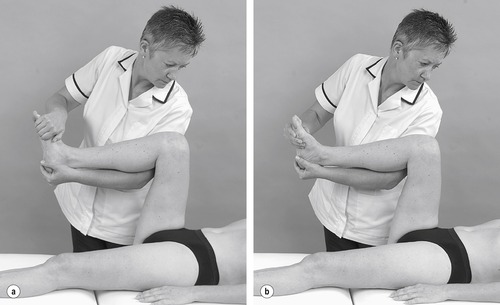 |
| Figure 11.17
Passive (a) lateral and (b) medial rotation.
|
• Passive medial rotation (Fig. 11.17b)
 |
| Figure 11.18
Posterior drawer test.
|
 |
| Figure 11.19
Assessment of laxity of the posterior cruciate ligament.
|
 |
| Figure 11.20
Assessment of laxity of the posterior cruciate ligament, alternative position.
|
• Anterior drawer test (Fig. 11.21)
 |
| Figure 11.21
Anterior drawer test.
|
• Lachman test (Fig. 11.22)
 |
| Figure 11.22
Lachman test.
|
Provocation tests for the menisci (Saunders 2000)
• Flexion, lateral rotation and valgus (Fig. 11.23)
 |
| Figure 11.23
Flexion, lateral rotation and valgus.
|
• Flexion, lateral rotation and varus (Fig. 11.24)
 |
| Figure 11.24
Flexion, lateral rotation and varus.
|
• Flexion, medial rotation and valgus (Fig. 11.25)
 |
| Figure 11.25
Flexion, medial rotation and valgus.
|
• Flexion, medial rotation and varus (Fig. 11.26)
 |
| Figure 11.26
Flexion, medial rotation and varus.
|
Prone lying
• Resisted knee extension (Fig. 11.27)
 |
| Figure 11.27
Resisted knee extension.
|
• Resisted knee flexion (Fig. 11.28)
 |
| Figure 11.28
Resisted knee flexion.
|
Palpation
• Once a diagnosis has been made, the structure at fault is palpated for the exact site of the lesion
The combined history and examination are important at the knee. The symptoms described by the patient result from functional weight-bearing activities but the knee is examined clinically in a non-weight-bearing position. Lesions vary from simple contusions, muscle strains and ligament sprains to arthritis and major ligamentous rupture and instability. It is important clinically to be able to diagnose lesions at the knee, but also to appreciate the limits of clinical examination and determine when onward referral for specialist opinion is necessary.
With more chronic knee problems, the hip and lumbar spine should be cleared first to eliminate more proximal causes of pain referring to the knee.
The acute knee should be examined as soon as possible after injury, before effusion causes pain, apprehension and limited movement. Effusion makes it difficult to test accurately for ligamentous instability and to apply provocative meniscal tests. The acute knee is usually managed conservatively until the traumatic arthritis subsides. Residual instability which fails to respond to conservative management or internal derangement due to meniscal lesions can be dealt with surgically at a later date, and neither is usually considered to be an emergency.
Palpation tests are conducted for signs of activity within the joint. Temperature changes are assessed using the dorsal aspect of the same hand and comparing like with like. Inflammatory conditions will show an increase in heat compared with the other side. It may be necessary to repeat this test at the end of the examination to assess whether an inflammatory response has been triggered by the examination, giving an indication of the irritability of the lesion.
Several tests exist for swelling and the choice is left to the reader on the basis of personal opinion on effectiveness and preference. A sensitive test for minor swelling involves placing the finger and thumb of one hand on either side of the patella just below the bony periphery. The web between the index finger and thumb of the other hand applies compression to the suprapatellar bursa which squeezes fluid out into the joint cavity and, if positive, is felt to part the finger and thumb of the other hand. Other tests involve wiping the fluid from one side of the joint to the other; compression of the suprapatellar bursa; and compression at the front of the joint just below the patella to assess fluctuation of fluid; or pressing down on the patella to assess for the presence of a patellar ‘tap’.
Synovial thickening is assessed by palpation of the medial and lateral femoral condyles.
Thickening of the synovium is normal here because of the presence of synovial plica and the medial plica is more obvious to palpation. Assessment for excessive thickening of the synovium is confirmed if the tissue feels ‘boggy’ to the touch. Hill et al (2001) regard synovial thickening as a contributor to pain in the osteoarthritic knee and an indication of the severity of the disease.
The position of the patella should be assessed for size and to see if it is shifted, tilted or rotated with respect to the other side. It should be emphasized here that the orthopaedic medicine approach has limited relevance to patellofemoral malalignment syndromes. The interested reader is referred to other texts on this subject.
The primary passive movements of flexion and extension are performed to assess the tibiofemoral joint. Pain, range of movement and end-feel are noted, which will indicate the presence of the capsular or non-capsular pattern. Bijl et al (1998) found an indication of the capsular pattern of the knee, but could not recommend it as a valid test for arthritis. In contrast, Fritz et al (1998) found evidence for the existence of a capsular pattern to support the identification of patients with knee joint arthrosis or arthritis. Passive flexion normally has a soft end-feel and passive extension a hard end-feel. The thigh is fixed above the knee and the foot is lifted to assess the range of hyperextension present, normally 5–10°.
A further test is conducted for the end-feel of extension whereby the leg is lifted into approximately 10° of flexion and dropped into extension to assess for the normal, bony hard end-feel. This is sometimes known as the ‘bounce home’ test and an abnormally ‘soft’ or ‘springy’ end-feel indicates the end of range has not been reached due to a meniscal lesion, loose body or joint effusion. The presence of the non-capsular pattern indicates a ligamentous lesion or a loose body in the joint, or possibly a meniscal problem.
The secondary passive movements at the knee are applied to assess the ligaments. It is important to compare the two limbs since, although joint motion varies considerably within the population, there is very little variation between right and left in a normal subject (Daniel 1990). The tests depend on the muscles being relaxed and the eye, feel and experience of the examiner, who is looking for an excessive range of movement compared with the asymptomatic knee and an abnormal soft end-feel with no definite end-point if laxity is present.
Secondary passive movements are applied to the knee in a loose packed position of 20–30° of flexion since no passive or accessory movements should be present with the knee in full extension. If movement can be detected in the close packed position, serious ligamentous disruption is present, with accompanying damage to capsular components. Minor ligamentous laxity may be subclinical; therefore recognition of such symptoms from the history leads to onward referral for more detailed assessment of ligamentous laxity.
The intention here is to list the ligaments that need to be tested, with the figures providing illustrations of suggested testing methods. The methods are not proposed as the ‘best’ way of testing and will not be described in detail within the text. The interested reader is referred to the fuller descriptions of these and other methods to be found in textbooks devoted to the knee and sports injuries.
Butler et al (1980) referred to the concept of primary and secondary ligament restraints to movement in a specific direction. A ligament may act as a primary restraint in one direction and as a secondary restraint in another. Rupture of a primary restraint results in excessive movement; rupture of the secondary restraint to that movement, with the primary restraint intact, does not result in increased movement. Rupture of both primary and secondary restraint produces a much greater increase in movement. For example, rupture of the anterior cruciate ligament (primary restraint) produces some increase in anterior translation, rupture of the medial collateral ligament (secondary restraint) produces no detectable increase in anterior translation and rupture of both (primary and secondary restraints) results in a much greater increase in movement.
Orthopaedic medicine treatment techniques will be directed at simple ligamentous sprains, but it is important to recognize more serious ligament disruption or intra-articular derangement due to a meniscal lesion in order to make the appropriate onward specialist referral.
Valgus and varus stresses are applied to the knee in approximately 20–30° of flexion and assess the primary stabilizing function of the medial and lateral collateral ligaments, respectively. The range of movement available and any pain reproduced are noted and compared with the asymptomatic knee. The end-feel is assessed, which is normally firm elastic.
Axial rotation should be tested at 90° of knee flexion as the range of movement is greatest in this position. Passive lateral rotation is usually 45° and assesses the medial coronary ligaments, and passive medial rotation is usually 35° and tests the lateral coronary ligaments.
The posterior and anterior drawer tests are both performed with the knee at 90° of flexion. The neutral position of the resting knee must be established compared with the contralateral normal knee.
The posterior drawer test is applied first for the posterior cruciate ligament, since a deficient posterior cruciate ligament could give a false-positive to anterior translation. As the tibia is pushed posteriorly, the thumbs rest over the anterior joint line to assess the ‘sag-back’ or step created anteriorly by the excessive posterior drawer. Isolated rupture of the posterior cruciate ligament is a rare lesion, but the posterior drawer test is a sensitive and specific test for the posterior cruciate ligament (Rubinstein et al 1994, Malanga et al 2003, Palastanga et al 2006).
The anterior drawer test assesses the anterior cruciate ligament, although it is considered an insensitive and poor diagnostic indicator of lesions of this ligament, especially in the acute knee (Katz & Fingeroth 1986, Malanga et al 2003, Shaerf & Banerjee 2008). The haem-arthrosis and traumatic arthritis ‘splint’ the knee, making it difficult to place the knee in 90° of flexion, and pain produces protective spasm in the hamstrings preventing anterior tibial translation. In a chronic knee, the secondary stabilizing role of an intact medial collateral ligament may prevent anterior translation at 90° of knee flexion. With a more chronic injury the reliability of both the anterior drawer test and the Lachman test is good at 95–99% (Mitsou & Vallianatos 1988). Bowditch (2001) is less convinced, believing that a positive drawer test at 90° in the chronic knee may be due to laxity of the secondary constraints, e.g. the medial collateral ligament.
The Lachman test is a clinical test with a high diagnostic accuracy to determine anterior cruciate laxity (Smith & Green 1995, Malanga et al 2003, Shaerf & Banerjee 2008). The Lachman test may be difficult to perform especially if the limb is large or the patient unable to relax sufficiently. Several modifications have been made to the Lachman test since it was first described by Torg et al in 1974, including a ‘drop leg’ Lachman test described by Adler et al (1995) and a reversed Lachman test described by Cailliet (1992). An intact anterior cruciate ligament should provide a normal hard end-feel or ‘stop’ to the drawer movement applied. The end-feel with a ruptured anterior cruciate ligament will feel ‘soft’ or absent when compared to the other knee (Bowditch 2001, Shaerf & Banerjee 2008).
Similarly, the pivot-shift test has several methods of application (see Malanga et al 2003, Hattam & Smeatham 2010). It is essentially a dynamic test to determine the degree of instability related to anterior cruciate ligament injury and has a low false-negative rate (Shaerf & Banerjee 2008). However, it may also be difficult to apply in the acute knee due to pain and swelling.
Four provocation tests are applied if the history indicates a meniscal lesion. Each meniscus is put under compression and stress during combined movements of flexion, valgus, varus and both rotations.
Other traditional tests for a meniscal lesion include the ‘bounce home’ test of passive knee extension for end-feel, the McMurray’s test which takes the leg from a position of flexion towards extension, with medial or lateral rotation of the tibia, and Apley’s grind or compression test (see Hattam & Smeatham 2010). There is mixed support for the various meniscal tests in the literature. Joint line tenderness seems to be the best clinical indicator of medial meniscus injury and there are reports of the low specificity and sensitivity rates associated with the McMurray’s test (Malanga et al 2003). Mohan & Gosal (2007) examined their own reliability in clinical diagnosis of meniscal tears and recorded their accuracy as 88% for medial meniscal lesions and 92% for lateral, being as reliable, and in some cases more reliable, than MRI. They used the McMurray test and joint line tenderness along with the history to make their diagnosis.
Negative clinical testing is not conclusive evidence that a meniscal lesion does not exist. If the history is indicative, or the patient is experiencing recurrent episodes of locking and/or giving way, referral should be made for specialist opinion with arthroscopy, in modern practice the ‘gold standard’ for diagnosis at the knee (Curtin et al 1992).
The resisted tests are applied looking for pain and power. Resisted knee extension tests the quadriceps and resisted knee flexion the hamstrings. Having established that there is no pain on testing the muscles in the mid-position, accessory provocation tests may be included to provoke minor contractile lesions. The quadriceps and hamstrings can be tested in varying degrees of knee flexion and extension, and isotonically. The hamstring muscles may be tested in conjunction with medial or lateral rotation to isolate the lesion to the medial or lateral hamstrings. Popliteus may be assessed by testing resisted knee flexion in conjunction with resisted medial rotation of the tibia (Fig. 11.29).
 |
| Figure 11.29
Resisted knee flexion and medial rotation of the tibia.
|
CAPSULAR LESIONS
The presence of the capsular pattern indicates arthritis and the history indicates the cause of the arthritis. The possibilities are an acute episode of degenerative osteo-arthrosis, inflammatory arthritis, such as rheumatoid arthritis, or traumatic arthritis.
Traumatic arthritis is usually a secondary response to a ligamentous lesion at the knee. As a capsular ligament, damage to the medial collateral ligament can produce a secondary traumatic arthritis; a ruptured cruciate ligament may also produce a haemarthrosis.
Symptomatic osteoarthrosis and inflammatory arthritis may benefit from an intra-articular injection of cortico-steroid with some evidence for relief of moderate to severe pain (Conaghan et al 2008). Treatment for traumatic arthritis should be directed to the cause of the lesion, i.e. the ligamentous injury.
Position the patient comfortably in supine-lying with the knee supported in extension. Glide the patella medially, pressing down on the lateral edge to lift the medial border (Fig. 11.30). Insert the needle halfway along the medial border of the patella, aiming laterally and slightly posteriorly, parallel with the articular surface of the patella (Fig. 11.31). Once the needle is intra-articular, deliver the injection as a bolus. The patient is advised to maintain a period of relative rest for approximately 2weeks following injection. Chakravarty & Pharoah (1994) demonstrated that 24 h of complete bed rest following injection of the knee joint for rheumatoid arthritis produced a more prolonged benefit.
 |
| Figure 11.30
Injection of the knee joint.
|
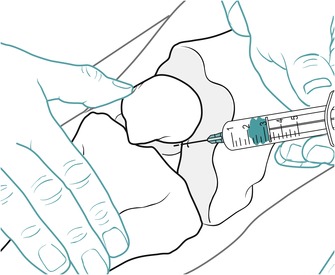 |
| Figure 11.31
Injection of the knee joint showing direction of approach and needle position.
|
Controversy exists over repeated corticosteroid injections into weight-bearing joints and its association with the development of steroid arthropathy, with opposing views being supported (Parikh et al 1993, Cameron 1995). Raynauld et al (2003) conducted a randomized, double-blind, placebo-controlled trial to determine the efficacy of long-term intra-articular corticosteroid injection (40 mg triamcinolone acetonide every 3 months) in osteoarthritis of the knee. The 1- and 2-year follow-up showed no difference in the loss of joint space over time between the corticosteroid injection group and the saline-injected group. There was a trend in the corticosteroid group to show greater symptomatic relief, with pain and stiffness significantly improved. The authors concluded that there was no significant deleterious effect on the anatomical joint structure in either group, indicating that repeated intra-articular injections are safe.
Chapter 10 includes a short discussion stimulated by a study by Kaspar & de Van de Beer (2005) that found that the incidence of infection increased after hip arthroplasty where the hip had previously been injected with corticosteroid. Horne et al (2008) looked at the incidence of infection following total knee arthroplasty where the knee had previously been injected with corticosteroid. In contrast to the findings of Kaspar & de Van de Beer, no link between previous injection and post-operative infection was found, even where multiple injections had been given.
Baker et al (2001) conducted a randomized controlled trial to examine the efficacy of home-based progressive strength training in older adults with knee osteoarth-ritis. Exercises included functional squats, step-ups and isotonic exercises using ankle weights and the results demonstrated that a 4-month home-based exercise programme significantly decreased pain and improved physical function. This study supports the role of strength training in osteoarthritis of the knee and progressive strengthening should be included as part of overall management.
NON-CAPSULAR LESIONS
Loose body
From the history, symptoms of momentary giving way on weight-bearing accompanied by twinges of pain indicate a possible loose body in the knee joint. The loose body may be a fragment of cartilage or bone, or both (osteochondral), and can be associated with degenerative osteo-arthrosis in the older adult (Saotome et al 2006), or a flap of meniscus which may momentarily give way or lock on weight-bearing. Although its ability to act as a loose body is unclear, a ‘floating’ meniscus may be visible on magnetic resonance imaging where the coronary ligaments are disrupted or stretched, rather than the meniscus itself, and the meniscus commonly stays intact (Bikkina et al 2005). An anterior cruciate ligament tear can present as a loose body and a tear should be considered if the symptoms arose after trauma.
Loose bodies can be stable, fixed in a synovial recess or bursa, or attached to synovial membrane, where they tend not to be displaced. Unstable loose bodies can move freely in the joint to become trapped at irregular intervals between the articular bone ends, causing intermittent symptoms and internal joint derangement (Bianchi & Martinoli 1999).
Osteochondritis dissecans may affect the knee in adol-escents, usually between the ages of 15 and 20 years. A small fragment of bone becomes demarcated from a condyle and detaches to form a loose body. The symptoms are usually pain, swelling, locking and giving way. On examination, a non-capsular pattern is present with a small limitation of flexion or extension, but not both. The end-feel is characteristically springy.
If the joint should lock, it is usually temporary and it unlocks spontaneously. A joint which requires manipulative unlocking normally requires referral for specialist opinion with possible arthroscopy. The manipulation may provide temporary relief however, if surgery is not an option.
A loose body may become impinged between the joint surfaces in degenerative osteoarthrosis. If the loose fragment impinges on the medial side of the joint, the patient presents with signs of an intrinsic medial collateral sprain, but in the absence of trauma. The capsular pattern of degenerative osteoarthrosis is present with a non-capsular pattern superimposed; the patient complains of increased pain on a valgus stress. The primary lesion should be treated and the secondary ligamentous sprain should then subside.
The treatment of choice to reduce a loose body is strong traction together with Grade A mobilization, theoretically aiming to move the loose body to another part of the joint and to restore full, pain-free movement.
The strong traction is applied to the joint and a medial or lateral movement is applied simultaneously with a movement from flexion towards extension.
Loose-body mobilization technique 1 (Saunders 2000)
This technique may only be applied to a relatively fit patient, but it enables the technique to be applied single-handedly.
Position the patient in supine lying with the legs hanging over the end of the couch, the thighs supported. Arrange the couch so that it is as high as it will go and elevate the head end of the couch. Run your hand down the posterior aspect of the ankle, grasping the calcaneus and pulling the ankle into dorsiflexion. Place the other hand on top of the talus in order to rotate the leg into either medial or lateral rotation (Figure 11.32 and Figure 11.33) (position your hands such that the hand on top of the foot will be pulling, not pushing, into rotation). Bend your knees and straighten your arms to apply traction (Fig. 11.34). Once traction is established, straighten your knees to extend the patient’s knee, smartly rotating the leg at the same time (Fig. 11.35).
 |
| Figure 11.32
Loose-body mobilization for the knee 1; hand position for mobilization into medial rotation.
|
 |
| Figure 11.33
Loose-body mobilization for the knee 1; hand position for mobilization into lateral rotation.
|
 |
| Figure 11.34
Loose-body mobilization for the knee 1; starting position applying traction.
|
 |
| Figure 11.35
Loose-body mobilization for the knee 1; ending the manoeuvre, avoiding full extension of the patient’s knee.
|
Reassess the patient for an increase in range and a change in the end-feel. If the technique has helped, it can be repeated; if not, change your hand position to effect the opposite rotation. The basis of this technique is traction, rotation and a movement towards extension of the knee. It can be modified to suit the patient or operator and you are encouraged to be inventive with the technique. It can be applied with the patient sitting over the edge of the bed, raised to a suitable height, with the operator sitting on the floor; a ‘seat belt’ may be applied to help the traction.
Loose-body mobilization technique 2 (Cyriax 1984, Cyriax & Cyriax 1993)
This technique requires an assistant. Position the patient in prone-lying with the knee flexed to 90°. Stand adjacent to the patient’s flexed knee, placing your foot distal to the patient, on the couch. Place the web between your index finger and thumb of one hand around the calcaneus to pull the ankle into dorsiflexion; the other hand wraps comfortably around the dorsum of the foot. Lift the patient’s foot onto your flexed knee (Fig. 11.36a) and plantarflex your foot to raise the knee from the couch (Fig. 11.36b). Ask the assistant to apply the traction to the knee joint by placing two hands behind the knee joint and applying body weight to the thigh (Fig. 11.36c). Once traction is established, remove your foot from the couch and step down to the side (Fig. 11.36d). Maintain the traction as you smartly rotate the lower leg, simultaneously moving from flexion towards extension (Fig. 11.36e). Reassess and repeat as necessary.
 |
| Figure 11.36
Loose-body mobilization for the knee 2: (a) starting position; (b) plantarflexing foot to raise knee; (c) assistant applying counter-pressure through the thigh to apply distraction at the knee; (d) Grade A mobilization applied whilst moving towards extension and maintaining distraction; (e) completion of the manoeuvre.
|
Medial collateral ligament sprain
The medial collateral ligament is the ligament most vulnerable to injury at the knee, but the following principles of treatment may also be applied to the lateral collateral ligament if it is the site of the lesion. As the lateral collateral ligament is not associated with the joint capsule, the acute effusion common to medial collateral sprain is likely to be absent.
The collateral and cruciate ligaments function together to control and stabilize the knee. The medial collateral ligament is anatomically related to the medial meniscus and functionally related to the anterior cruciate ligament. Injury may result in ‘O’Donaghue’s unhappy triad’, affecting all three structures (Evans 1986, Staron et al 1994). If tears of the medial meniscus and anterior cruciate ligament are confirmed by MRI or arthroscopy, subtle signs of medial collateral ligament sprain should be sought, since the three conditions usually coexist (Staron et al 1994). Nakamura & Shino (2005) observe that there is an increased prevalence of ligament injuries at the knee in female athletes, particularly the anterior cruciate ligament, due to hormones/menstrual cycle and structural differences.
Rupture of the cruciate ligaments or a meniscal lesion produces an acute effusion which can be managed conservatively as for the acute phase of medial collateral ligament sprain. Once the acute phase has settled, a full assessment of the knee can be carried out, including assessment for ligamentous laxity and the provocative meniscal tests. A decision may then be taken concerning onwards referral for specialist opinion.
Ligament injuries are graded 1–3 according to the amount of laxity and the end-feel (Hartley 1995, Nakamura & Shino 2005, Azar 2006). The following is applied to the medial collateral ligament, but it should be noted that assessment for laxity on the acute knee may not be possible due to the effusion and painful muscle spasm. Brotzman & Wilk (2003) have proposed ranges of valgus movement that are likely to be associated with the grades of injury as a guide:
Grade l
In a Grade I injury there is stretching and microfailure of some fibres of the ligament, pain, tenderness and swelling at the site of the injury, possibly a mild capsular pattern as the medial collateral ligament is an integral part of the capsule, no notable elongation or clinical instability, and a firm elastic end-feel. Normal valgus laxity 0–5 mm in 20–30° flexion.
Grade ll
Grade II injury is associated with moderate–major tearing of the ligament fibres, some exceeding their elastic limit, pain and tenderness at the site of injury, moderate to severe swelling, movement limited in the capsular pattern, a minor degree of ligamentous laxity noted clinically, and a relatively firm elastic end-feel with a definite end-point. Valgus stress test applied at 20° flexion 5–10 mm.
Grade lll
Grade III injury is diagnosed when there is macrofailure, or complete rupture of the ligament, swelling, possibly haemarthrosis and a capsular pattern of limited movement, severe pain at the time of injury, but relatively little since, definite ligamentous laxity noted, and the joint may click as it returns to the neutral position. There is a soft end-feel with no definite end-point. Valgus stress test at 30° flexion>10 mm
Not all major ligamentous ruptures require surgical reconstruction, and decisions are based on the lifestyle of the patient or the site of the injury. Azar (2006) explored the consensus for treatment of Grade lll injuries and found that there was a tendency towards non-operative management if the injury was at the femoral attachment of the ligament, with surgical repair for lesions at the tibial insertion. A good functional recovery from ligamentous laxity may be achieved by strengthening the dynamic stabilizers of the knee, the hamstrings and quadriceps muscles, while maintaining control with appropriate braces.
If haemarthrosis is present in the early acute knee, the advice has traditionally been that it should be aspirated, although Shaerf & Banerjee (2008) clarify that this is not indicated unless there is a tense haemarthrosis with a fixed flexion deformity, or there is the need for pain relief because of the distension of the joint capsule. Wallman & Carley (2002) conducted a review to establish whether aspiration of a traumatic knee arthrosis improved patients’ symptoms but, in spite of reviewing 267 papers, they found no reference to the outcome of aspiration and no conclusions could be drawn. Aspiration of haemarthrosis is currently conducted less routinely and more research is required to guide practice.
From the history, medial collateral ligament sprain is possible if the knee is subjected to excessive valgus rotation of the flexed knee or a hyperextension forcse. A combination of trauma may occur and, as already stated, the medial collateral ligament can be damaged in association with the anterior cruciate ligament and medial meniscus.
Acute medial collateral ligament sprain
Initially, the lesion is accompanied by a secondary traumatic arthritis which presents with a capsular pattern of limited movement. It may be difficult to apply provocative stress tests to either the ligament or menisci to assess associated damage. The history of the mechanism of the injury, the position of the leg and the forces applied will indicate medial collateral ligament sprain. The valgus test will produce pain to confirm diagnosis, but the grade of sprain will be difficult to ascertain initially since the reflex muscle spasm and effusion effectively splint the knee. Presence of haemarthrosis indicates possible anterior cruciate ligament damage and the Lachman test can at least be applied to the acute knee. Haemarthrosis and the presence of a positive Lachman test may indicate onward referral for specialist opinion.
The acute situation is managed conservatively with daily treatment initially, consisting of PRICE (see Ch. 4). Gentle transverse frictions are started as early as possible, depending on the irritability of the lesion, to gain some movement of the ligament over the underlying bone. This is followed by Grade A mobilization to maintain the function of the ligament.
The patient is encouraged to maintain a normal gait pattern with the aid of crutches if necessary. Once it is judged that the tensile strength of the healing ligament has improved, the depth of transverse frictions is gradually increased and the range of active pain-free movement becomes greater, aiming to apply a directional stress to encourage alignment of fibres. The regime continues until a full range of pain-free movement is restored, always guided by reassessment for a reduction or exacerbation of symptoms. Other exercises are incorporated as appropriate, aiming towards full rehabilitation of the patient.
Transverse frictions for acute sprain of the medial collateral ligament (Cyriax 1984, Cyriax & Cyriax 1993)
Position the patient in half-lying with enough pillows to support the knee in the maximum amount of extension that can be achieved without causing pain. Palpate for the site of the lesion, which may be difficult to locate due to the swelling. However, the commonest site of sprain is at the joint line and this can be located by following the advice given in the surface marking and palpation section earlier in the chapter. Place two or three fingers across the site of the lesion and gently apply transverse frictions to achieve an analgesic effect (Fig. 11.37). Once some analgesia and depth are achieved, apply deeper transverse frictions for approximately six sweeps, aiming to move the ligament fibres over the underlying bone in imitation of its normal function. Follow this immediately with Grade A active mobilization towards extension.
 |
| Figure 11.37
Transverse friction massage of the acute medial collateral ligament sprain, in extension.
|
Next, support the knee in the maximum amount of flexion that can be achieved without pain, and repeat the friction technique as above (Fig. 11.38). Follow this immediately with Grade A active exercises towards flexion.
 |
| Figure 11.38
Transverse friction massage of the acute medial collateral ligament sprain, in flexion.
|
On a daily basis, the pain and swelling reduce and the range of movement increases. The knee should not be pushed towards extension as the medial collateral ligament is taut in extension and may become overstretched.
The usual exercises for maintenance of muscle strength should be included together with gait re-education and, eventually, full rehabilitation according to the patient’s needs. Treating the ligament in this way maintains its mobility, length and function and should avoid the need to stretch.
An uncommon complication of medial collateral ligament sprain is Stieda–Pellegrini’s syndrome (also known as Pellegrini–Stieda syndrome or Pellegrini–Stieda disease) and this should be considered if the range of movement at the knee fails to improve as expected (Cyriax 1982). It is believed that, following trauma to the medial collateral ligament, calcium is deposited within the ligament, usually near the superior medial femoral condyle (Wang & Shapiro 1995). Active movement of the knee joint is continued and corticosteroid injection may be appropriate if the pain persists.
Chronic medial collateral ligament sprain
The patient has a past history of sprain to the ligament which may have largely settled without treatment. However, activity still causes pain and transient swelling around the ligament. On examination, the patient may have end-range pain or limitation of movement of passive flexion, extension or both.
The valgus stress test produces the pain, as may hyperextension and passive lateral rotation – movements which tighten the ligament. Assessment should be made for instability and any associated structural damage of the cruciate ligaments and/or menisci.
The ligament has developed adhesions which interfere with the normal gliding function of the ligament. The principle of treatment is to rupture the unwanted adhesions with a Grade C manipulation, once the ligament has been prepared by deep transverse frictions. Following manipulative rupture, the patient is instructed to mobilize vigorously in order to maintain the movement gained through manipulation.
Grade C manipulation for chronic sprain of the medial collateral ligament (Cyriax 1984, Cyriax and Cyriax 1993)
The ligament is prepared for the manipulation with transverse frictions to achieve the analgesic effect. If passive extension is limited, position the patient in half-lying with the knee in maximum extension and locate the site of the lesion by palpation, commonly at the joint line. Apply the transverse frictions with the index finger reinforced by the middle finger and the thumb placed on the opposite side of the knee for counterpressure (Fig. 11.39). Direct the pressure down onto the ligament and sweep transversely across the fibres, keeping the finger parallel to the upper border of the tibia. Treatment is applied until the analgesic effect is achieved.
 |
| Figure 11.39
Transverse friction massage of the chronic medial collateral ligament sprain in extension.
|
The Grade C manipulation follows immediately after achieving the analgesic effect. Place one hand just above the knee to maintain the thigh on the couch. Wrap the other hand around the posterior aspect of the heel. Lean on the thigh, lifting the lower leg and, once end-range extension is achieved, apply the overpressure by a minimal amplitude, high velocity thrust applied by side-flexing your body (Fig. 11.40).
 |
| Figure 11.40
Grade C manipulation into extension.
|
If flexion is limited, next place the knee in maximum flexion. The direction of the transverse frictions will have to be adjusted to run parallel to the upper tibia, remembering that the ligament moves backwards a little in flexion (Fig. 11.41).
 |
| Figure 11.41
Transverse friction massage of the chronic medial ligament sprain in flexion.
|
The Grade C manipulation follows immediately after achieving the analgesic effect by applying an overpressure towards flexion with the knee placed into lateral rotation, to achieve full range, since the insertion of the medial collateral ligament sweeps forward. Place the hip and knee in maximum flexion. Cup the heel into your hand and pull the leg into lateral rotation by resting your forearm along the medial border of the foot (Fig. 11.42a). Maintain the lateral rotation and take the leg into maximum passive flexion. A minimal amplitude, high velocity thrust is applied into flexion (Fig. 11.42b). The technique can be modified to apply the thrust in the direction of the lateral rotation, or to add a valgus stress if assessment of the patient shows movement to be limited in these directions.
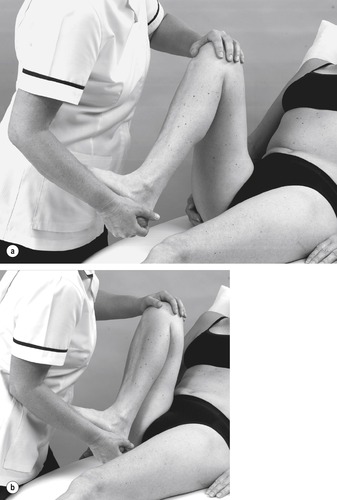 |
| Figure 11.42
Grade C manipulation into flexion: (a) starting position; (b) completion of the manoeuvre.
|
Coronary ligaments
The patient presents with a history of rotational strain and on examination there is pain on the appropriate passive rotation. The coronary ligaments may be involved in a hyperextension injury since the menisci move forwards during extension of the tibiofemoral joint. Ligament sprain can coexist with meniscal injury, or the ligaments can be disrupted or stretched rather than the adjacent meniscus itself, which stays intact. This may appear as a floating meniscus on MRI (Bikkina et al 2005). The longer lateral coronary ligaments are less vulnerable to trauma than the shorter medial coronary ligaments and the attachment of the medial meniscus to the deep part of the medial collateral ligament makes the medial aspect of the joint more susceptible to injury.
A sprain of the medial coronary ligaments will be discussed, but if the lesion lies in the lateral coronary ligaments, the same principles apply.
An effusion may be present depending on the severity of the lesion, but this is not usually as obvious as that associated with injury to the collateral or cruciate ligaments. Medial coronary ligament sprain produces pain on passive lateral rotation of the tibia with the tibiofemoral joint at 90° of flexion. Pain may also be provoked by passive extension as the menisci move forwards on the tibia. Palpation confirms the site of the lesion, which is usually on the superior surface of the anteromedial aspect of the medial meniscus where the coronary ligaments attach the meniscus to the tibial plateau. It is essential that full palpation is conducted, including through the medial collateral ligament, to determine the extent of the lesion.
Transverse frictions to the coronary ligaments
The treatment of choice is transverse frictions. Position the patient comfortably in half-lying with the knee in flexion and lateral rotation to expose the medial tibial condyle. Place an index finger reinforced by the middle finger on top of the edge of the medial meniscus at the site of the lesion in the medial coronary ligaments. Consider the position of the coronary ligaments that act as oblique ‘staples’ between the medial meniscus and the edge of the tibial plateau. Direct the pressure down onto the ligaments and sweep transversely across the fibres (Fig. 11.43). The transverse frictions are given for 10 min after the analgesic effect is achieved. Since the ligaments do not span the joint line, exercises or mobilization are not appropriate.
 |
| Figure 11.43
Transverse friction massage of the medial coronary ligaments.
|
The ligaments may be injected, using the same position as for the transverse frictions and applying the general principles with regard to dosage, a peppering technique and advising relative rest for up to 2 weeks (Figure 11.44 and Figure 11.45).
 |
| Figure 11.44
Injection of the medial coronary ligaments.
|
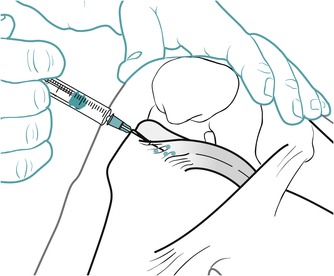 |
| Figure 11.45
Injection of the medial coronary ligaments showing direction of approach and needle position. Amended DRAWING
|
Bursitis
Overuse or excessive friction can affect any of the bursae around the knee. The patient presents with pain localized to the site of the lesion and there may be local swelling. The prepatellar and infrapatellar bursae are commonly involved and, if swelling is a problem, the bursa can be drained. Bursitis may respond to locally applied electrotherapy or an injection of corticosteroid into the bursa. Before injecting the bursa, however, it is important to be sure that no infection is present, since septic bursitis is possible in the superficial bursae.
Pes anserinus syndrome may involve the tendons and/or bursa, but the condition may mimic medial collateral ligament sprain. Pain and tenderness occur 5–6 cm below the medial joint line; this is aggravated by activity and there may be slight swelling and crepitus over the bursal area. Treatment consists of locally applied anti-inflammatory modalities or applying the principles of corticosteroid injection (Safran & Fu 1995, Kesson et al 2003).
Excessive friction may cause iliotibial band syndrome involving the iliotibial tract and the underlying bursa. It occurs particularly in long-distance runners and cyclists and is often associated with tightness of the iliotibial tract (Safran & Fu 1995). Pain is felt laterally, 2–3 cm proximal to the knee joint. Aggravating factors are downhill running and climbing stairs. Local anti-inflammatory modalities may be applied together with a change in training techniques. General principles of treatment may be applied.
Position the patient with the knee supported in extension. Palpate for the tender area of the bursa and mark a point for insertion. Insert the needle into the midpoint of the tender area and inject as a bolus. Injection of the superficial infrapatellar bursa is illustrated in Figure 11.46 and Figure 11.47, but the same principles can be applied to any bursa involved.
 |
| Figure 11.46
Injection of the superficial infrapatellar bursa.
|
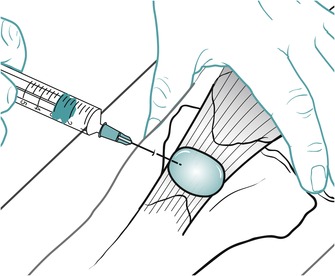 |
| Figure 11.47
Injection of the superficial infrapatellar bursa showing direction of approach and needle position.
|
CONTRACTILE LESIONS
Quadriceps
Direct trauma to the quadriceps muscle belly causes swelling and superficial bruising which eventually tracks down the leg. Known in sporting circles as ‘cork thigh’, it has the potential to develop myositis ossificans traumatica, particularly if the contusion is accompanied by persistent gross limitation of knee flexion (Norris 2004).
Transverse frictions to the quadriceps muscle belly
Position the patient in sitting with the knee straight to place the muscle belly in a shortened position. Locate the site of the lesion and, using the fingers, apply transverse frictions (Fig. 11.48). After the analgesic effect is achieved, apply six effective sweeps to the acute, irritable lesion and 10 min of deep transverse frictions for the chronic, non-irritable lesion, followed up by active Grade A exercises.
 |
| Figure 11.48
Transverse friction massage to the quadriceps muscle belly.
|
Tendinopathy of the medial and lateral quadriceps expansions
The patient usually presents with a gradual onset of pain felt locally at the front of the knee associated with overuse. On examination there is pain on resisted knee extension and tenderness located at the medial, lateral or both borders of the patella. Often the lesion lies at the ‘corners’ of the patella.
Transverse frictions to the quadriceps expansions (Cyriax 1984, Cyriax & Cyriax 1993)
Having established the site of the lesion, deep transverse frictions are applied to the chronic lesion. Position the patient comfortably with the knee supported and relaxed in extension. Push and hold the patella to one side. Use the middle finger reinforced by the index finger and rotate the forearm to direct the pressure up and under the edge of the patella (Figure 11.49 and Figure 11.50). Sweep transversely across the fibres in a superior–inferior direction and continue treatment for 10 min after the analgesic effect has been achieved. It may be necessary to treat several areas around the patella. Relative rest is advised where functional movements may continue, but no overuse or stretching until the structure is pain-free on resisted testing.
 |
| Figure 11.49
Transverse friction massage of the quadriceps expansions, medial.
|
 |
| Figure 11.50
Transverse friction massage of the quadriceps expansions, lateral.
|
Overuse lesions of the quadriceps expansions may be secondary to malalignment or abnormal tracking of the patella. Treatment may be incorporated into a regime of corrective taping and re-education of the oblique portion of vastus medialis.
Patellar tendinopathy
Patellar tendinopathy is a degenerative, not inflammatory, condition of the patellar tendon and is most likely to be the result of excessive load-bearing (Khan et al 2005). There are two sites for patellar tendinopathy:
• At the apex of the patella (infrapatellar tendon)
• At the base of the patella (suprapatellar tendon).
The most common is infrapatellar tendinopathy and it may be associated with repetitive jumping actions (‘jumper’s knee’). The repetitive overuse results in microfailure and fraying of the tendon fibres and areas of focal degeneration (Curwin & Stanish 1984).
The symptoms and signs are similar to those described for tendinopathy of the quadriceps expansions, but the site of the lesion will be located to either the infra- or suprapatellar tendons. Treatment may be deep transverse frictions or corticosteroid injection followed by relative rest. Infrapatellar fat pad inflammation (Hoffa’s disease) produces symptoms that mimic infrapatellar tendinopathy, but pain is produced by gentle squeezing of the fat pad at either side of the lower patella (Curwin & Stanish 1984).
Transverse frictions to the infrapatellar and suprapatellar tendons; teno-osseous junctions (Cyriax 1984, Cyriax & Cyriax 1993)
Position the patient comfortably with the knee relaxed and supported in extension. Apply the web space between your index finger and thumb of one hand to the base of the patella, tilting the apex. Using the middle finger of the other hand reinforced by the index, supinate the forearm to direct the pressure up under the apex of the patella and sweep transversely across the fibres of the infrapatellar tendon (Fig. 11.51). The lesion may be found slightly to either side of the apex. If so, after tilting the patella, angle the finger to friction in line with the edge of the patella. Ten minutes’ transverse frictions are applied after the analgesic effect is achieved. Relative rest is advised where functional movements may continue, but no overuse or stretching until the structure is pain-free on resisted testing.
 |
| Figure 11.51
Transverse friction massage of the infrapatellar tendon, teno-osseous junction.
|
Position the patient as described for the transverse frictions technique, applying pressure to the base of the patella with your stabilizing hand, to make the apex accessible (Fig. 11.52). Insert the needle just distal to the apex of the patella and advance until contact is made with bone. Deliver the injection by a peppering technique, fanning out to deposit two parallel rows of droplets of corticosteroid across the full width of the teno-osseous junction (Fig. 11.53). Note that the injection is delivered at the teno-osseous junction at the tendon–bone interface and not the body of the tendon, which is contraindicated. The patient is advised to maintain a period of relative rest for approximately 2 weeks following injection.
 |
| Figure 11.52
Injection of the infrapatellar tendon, teno-osseous junction.
|
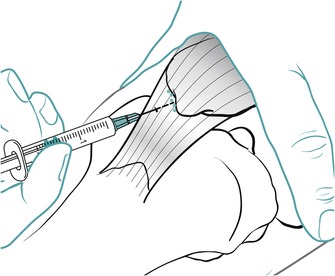 |
| Figure 11.53
Injection of the infrapatellar tendon, teno-osseous junction, showing direction of approach and needle position.
|
For treatment of suprapatellar tendinopathy, the above principles are applied with the base of the patella tilted upwards (Figure 11.54, Figure 11.55 and Figure 11.56).
 |
| Figure 11.54
Transverse friction massage of the suprapatellar tendon, teno-osseous junction.
|
 |
| Figure 11.55
Injection of the suprapatellar tendon, teno-osseous junction.
|
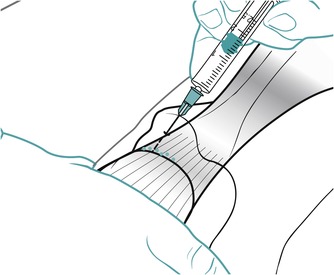 |
| Figure 11.56
Injection of the suprapatellar tendon, teno-osseous junction, showing direction of approach and needle position.
|
Selfe et al (2008) note that evidence that patellar taping is effective at relieving patellofemoral pain is emerging from the literature. The mechanical effects of taping are still under debate but there may be a role for taping in the management of patellar tendinopathy. Brukner & Khan (2007) summarize studies documenting the effectiveness of strengthening exercises on patellar tendinopathy. Exercise-based interventions including squatting, isokinetics and weights apparently reduced pain in three studies. More recently the focus has been on the role of eccentric training programmes with the use of a 25° decline board specifically to load the extensor mechanism of the knee. Studies have suggested that this too can reduce pain. A progressive strengthening programme is appropriate, with the next stage being approached when the previous workload is managed easily, the pain remains under control and the improvement in function is satisfactory (Brukner & Khan 2007).
Tendinopathy of the insertions of the hamstring muscles
The patient presents with pain localized to the posterior aspect of the knee following a history of overuse. Pain is reproduced by resisted knee flexion and the site of tenderness is located medially or laterally according to the tendons involved. Principles of treatment can be applied using either deep transverse frictions or corticosteroid injection to the teno-osseous insertions via a peppering technique. Relative rest is advised where functional movements may continue, but no overuse or stretching until the structure is pain-free on resisted testing.
Lesions of the hamstrings muscle belly and the tendon of origin are discussed in Chapter 10. Lesions of gastrocnemius are discussed in Chapter 12.
REFERENCES
Adler, G.G.; Hoekman, R.A.; Beach, D.M., Drop leg Lachman test, Am. J. Sports Med. 23 (1995) 320–323.
Amiel, D.; Kuiper, S.; Akeson, W.H., Cruciate ligaments, In: (Editors: Daniel, D.; Akeson, W.H.; O’Connor, J.J.) Knee Ligaments: Structure, Function, Injury and Repair ( 1990)Lippincott, Williams & Wilkins, Philadelphia, pp. 365–376.
Azar, F., Evaluation and treatment of chronic medial collateral ligament injuries of the knee., Sports Med. Arthroscopy Rev. 14 (2) ( 2006) 84–90.
Baker, C.L., Acute haemarthrosis of the knee, J. Med. Assoc. Ga. 81 (6) ( 1992) 301–305.
Baker, K.R.; Nelson, M.E.; Felson, D.T.; et al., The efficacy of home based progressive strength training in older adults with knee osteoarthritis: a randomised controlled trial, J. Rheumatol. 28 (7) ( 2001) 1655–1665.
Barrack, R.L.; Skinner, H.B., The sensory function of knee ligaments, In: (Editors: Daniel, D.; Akeson, W.H.; O’Connor, J.J.) Knee Ligaments: Structure, Function, Injury and Repair ( 1990)Lippincott, Williams & Wilkins, Philadelphia, pp. 95–112.
Bessette, G.C., The meniscus, Orthopaedics 15 (1992) 35–42.
Bianchi, S.; Martinoli, C., Detection of loose bodies in joints, Radiol. Clin. N. Am. 37 (4) ( 1999) 679–690.
Bijl, D.; van Baar, M.E.; Oostendorp, R.A.B.; et al., Validity of Cyriax’ concept of capsular pattern for the diagnosis of osteoarthritis of hip and/or knee, Scand. J. Rheumatol. 27 (1998) 347–351.
Bikkina, R.; Tujo, C.; Schraner, A.; et al., The “floating” meniscus: MRI in knee trauma and implications for surgery, Am. J. Roentgenol. 184 (2005) 200–204.
Boles, C.A.; Martin, D.F., Synovial plicae in the knee, Am. J. Roentgenol. 177 (2001) 221–227.
Bongers, E.; van Kampen, A.; van Bokhoven, H.; et al., Human syndromes with congenital anomalies and the underlying defects, Clin. Genet. 68 (4) ( 2005) 302–319.
Bowditch, M., Anterior cruciate ligament rupture and management, Trauma 3 (4) ( 2001) 246–261.
Bozkurt, M.; Yilmaz, E.; Atlihan, D.; et al., The proximal tibiofibular joint, Clin. Orthop. Relat. Res. 406 (2003) 136–140.
Brotzman, S.B.; Wilk, K.E., Clinical Orthopaedic Rehabilitation. 2nd edn ( 2003)Mosby, Edinburgh.
Brukner, P.; Khan, K., Clinical Sports Medicine. 3rd edn ( 2007)McGraw-Hill, Sydney.
Burks, R.T., Gross anatomy, In: (Editors: Daniel, D.; Akeson, W.H.; O’Connor, J.J.) Knee Ligaments: Structure, Function, Injury and Repair ( 1990)Lippincott, Williams & Wilkins, Philadelphia, pp. 59–75.
Butler, D.L.; Noyes, F.R.; Grood, E.S., Ligamentous restraints to anterior–posterior drawer in the human knee, J. Bone Joint Surg. 62A (1980) 259–270.
Cailliet, R., Knee Pain and Disability. 3rd edn ( 1992)F A Davis, Philadelphia.
Cameron, G., Steroid arthropathy – myth or reality?J. Orthop. Med. 17 (1995) 51–55.
Chakravarty, K.; Pharoah, P.D., A randomized controlled study of post-injection rest following intra-articular steroid therapy for knee synovitis, Br. J. Rheumatol. 33 (5) ( 1994) 464–468.
Conaghan, P.G.; Dickson, J.; Grant, R.L., Care and management of osteoarthritis in adults: summary of NICE guidance. Guideline Development Group, Br. Med. J. 336 (7642) ( 2008) 502–503.
Curtin, W.; O’Farrell, D.; McGoldrick, F.; et al., The correlation between clinical diagnosis of knee pathology and findings in arthroscopy, Irish J. Med. Sci. 161 (1992) 135–136.
Curwin, S.; Stanish, W.D., Jumper’s Knee, Tendinitis – Its Etiology and Treatment. ( 1984)Collamore Press, Massachusetts.
Cyriax, J., 8th ednTextbook of Orthopaedic Medicine. Vol. 1 ( 1982)Baillière Tindall, London.
Cyriax, J., 11th ednTextbook of Orthopaedic Medicine. Vol. 2 ( 1984)Baillière Tindall, London.
Cyriax, J.; Cyriax, P., Cyriax’s Illustrated Manual of Orthopaedic Medicine. ( 1993)Butterworth Heinemann, Oxford.
Daniel, D.M., Diagnosis of a ligament injury, In: (Editors: Daniel, D.; Akeson, W.H.; O’Connor, J.J.) Knee Ligaments: Structure, Function, Injury and Repair ( 1990)Lippincott, Williams & Wilkins, Philadelphia, pp. 3–10.
Edwards, D.; Villar, R., Anterior cruciate ligament injury, Practitioner 237 (1993) 113–117.
El-Dieb, A.; Yu, J.S.; Huang, G.-S.; et al., Pathologic conditions of the ligaments and tendons of the knee, Radiol. Clin. N. Am. 40 (2002) 1061–1079.
Evans, P., The Knee Joint. ( 1986)Churchill Livingstone, Edinburgh.
Felson, D.T.; Chaisson, C., Understanding the relationship between body weight and osteoarthritis., Baillières Clin. Rheumatol. 11 (4) ( 1997) 671–681.
Felson, D.T.; Anderson, J.J.; Naimark, A.; et al., Obesity and knee osteoarthritis, Ann. Intern. Med. 109 (1) ( 1988) 18–24.
Fritz, J.M.; Delitto, A.; Efhard, R.E.; et al., An examination of the selective tissue tension scheme with evidence for the concept of the capsular pattern of the knee, Phys. Ther. 78 (10) ( 1998) 1046–1056.
Greenhill, B.J., The importance of the medial quadriceps expansion in medial ligament injury, Can. J. Surg. 10 (3) ( 1967) 312–317.
Greis, P.E.; Bardana, D.D.; Holmstrom, M.C.; et al., Meniscal injury, I. Basic science and evaluation, J. Am. Acad. Orthop. Surg. 10 (3) ( 2002) 168–176.
Hartley, A., Practical Joint Assessment – Lower Quadrant. 2nd edn ( 1995)Mosby, London.
Hattam, P.; Smeatham, A., Special Tests in Musculoskeletal Examination. ( 2010)Churchill Livingstone, Edinburgh.
Hill, C.L.; Gale, D.G.; Chaisson, C.R.; et al., Knee effusions, popliteal cysts and synovial thickening: Association with knee pain., J. Rheumatol. 28 (6) ( 2001) 1330–1337.
Horne, G.; Devane, P.; Davidson, A.; et al., The influence of steroid injections on the incidence of infection following total knee arthroplasty, NZ Med. J. 121 (1268) ( 2008) 1–11.
Jacobson, J.A.; Lenchik, L.; Ruhoy, M.K.; et al., MR imaging of the infrapatellar fat pad of Hoffa, Radiographics 17 (3) ( 1997) 675–691.
Kapandji, I.A., 5th ednThe Physiology of the Joints: Lower Limb. Vol. 2 ( 1987)Churchill Livingstone, Edinburgh.
Kaspar, S.; de Van de Beer, J., Infection in hip arthroplasty after previous injection of steroid, J. Bone Joint Surg. 87-B (2005) 454–457.
Katz, J.W.; Fingeroth, R.J., The diagnostic accuracy of ruptures of the anterior cruciate ligament comparing the Lachman test, the anterior drawer sign, and the pivot shift test in acute and chronic knee injuries, Am. J. Sports Med. 14 (1986) 88–91.
Kesson, M.; Atkins, A.; Davies, I., Musculoskeletal Injection Skills. ( 2003)Butterworth Heinemann, Oxford.
Khan, K.M.; Cook, J.L.; Maffulli, N., Patellar tendinopathy and patellar tendon rupture, In: (Editors: Maffulli, N.; Renström, P.; Leadbetter, W.B.) Tendon Injuries: Basic Science and Clinical Medicine ( 2005)Springer-Verlag, London, pp. 166–177.
LaPrade, R.F., The anatomy of the deep infrapatellar bursa of the knee, Am. J. Sports Med. 26 (1) ( 1998) 129–132.
Llopis, E.; Padrón, M., Anterior knee pain, Eur. J. Radiol. 62 (1) ( 2007) 27–43.
Malanga, G.A.; Andrus, S.; Nadler, S.F.; et al., Physical examination of the knee: a review of the original test description and scientific validity of common orthopaedic tests, Arch. Phys. Med. Rehabil. 84 (2003) 592–603.
Mitsou, A.; Vallianatos, P., Clinical diagnosis of ruptures of the anterior cruciate ligament: a comparison between the Lachman test and anterior draw sign, Injury 19 (6) ( 1988) 427–428.
Mohan, B.; Gosal, H., Reliability of clinical diagnosis in meniscal tears, Int. Orthop. 31 (2007) 57–60.
Nakamura, N.; Shino, K., The clinical problems of ligament healing of the knee, Sports Med. Arthroscopic Rev. 13 (3) ( 2005) 118–126.
Nordin, M.; Frankel, V.H., Basic Biomechanics of The Musculoskeletal System. 3rd edn ( 2001)Lippincott, Williams & Wilkins, Philadelphia.
Norris, C.M., Sports Injuries: Diagnosis and Management for Physiotherapists. 3rd edn ( 2004)Butterworth Heinemann, Oxford.
Palastanga, N.; Field, D.; Soames, R., Anatomy and Human Movement. 5th edn ( 2006)Butterworth-Heinemann, Edinburgh.
Parikh, J.R.; Houpt, J.B.; Jacobs, S.; et al., Charcot’s arthropathy of the shoulder following intra-articular corticosteroid injections, J. Rheumatol. 20 (1993) 885–887.
Perko, M.M.J.; Cross, M.J.; Ruske, D.; et al., Anterior cruciate ligament injuries, clues for diagnosis, Med. J. Aust. 157 (1992) 467–470.
Pope, T.L.; Winston-Salem, N.C., MR imaging of the knee ligaments, J. South. Orthop. Assoc. 5 (1) ( 1996) 46–62.
Raynauld, J.-P.; Buckland-Wright, C.; Ward, R.; et al., Safety and efficacy of long-term intraarticular steroid injection in osteoarthritis of the knee, Arthritis Rheum. 48 (2) ( 2003) 370–377.
Rubinstein, R.A.; Shelbourne, K.D.; McCarroll, J.R.; et al., The accuracy of the clinical examination in the setting of posterior cruciate ligament injuries, Am. J. Sports Med. 22 (1994) 550–557.
Safran, M.R.; Fu, F.H., Uncommon causes of knee pain in the athlete, Orthop. Clin. N. Am. 26 (1995) 547–559.
Saotome K, Tamai K, Osada D, et al, 2006. Histologic classification of loose bodies in osteoarthrosis. J. orhtop. Sci. 11 (6), 607–613.
Saunders, S., Orthopaedic Medicine Course Manual. ( 2000)Saunders, London.
Schenck, R.C.; Heckman, J.D., Injuries of the knee, Clin. Symp. 45 (1993) 2–32.
Schweitzer, M.E.; Tran, D.; Deely, D.M.; et al., Medial collateral ligament injuries: evaluation of multiple signs, prevalence and location of associated bone bruises, and assessment with MR imaging, Radiology 194 (3) ( 1995) 825–829.
Selfe, J.; Richards, J.; Thewlis, D.; et al., The biomechanics of step descent under different treatment modalities used in patellofemoral pain, Gait Posture 27 (2) ( 2008) 258–263.
Shaerf, D.; Banerjee, A., Assessment and management of post-traumatic haemarthrosis of the knee, Br. J. Hosp. Med. 69 (8) ( 2008) 459–460; 462–463.
Smith, B.W.; Green, G.A., Acute knee injuries: Part I. History and physical examination, Am. Fam. Phys. 51 (1995) 615–621.
Staron, R.B.; Haramati, N.; Feldman, F.; et al., O’Donaghue’s triad: magnetic resonance imaging evidence, Skeletol Radiol. 23 (1994) 633–636.
Torg, J.S.; Conrad, W.; Kalen, V., Clinical diagnosis of anterior cruciate ligament instability in the athlete, Am. J. Sports Med. 4 (1974) 84–93.
Valley, V.T.; Shermer, C.D., Use of musculoskeletal ultrasonography in the diagnosis of pes anserine tendinopathy: a case report, J. Emerg. Med. 20 (1) ( 2000) 43–45.
Wallman, P.; Carley, S., Aspiration of acute traumatic knee haemarthrosis, Emerg. Med. J. 19 (1) ( 2002) 50.
Wang, J.C.; Shapiro, M.S., Pellegrini–Steida syndrome, Am. J. Orthop. 24 (6) ( 1995) 493–497.
Woo, S.L.-Y.; Wang, C.; Newton, P.O.; et al., The response of ligaments to stress deprivation and stress enhancement, In: (Editors: Daniel, D.; Akeson, W.H.; O’Connor, J.J.) Knee Ligaments: Structure, Function, Injury and Repair ( 1990)Lippincott, Williams & Wilkins, Philadelphia, pp. 337–350.