Chapter 1
The Interviewer’s Questions
What is spoken of as a “clinical picture” is not just a photograph of a man sick in bed; it is an impressionistic painting of the patient surrounded by his home, his work, his relations, his friends, his joys, sorrows, hopes and fears.
Francis Weld Peabody (1881–1927)
Basic Principles
Good communication skills are the foundation of excellent medical care. Even with the exciting new technology that has appeared since 2000, communicative behavior is still paramount in the care of patients. Studies have shown that good communication improves health outcomes by resolving symptoms and reducing patients’ psychological distress and anxiety. In the United States, 85% of all malpractice law suits are based on poor communication skills. It is not that the doctor didn’t know enough; the doctor did not communicate well enough with the patient!
Technologic medicine cannot substitute for words and behavior in serving the ill. The quality of patient care depends greatly on the skills of interviewing, because the relationship that a patient has with a physician is one of the most extraordinary relationships between two human beings. Within a matter of minutes, two strangers—the patient and the healer—begin to discuss intimate details about a person’s life. Once trust is established, the patient feels at ease discussing the most personal details of the illness. Clearly, a strong bond, a therapeutic alliance, has to have been established.
The main purpose of an interview is to gather all basic information pertinent to the patient’s illness and the patient’s adaptation to illness. An assessment of the patient’s condition can then be made. An experienced interviewer considers all the aspects of the patient’s presentation and then follows the leads that appear to merit the most attention. The interviewer should also be aware of the influence of social, economic, and cultural factors in shaping the nature of the patient’s problems. Other important aspects of the interview are educating the patient about the diagnosis, negotiating a management plan, and counseling about behavioral changes.
Any patient who seeks consultation from a clinician needs to be evaluated in the broadest sense. The clinician must be keenly aware of all clues, obvious or subtle. Although body language is important, the spoken word remains the central diagnostic tool in medicine. For this reason, the art of speaking and active listening continues to be central to the doctor-patient interaction. Active listening takes practice and involves awareness of what is being said in addition to body language and other nonverbal clues. For the novice interviewer, it is very easy to think only about your next question without observing the entire picture of the patient, as described masterfully in the quote by Peabody that introduced this chapter. Once all the clues from the history have been gathered, the assimilation of those clues into an ultimate diagnosis is relatively easy.
Communication is the key to a successful interview. The interviewer must be able to ask questions of the patient freely. These questions must always be understood easily and adjusted to the medical sophistication of the patient. If necessary, slang words describing certain conditions may be used to facilitate communication and avoid misunderstanding.
The success of any interview depends on its being patient-centered and not doctor-centered. Encourage the patient to tell his or her story and follow the patient’s leads to better comprehend the problems, concerns, and requests. Do not have your own list of “standard questions” as would occur in a symptom-focused, doctor-centered interview. Patients are not standard; don’t treat them as such. Allow the patient to tell his or her story in his or her own words. In the words of Sir William Osler (1893), “Listen to your patient. He is telling you the diagnosis. . . . The good physician treats the disease; the great physician treats the patient who has the disease.” No truer words have been spoken.
Once the patient has told his or her story of the history of the present illness, it is customary for you to move from open-ended questions to direct, more focused questions. Always start by casting a wide net and then gradually close the net to develop your differential diagnosis. Start general and then get more specific to clarify the patient’s story and symptoms.
Using an Interpreter
Health care providers are increasingly treating patients across language barriers. In 2006, nearly 49.6 million Americans had a “mother tongue” other than English; an additional 22.3 million (8.4%) had limited English proficiency. Lack of English proficiency can have deleterious effects. For any patient who speaks a language other than that of the health care provider, it is important to seek the help of a trained medical interpreter. Unless fluent in the patient’s language and culture, the health care provider should always use an interpreter. The interpreter can be thought of as a bridge, spanning the ideas, mores, biases, emotions, and problems of the clinician and patient. The communication is very much influenced by the extent to which the patient, the interpreter, and the provider share the same understanding and beliefs regarding the patient’s problem. The best interpreters are those who are familiar with the patient’s culture. The interpreter’s presence, however, adds another variable in the doctor-patient relationship; for example, a family member who translates for the patient may alter the meaning of what has been said. When a family member is the interpreter, the patient may be reluctant to provide information about sensitive issues, such as sexual history or substance abuse. It is therefore advantageous to have a disinterested observer act as interpreter. On occasion, the patient may request that a family member be the interpreter. In such a case, clinicians should respect the patient’s wishes. Friends of the patient, although helpful in times of emergency, should not be relied on as translators because their skills are unknown and confidentiality is a concern. The clinician should also master a number of key words and phrases in several common languages to gain the respect and confidence of patients. When using an interpreter, clinicians should remember the following guidelines:
1. Choose an individual trained in medical terminology.
2. Choose a person of the same sex as the patient and of comparable age.
3. Talk with the interpreter beforehand to establish an approach.
4. When speaking to the patient, watch the patient, not the interpreter.
5. Do not expect a word-for-word translation.
6. Ask the interpreter about the patient’s fears and expectations.
7. Use clear, short, and simple questions.
9. Keep your explanations brief.
10. Avoid questions using if, would, and could, because these require nuances of language.
The U.S. Department of Health and Human Services has put together a useful mnemonic (INTERPRET) for working with interpreters in a cultural setting:
Even with a trained translator, health care workers are ultimately responsible for ensuring safe and effective communication with their patients. A recent article (Schenker et al., 2008) describes a conceptual framework of when to call for an interpreter and what to do when one is not available.
When speaking with the patient, the interviewer must determine not only the main medical problems but also the patient’s reaction to the illness. This is of great importance. How has the illness affected the patient? How has he or she reacted to it? What influence has it had on the family? On work? On social life?
The best interview is conducted by an interviewer who is cheerful, friendly, and genuinely concerned about the patient. This type of approach is clearly better than that of the interviewer who acts like an interrogator shooting questions from a standard list at the poor, defenseless patient. Bombarding patients with rapid-fire questions is a technique that should not be used.
Important Interviewing Concepts
In the beginning, the patient brings up the subjects that are easiest to discuss. More painful experiences can be elicited by tactful questioning. The novice interviewer needs to gain experience to feel comfortable asking questions about subjects that are more painful, delicate, or unpleasant. Timing of such questions is critical.
A cardinal principle of interviewing is to permit patients to express their stories in their own words. The manner in which patients tell their stories reveals much about the nature of their illnesses. Careful observation of a patient’s facial expressions, as well as body movements, may provide valuable nonverbal clues. The interviewer may also use body language such as a smile, nod, silence, hand gesture, or questioning look to encourage the patient to continue the story.
Listening without interruption is important and requires skill. If given the chance, patients often disclose their problems spontaneously. Interviewers need to hear what is being said. They must allow the patient to finish his or her answer even if there are pauses while the patient processes his or her feelings. All too often, an interview may fail to reveal all the clues because the interviewer did not listen adequately to the patient. Several studies have shown that clinicians commonly do not listen adequately to their patients. One study showed that clinicians interrupt the patient within the first 15 seconds of the interview. The interviewers are abrupt, appear uninterested in the patient’s distress, and are prone to control the interview.
As mentioned earlier, the best clinical interview focuses on the patient, not on the clinician’s agenda.
An important rule for improved interviewing is to listen more, talk less, and interrupt infrequently. Interrupting disrupts the patient’s train of thought. Allow the patient, at least in part, to control the interview.
Interviewers should be attentive to how patients use their words to conceal or reveal their thoughts and history. Interviewers should be wary of quick, very positive statements such as, “Everything’s fine,” “I’m very happy,” or “No problems.” If interviewers have reason to doubt these statements, they may respond by saying, “Is everything really as fine as it could be?”
If the history given is vague, the interviewer may use direct questioning. Asking “how,” “where,” or “when” is generally more effective than asking “why,” which tends to put patients on the defensive. Often replacing the word “Why . . .” with “What’s the reason . . .” will allow for better, less confrontational dialogue. The interviewer must be particularly careful not to disapprove of certain aspects of the patient’s story. Different cultures have different mores, and the interviewer must listen without any suggestion of prejudice.
Always treat the patient with respect. Do not contradict or impose your own moral standards on the patient. Knowledge of the patient’s social and economic background will make the interview progress more smoothly. Respect all patients regardless of their age, gender, beliefs, intelligence, educational background, legal status, practices, culture, illness, body habitus, emotional condition, or economic state.
Clinicians must be compassionate and interested in the patient’s story. They must create an atmosphere of openness in which the patient feels comfortable and is encouraged to describe the problem. These guidelines set the foundation for effective interviewing.
The interviewer’s appearance can influence the success of the interview. Patients have an image of clinicians. Neatness counts; a slovenly interviewer might be considered immature or careless, and his or her competence may be questioned from the start. Surveys of patients indicate that patients prefer medical personnel to dress in white coats and to wear shoes instead of sneakers.
As a rule, patients like to respond to questions in a way that satisfies the clinician to gain his or her approval. This may represent fear on the part of patients. The clinician should be aware of this phenomenon.
The interviewer must be able to question patients about subjects that may be distressing or embarrassing to the interviewer, the patient, or both. Answers to many routine questions may cause embarrassment to interviewers and leave them speechless. Therefore there is a tendency to avoid such questions. The interviewer’s ability to be open and frank about such topics promotes the likelihood of discussion in those areas.
Very often, patients feel comfortable discussing what an interviewer might consider antisocial behavior. This may include drug addiction, unlawful actions, or sexual behavior that does not conform to societal norms. Interviewers must be careful not to pass judgment on such behavior. Should an interviewer pass judgment, the patient may reject him or her as an unsuitable listener. Acceptance, however, indicates to the patient that the interviewer is sensitive. It is important not to imply approval of behavior; this may reinforce behavior that is actually destructive.
Follow the “rule of five vowels” when conducting an interview. According to this rule, a good interview contains the elements of audition, evaluation, inquiry, observation, and understanding. Audition reminds the interviewer to listen carefully to the patient’s story. Evaluation refers to sorting out relevant from irrelevant data and to the importance of the data. Inquiry leads the interviewer to probe into significant areas in which more clarification is required. Observation refers to the importance of nonverbal communication, regardless of what is said. Understanding the patient’s concerns and apprehensions enables the interviewer to play a more empathetic role.
Speech Patterns
Speech patterns, referred to as paralanguage components, are relevant to the interview. By manipulating the intonation, rate, emphasis, and volume of speech, both the interviewer and the patient can convey significant emotional meaning through their dialogue. By controlling intonation, the interviewer or patient can change the entire meaning of words. Because many of these features are not under conscious control, they may provide an important statement about the patient’s personal attributes. These audible parameters are useful in detecting a patient’s anxiety or depression, as well as other affective and emotional states. The interviewer’s use of a warm, soft tone is soothing to the patient and enhances the communication.
Body Language
A broad interest in body language has evolved. Body language, technically known as kinesics, is a significant aspect of modern communications and relationships. This type of nonverbal communication, in association with spoken language, can provide a more comprehensive picture of the patient’s behavior. Your own body language reveals your feelings and meanings to others. Your patient’s body language reveals his or her feelings and meanings to you. The sending and receiving of body language signals happens on conscious and unconscious levels.
It is well known that the interviewer may learn more about the patient from the way the patient tells the story than from the story itself. A patient who moves about in a chair and looks embarrassed is uncomfortable. A frown indicates annoyance or disapproval. Lack of comprehension is indicated by knitted brows. Body language experts generally agree that hands send more signals than any part of the body except for the face. A patient who strikes a fist on a table while talking is dramatically emphasizing what he or she is saying. A patient who slips a wedding band on and off may be ambivalent about his or her marriage. A palm placed over the heart asserts sincerity or credibility. Many people rub or cover their eyes when they refuse to accept something that is pointed out. When patients disapprove of a statement made by the interviewer but restrain themselves from speaking, they may start to remove dust or lint from their clothing.
Six universal emotional facial expressions are recognized around the world. The use and recognition of these expressions is genetically inherited rather than socially conditioned or learned. Although minor variations and differences are found among isolated people, the following basic human emotions are generally used, recognized, and part of humankind’s genetic character:
Of interest, Charles Darwin was first to make these claims in his book The Expressions of the Emotions in Man and Animals, published in 1872.
Smiling is an important part of body language. As a general rule, a genuine smile is symmetrical and produces creases around the eyes and mouth, whereas a fake smile tends to be a mouth-only gesture.
Arms act as defensive barriers when across the body, and conversely indicate feelings of openness and security when in open positions, especially combined with open palms. Arms are quite reliable indicators of mood and feeling, especially when interpreted with other body language. For example:
• Crossed arms may indicate defensiveness.
• Crossed arms and crossed legs probably indicate defensiveness.
Full interpretation of body language can be made only in the context of the patient’s cultural and ethnic background because different cultures have different standards for nonverbal behavior. Middle Eastern and Asian patients often speak with dropped eyelids. This type of body language indicates depression or lack of attentiveness in a patient from the United States. The interviewer may use facial expressions to facilitate the interview. An appearance of attention demonstrates an interest in what the patient is describing. Attentiveness on the part of the interviewer is also indicated by leaning slightly forward toward the patient.
Body language in a certain situation might not mean the same in another. Occasionally, body language isn’t what it seems. For example:
• Someone rubbing his or her eye might have an irritation, rather than being disbelieving or upset.
• Someone with crossed arms might be keeping warm, rather than being defensive.
• Someone scratching his or her nose might actually have an itch, rather than concealing a lie.
A single body language signal isn’t as reliable as several signals. As with any system of evidence, groups of body language signals provide much more reliable indication of meaning than one or two signals in isolation. Avoid interpreting only single signals. Look for combinations of signals that support an overall conclusion, especially for signals that can mean two or more quite different things. It is important to recognize that body language is not an exact science.
Touch
Touching the patient can also be very useful. Touch can communicate warmth, affection, caring, and understanding. Many factors, including gender and cultural background, as well as the location of the touch, influence the response to the touch. Although there are wide variations within each cultural group, Latinos and people of Mediterranean descent tend to use a great deal of contact, whereas British and Asians tend not to use contact. Scandinavians and Anglo-Saxon Americans are in the middle of this range. Be aware, however, that certain religious groups prohibit touching a person of the opposite sex. In general, the older the patient, the more important touch is. Appropriate placement of a hand on a patient’s shoulder suggests support. Never place a hand on a patient’s leg or thigh, because this is a threatening touch. An interviewer who walks with good posture to a patient’s bedside can hope to gain the patient’s respect and confidence. An interviewer who maintains eye contact with the patient conveys interest in the patient.
Depersonalization of the Doctor-Patient Relationship
In this age of biomedical advancements, a new problem has arisen: a depersonalization of the doctor-patient relationship. Clinicians may order computed tomography scans or sonograms without taking the appropriate time to speak with the patient about the tests. Both doctor and patient may feel increasingly neglected, rejected, or abused. Patients may feel dehumanized on admission to the hospital. Many find themselves in a strange environment, lying naked while clothed people march in and out of the room and touch them, tell them what to do, and so forth. They may be apprehensive because they have a problem that their health care provider considers too serious to be treated on an outpatient basis. Their future is filled with uncertainty. A patient admitted to the hospital is stripped of clothing and often of dentures, glasses, hearing aids, and other personal belongings. A name tag is placed on the patient’s wrist, and he or she becomes “the patient in 9W-310.” This lowers the morale of the patient even more. At the same time, clinicians may be pressed for time, overworked, and sometimes unable to cope with everyday pressures. They may be irritable and pay inadequate attention to the patient’s story. They may eventually come to rely on the technical results and reports. This failure to communicate weakens the doctor-patient relationship.
Inexperienced interviewers not only must learn about the patient’s problems but also must gain insight into their own feelings, attitudes, and vulnerabilities. Such introspection enhances the self-image of the interviewer and results in the interviewer’s being perceived by the patient as a more careful and compassionate human being to whom the patient can turn in a time of crisis.
A good interviewing session determines what the patients comprehend about their own health problems. What do the patients think is wrong with them? Do not accept merely the diagnosis. Inquire specifically as to what the patient thinks is happening. What kind of effect does the illness have on the patient’s work, family, or financial situation? Is there a feeling of loss of control? Does the patient feel guilt about the illness? Does the patient think that he or she will die? By pondering these questions, you can learn much about patients, and patients will realize that you are interested in them as whole persons, not merely as statistics among the hospital admissions.
Medical Malpractice and Communication Skills
The literature indicates that malpractice suits have increased at an alarming rate. A good doctor-patient relationship is probably the most important factor in avoiding malpractice claims. As mentioned previously, most malpractice litigation is the result of a deterioration in communication and of patient dissatisfaction rather than of true medical negligence. The patient who is likely to sue has become dissatisfied with the clinician and may have lost respect for him or her. From the patient’s point of view, the most serious barriers to a good relationship are the clinician’s lack of time; seeming lack of concern for the patient’s problem; inability to be reached; attitude of superiority, arrogance, or indifference; and failure to inform the patient adequately about his or her illness. Failure to discuss the patient’s illness and treatment in understandable terms is viewed as a rejection by the patient. In addition, the congeniality and competence of a physician’s office staff can go a long way toward avoiding malpractice suits. Physicians who have never been sued orient their patients to the process of the visit, use facilitative comments, ask the patient for opinions, use active learning, use humor and laughter, and have longer visits. A doctor-patient relationship based on honesty and understanding is thus recognized as essential for good medical practice and the well-being of the patient.
It is sometimes difficult for a novice interviewer to remember that there is no need to try to make a diagnosis out of every bit of information obtained from the interview. Accept all the clues and then work with them later when trying to establish a diagnosis.
If during the interview you cannot answer a question, do not. You can always act as the patient’s advocate; listen to the question and then find someone who can provide an appropriate answer.
Doctor-Patient Engagement
A very important task of communication is to engage the patient. A helpful way of building rapport with a patient is to be curious about the person as a whole. Ask, “Before we begin, tell me something about yourself.” When the patient returns, mention something personal that you learned from a previous visit, for instance, “How was your trip to Seattle to see your son?” Another part of engagement is to determine the patient’s expectations from the visit; for instance, ask, “What are you hoping to accomplish today?” At the conclusion of the visit, ask, “Is there anything else you are concerned about?” If the patient has several problems, it is acceptable to say, “We might need to discuss that problem at another visit. I want to be certain that we completely evaluate your main concern today.”
Privacy Standards
On April 14, 2003, the first federal privacy standards were put in place to protect the medical records and other health information of patients. The U.S. Congress asked the Department of Health and Human Services to issue privacy protection as part of the Health Insurance Portability and Accountability Act (HIPAA) of 1996. HIPAA regulations include provisions designed to encourage electronic transactions and to safeguard the security and confidentiality of health information. The final regulations cover health plans, health care clearinghouses, and health care providers who conduct financial and administrative transactions electronically. In short, these regulations regarding patient confidentiality limit the ways in which health care providers, health plans, pharmacies, hospitals, clinics, and other entities can use patients’ personal medical information. These regulations ensure that medical records and other identifiable health information, whether on paper, in computers, or orally communicated, are protected.
In summary, the medical interview is a blend of the cognitive and technical skills of the interviewer and the feelings and personalities of both the patient and the interviewer. The interview should be flexible and spontaneous and not interrogative. When used correctly, it is a powerful diagnostic tool.
Symptoms and Signs
The clinician must be able to elicit descriptions of, and recognize, a wide variety of symptoms and signs. Symptom refers to what the patient feels. Symptoms are described by the patient to clarify the nature of the illness. Shortness of breath, chest pain, nausea, diarrhea, and double vision are all symptoms. These labels help the patient describe the discomfort or distress that he or she is experiencing. Symptoms are not absolute; they are influenced by culture, intelligence, and socioeconomic background. As an example, consider the symptom of pain. Patients have different thresholds of pain. This is discussed further in Chapter 27, Caring for Patients in a Culturally Diverse Society, which can be accessed on the internet version of this textbook.
Constitutional symptoms are symptoms that commonly occur with problems in any of the body systems, such as fever, chills, weight loss, or excessive sweating.
A sign is what the examiner finds. Signs can be observed and quantified. Certain signs are also symptoms. For example, a patient may describe episodes of wheezing; this is a symptom. In addition, an examiner may hear wheezing during a patient’s physical examination; this is a sign.
The major task of the interviewer is to sort out the symptoms and signs associated with a specific illness. A major advantage that the seasoned interviewer has over the novice is a better understanding of the pathophysiologic processes of disease states. The novice operates under the limitation of not knowing all the signs and symptoms of the associated diseases. With experience and education, the novice will recognize the combination of symptoms and signs as they relate to the underlying illness. For any given disease, certain symptoms and signs tend to occur together. When there is only an isolated symptom, the interviewer must be careful in making a definitive assessment.
Conducting an Interview
Getting Started and Introduction
The diagnostic process begins at the first moment of meeting. You should be dressed appropriately, wearing a white coat with your name badge identifying you as a member of the health care team. Patients expect this standard of professional attire. Casual attire may signify condescension.
Introduce yourself, greet the patient by last name, make eye contact, shake hands firmly, and smile. You may wish to say something like
Alternatively, you may say,
or
The term student doctor should generally be avoided because patients may not actually understand this term; they may hear only the word doctor. The introduction also includes a statement of the purpose of the visit. The welcoming handshake can serve to relax the patient.
It is appropriate to address patients by their correct titles—“Mr.,” “Mrs.,” “Miss,” “Dr.,” “Ms.”—unless they are adolescents or younger. A formal address clarifies the professional nature of the interview. For a woman, the default always is “Ms.” unless you know positively that a woman wishes to be addressed as “Miss” or “Mrs.” Name substitutes such as “dear,” “honey,” or “grandpa” are not to be used. Also, avoid using “Sir” or “Ma’am.” “Ma’am” is mostly obsolete, with a few exceptions. It is commonly used to address any woman in the southern or southwestern areas of the United States. Use the patient’s name. If you are not sure about the pronunciation, ask the patient how to say his or her name correctly.
The patient may address an interviewer as Ms. Jones, for example, or might elect to use the interviewer’s first name. It is not correct for an interviewer to address the patient by his or her first name, because this changes the professional nature of this first meeting.
If the patient is having a meal, ask whether you can return when he or she has finished eating. If the patient is using a urinal or bedpan, allow privacy. Do not begin an interview in this setting. If the patient has a visitor, you may inquire whether the patient wishes the visitor to stay. Do not assume that the visitor is a family member. Allow the patient to introduce the person to you.
The interview can be helped or hindered by the physical setting in which the interview is conducted. If possible, the interview should take place in a quiet, well-lit room. Unfortunately, most hospital rooms do not afford such luxury. The teaching hospital with four patients in a room is rarely conducive to good human interactions. Therefore make the best of the existing environment. The curtains should be drawn around the patient’s bed to create privacy and minimize distractions. You may request that the volume of neighboring patients’ radios or televisions be turned down. Lights and window shades can be adjusted to eliminate excessive glare or shade. Arrange the patient’s bed light so that the patient does not feel as if he or she is under interrogation.
You should make the patient as comfortable as possible. If the patient’s eyeglasses, hearing aids, or dentures were removed, ask whether the patient would like to use them. It may be useful to use your stethoscope as a hearing aid for hearing-impaired patients. The ear tips are placed in the ears of the patient, and the diaphragm serves as a microphone. The patient may be in a chair or lying in bed. Allow the patient the choice of position. This makes the patient feel that you are interested and concerned, and it allows the patient some control over the interview. If the patient is in bed, it is a nice gesture to ask whether the pillows should be arranged to make him or her more comfortable before the interview begins.
To Stand or to Sit?
Normally, the interviewer and patient should be seated comfortably at the same level. Sometimes it is useful to have the patient sitting even higher than the interviewer to give the patient the visual advantage. In this position, the patient may find it easier to open up to questions. The interviewer should sit in a chair directly facing the patient to make good eye contact. Sitting on the bed is too familiar and not appropriate. It is generally preferred that the interviewer sit at a distance of about 3 to 4 feet from the patient. Distances greater than 5 feet are impersonal, and distances closer than 3 feet interfere with the patient’s “private space.” The interviewer should sit in a relaxed position without crossing arms across the chest. The crossed-arms position is not appropriate because this body language projects an attitude of superiority and may interfere with the progress of the interview.
If the patient is bedridden, raise the head of the bed, or ask the patient to sit so that your eyes and the patient’s eyes are at the same level. Avoid standing over the patient. Try to lower the bed rail so that it does not act as a barrier to communication, and remember to put it back up at the conclusion of the session.
Regardless of whether the patient is sitting in a chair or lying in bed, make sure that he or she is appropriately draped with a sheet or robe.
The Opening Statement
Once the introduction has been made, the interview may begin with a general, open-ended question, such as “What medical problem has brought you to the hospital?” or “I understand you are having. . . . Tell me more about the problem.” This type of opening remark allows the patient to speak first. The interviewer can then determine the patient’s chief complaint: the problem that is regarded as paramount. If the patient says, “Haven’t you read my records?” it is correct to say, “No, I’ve been asked to interview you without any prior information.” Alternatively, the interviewer could say, “I would like to hear your story in your own words.”
Patients can determine very quickly if you are friendly and personally interested in them. You may want to establish rapport by asking them something about themselves before you begin diagnostic questioning. Take a few minutes to get to know the patient. If the patient is not acutely ill, you may want to say, “Before I find out about your headache, tell me a little about yourself.” This technique puts the patient at ease and encourages him or her to start talking. The patient usually talks about happy things in his or her life rather than the medical problems. It also conveys your interest in the patient as a person, not just as a vehicle of disease.
The Narrative
Novice interviewers are often worried about remembering the patient’s history. However, it is poor form to write extensive notes during the interview. Attention should be focused more on what the person is saying and less on the written word. In addition, by taking notes, the interviewer cannot observe the facial expressions and body language that are so important to the patient’s story. A pad of paper may be used to jot down important dates or names during the session.
After the introductory question, the interviewer should proceed to questions related to the chief complaint. These should naturally evolve into questions related to the other formal parts of the medical history, such as the present illness, past illnesses, social and family history, and review of body systems. Patients should largely be allowed to conduct the narrative in their own way. The interviewer must select certain aspects that require further details and guide the patient toward them. Overdirection is to be avoided because this stifles the interview and prevents important points from being clarified.
Small talk is a useful method of enhancing the narrative. Small talk, also known as “chit-chat,” is neither random nor pointless, and studies in conversation analysis indicate that it is actually useful in communication. It has been shown that during conversations, the individual who tells a humorous anecdote is the one who is in control. For example, if an interviewer interjects a humorous remark during an interview and the patient laughs, the interviewer is in control of the conversation. If the patient does not laugh, the patient may take control.
Be alert when a patient says, “Let me ask you a hypothetical question” or “I have a friend with . . . ; what do you think about . . . ?” In each case, the question is probably related to the patient’s own concerns.
A patient often uses utterances such as “uh,” “ah,” and “well” to avoid unpleasant topics. It is natural for a patient to delay talking about an unpleasant situation or condition. Pauses between words, as well as the use of these words, provide a means for the patient to put off discussing a painful subject.
When patients use vague terms such as “often,” “somewhat,” “a little,” “fair,” “reasonably well,” “sometimes,” “rarely,” or “average,” the interviewer must always ask for clarification: “What does sometimes mean?” “How often is often?” Even terms such as “dizzy,” “weak,” “diarrhea,” and “tired” necessitate explanation. Precise communication is always desirable, and these terms, among others, have significant variations in meaning.
The interviewer should be alert for subtle clues from the patient to guide the interview further. There are a variety of techniques to encourage and sustain the narrative. These guidelines consist of verbal and nonverbal facilitation, reflection, confrontation, interpretation, and directed questioning. These techniques are discussed later in this chapter.
The Closing
It is important that the interviewer pace the interview so that adequate time is left for the patient to ask questions and for the physical examination. About 5 minutes before the end of the interview, the interviewer should begin to summarize the important issues that were discussed.
If the patient asks for an opinion, it is prudent for the novice interviewer to answer, “I am a medical student. I think it would be best to ask your doctor that question.” You have not provided the patient with the answer that he or she was seeking; however, you have not jeopardized the existing doctor-patient relationship by possibly giving the wrong information or a different opinion.
At the conclusion, it is polite to encourage the patient to discuss any additional problems or to ask any questions: “Is there anything else you would like to tell me that I have not already asked?” “Are there any questions you might like to ask?” Usually, all possible avenues of discussion have been exhausted, but these remarks allow the patient the “final say.”
Thus a good closure should consist of the following four parts:
Basic Interviewing Techniques
The successful interview is smooth and spontaneous. The interviewer must be aware of subtleties and be able to pick up on these clues. The successful interviewer sustains the interview. Several techniques can be used to encourage someone to continue speaking, and this section discusses those interviewing techniques. Each technique has its limitations, and not all of them are used in every interview.
Questioning
The secret of effective interviewing lies in the art of questioning. The wording of the question is often less important than the tone of voice used to ask it. In general, questions that stimulate the patient to talk freely are preferred.
Open-Ended Questions
Open-ended questions are used to ask the patient for general information. This type of question is most useful in beginning the interview or for changing the topic to be discussed. An open-ended question allows the patient to tell his or her story spontaneously and does not presuppose a specific answer. It can be useful to allow the patient to “ramble on.” An open-ended question is a question that cannot be answered by saying “Yes” or “No.” Examples of open-ended questions are the following:
“What kind of medical problem are you having?”
“Are you having stomach pain? Tell me about it.”
“Tell me about your headache.”
“How was your health before your heart attack?”
Too much rambling, however, must be controlled by the interviewer in a sensitive but firm manner. This freedom of speech should obviously be avoided with overtalkative patients, whereas it should be used often with silent patients.
Direct Questions
After a period of open-ended questioning, the interviewer should direct the attention to specific facts learned during the open-ended questioning period. These direct questions serve to clarify and add detail to the story. This type of question gives the patient little room for explanation or qualification. A direct question can usually be answered in one word or a brief sentence; for example:
Care must be taken to avoid asking direct questions in a manner that might bias the response.
Symptoms are classically characterized according to several dimensions or elements, including bodily location, onset (and chronology), precipitating (and palliating) factors, quality, radiation, severity, temporal, and associated manifestations. These elements may be used as a framework to clarify the illness. Examples of appropriate questions follow.
Onset (and Chronology)
Precipitating Factors
Palliating Factors
Radiation
Severity (or Quantity)
“On a scale from 1 to 10, with 10 the worst pain you can imagine, how would you rate this pain?”
“How has the pain affected your lifestyle?”1
“What do you mean by ‘a lot’?”
“How many sanitary napkins do you use?”
“How many times did you vomit?”
“What kind of effect does the pain have on your work?”
“How does the pain compare with the time you broke your leg?”
Temporal
Associated Manifestations
“Do you have any other symptoms?”
“Do you ever have nausea with the pain?”
“Have you noticed other changes that happen when you start to sweat?”
“Before you get the headache, do you ever experience a strange taste or smell?”
The mnemonic O-P-Q-R-S-T, which stands for onset (chronology), precipitating (or palliative), quality, radiation, severity, and temporal, is useful in helping the interviewer remember these important dimensions of a symptom. The setting is also important to determine. Did the symptom occur when exposed to certain environmental conditions, during specific activities, during emotional periods, or under other circumstances?
Question Types to Avoid
There are several types of questions that should be avoided. One is the suggestive question, which provides the answer to the question. For example:
A better way to ask the same question would be as follows:
The why question carries tones of accusation. This type of question almost always asks a patient to account for his or her behavior and tends to put the patient on the defensive; for example:
The answers to such questions, however, are important. As mentioned previously, try rephrasing as “What is the reason . . . ?” The “why” question is useful in daily life with friends and family, with whom you have a relationship different from that with your patients; do not use it with patients.
The multiple or rapid-fire question should also be avoided. In this type of question, there is more than one point of inquiry. Don’t barrage the patient with a list of questions. The patient can easily get confused and respond incorrectly, answering no part of the question adequately. The patient may answer only the last inquiry heard; for example:
The other problem with multiple questions is that you may think you have asked the question, but the patient has answered only part of it. For example, in the first inquiry just mentioned, the patient may answer “No” to indicate “no chills,” but if you ask about the symptoms separately, you might find out that the patient does have a history of night sweats.
Questions should be concise and easily understandable. The context should be free of medical jargon. Frequently, novice interviewers try to use their new medical vocabularies to impress their patients. They may sometimes respond to the patient with technical terms, leaving the patient feeling confused or put down. By using medical jargon, the interviewer distances himself or herself from the patient. This use of technical medical terms is sometimes called doctorese or medicalese. For example:
“You seem to have a homonymous hemianopsia.”
“Have you ever had a myocardial infarction?”
“We perform Papanicolaou smears to check for cervical carcinoma in situ.”
“I am going to order a CBC with differential.”
“The MUGA scan shows that you have congestive heart failure.”
Medical terminology, as a rule, should not be used in conversations with patients. Technical terms scare patients who are unfamiliar with them. Every medical and nursing student understands the term heart failure, but a patient might interpret it as failure of the heart to pump—that is, cardiac standstill, or death. Although patients should be given only as much information as they can handle, adequate explanations must always be provided. A partial explanation can leave the patient confused and fearful. Conversely, patients may try to use medical terms themselves. Do not take these terms at face value; ask patients to describe what they mean. For example, some patients may use “heart attack” to describe angina, “stroke” to describe a transient ischemic attack, “spells” to describe dizziness, or “water pills” or “heart pills” when referring to their medication.
A leading or biased question carries a suggestion of the kind of response for which the interviewer is looking. For example, “You haven’t used any recreational drugs, have you?” suggests that the interviewer disapproves of the patient’s use of drugs. If the patient has used recreational drugs, he or she may not admit it under this line of questioning. Instead, ask, “Do you use recreational drugs?” Questions should be asked in the positive or affirmative mode, not the negative. Questions asked in the affirmative or positive mode convey a nonjudgmental approach and encourage the patient to answer more candidly without the fear of being blamed for an action.
It is also incorrect to ask, “You don’t have diabetes, do you?” or “You haven’t been wheezing, have you?” Instead, the interviewer should ask in the positive affirmative mode, “Do you have diabetes?” or “Have you been wheezing?” A leading question may also invite a particular answer. For example, “Did you notice that the pain came on after you vomited?”
In addition to avoiding certain types of questions, the interviewer should avoid certain situations. For example, patients may respond to a question in an unexpected manner, resulting in a period of unexpected silence on the part of the interviewer. This “stumped silence” can be interpreted by the patient in a variety of ways. The interviewer must be able to respond quickly in such instances, even if it means broaching another topic.
If a patient suggests that a test not be performed, perhaps because of an underlying fear of the test, the interviewer should never respond by stating, “I’m the doctor. I’ll make the decisions.” The interviewer should recognize the anxiety and handle the response from that point of view. He or she should ask the patient, “What are your concerns about taking the test?”
If a patient appears overweight, ask first whether there has been any change in the patient’s weight before asking whether he or she has tried to lose weight. The patient may have lost 30 pounds already but is still overweight. Never refer to an overweight person as obese.
Finally, assume nothing about patients’ knowledge of their disease, their sexual orientation or experiences, their education, their family, or their knowledge of illness in general. People come from different backgrounds and have different beliefs based on culture, religion, and experience. It is incorrect to assume that if a medicine has been prescribed for an illness, the patient is taking it correctly or actually taking it at all. Do not even presume that a patient is happy or sad about an event in his or her life or in the lives of friends and family. It is much safer to ask questions in the following manner:
Silence
Silence is most useful with silent patients. Silence should never be used with overtalkative patients, because letting them talk continuously would not allow the interviewer to control the interview. This difficult type of communication, when used correctly, can indicate interest and support. Silence on the part of the patient can be related to hostility, shyness, or embarrassment. The interviewer should remain silent, maintaining direct eye contact and attentiveness. The interviewer may lean forward and even nod. After no more than 2 minutes of silence, the interviewer may say,
If the patient remains silent, another method of sustaining the interview must be chosen.
The interviewer must use silence when the patient becomes overwhelmed by emotion. This act allows the patient to release some of the tension evoked by the history and indicates to the patient that it is acceptable to cry. Handing the patient a box of tissues is a supportive gesture. It is inappropriate for the interviewer to say, “Don’t cry” or “Pull yourself together” because these statements imply that the patient is wasting the interviewer’s time or that it is shameful to show emotions.
It is important to use silence correctly. An interviewer who remains silent, becomes fidgety, reviews notes, or makes a facial expression of evaluation will inhibit the patient. The patient may perceive the frequent use of silence by the interviewer as aloofness or a lack of knowledge.
Facilitation
Facilitation is a technique of verbal or nonverbal communication that encourages a patient to continue speaking but does not direct him or her to a topic. A common verbal facilitation is “Uh huh.” Other examples of verbal facilitations include “Go on,” “Tell me more about that,” “And then?” and “Hmm.”
An important nonverbal facilitation is nodding the head or making a hand gesture to continue. Moving toward the patient connotes interest. Be careful not to nod too much, as this may convey approval in situations in which approval may not be intended.
Often, a puzzled expression can be used as a nonverbal facilitation to indicate, “I don’t understand.”
Confrontation
Confrontation is a response based on an observation by the interviewer that points out something striking about the patient’s behavior or previous statement. This interviewing technique directs the patient’s attention to something of which he or she may or may not be aware. The confrontation may be either a statement or a question; for example:
“Is there any reason why you always look away when you talk to me?”
“You sound uncomfortable about it.”
Confrontation is particularly useful in encouraging the patient to continue the narrative when there are subtle clues given. By confronting the patient, the interviewer may enable the patient to explain the problem further. Confrontation is also useful to clarify discrepancies in the history.
Confrontation must be used with care; excessive use is considered impolite and overbearing. If correctly used, however, confrontation can be a powerful technique. Suppose a patient is describing a symptom of chest pain. By observing the patient, you notice that there are now tears in the patient’s eyes. By saying sympathetically, “You look very upset,” you are encouraging the patient to express emotions.
Interpretation
Interpretation is a type of confrontation that is based on inference rather than on observation. The interviewer interprets the patient’s behavior, encouraging the patient to observe his or her own role in the problem. The interviewer must fully understand the clues the patient has given before he or she can offer an interpretation. The interviewer must look for signs of underlying fear or anxiety that may be indicated by other symptoms, such as recurrent pain, dizziness, headaches, or weakness. Once these underlying fears have been discovered, the patient may be led to recognize the inciting event during future interviews. Interpretation frequently opens previously unrecognized lines of communication. Examples are the following:
“You seem to be quite happy about that.”
“Are you afraid you’ve done something wrong?”
“I wonder whether there’s a relation between your dizziness and arguments with your wife.”
Interpretation can demonstrate support and understanding if used correctly.
Reflection
Reflection is a response that mirrors or echoes that which has just been expressed by the patient. It encourages the patient to expound further on details of the statement. The tone of voice is important in reflection. The intonation of the words may indicate entirely different meanings. For example:
In this example, the emphasis should be on “2012.” This asks the patient to describe the conditions that did not allow him or her to work. If the emphasis is incorrectly placed on “worked,” the interviewer immediately puts the patient on the defensive, implying, “What did you do with your time?” Although often very useful, reflection can hamper the progress of an interview if used improperly.
Support
Support is a response that indicates an interest in or an understanding of the patient. Supportive remarks promote a feeling of security in the doctor-patient relationship. A supportive response might be “I understand.” An important time to use support is immediately after a patient has expressed strong feelings. The use of support when a patient suddenly begins to cry strengthens the doctor-patient relationship. Two important subgroups of support are reassurance and empathy.
Reassurance
Reassurance is a response that conveys to the patient that the interviewer understands what has been expressed. It may also indicate that the interviewer approves of something the patient has done or thought. It can be a powerful tool, but false reassurance can be devastating. Good examples of reassurance are the following:
“That’s wonderful! I’m delighted that you started in the rehabilitation program at the hospital.”
“That’s great that you were able to stop smoking.”
“It’s understandable why you are so upset after your accident.”
“It’s good you came in today. We will do everything to help you.”
The use of reassurance is particularly helpful when the patient seems upset or frightened. Reassurance must always be based on fact. Reassurance is very important because it tells the patient that his or her fears are understandable and real.
False reassurances restore a patient’s confidence but ignore the reality of the situation. Telling a patient that his or her “surgery will be successful” clearly discounts the known morbidity and mortality rates associated with it. The patient wants to hear such reassurance, but it may be false.
Never tell a patient to relax. Patients are often nervous and are entitled to be upset or worried. Try to instill confidence in your patient instead of trying to talk the patient out of being nervous. These comments may be counterintuitive. Telling a patient to be calm may send the message that you are uncomfortable with their problem or that you do not really understand the problem’s severity.
Empathy
Empathy is a response that recognizes the patient’s feeling and does not criticize it. It is understanding, not an emotional state of sympathy. You try to put yourself in the shoes of the patient. The empathic response is saying, “I hear what you’re saying.” The use of empathy can strengthen the doctor-patient relationship and allow the interview to flow smoothly. Examples of empathy are the following:
“I’m sure your daughter’s problem has given you much anxiety.”
“The death of someone so close to you is hard to take.”
“I guess this has been kind of a silent fear all your life.”
The last two examples illustrate an important point: it is critical to give credit to patients to encourage their role in their own improvement.
It is really impossible, however, to put yourself in the shoes of the patient because of a difference in age, gender, life experiences, education, culture, religion, and other factors. An extremely empathic statement, which sounds counterintuitive, is “It’s impossible for me to fully understand how you are feeling, but how can I help you? How can we work together to get past this problem?”
Empathetic responses can also be nonverbal. An understanding nod is an empathetic response. In certain circumstances, placing a hand on the shoulder of an upset patient communicates support. The interviewer conveys that he or she understands and appreciates how the patient feels without actually showing any emotion.
Transitions
Transitional statements are used as guides to allow the patient to understand better the logic of the interviewer’s questioning and for the interview to flow more smoothly from one topic to another. An example of a transitional statement might be, after learning about the current medical problem, the interviewer’s statement, “Now I am going to ask you some questions about your health history.” Other examples while the history is documented might be, “I am now going to ask you some questions about your family,” and “Let’s talk about your lifestyle and your activities in a typical day.”
Usually, the line of questioning being pursued is obvious to the patient, so transitions are not always needed. Transitioning to the sexual history, however, often requires a transitional statement. As an example, a transitional statement such as “I am now going to ask you some routine questions about your sexual history” may bridge to this area comfortably for both the patient and interviewer. An alternative transitional statement might be, “To determine your risk for several diseases, I am now going to ask you some questions about your sexual health [or sexual activity, or sexual habits].” Avoid phrases such as “personal habits” or “personal history,” because these expressions send the message of what the interviewer considers these habits to be; the patient may be more open to discuss this area and may not consider it “personal.” It is better to ask about “sexual habits,” “sexual activity,” or “sexual health,” rather than “sexual life.” Other words to be avoided include “like to,” “want to,” “need to,” or “have to” (e.g., “I would now like to ask you some questions about your sexual habits” or “I now have to ask you some questions about your sexual habits”). As will be discussed in subsequent chapters, always use specific language. Refer to the genitalia with explicit terms such as vagina, penis, uterus, and so on; do not use the term “private parts.”
Format of the History
The information obtained by the interviewer is organized into a comprehensive statement about the patient’s health. Traditionally, the history has been obtained by using a disease-oriented approach emphasizing the disease process that prompted the patient to seek medical advice. For example, a patient may present with shortness of breath; the interview would be conducted to ascertain the pathologic causes of the shortness of breath.
An alternative approach to obtaining the history is a patient-oriented one. This entails evaluating the patient and his or her problems more holistically. By using this approach, the health care provider can elicit a more complete history, keeping in mind that other symptoms (e.g., pain from arthritis, weakness, depression, anxiety) may have an effect on the patient’s shortness of breath. For example, if a patient has arthritis and cannot walk, shortness of breath may manifest as less severe than if the patient were able to walk and experienced shortness of breath with minimal activity. In this way, the entire patient is taken into account.
The major traditional sections of the history, with some patient-oriented changes, are as follows:
• History of the present illness and debilitating symptoms
• Occupational and environmental history
• Psychosocial and spiritual history
Source and Reliability
The source and reliability contains identifying data; source of the history; and, if appropriate, the source of the referral. The identifying data consist of the age and gender of the patient. The source of information is usually the patient. If the patient requires a translator, the source is the patient and the translator. If family members help in the interview, their names should be included in a single-sentence statement. The source could also be a medical record.
The reliability of the interview should be assessed. Is the patient competent to provide a history? Often determination of orientation to person, time, and place (discussed in Chapter 18, The Nervous System) is done early in the interview to assess the cognitive function of the person. If the patient is not oriented to person, time, and place, a statement such as, “The patient is a 76-year-old white man with a moderate cognitive impairment as manifested by a lack of orientation to person, time, and place who presents with. . . .” This indicates that the rest of the history needs to be taken with “a grain of salt” or that some or all of the history that follows may be inaccurate. The date and time of the interaction is also vital for the record.
Chief Complaint
The chief complaint is the patient’s brief statement explaining why he or she sought medical attention. Try to actually quote the patient’s own words. It is the answer to the question, “What is the medical problem that brought you to the hospital?” or “How can I help you today?” The chief complaint might then be:
“I’ve been having chest pain for the past 5 hours.”
“I have had terrible nausea and vomiting for 2 days.”
“I’ve got a splitting headache for the last few days.”
Patients sometimes use medical terms. The interviewer must ask the patient to define such terms to ascertain what the patient means by them.
History of Present Illness and Debilitating Symptoms
The history of the present illness refers to the recent changes in health that led the patient to seek medical attention at this time. It describes the information relevant to the chief complaint. It should answer the questions of what, when, how, where, which, who, and why. It provides a clear, chronologic explanation of the patient’s symptoms accounting for the reason the patient has sought medical attention.
Chronology is the most practical framework for organizing the history. It enables the interviewer to comprehend the sequential development of the underlying pathologic process. In this section, the interviewer gathers all the necessary information, starting with the first symptoms of the present illness and following its progression to the present day. To establish the beginning of the present illness, it is important to verify that the patient was entirely well before the earliest symptom. Patients often do not remember when a symptom developed. If the patient is uncertain about the presence of a symptom at a certain time, the interviewer may be able to relate it to an important or memorable event, for example, “Did you have the pain during your summer vacation?” In this part of the interview, mainly open-ended questions are asked because these afford the patient the greatest opportunity to describe the history.
In the patient-centered evaluation, the interviewer must determine whether any debilitating symptoms are also present and what effect they have on the patient. These symptoms include pain, constipation, weakness, nausea, shortness of breath, depression, and anxiety.
For each symptom, seven attributes are important to ascertain. They are:
• Location
• Quality
• Severity
• Timing, including onset, duration, and frequency
The effect of the symptom or condition on the patient’s life must be assessed. One can simply ask, “How has your problem interfered with your daily life?”
Pain
Pain is one of the most debilitating symptoms and has traditionally been underrecognized. Unrelieved pain is very common and is one of the most feared symptoms of illness. Surveys indicate that 20% to 30% of the U.S. population experiences acute or chronic pain, and it is the most common symptom experienced by hospitalized adults. More than 80% of patients with cancer and more than two thirds of patients dying of noncancer illnesses experience moderate to severe pain. There are approximately 75 million episodes of acute pain per year resulting from traumatic injuries and surgical procedures. Acute pain is caused by trauma or medical conditions, is usually brief, and abates with resolution of the injury. Chronic pain persists beyond the period of healing or is present for longer than 3 months.
The effect of pain on the quality of life is important to understand. Untreated or undertreated pain impairs physical and psychological health, functional status, and quality of life. In particular, pain may produce unnecessary suffering; decrease physical activity, sleep, and appetite, which further weakens the patient; may increase fear and anxiety that the end is near; may cause the patient to reject further treatment; may diminish the ability to work productively; may diminish concentration; may decrease sexual function; may alter appearance; and may diminish the enjoyment of recreation and social relationships. In addition, pain has been associated with increased medical complications, increased use of health care resources, decreased patient satisfaction, and unnecessary suffering. In the United States, the economic costs of undertreated pain approach $80 billion per year in treatment, compensation, and lost wages.
Because of health care providers’ lack of knowledge about analgesics, negative attitudes toward the use of pain control, and lack of understanding about addiction, and because of drug regulations and the cost of effective pain management, patients often suffer unnecessarily from inadequate pain control. A study of medical inpatients and the use of narcotic analgesics revealed that 32% of patients were continuing to experience “severe” distress despite the analgesic regimen, and 41% were in “moderate” distress. Breitbart and colleagues (1996) also revealed that pain was dramatically undertreated in ambulatory patients with acquired immune deficiency syndrome (AIDS). Of patients experiencing severe pain, only 7.3% received opioid analgesics at the recommended doses. Approximately 75% with severe pain received no opioid analgesics at all. The Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatment (1995) indicated that 50% of conscious patients who died in a hospital suffered “moderate-severe” pain during their last week of life.
Cleeland and associates (1997) reported that members of ethnic minority groups are likely to receive inadequate treatment for pain. Their study showed that minority patients were three times more likely to be undertreated for pain. Sixty-five percent of minority patients did not receive guideline-recommended analgesic prescriptions. Latino patients reported less pain relief than did African-American patients. Morrison and colleagues (2000) investigated the availability of commonly prescribed opioid analgesics in pharmacies in New York City. They found that 50% of a random sample of pharmacies surveyed did not stock sufficient medications to treat patients with severe pain adequately. Pharmacies in predominantly nonwhite areas were less likely to stock opioid analgesics than were pharmacies in predominantly white neighborhoods.
Whatever the cause of pain, health care providers must ask repeatedly about the presence of pain and the adequacy of its control:
“Have you had pain in the past week?”
“Tell me where your pain is located.”
“How has the pain affected your life?”
It is often useful with geriatric patients to say, “Many people have pain. Is there anything you want to tell me?” In cognitively impaired patients, the interviewer should ask about the real-time assessment of pain: pain now, not pain in the past 3 days.
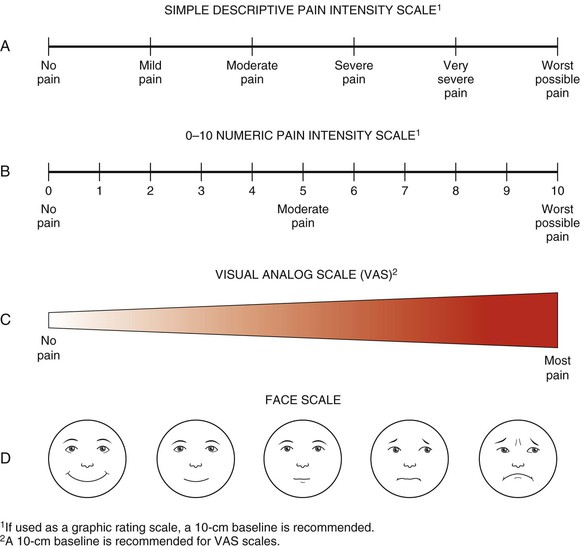
Patients must be able to assess pain with easily administered rating scales and should document the efficacy of pain relief at regular intervals after the initiation or modification of treatment. In addition, it is vital to teach patients and their families how to promote effective pain management at home. The interviewer should ask patients to quantify their pain and should try using some form of pain rating scale. There are four commonly used scales:
These scales are illustrated in Figure 1-1.
Past Medical History
The past medical history consists of the overall assessment of the patient’s health before the present illness. It includes all of the following:
General State of Health
As an introduction to the past medical history, the interviewer may ask, “How has your health been in the past?” If the patient does not elaborate about specific illnesses, but says only “Excellent” or “Fair,” for example, the interviewer might ask, “What does ‘excellent’ mean to you?” Direct questioning is appropriate and allows the interviewer to focus on pertinent points that need elaboration.
Past Illnesses
The record of past illnesses should include a statement of childhood and adult problems. Recording childhood illnesses is obviously more important for pediatric and young adult interviewees. All patients should nevertheless be asked about measles, mumps, whooping cough, rheumatic fever, chickenpox, polio, and scarlet fever. Older patients may respond, “I really don’t remember.” It is important to remember that a diagnosis given to the interviewer by a patient should never be considered absolute. Even if the patient was evaluated by a competent clinician in a reputable medical center, the interviewer may have misunderstood the information given.
Prior Injuries and Accidents
The patient should be asked about any prior injuries or accidents: “Have you ever been involved in a serious accident?” The type of injury and the date are important to record.
Hospitalizations
All hospitalizations must be indicated, if not already described. These include admissions for medical, surgical, and psychiatric illnesses. The interviewer should not be embarrassed to ask specifically about psychiatric illness, which is a medical problem. Interviewer embarrassment inevitably leads to patient embarrassment and reinforces the “shame” associated with psychiatric illness. Student interviewers should learn to ask direct questions in a sensitive manner. The interviewer might ask, “Have you ever been in therapy or counseling?” or “What nervous or emotional problems have you had?” Another way to ask about psychiatric hospitalizations is to ask, “Have you ever been hospitalized for a nonmedical or nonsurgical reason?”
Surgery
All surgical procedures should be specified. The indication, type of procedure, date, hospital, and surgeon’s name should be documented, if possible.
Allergies
All allergies should be described. These include environmental (including insects), ingestible, and drug-related reactions. The interviewer should seek specificity and verification of the patient’s allergic response. “How do you know you’re allergic?” “What kind of problem did you have when you took . . . ?” The specific symptoms of an allergy (e.g., rashes, nausea, itching, anaphylaxis) should be clearly indicated.
Immunizations
It is important to determine the immunization history of all patients. Tetanus and diphtheria immunity is present in fewer than 25% of adults, and fewer than 25% of targeted groups receive influenza vaccines yearly. Tetanus and diphtheria are preventable, and the current recommendation is to use the combined toxoid whenever either immunization is considered. Any patient who has never received this toxoid receives an initial injection and follow-up doses at 1 month and 6 to 12 months. A booster dose is required every 10 years.
All patients with chronic cardiovascular, pulmonary, metabolic, renal, or hematologic disorders and patients with immunosuppression should be vaccinated yearly against influenza. Patients older than 65 years should also receive the vaccine.
Indications for the pneumococcal polysaccharide vaccine are similar to those for the influenza vaccine. In addition, patients with multiple myeloma, lymphoma, alcoholism, cirrhosis, and functional or anatomic asplenia should receive the vaccine. This vaccine usually provides lifelong immunity. Revaccination every 6 years is necessary only in asplenic patients because they are at high risk for pneumococcal infection.
Hepatitis A is one of the most common vaccine-preventable infections acquired during travel. Hepatitis A is a liver disease caused by the hepatitis A virus. Hepatitis A can affect anyone and is transmitted by the fecal-oral route. In the United States, hepatitis A can occur in situations ranging from isolated cases of disease to widespread epidemics. Good personal hygiene and proper sanitation can help prevent hepatitis A. Vaccines are also available for long-term prevention of hepatitis A virus infection in persons 12 months of age and older. The first dose of hepatitis A vaccine should be administered as soon as travel to countries with high or intermediate endemicity is considered. One month after receiving the first dose of monovalent hepatitis A vaccine, 94% to 100% of adults and children have protective concentrations of antibody. The final dose in the hepatitis A vaccine series is necessary to promote long-term protection. Immune globulin is available for short-term prevention of hepatitis A virus infection in individuals of all ages.
Hepatitis B vaccine should be given to all health care providers, staff of institutions for developmentally disabled patients, intravenous drug abusers, patients with multiple sexual partners, hemodialysis patients, sexual partners of hepatitis B carriers, and patients with hemophilia. Complete immunization necessitates three injections: an initial dose and follow-up doses at 1 month and at 6 to 12 months. Booster doses are not required. For best results, persons at high risk of exposure (especially medical, dental, and nursing students) should receive immunization before possible exposure.
Haemophilus influenzae type B (Hib) vaccine is now used routinely in children to prevent invasive H. influenzae diseases. In 2005, Hib was estimated to have caused 3 million cases of serious disease, notably pneumonia and meningitis, and 450,000 deaths in young children. Meningitis and other serious infections caused by Hib disease can lead to brain damage or death. Hib disease is preventable by immunizing all children younger than 5 years with an approved Hib vaccine. Several Hib vaccines are available. The general recommendation is to immunize children with a first dose at 2 months of age and to follow with additional doses according to the schedule for the vaccine being used. Three to four doses are needed, depending on the brand of Hib vaccine used. Hib vaccine should never be given to a child younger than 6 weeks, because this might reduce his or her response to subsequent doses.
Between 1991 and 1992, there was a 75% decrease in the number of cases of measles, mumps, and rubella (MMR), presumably because of the use of the MMR vaccine. This vaccine is now typically given in childhood, but it should also be given to adult health care providers who have not had the diseases. Because the vaccine contains a live virus, it should not be given to pregnant patients, those with generalized malignancies, those receiving steroid therapy, those with active tuberculosis, or those receiving antimetabolites.
The Advisory Committee on Immunization Practices annually reviews the recommended adult immunization schedule to ensure that the schedule reflects the current recommendations for the licensed vaccines. It is advisable for the health care worker to review these guidelines regularly.
Substance Abuse
A careful review of any substance abuse by the patient is included in the past medical history. Substance abuse includes cigarette smoking and the use of alcohol and recreational drugs. In the United States in 2007, an estimated 46 million people were smokers. Approximately 23% of men and 19% of women smoke. As many as 30% of all deaths related to coronary heart disease in the United States each year are attributable to cigarette smoking; the risk is strongly dose-related. Smoking also nearly doubles the risk of ischemic stroke. Smoking acts synergistically with other risk factors, substantially increasing the risk of coronary disease. Smokers are also at increased risk for peripheral vascular disease, cancer, chronic lung disease, and many other chronic diseases. Cigarette smoking is the single most alterable risk factor contributing to premature morbidity and mortality in the United States, accounting for approximately 430,000 deaths annually.
The interviewer should always ask whether the patient smokes and for how long: “Do you use nicotine in any form: cigarettes, cigars, pipes, chewing tobacco?” A pack-year is the number of years a patient has smoked cigarettes multiplied by the number of packs per day. A patient who has smoked 2 packs of cigarettes a day for the past 25 years has a smoking history of 50 pack-years. If the patient answers that he or she does not smoke now, the interviewer should inquire whether the patient ever smoked. If the patient has quit smoking, indicate for how long.
It has been estimated that the incidence of hazardous alcohol drinking in the United States ranges from 4% to 5% among women and 14% to 18% among men. In primary care settings, the prevalence rates range from 9% to 34% for hazardous drinking. Although studies have shown the beneficial effects of moderate alcohol consumption (one to two drinks daily), these effects are lost at higher doses. Heavy alcohol consumption is associated with many medical problems (e.g., hypertension, decreased cardiac function, arrhythmias, hemorrhagic stroke, ischemic stroke, liver disease, increased risk of breast cancer), as well as behavioral and psychiatric problems. According to the American Psychiatric Association and the National Institute on Alcohol Abuse and Alcoholism, “moderate drinking” for men is defined as less than 2 drinks per day; for women and persons older than 65 years, it is defined as less than 1 drink per day.
The history of alcohol consumption and dependency should be integrated into the general history immediately after the interviewer inquires about less threatening subjects such as smoking. It is easy to miss alcohol dependency unless specific direct questions are asked. It is acceptable to broach the topic of alcoholism by asking, “Please tell me about your drinking of alcohol.” The interviewer should focus not on the quantity of alcohol consumed but rather on the adverse effects of drinking. By asking, “How much do you drink?” the interviewer may put the patient on the defensive. This type of question may also create an unnecessary power struggle between patient and interviewer. Ask instead, “How much can you drink?” which puts the patient and interviewer in a position of alliance. Most individuals who drink heavily also underestimate the quantities they consume. The interviewer can often learn more about the quantity of alcohol consumed by asking about the patient’s feelings and interpersonal relationships than by asking directly about the amount. The interviewer should determine whether the patient drives while intoxicated, has suffered amnesia of events that occurred during drinking, neglects or abuses his or her family, or has missed work as a result of alcohol consumption.
Ewing and Rouse (1970) developed the CAGE questionnaire as a formal screening instrument to help identify patients in primary care with alcohol problems. The acronym CAGE helps the interviewer remember the four clinical interview questions that focus on the social and behavioral aspects of alcohol problems: the effect alcohol has on one’s lifestyle. Once it is established that a patient drinks alcohol, the following questions should be asked:
“Have you ever felt you should Cut down on your drinking?”
“Have people Annoyed you by criticizing your drinking?”
Since its introduction, the CAGE questionnaire has been shown to be one of the most efficient and effective screening devices for detecting alcoholism. In a primary care setting, CAGE scores of 2 (two positive responses) have a sensitivity of 77% to 94% and a specificity of 79% to 97% for a current diagnosis of alcohol abuse. One positive CAGE response has a sensitivity of 21% to 71% and a specificity of 84% to 95%. The history of alcohol consumption and dependency can be further assessed by using the sets of questions referred to by the acronyms HALT, BUMP, and FATAL DT.
The HALT questions are as follows:
“Do you usually drink to get High?”
“Do you ever find yourself Looking forward to drinking?”
“Have you noticed whether you seem to be becoming Tolerant of alcohol?”
The BUMP questions are as follows:
“Have you ever had Blackouts?”
“Have you ever used alcohol in an Unplanned2 way?”
“Do you ever drink alcohol for Medicinal3 reasons?”
“Do you find yourself Protecting4 your supply of alcohol?”
The final acronym reminds the interviewer about other major associations with alcoholism. The FATAL DT questions are as follows:
“Is there a Family history of alcoholic problems?”
“Have you ever been a member of Alcoholics Anonymous?”
“Do you Think you are an alcoholic?”
“Have you ever Attempted or had thoughts of suicide?”
“Have you ever had any Legal problems related to alcohol consumption?”
These questions provide the interviewer with a useful, thoughtful, and organized approach to the interview strategy designed to identify patients with a drinking problem.
In the late stages of alcoholism, a person may suffer delirium tremens (DTs). DTs are completely different from the hallucinations that occur in the earlier stages of alcoholism. During hallucinations, the patient may see or hear “things.” DTs occur 24 to 96 hours after withdrawal from alcohol; occasionally patients hallucinate or have convulsions, but all patients tremble. DTs are the most severe form of withdrawal and are fatal in one of every four cases.
The interviewer must ask all patients about the use of other drugs. People who use recreational drugs often engender negative feelings or anger in the interviewer. These feelings are almost unavoidable. The interviewer must not allow these feelings to interfere with empathetic interviewing. A useful way of approaching the topic of recreational drugs is to ask,
“Have you ever used drugs other than those required for medical reasons?”
“Do you use drugs other than those prescribed by a physician?”
If the answer to any of these questions is affirmative, the interviewer should determine the types of drugs used, the routes of administration, and the frequency of use. In contrast to alcohol abusers, drug abusers are more likely to magnify their use. The interviewer must ask all patients with a history of drug abuse the following questions:
“What type of drugs do you use?”
“At what age did you start using drugs?”
“What was your period of heaviest use?”
“What is your recent pattern of use?”
“Are larger doses necessary to get the same effect now?”
“What do you feel when you take the drug?”
“Have you ever tried to quit? What happened?”
“Have you ever had any convulsions after taking the drug?”
“Do you use more than one drug at a time?”
“Do you use drugs on a continuous basis?”
“Have you been in trouble at work because of drug use?”
“Have you ever had withdrawal symptoms as a result of your use of drugs?”
It is important to use simple words and expressions when inquiring about recreational drugs. It may also be more appropriate to use slang than to use more formal terms. For example, “Do you ever shoot up or snort coke?” may be better understood than “Have you ever taken cocaine intravenously or by insufflation?” With experience, the interviewer acquires relevant knowledge about recreational drugs. Knowing the local street names for drugs can be as important as knowing the pharmacologic effects and may provide a means of better communication. It should be recognized that these street names are often different from place to place and change from time to time.
It should also be recognized that any medication can be abused. Drugs such as propranolol and metoprolol (beta blockers used in the treatment of hypertension) are not usually considered recreational drugs. They are, however, frequently abused by the acting community to relieve performance anxiety, or stage fright.
Diet
In questioning a patient about diet, it is useful to ask the patient to describe what he or she ate the day before, including all three meals plus any snacks. How many fish meals does he or she have each week? What is the proportion of red meat in the diet in comparison with fish or poultry? How much saturated fat is there in the diet? Does the patient add salt when he or she cooks, and does he or she add salt at the table? Has his or her diet changed recently? What kinds of foods does the patient like or dislike, and why? Are there any food intolerances? Does the patient eat foods with a high fiber content, such as whole-grain breads and cereals, bran, fresh fruits, and vegetables? Does the patient eat high-fiber snack foods (which include sesame bread sticks, date-nut bread, oatmeal cookies, fig bars, granola bars, and corn chips)? What is the consumption of sodium? Pickled foods, cured meats, snack foods, and prepared soups have a high sodium content. The consumption of caffeine-containing products such as coffee, tea, sodas, and chocolate is important to determine. Caffeine ingestion may produce a variety of symptoms, including heart palpitations, fatigue, lightheadedness, headaches, irritability, and many gastrointestinal symptoms. The interviewer should also ascertain the amount of exercise the patient gets.
Sleep Patterns
It is important to know a patient’s sleep patterns because this may provide information about the patient’s psychological problems. Sleep-related complaints such as insomnia and excessive daytime somnolence impair the lives of 20% to 50% of Americans. Obstructive sleep apnea is a common and important health problem. It is discussed in Chapter 9, The Oral Cavity and Pharynx.
More than 60% of patients with psychiatric problems complain of disturbed sleep patterns. Eighty percent of patients with depression complain of disturbed sleep. The most common problem in patients with posttraumatic stress disorder is disturbed sleep; more than 50% of patients with chronic pain experience sleep problems.
An estimated 200,000 automobile accidents a year are caused by excessive sleepiness on the part of drivers; 20% of drivers report that they have fallen asleep behind the wheel. The following questions should be asked:
Medications
All current medications should be noted. The following questions should be asked:
“Do you use any prescription medications?”
“Do you use any over-the-counter medications?”
The name (generic or trade), dose, route of administration, and frequency of use need to be recorded. If possible, the patient should show the interviewer the bottles and demonstrate how the medications are taken. The interviewer should note whether the patient is taking them according to the directions on the bottle. Frequently, patients consider over-the-counter medications such as vitamins, laxatives, antacids, or cold remedies not worth mentioning; the interviewer should ask specifically about each of these types of drugs. The interviewer should determine the type of contraception used, if any, and whether a woman has used or uses birth control pills.
Alternative Therapies
The use of alternative therapies is extremely common, as discussed in Chapter 28, Understanding Complementary and Alternative Medicine, available online. The patient and the health care provider must be comfortable with how questions about these therapies are asked. Avoid using the terms unorthodox therapy or unconventional medicine. These labels may be perceived as judgmental and could inhibit free discussion. You might start by saying, “Many patients frequently use other kinds of therapy when they have the symptoms you described. Have you used or thought about using massage, herbs, chiropractic, acupuncture, vitamin, or other different therapies for your problem or for any other reasons?”
Health Maintenance
Clinicians can play a key role in the identification and management of medical, social, and psychiatric problems. Counseling skills include building a supportive therapeutic relationship with the patient and family. A patient’s family is often helpful in confirming the diagnosis and developing the treatment plan. Health maintenance consists of three main areas: disease detection, disease prevention, and health promotion.
Ask patients whether they have regular doctors and routine medical checkups. When was their last dental examination? Do they get their eyes checked periodically? Are they aware of their cholesterol levels? Do they do anything for exercise? If the patient is a woman, does she see a gynecologist regularly? Does she perform breast self-examination? When were her last mammogram and her last Papanicolaou smear obtained? If the patient is a man, does he perform routine testicular self-examination?
Tobacco use is probably the main avoidable cause of morbidity and mortality in the world. It is responsible for more than 450,000 deaths each year from cancer, heart disease, stroke, and chronic obstructive lung disease in the United States alone. Despite this fact, however, tobacco use is still prevalent. The Centers for Disease Control and Prevention estimates that 25% of all Americans still smoke and that more than 3000 children and adolescents become regular users every day. It is estimated that the cost of medical care for tobacco-related illness in the United States is more than $50 billion annually, and the cost of lost productivity and forfeited wages resulting from disability is an additional $50 billion per year. Despite these staggering statistics, health care providers often fail to treat tobacco use effectively. Health care providers have unique access to patients who use tobacco, and yet studies show that fewer than half of individuals who use tobacco reported being urged to quit by their physicians.
Health care providers must determine and document the tobacco use status of all patients. If patients use tobacco, they should be offered smoking cessation treatment at every office visit. It has been shown that a discussion of only 3 minutes per visit can be effective. More intensive treatment with other medical therapies, social support, and other specific skills is more effective in producing long-term results. In addition to nicotine replacement products, such as nicotine patches, nicotine gum, nicotine lozenges, nicotine nasal spray, and nicotine inhalers, varenicline (Chantix®) has been introduced to help someone quit smoking. It is nonnicotine prescription medicine specifically developed to help adults quit smoking. Varenicline, approved by the U.S. Food and Drug Administration in 2006, contains no nicotine, but it targets the same receptors as nicotine. It is believed to block nicotine from these receptors. It is the only prescription treatment of its kind at this time. Studies have demonstrated that at the end of 12 weeks of varenicline therapy, 44% of patients were able to quit smoking. It also helped reduce the urge to smoke.
It also has been demonstrated, however, that there are times when patients are unreceptive or even resentful if the issue is broached. According to the “stages of change” model, success is most likely when the health care provider is sensitive to the patient’s stage. Stage 1 is the precontemplation stage in which the smoker is in denial about the hazards of smoking and is not willing to stop. Stage 2 is the contemplation stage, when the patient acknowledges a willingness to quit but has not determined when that will occur. Stage 3 is the action stage, during which the patient has prepared for a change, is engaged in changing behavior, and has a plan for smoking cessation. Stage 4 is the maintenance stage, during which the health care provider needs to encourage the patient about the experience of quitting. Stage 5 is the relapse. Smokers generally make three or more attempts to quit smoking before permanent success is achieved.
Patients should be told in clear, strong language that it is in their best interest to quit smoking. Say, “I think that it is important for you to quit smoking, and I will help you. I need you to know that quitting smoking is the most important thing you can do to protect your current and future health.”
Also remember to ask the questions about alcohol consumption discussed in the previous section.
Counseling is very important, but interviewers must remember that a patient must want to change his or her behavior. If he or she does not, interviewers should indicate to the patient that they will provide support when the patient is ready.
Finally, do not forget to ask all patients whether they wear seat belts in cars or use helmets if they ride bicycles or motorcycles.
Occupational and Environmental History
The occupational and environmental history concerns exposure to potential disease-producing substances or environments. Occupational exposures account for an estimated 50,000 to 70,000 deaths annually in the United States. More than 350,000 new cases of occupational disease are recognized each year. These diseases can involve every organ system. Because they often mimic other diseases, occupational diseases may be incorrectly ascribed to some other cause. One of the important barriers to the accurate diagnosis of occupational and environmental diseases is the long latency between exposure and appearance of the illness.
Many occupational diseases have been well described over the years: malignant mesothelioma in workers exposed to asbestos; cancer of the bladder in workers exposed to aniline dye; malignant neoplasms of the nasal cavities in woodworkers; pneumoconiosis in coal miners; silicosis in sandblasters and quarry workers; leukemia in those exposed to benzene; hepatic angiosarcoma in workers exposed to vinyl chloride; byssinosis in cotton industry workers; skin cancer in those chronically exposed to the sun, such as sailors; ornithosis in bird breeders; toxic hepatitis in solvent users and workers in the plastics industry; and chronic bronchitis in individuals exposed to industrial dusts. It has been shown that there is an association between sterility in men and women and exposure to certain pesticides and an association between dementia and exposure to certain solvents.
The environment is also responsible for significant morbidity and mortality rates. Lead, radon, pesticides, and air pollution cause illness and death. Examples include Chernobyl, with its widespread high levels of radiation; Minamata Bay in Japan, with its mercury poisoning; Hopewell, Virginia, with its poisoning pesticide chlordecone; and Bhopal, India, where a leak at an industrial plant exposed hundreds of thousands of people to toxic methyl isocyanate gas. In India, thousands died shortly after exposure, and more than 200,000 people have suffered illness from the gas. The long-range effects of these agents have yet to be determined.
A careful occupational and environmental history is the most effective means of properly diagnosing occupational and environmental diseases. It is important to inquire about all occupations and the duration of each. The history should include more than just a listing of jobs. The duration and precise activities must be ascertained. The use of protective devices and cleanup practices, as well as work in adjacent areas, must also be determined. The job title (e.g., electrician, machine operator) is important, but actual exposure to hazardous materials may not be reflected in these descriptions. Industrial work areas are complex, and it is important to ascertain the actual location of work in relation to other areas in which hazardous materials are used. It is well known that just living near areas of industrial toxins is linked to the development of disease many years later. It is therefore relevant to inquire whether the patient resides or ever resided near mines, farms, factories, or shipyards. The following questions regarding occupational and environmental exposure should be asked of all patients:
“What type of work do you do?”
“How long have you been doing this work?”
“Are you exposed to any hazardous materials? Do you ever use protective equipment?”
“What kind of work did you do before you had your current job?”
“What was your wartime employment, if any?”
“Where do you live? For how long?”
“Have you ever lived near any factories, shipyards, or other potentially hazardous facilities?”
“What types of hobbies do you have? What types of exposures are involved?”
Attention must be paid to any temporal relationship between the onset of illness and toxic exposure in the workplace. Did the symptoms start after the patient began a new job? Did the symptoms abate during a vacation and then recur when the patient resumed work? Were the symptoms related to the implementation of any new chemical or process? Is there anyone else at work or are there any neighbors with a similar illness?
Biographic Information
Biographic information includes the date and place of birth, sex, race, and ethnic background.
Family History
The family history provides information about the health of the entire family, living and dead. Pay particular attention to possible genetic and environmental aspects of disease that might have implications for the patient. Is the patient aware of any genetically determined disease in the family? Is there a history of cancer, specifically colon, breast, ovarian, or prostate? Is there a history or premature cardiovascular disease? Is here a history of diabetes; thyroid, liver, lung, blood, or renal disease; or rheumatologic disorders?
Determine the age and health of all the immediate family members. If a family member is deceased, record the age of the person and the cause of death. This information can be indicated on a pedigree, or family chart, showing each immediate relative, including parents and grandparents, siblings, children, and grandchildren. It is important to inquire how a family member’s illness affects the patient psychologically.
It is important to inquire where the patient’s parents were born. Where were the grandparents born? In what setting, urban or rural, did the patient grow up? In what country did the parents grow up? If the patient was born in another country, at what age did he or she come to the United States? Does the patient maintain contact with other family members? Was the original family name changed? If the patient is married, is the spouse of the same ethnic background as the patient? What is the patient’s native language?
The answers to these questions provide valuable information as a heritage assessment.
Psychosocial and Spiritual History
The psychosocial history includes information on the education, life experiences, and personal relationships of the patient. This section should include the patient’s lifestyle, other people living with the patient, schooling, military service, religious beliefs (in relation to the perceptions of health and treatment), and marital or significant-other relationships. You can start by asking one of the following questions:
“Tell me a little about yourself: your background, education, work, family.”
A statement regarding the patient’s knowledge of symptoms and illness is important. Has the illness caused the patient to lose time from work? What kind of insight does the patient have with regard to the symptom? Does he or she think about the future? If so, how does it look? An excellent question that can elicit a vast amount of information is “What is your typical day like?”
A spiritual history provides information about what gives meaning to the patient’s life. Spirituality helps patients cope with serious illnesses, debilitation, and dying. This part of the medical history provides excellent insight into the patient’s spiritual needs and belief systems. Meditation and prayer can complement medical care. Spirituality can offer hope to those with chronic disease and may even provide new meaning to their suffering. Several studies have revealed the beneficial effect of spirituality with regard to stress reduction, recovery from illness, mitigation of pain, and faster recovery from surgery. Puchalski and Romer (2000) suggested that a spiritual history might begin with an introductory question such as
Sexual, Reproductive, and Gynecologic History
The sexual history has traditionally been part of the psychosocial history or review of systems. However, because the sexual, reproductive, and gynecologic history is so vital for the complete evaluation of the patient, these histories are now considered a separate part of the interview.
There are several reasons for documenting a sexual history. Sexual drive is a sensitive indicator of general well-being. Anxiety, depression, and anger may relate to sexual dysfunction; however, many physical symptoms can lead to sexual problems. In addition, it is critical to identify risk behaviors. A well-documented sexual history enables the examiner to establish norms of sexuality for the patient. Opening up the interview to issues of sexuality allows the interviewer to educate the patient about human immunodeficiency virus (HIV)–related illnesses, sexually transmitted diseases, and pregnancy prevention. It is an excellent opportunity to provide useful information to the patient.
It is important to ask about sexual activity in children, as well as in older adults. Child abuse is very common, and the interviewer must identify it as early as possible. Interviewers must not assume that a senior citizen is sexually inactive. Sexuality is a part of normal life, and many older adults enjoy sexual contact.
Tailor your questions and terms to each specific interview. Can vernacular terms be used in the interview? Patients and interviewers may fear the use of these terms because of their emotional charge. Sometimes patients, because of embarrassment about using these terms, may try to express their symptoms with inaccurate medical terminology. Often the use of street language leads to a more relaxed and informative discussion, especially with younger adults.
The interviewer must inquire about sexual relationships in a nonjudgmental manner. Direct questions regarding oral and anal sex, sexual contacts, and sexual problems are very important. Patients are frequently less inhibited than are novice interviewers when discussing sexual behavior. If a patient’s sexual preference is in doubt, the term partner rather than a gender-specific term is appropriate. There is no easy way to ask about sexual preference, but it is vital to know. Asking the patient whether he or she has had any contact with individuals with AIDS or AIDS-related illness is appropriate. The term homosexual as an adjective for gender (e.g., “homosexual man”) should be avoided.
There are several general questions that can help broach the topic of sexual activity. In general, the best way to introduce the sexual history is to say, “Now I am going to ask you some questions about your sexual health and practices.” Because the question, “Are you sexually active?” can be ambiguous, it is better to ask, “Have you ever had intimate physical contact with anyone?” If the answer is “Yes,” the next question should be “Did that contact include sexual intercourse?” The interviewer should also then ask, “Are your partners male, female, or both?”
It is not acceptable to ask whether the person has “had sex” or is “sexually active,” because there is great variability in the way individuals define these phrases. In one study, 599 college students attending a major midwestern university were asked, “Would you say you ‘had sex’ with someone if the most intimate behavior you engaged in was . . . (mark ‘yes’ or ‘no’ for each behavior).” There were 11 items on the list, including “deep kissing,” “oral contact on your breasts/nipples,” “you touch other’s genitals,” “oral contact with other’s genitals,” and “penile-vaginal intercourse.” Although 99.7% agreed that penile-vaginal intercourse qualified as “had sex,” 19% did not believe that penile-anal intercourse meant “had sex.” Only 40% felt that they “had sex” if oral-genital contact was their most intimate behavior. The study suggests that Americans hold widely divergent opinions about what behaviors do and not constitute having “had sex.” Therefore, a better question to ask is “What is the most intimate physical contact you have had with someone else?”
Some of the following questions about specific sexual behaviors and satisfaction may also be helpful in acquiring a sexual history:
“Are you having any sexual problems?”
“Have you had any difficulty achieving orgasm?”
“How frequently does it occur that your partner desires sexual intercourse and you do not?”
“Are there any questions pertaining to your sexual performance that you would like to discuss?”
“Most people experience some disappointment in their sexual function. Can you tell me what disappointments you might have?”
“Have you ever had a sexually transmitted disease?”
“Have you been tested for HIV?” If yes, “What was the result?”
Asking a patient “How many sexual partners do you have or have you had?” is rather intrusive and does not help very much. It is much better to determine whether a person routinely uses protection with condoms, if appropriate. It is true, however, that studies have shown that the more sexual partners a woman has had, the greater is the chance that she will develop cervical carcinoma.
It is less appropriate to ask “What activities and positions does your sexual contact include?” than to ask specifically about oral-genital, penile-vaginal, or penile-anal contact tailored specifically to the individual patient.
Health care providers, regardless of their sexual orientation, must provide the highest standard of care to all patients. They must reconcile their own fears and prejudices about homosexuality. In 1978, only one third of Americans believed that they knew a gay man or lesbian; in 1996, approximately two thirds of Americans reported that they knew someone who was gay or lesbian. Despite this fact, there is a significant degree of homophobia in society. By definition, homophobia is the “irrational fear of, aversion to, or discrimination against homosexuality or homosexuals.” The medical and psychological effects of homophobia can pose a significant health hazard to gay and lesbian patients and can be detrimental to establishing a strong doctor-patient relationship. If a gay or lesbian patient senses this discrimination, he or she may become alienated from the health care system and not use standard screening modalities, thus risking higher mortality and morbidity from disease. One study revealed that 98% of gay and lesbian patients believed that it was medically important to inform their physicians of their sexual orientation, but 64% believed that in doing so, they risked receiving substandard care. In the same study, 88% of the patients reported that their physicians made disparaging remarks about gay and lesbian patients. Because homophobia is widespread in society, a gay or lesbian patient should have the confidence to speak candidly with his or her physician. At the time of publication of this book, the term gay is being replaced with “men having sex with men.”
Violence and Abuse
Domestic violence, rape, child abuse, sibling violence, and elder abuse are rampant and have reached staggering proportions. Of all domestic violence victims, 90% to 95% are women, and the perpetrators are mostly men. Every year, women experience 4.8 million intimate partner–related physical assaults and rapes. The violence is often a combination of physical, sexual, and psychological abuse, and the signs and symptoms may be subtle or obvious. It is therefore important to ask all patients whether they have ever been emotionally, physically, or sexually abused.
Much of the violence against women is perpetrated by their intimate partners or in relationships that are commonly protective, such as that of father and daughter. U.S. Department of Justice studies indicate that a woman is more likely to be raped, assaulted, or murdered by a male partner or ex-partner than by a stranger. Up to 45% of abused women are beaten during pregnancy. Four percent of all male homicide victims are killed by spouses or female partners. As many as 1 per 7 women seen in emergency departments has symptoms related to abuse. A national survey indicated that more than 2 million women are severely beaten by their male partners each year. It is recognized that such violence is vastly underreported; the actual number of cases is probably double the number reported. Clinicians frequently treat the injuries only symptomatically and often fail to recognize the abuse. Fourty-four percent of rape victims are under the age of 18 years; 80% percent are under the age of 30 years. It has been estimated that every two minutes, someone in the United States is sexually assaulted, and each year there are about 207,754 victims of sexual assault. Only 46% of sexually assaulted individuals report it to the police. Approximately two-thirds of assaults are committed by someone known to the victim.
Although many women who are victims of abuse do not volunteer any information, they often discuss the incidents if asked simple, direct questions in a nonjudgmental way and in a confidential setting. Be aware of the possibility of domestic violence in any woman with multiple medical visits for sexual dysfunction; multiple, unexplained bruises; chronic pelvic pain; fatigue; chest pain; gastrointestinal disturbances; headaches; depression; anxiety; panic attacks; eating disorders; substance abuse; suicidal attempts; and abdominal pain.
Because the perpetrator often accompanies the victim to the interview, ask any other person present to leave while you speak to the patient. Begin with the following direct question: “Since domestic violence is so common, I’ve begun to ask about it routinely. At any time, has your partner hit, kicked, or otherwise hurt or frightened you?” If the patient answers in the affirmative, encourage her to talk about it. Alternatively, you may ask, “Do you feel safe in your relationship?” Always listen nonjudgmentally to encourage the patient to continue talking about the episode. Showing support is very important. A statement such as “You are not alone” or “Help is available for you” shows empathy. It is crucial to assess the danger to the patient as quickly as possible before she leaves the medical facility. If the patient is in imminent danger, determine whether she can stay with friends or family. A shelter for battered women may be an alternative. Finally, provide the patient with the telephone number of the local domestic violence hotline.
If the patient answers “no” to your introductory query and you suspect some form of domestic violence, be aware of the clinical findings that may indicate abuse:
• Injury to head, neck, breasts, abdomen, or genitals
• Multiple injuries that seem inconsistent with the patient’s story
• Unusual explanation for the injury
• Vaginal bruises or lacerations
• A partner who seems overly protective and doesn’t want to leave the room
Any of these injuries must have a plausible explanation. If there is none, it is appropriate to ask further questions, but the partner must not be present. You might say, “It looks as if you’ve been hurt. Can you tell me how it happened?” Another approach could be “Sometimes when people feel the way you do, it’s because they may have been abused. Is this happening to you?” Even if a patient is in an abusive setting and she fails to acknowledge it once you have provided an opportunity, allow her to return to discuss it at a later date. Serious injury and homicide often result once a person attempts to leave an abusive partner. Allow her to make the decision to leave. You will have indicated your support.
The global prevalence of child sexual abuse has been estimated at 19.7% for females and 7.9% for males, according to a 2009 study published in Clinical Psychology Review that examined 65 studies from 22 countries. According to the National Child Abuse and Neglect Data System, whose latest statistics are for 2005, an estimated 3.3 million referrals of child abuse or neglect were received by public social service agencies. Of these referrals, 899,000 children were confirmed to be victims of abuse or neglect (U.S. Department of Health and Human Services, 2007). That means approximately 12 out of every 1000 children up to age 18 in the United States were found to be victims of maltreatment in 2005.
A history of childhood sexual abuse is nearly always associated with enduring physical and psychological sequelae. There are many somatic disorders that may result after abuse. These include eczema, sleep disorders, sexual dysfunction, substance abuse, eating disorders, headaches, “mystery” pain, depression, asthma, and a wide variety of phobias. Health care providers have an ethical and legal responsibility to report all cases of suspected child abuse and to protect the child from further abuse. Any injury that cannot be adequately explained should raise concern about either nonaccidental injury or neglect. Injuries to the skin are seen in 90% of abused children (see Figure 21-32). Multiple injuries in various stages of healing almost always indicate repeated beatings.
Male rape is also on the rise. According to the District of Columbia Rape Crisis Center, 1 of every 7 boys in the United States is raped before 18 years of age. Every year, men experience 2.9 million assaults. Most male rape victims are raped by other men, in the sense that they are forced to submit to anal intercourse, masturbation of the offender, oral sex, or other sex acts. Information about male rape is scarce because male victims, like their female counterparts, feel humiliation and shame and are reluctant to report it. Many men believe that if they have been raped by another man, it implies that the victim has homosexual tendencies.
Reproductive and Gynecologic History
The reproductive and gynecologic history obtains information about a woman’s age at menarche, regularity of menstrual flow, and duration of periods. In addition, the number of pregnancies, number of deliveries, number of abortions (spontaneous or induced), and complications of pregnancies are included in this part of the history. It is also vital to determine whether the woman was exposed to diethylstilbestrol through her mother’s use during pregnancy. This is particularly important in any woman born before 1975. Other important questions are discussed in Chapter 16, Female Genitalia.
In the reproductive history for a man, it is important to inquire about sexual interest, function, satisfaction, and any sexual problems. Has the man been unable to procreate? If so, is he aware of the reason? Other questions for men are discussed in Chapter 15, Male Genitalia and Hernias.
Review of Systems
The review of systems summarizes in terms of body systems all the symptoms that may have been overlooked in the history of the present illness or in the medical history. By reviewing the list of possible symptoms in an orderly manner, the interviewer can specifically check each system and uncover additional symptoms of “unrelated” illnesses not yet discussed. The review of systems is best organized from the head down to the extremities, and the questions can be asked during the physical examination of that body area. Patients are told that they are going to be asked whether they have ever had a particular symptom and should answer “yes” or “no.” If they answer in the affirmative, further direct questioning is appropriate. The interviewer need not repeat questions that were previously answered, unless clarification of the data is necessary.
Table 1-1 is the review of systems, about which questions should be asked of all patients. The questions should be understandable to the patient. For example, a question regarding paroxysmal nocturnal dyspnea should be asked in this manner:
Each of the organ- and system-specific chapters that follow discusses the review of symptoms in more detail. Hints about specific questioning and pathophysiologic features of the symptoms are also provided.
Sometimes, a patient may answer all the questions in the affirmative. If the interviewer detects that this is occurring, it may be useful to ask a question about a physiologically impossible condition. For example, if a patient answers “yes” when asked, “Do your stools glow in the dark?” the interviewer should not continue with the review of systems. The interviewer can state in the written history or in the verbal presentation that “the patient has a positive review of systems.”
Because the goal of the medical history is to acquire as much information about each illness as possible, other specific questions related to the particular patient may be indicated. Look at the patient shown in Figure 1-2. Note the large jaw and nose. If you saw such a patient, you might try to determine when the facial changes occurred. In such a case, you could ask the man whether he has noticed a change in his hat or baseball cap size and when he first noticed it.
Figure 1–2 Acromegaly: facial characteristics.
Look at Figure 1-3, in which the right hand of the same patient (on the right) is compared with the right hand of a normal individual. Asking about a change in glove size would be useful with this particular patient. It would be appropriate to inquire whether there has been a change in shoe size as well.
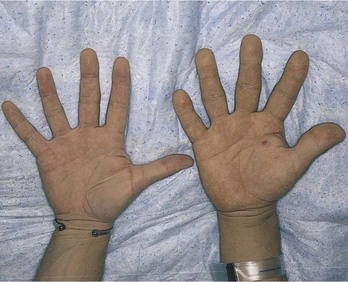
Figure 1–3 Acromegaly: characteristics of hands. Note the stubby fingers of the patient on the right, compared with the fingers of a normal hand on the left.
A useful bit of information may be an old photograph of the patient to help determine when the suspected changes occurred. Compare Figure 1-2 with the photograph in Figure 1-4 (of the same patient taken 20 years earlier). Notice the bulging forehead and the prominent jaw in the later photograph. The patient has acromegaly, a condition of abnormal, excess growth hormone secreted by a pituitary tumor. The changes are insidious, occurring over many years. The photograph was helpful in determining the changes in bone and soft tissue structure.
Figure 1–4 Photograph of the patient shown in Figure 1-2, taken 20 years earlier. Compare the facial features (i.e., nose and chin) in the two photographs.
Taking Notes
As a novice interviewer, you may feel compelled to take down all of the history for fear that you might forget some important parts. It is best to jot down only short phrases and specific dates and write the entire history up later; do not concentrate more on the notes than on what the patient is saying and his or her body language. If you are using electronic medical records, try to face the patient as you write your note on the computer screen to maintain eye contact.
Concluding Thoughts
A medical history must be dynamic. Every history is different. All patients are asked the standard questions, but each patient should be evaluated individually. There is no limit to the questions to be asked.
The written history is a permanent, legal document of the patient’s health history. The information that is recorded must be accurate and objective. On the basis of all the information gleaned from the patient’s history, the interviewer carefully summarizes all the data into a readable format. Anything that is written in a patient’s record could be presented to a court of law. Only objective data should be included. Opinions or statements about previous care and therapy must be avoided.
By convention, when the review of systems is stated or written, all symptoms that the patient has experienced are indicated first. Symptoms never experienced are indicated afterward. The pertinent positive symptoms are symptoms that have possible relevance to the present illness. Pertinent negative symptoms are symptoms that are not present but are often related to the present illness.
If information in the review of systems has been described previously—in the history of present illness, for example—it is correct to indicate under the systems review of that symptom, “see history of present illness.”
As you proceed with the interview, you may sense that it is not going well. Is the patient comfortable? Is there a language barrier? Did you say or do something to interfere with the rapport? Is the patient intimidated? Is the patient concerned about confidentiality? Is the patient reluctant to talk in the presence of family members? Is the patient able to express his or her feelings? These issues reflect just a few of the common reasons for lack of progression of an interview. If you can alleviate the problems, do so. If you notice that the patient has suddenly become less communicative, you could say, “Is there anything that I have said or have asked that has made you upset?” Perhaps interviewing the patient on another day but using the same approach will be more successful.
Putting the Patient at Ease
The key to success in an interview is the ability to put the patient at ease. To do so, the interviewer must be relaxed. What techniques are available to the interviewer and patient to relax? One useful approach is the visualization of color; for example, if the interviewer were to say, “Close your eyes and visualize the color blue,” the patient would feel a definite response in body as well as in mind. If the patient were then to let that image dissolve, take a few breaths, close the eyes again, and visualize the color red, he or she would notice that the response to this color is quite different. Red creates a different state of mind than do blue, green, yellow, and so forth.
Whether this is entirely a result of psychological association is irrelevant to this discussion. The point is that because people respond strongly to color, interviewers can influence the state of mind of patients and themselves by suggesting an atmosphere of color that calms, warms, cheers, cools, and so forth, depending on what is called for in the situation. Because color can help a patient relax, it can have beneficial effects on blood pressure, heart rate, and other bodily functions.
The same is true of the visualization of environments that are pleasant, beautiful, and peaceful. Having the patient take a few moments, with eyes closed, to imagine himself or herself in a garden or a quiet pine forest can substantially lessen nervousness and tension. The connection between relaxation and health is becoming more widely understood and accepted. According to studies in behavioral medicine, the practice of meditation has a beneficial effect in the treatment of hypertension, some heart problems, depression, and anxiety, among other illnesses.
Many visualization techniques are far from new. In the Tibetan approach to medicine, a system that developed between the fourth and twelfth centuries, there is a direct connection between the state of a person’s mind and the state of his or her health.
In the next chapter, the patient’s responses to the questions are investigated, and the influence of background and age on those responses is observed.
The bibliography for this chapter is available at studentconsult.com.
Bibliography
Abraham JL. Management of pain and spinal cord compression in patients with advanced cancer. ACP-ASIM End-of-Life Care Consensus Panel. American College of Physicians–American Society of Internal Medicine. Ann Intern Med. 1999;131:37.
Adler G, Buie DH. The misuses of confrontation with borderline patients. Int J Psychoanal Psychother. 1972;1:109.
Advisory Committee on Immunization Practices. Recommended adult immunization schedule: United States, 2013. Ann Intern Med. 2013;158:191.
American Humane Association. Child sexual abuse. http://www.americanhumane.org/children/stop-child-abuse/fact-sheets/child-sexual-abuse.html; 2013 [Accessed February 1] .
Centers for Disease Control and Prevention (CDC). Prevention of Hepatitis A through active or passive immunization. Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep. 2006;55(RR07):1 http://www.cdc.gov/mmwr/preview/mmwrhtml/rr5507a1.htm.
Barrier PA. Domestic violence. Mayo Clin Proc. 1998;73:271.
Benson H, Klipper MZ. The relaxation response. Wing Books: New York; 1975.
Berkman ND, et al. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med. 2011;155:97.
Bernstein J. Conversations in public places. J Commun. 1975;25:85.
Bradley KA, et al. Screening for problem drinking: comparison of CAGE and AUDIT. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. J Gen Intern Med. 1998;13:379.
Brady AK. Medical Spanish. Ann Intern Med. 2010;152:127.
Breitbart W, et al. The undertreatment of pain in ambulatory AIDS patients. Pain. 1996;65:243.
Brown BL, Strong WJ, Rencher AC. Perceptions of personality from speech: effects of manipulation of acoustical parameters. Acoust Soc Am J. 1973;54:29.
Buchwald D, et al. The medical interview across cultures. Patient Care. 1993;27:141.
Buckman R. How to break bad news: a guide for health care professionals. Johns Hopkins University Press: Baltimore; 1992.
Bush B, et al. Screening for alcohol abuse using the CAGE questionnaire. Am J Med. 1987;83:231.
Centers for Disease Control and Prevention. State-specific smoking-attributable mortality and years of potential life lost—United States, 2000–2004. MMWR Morb Mortal Wkly Rep. 2009;58(02):29 http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5802a2.htm.
Centers for Disease Control and Prevention. 2012 Surgeon General’s report—preventing tobacco use among youth and young adults. [Updated May 15, 2012. Available at] http://www.cdc.gov/tobacco/data_statistics/sgr/2012/index.htm [Accessed January 31, 2013] .
Centers for Disease Control and Prevention. 2012 vaccine recommendations: what they mean for you. [Updated February 17, 2012. Available at] http://www.cdc.gov/Features/AdultVaccines/ [Accessed January 2013] .
Centers for Disease Control and Prevention. Commit to Quit Smoking in 2013. [Updated December 24, 2012. Available at] http://www.cdc.gov/Features/SmokingCessation/ [Accessed January 31, 2013] .
Centers for Disease Control and Prevention. Immunization schedules. [January 29, 2013. Available at] http://www.cdc.gov/vaccines/schedules/hcp/adult.html [Accessed January 31, 2013] .
Chafetz ME. No patient deserves to be patronized. Med Insight. 1970;2:68.
Chapman A. Body language: how to read body language signs and gestures—non-verbal communications—male and female, for work, social, dating, and mating relationships, 2009-2012. [Available at] http://www.businessballs.com/body-language.htm [Accessed February 1, 2013] .
Cherpitel CJ. Performance of screening instruments for identifying alcohol dependence in the general population, compared with clinical populations. Alcohol Clin Exp Res. 1998;22:1399.
Cleeland CS, et al. Pain and treatment of pain in minority patients with cancer. The Eastern Cooperative Oncology Group Minority Outpatient Pain Study. Ann Intern Med. 1997;127:813.
Cleeland CS, et al. Pain and its treatment in outpatients with metastatic cancer. N Engl J Med. 1994;330:592.
Coulehan JL, et al. “Let me see if I have this right . . .”: words that build empathy. Ann Intern Med. 2001;135:221.
Eisenberg DM. Advising patients who seek alternative medical therapies. Ann Intern Med. 1997;127:67.
Ende J, Rockwell S, Glasgow M. The sexual history in general medicine practice. Arch Intern Med. 1984;144:558.
Ewing JA. Detecting alcoholism: the CAGE questionnaire. JAMA. 1984;252:1905.
Faust S, Drickey R. Working with interpreters. J Fam Pract. 1986;22:131.
Fields R. Drugs in perspective: a personalized look at substance use and abuse. ed 4. McGraw-Hill: Boston; 2001.
Fiellin DA, Reid MC, O’Connor PG. Outpatient management of patients with alcohol problems. Ann Intern Med. 2000;133:815.
Fiore AE. Hepatitis A transmitted by food. Clin Infect Dis. 2004;38:705.
Flores G. Language barriers to health care in the United States. N Engl J Med. 2006;355:229.
Haffner L. Translation is not enough: interpreting in a medical setting. West J Med. 1992;157:255.
Hardt E, Jacobs EA, Chen A. Insights into the problems that language barriers may pose for the medical interview. J Gen Intern Med. 2006;21:1357.
Hewitt LN, Bhavsar P, Phelan HA. The secrets women keep: intimate partner violence screening in the female trauma patient. J Trauma. 2011;70:320.
Holland JC, et al. The role of religious and spiritual beliefs in coping with malignant melanoma. Psychooncology. 1999;8:14.
Johnson CV, Mimiaga MJ, Bradford J. Health care issues among lesbian, gay, bisexual, transgender and intersex (LGBTI) populations in the United States: introduction. J Homosex. 2008;54:213.
Landrigan PJ, Baker DB. The recognition and control of occupational disease. JAMA. 1991;266:676.
Larsen KM, Smith CK. Assessment of nonverbal communication in the patient-doctor relationship. J Fam Pract. 1981;12:48.
Levinson W. Physician-patient communication: a key to malpractice prevention. JAMA. 1994;272:1619.
Levinson W, Gorawara-Bhat R, Lamb J. A study of patient clues and physician responses in primary care and surgical settings. JAMA. 2000;284:1021.
Levinson W, et al. Physician-patient communication: the relationship with malpractice claims among primary care physicians and surgeons. JAMA. 1997;277:553.
Marvel MK, et al. Soliciting the patient’s agenda: have we improved? JAMA. 1999;281:283.
Matthews D, Hingson R. Improving patient compliance: a guide to physicians. Med Clin North Am. 1977;61:879.
Mayfield D, McLeod G, Hall P. The CAGE questionnaire: validation of a new alcoholism screening instrument. Am J Psychiatry. 1974;131:1121.
McEwen BS. Protective and damaging effects of stress mediators. N Engl J Med. 1998;338:171.
Medline Plus, National Institutes of Health. Prescription drug abuse. [Available at] http://www.nlm.nih.gov/medlineplus/prescriptiondrugabuse.html [Accessed July 31, 2013] .
Meier DE, Morrison RS, Cassel CK. Improving palliative care. Ann Intern Med. 1997;127:225.
Molyneux A. Nicotine replacement therapy. BMJ. 2004;328:454.
Morrison RS, et al. “We don’t carry that”—failure of pharmacies in predominantly nonwhite neighborhoods to stock opioid analgesics. N Engl J Med. 2000;342:1023.
Mostaghimi A, Crotty BH. Professionalism in the digital age. Ann Intern Med. 2011;154:560.
Moyer VA, et al. Screening for intimate partner violence and abuse of elderly and vulnerable adults: US Preventative Services Task Force Recommendation Statement. Ann Intern Med. 2013;158:478.
Mutsch M, et al. Hepatitis A virus infections in travelers, 1988–2004. Clin Infect Dis. 2006;42:490.
Myerscough PR. Talking with patients: a basic clinical skill. Oxford University Press: Oxford, UK; 1992.
National Institute of Alcohol and Alcoholism. What is a standard drink? [Available at] http://www.niaaa.nih.gov/alcohol-health/overview-alcohol-consumption/standard-drink [Accessed January 2013] .
National Institute on Drug Abuse. Screening for drug use in medical settings. [April 2009. Available at] http://www.drugabuse.gov/sites/default/files/pdf/screening_qr.pdf [Accessed January 26, 2013] .
National Institutes of Health. Helping patients who drink too much: a clinician’s guide. [Available at] http://www.niaaa.nih.gov/publications/clinical-guides-and-manuals/helping-patients-who-drink-too-much-clinicians-guide [Accessed January 31, 2013] .
Neufeld B. SAFE questions: overcoming barriers to the detection of domestic violence. Am Fam Physician. 1996;53:2575.
O’Hanlan KA, et al. A review of the medical consequences of homophobia with suggestions for resolution. J Gay Lesbian Med Assoc. 1997;1:25.
Ong LML, et al. Doctor-patient communication: a review of the literature. Soc Sci Med. 1995;40:903.
Patnode CD, et al. Primary care-relevant interventions for tobacco use prevention and cessation in children and adolescents: a systematic evidence review for the U.S. Preventive Services Task Force. Ann Intern Med. 2013;158:253.
Peabody FW. The care of the patient. JAMA. 1927;88:877.
Platt FW, et al. “Tell me about yourself”: the patient-centered interview. Ann Intern Med. 2001;134:1083.
Post SG, Puchalski CM, Larson DB. Physicians and patient spirituality: professional boundaries, competency, and ethics. Ann Intern Med. 2000;132:578.
Puchalski CM, Romer AL. Taking a spiritual history allows clinicians to understand patients more fully. J Palliat Med. 2000;3:129.
Samet JH, Rollnick S, Barnes H. Beyond CAGE: a brief clinical approach after detection of substance abuse. Arch Intern Med. 1996;156:2287.
Sanders SA, Reinisch JM. Would you say you “had sex” if . . . ? JAMA. 1999;281:275.
Sargent JD, DiFranza JR. Tobacco control for clinicians who treat adolescents. CA Cancer J Clin. 2003;53:102.
Schenker Y, et al. Navigating language barriers under difficult circumstances. Ann Intern Med. 2008;149:264.
Sloan RP, Bagiella E, Powell T. Religion, spirituality, and medicine. Lancet. 1999;353:664.
Snyder L, for the American College of Physicians Ethics, Professionalism, and Human Rights Committee. American College of Physicians Ethics Manual. [6th ed] Ann Intern Med Suppl. 2012;156(1):73.
Spiro II. What is empathy and can it be taught? Ann Intern Med. 1992;116:843.
Steiner JF, Earnest MA. The language of medication-taking. Ann Intern Med. 2000;132:926.
Suchman AL, et al. A model of empathic communication in the medical interview. JAMA. 1997;277:678.
Sudore RL, Fried TR. Redefining the “planning” in advance care planning: preparing for end-of-life decision making. Ann Intern Med. 2010;153:256.
Tomlinson J, Milgrom ET. Taking a sexual history. West J Med. 1999;170:284.
Tonstad S, et al. Effect of maintenance therapy with varenicline on smoking cessation: a randomized controlled trial. JAMA. 2006;296:64.
Travis LB, et al. Cancer survivorship—genetic susceptibility and second primary cancers: research strategies and recommendations. J Natl Cancer Inst. 2006;98(1):15.
U.S. Department of Health and Human Services. Interpret too: working with interpreters in clinical settings. [Available at] https://www.thinkculturalhealth.hhs.gov/pdfs/InterpretTool.pdf [Accessed January 31, 2013] .
U.S. Department of Health and Human Services. The health consequences of smoking: a report of the Surgeon General. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health: Atlanta, Ga; 2004 http://www.surgeongeneral.gov/library/reports/smokingconsequences/.
U.S. Department of Health and Human Services. Health Information Privacy. [Available at] www.hhs.gov/ocr/privacy/ [Accessed January 31, 2013] .
Vertosick FT. Why we hurt: the natural history of pain. Harcourt: New York; 2000.
Victor JC, et al. Person-to-person transmission of hepatitis A virus in an urban area of intermediate endemicity: implications for vaccination strategies. Am J Epidemiol. 2006;163:204.
Zimmerman GL, Olsen CG, Bosworth MF. A “stages of change” approach to helping patients change behavior. Am Fam Physician. 2000;61:1409.
1 Note: This is probably a better question than the first question since it eliminates cultural differences in describing pain.
2 Drink more than you intended or have an additional drink after you decided you had had enough.
3 As a cure for anxiety, depression, or the “shakes.”
4 Buying enough alcohol just in case “company” arrives.