CHAPTER 29 The Immature Spine and Athletic Injuries
Most spine injuries in athletically active children and adolescents are chronic, resulting from repetitive demand on the immature spine during participation in sports. The most serious injuries are acute as a result of direct trauma. The age at which a child can be considered an athlete varies and may be 3 years old when a child puts on skis or 10 years old when he or she begins to ride bulls (Fig. 29–1). Several sports, such as skiing, football, and horseback riding, involve increased risk of acute traumatic events, making spine fracture a significant concern when considering an adolescent athlete. This chapter discusses the initial evaluation and on-field management of spine fractures; the complete treatment of spine fractures is covered elsewhere.
According to surveys of patients seen in sports medicine specialty clinics, the most common cause of back pain in adolescent athletes is stress fracture, or spondylolysis. Spine hyperextension and repeated twisting contribute to the high rate of spondylolysis seen in sports such as gymnastics, football, and weightlifting. The rate of spondylolysis in gymnasts is 20% compared with 5% to 6% in the general population.1
Principles of Diagnosis
History
The term interview implies an interaction with the patient as opposed to the traditional notion of extracting information from the patient. When allowed to tell his or her story, an adult patient takes an average of 90 seconds.2 Adolescents tend to be more taciturn and talk less than the average adult. The average physician cuts off the patient with a question after 18 seconds because he or she has formed a differential diagnosis. Such interruption stops the flow of information, and often the patient is never permitted to relate pertinent facts.
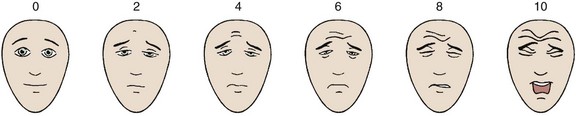
The use of a visual pain scale facilitates consistent documentation. The patient’s assessment of the intensity of the pain using a visual scale (Fig. 29–2) often stimulates a description of the circumstances that exacerbate or alleviate that pain. When making the differential diagnosis, the physician can classify the clinical syndrome into one of three categories: (1) nonmechanical back or leg pain (or both), (2) mechanical back or leg pain (or both), and (3) sciatica.
Warning signs for possible cancer include a history of cancer or constitutional symptoms such as fever or weight loss. Risk factors for infection include a history of recent bacterial infection, intravenous drug use, or an immunocompromised state. Patients with a spine cancer or spine infection often have pain that is not diminished by rest. Warning signs of possible spine fracture are major trauma (e.g., motor vehicle accident, blunt trauma, fall from a height), prolonged corticosteroid use, and osteoporosis. Symptoms suggestive of cauda equina syndrome, which requires urgent surgical consultation, include saddle anesthesia (found in 75% of patients); recent onset of bladder or bowel dysfunction (with urinary retention the most common symptom); and severe or progressive weakness of the lower extremities,3 especially involving both lower extremities.
There are several findings to note when ascertaining psychosocial contributions to nonorganic back pain, as follows4:
Genetics
The “wild card” in the etiology of sciatic pain is genetics. Ala-Kokko5 noted that scientific studies have identified specific versions of the genes encoding collagen, aggrecan, vitamin D receptor, and matrix metalloproteinase-3 that have significant associations with lumbar disc disease. Many other genes may also play a role in disc disease.6–8
Imaging
The Cochrane group performed a meta-analysis of the literature and concluded that there is no correlation between radiographic changes and back pain.9 Contrary to that opinion, researchers in Tokyo reported a study in which they correlated preparticipation spinal radiographs with the incidence of back pain and disability among young football players.10 They followed 171 high school and 742 college football players over a 1-year period. High school players with spondylolysis had a higher incidence of low back pain (79.8%) than players with no radiographic abnormality (37.1%). College players with spondylolysis, disc space narrowing, and spinal instability had a higher incidence of low back pain (80.5%, 59.8%, and 53.5%) than players with normal radiographs (32.1%). College players with spondylolysis had a higher incidence of low back pain than players with disc space narrowing and spinal instability.
Single Photon Emission Computed Tomography
With single photon emission computed tomography (SPECT), gamma camera detectors rotate around the patient in small increments (usually 3- or 6-degree steps), and emission data are obtained from different plane angles. Computer algorithms break the image into pixels, each of which represents an approximately 6-mm area of the planar image. Pixel data are used to render clinically useful volumetric images. SPECT is arguably the best screening examination for significant spinal abnormality versus nonspecific back pain in children and the first examination that should be ordered. Auerbach11 showed that SPECT exceeded MRI or plain radiography in accurately defining spondylolysis in a series of 100 children with significant back pain.
Principles of Treatment and Rehabilitation
Acute Treatment
When pain onset is acute and severe, bed rest may be necessary for 2 or 3 days for initial pain control. A longer period of bed rest quickly becomes counterproductive. The key to recovery is modified activity within a minimal range to start, followed by gentle progression of activity. The sooner the athlete begins a level of tolerated activity, the quicker and more effective is the recovery. Research and experience have dispelled the notion that prolonged absolute rest is beneficial for treatment of back pain.12
Bracing
Bracing is effective in some cases, if used intermittently and primarily as a tool for returning to activity. If used as a “crutch,” extended time in a brace produces atrophy and loss of motion. The Cochrane Collaboration reported a meta-analysis on the use of braces for low back pain in 2004.13 There was moderate evidence that lumbar supports are no more effective for primary prevention than other types of treatment or no intervention. The authors found no data promoting the effectiveness of lumbar supports for secondary prevention. This opinion is consistent with the generally held concept that passive treatment such as bracing should be limited to acute pain relief and that active rehabilitation is an early goal for return to participation in sports and prevention of future injury. Spinal manipulation can provide short-term improvement, but the evidence for longer term relief is inconclusive.14
Rehabilitation
Flexibility
Exercise programs that load the spine throughout the range of motion have poorer outcomes. Greater mobility is associated with poorer outcomes as well. The range of motion of the spine has little predictability for future low back pain. Programs emphasizing trunk stabilization with a neutral spine have had the most success.16–18 These programs emphasize increasing the range of motion of the hips and knees.
Muscle Performance (Strength versus Endurance)
The term strength is defined as the maximum force a muscle can produce during a single exertion to create joint torque. The term endurance refers to the ability to maintain a force for a period of time. Muscle performance includes strength and endurance. The few studies available suggest that endurance has a much greater prophylactic value than strength.19 The emphasis should be placed on endurance and should precede strengthening exercises in a gradual, progressive exercise program (i.e., longer duration, lower effort exercises).
Deep Water Running and Swimming
Walking in a swimming pool is a gentle strengthening exercise for the back. Deep water running is excellent for treating athletes with back pain. The buoyancy of the water helps to unload the spine. Athletes run in the deep end of a swimming pool, normally with the aid of a flotation vest. Water is about 800 times denser than air, so resistance met during water running is greater than when running on land. Deep water running can help to maintain aerobic performance for 6 weeks in trained endurance athletes; sedentary individuals can appreciate significantly increased maximal oxygen uptake. During spine rehabilitation programs, deep water running can be used for maintenance training, but deep water running is not a substitute for conventional training.20–22 Swimming is an excellent exercise for the back, but caution is advised for the novice. The swimming strokes can produce or exacerbate back injury if proper technique is not practiced.
Program Guidelines
The following caveats should be considered when prescribing and monitoring any “return to sport” rehabilitation program23:
Education
Several studies have documented the value of patient education in the treatment of spine problems.29 Education has been shown to be as valuable to the patient’s recovery as physical therapy. In 2004, Frost and colleagues29 measured the effectiveness of routine physical therapy compared with a single assessment session and advice from a physical therapist for patients with low back pain. They used a multicenter, randomized controlled trial in seven British National Health Service physiotherapy departments. These authors concluded that routine physical therapy was no more effective than a single assessment and advice session from a physiotherapist in treating low back pain.
In the physician’s office, handouts are an excellent source of education and can be reference guides for the patient during rehabilitation activities (Table 29–1). Good preprinted handouts are available from multiple sources, such as the Krames (http://www.krames.com/) or the AAOS (http://www.aaos.org/) websites. Personalizing the handouts gives the athlete assurance in his or her provider’s interest and commitment to the rehabilitation plan and confidence in the treatment plan on leaving the office. With the availability of digital radiography, it is inexpensive to give the patient a copy of his or her radiograph to take home. Being educated regarding the nature of the injury and being part of the rehabilitation team, and not merely the subject, motivates the athlete and can bring about speedier and more complete recovery.
| 1. Use good technique | An overhand pitch produces less strain than a side-arm pitch |
| 2. If it hurts, don’t do it | “No pain—no gain” is a poor concept. You feel the fatigue of a good workout, but you must recognize the pain of going beyond fatigue to injury |
| 3. Stop when fatigued | Avoid the temptation of an extra repetition. Sprints are best done after a rest |
| 4. Increase duration gradually | It takes time for the body to respond to increased demand and to strengthen |
| 5. Rest for a time after major increases | It is better to alternate 3 hard days with an easy day and then rest for 2 days |
| 6. Quit when you are tired | When you have exhausted the glycogen stored in your muscles, your technique falters, and you are prone to injury |
| 7. Do preventive exercises | Keep your body in balance by stretching to gain full range of motion and loosening contractures |
| 8. Remember your old injuries | When you recall your old injuries, you can work to avoid repeating them |
| 9. Warm up slowly | Use gentle stretching and gradually increasing effort to limber up muscles and deep breathing to stimulate the heart and lungs |
Disorders and Treatment
Low Back Pain in Adolescent Athletes
Lumbar spine pain or low back pain accounts for 5% to 8% of athletic injuries.30 Injuries are often due to poor conditioning of the spine, poor biomechanics, or repetitive stresses placed on the spine by the nature of the sport. Overuse injuries from repeated lumbar hyperextension may be common in children participating in sports such as gymnastics, volleyball, and rowing.
Historical studies show that the correct diagnosis of acute low back pain is established on the first visit only 2% of the time. After 6 weeks, the diagnostic accuracy increases to 15%, and it increases to 30% at 3 months.31 The physician’s initial visit is best used to rule out serious disorders, such as disc herniation or malignant disease. Although less than 1% of back pain complaints are related to serious spine pathology or require emergent treatment, such as neoplasm or cauda equina syndrome, it is important to exclude these conditions and reassure the patient accordingly.
Back pain that follows an acute injury is usually attributed to muscle strain. There is little scientific evidence showing muscle strain as a back pain generator, however, probably because pain produced by an injury cannot be differentiated to the various soft tissues of the back.32 The pain may be localized or diffuse. The patient frequently relates that more stiffness occurred after a night’s sleep. This type of back pain attributed to muscle strain tends to improve with time.
Mechanical backache secondary to poor posture is more common in sedentary children. Athletic children are less likely to report nonspecific back pain than their nonathletic counterparts. Children who do not walk to school and have a poor self-image of their health in general report more back pain. Multivariate analysis showed that the incidence of low back pain in adolescents is inversely related to time spent doing physical activity (e.g., regular walking or bicycling) and directly related to television or computer time.33
Posture and inactivity contribute to low back pain. The intervertebral discs have the highest fluid content in the morning, which influences the pressure generated on spinal tissues during flexion.34 Avoidance of flexion after arising in the morning significantly reduces nonspecific back pain.35
Spondylolysis
Spondylolysis is a stress fracture of the pars interarticularis. It is generally considered to be a low-risk fracture that heals on its own. The fracture occurs most frequently at L5, followed by L4 and L3. Spondylolysis occurs in 5% to 6% of the general population.1 The lesion is usually asymptomatic and appreciated only incidentally on a radiograph. Generally, no single traumatic event causes spondylolysis; rather, repetitive stress produces fatigue defects, and a single event may complete the fracture. These fractures may develop fibrous nonunion or heal in an elongated state.36
The incidence of pars defects is greater in adolescent athletes than in the general population and is a particular clinical problem for this population.37 Sports that require repetitive hyperextension or extension combined with rotation such as gymnastics, wrestling, and weightlifting are more often associated with a stress fracture of the pars interarticularis. White female gymnasts experience a rate of spondylolysis (11%) five times that of the general white female population.38 Certain participants in sports such as diving, weightlifting, wrestling, and gymnastics have disproportionately high rates of spondylolysis. A study of elite Spanish athletes showed the highest rates of spondylolysis in gymnasts and weightlifters followed by throwing athletes and rowers.39 Other reports suggest that a wide variety of sports increase the risk of spondylolysis, including soccer, volleyball, and baseball.40
A major concern for patients with defects in the pars interarticularis is the progressive development of symptomatic spondylolisthesis. The incidence of progressive spondylolisthesis is low (3% to 10%) and mainly occurs during adolescence.41,42 There is no known correlation between active sports participation and either the occurrence or the progression of spondylolisthesis.
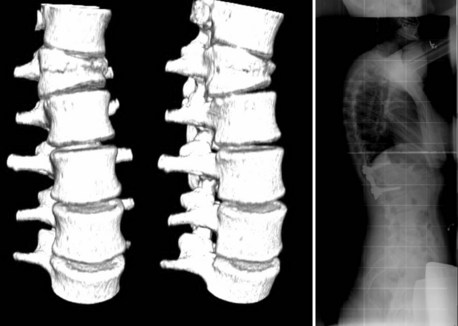
Diagnostic Imaging
A defect in the pars interarticularis is apparent in Figure 29–3, which shows a three-dimensional CT scan. The classic description of this appearance on the oblique view radiograph is that of a collar on the “Scottie dog.” Approximately 20% of the pars interarticularis lesions are seen only on the lateral oblique views, and CT may be necessary to show it.
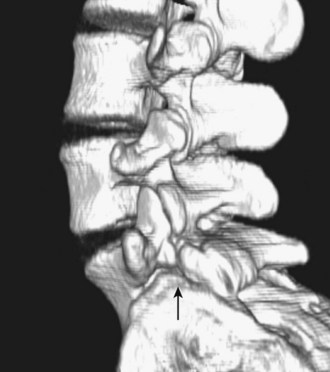
FIGURE 29–3 Spondylolysis. Three-dimensional CT scan shows pars interarticularis defect at end of arrow.
Magnetic resonance imaging should be used as the primary investigation for adolescents with back pain and suspected stress reactions of the pars interarticularis. Single-photon emission computed tomography (SPECT) use is limited by the high rate of false-positive and false-negative results and by considerable ionizing radiation exposure.42a
Treatment
Most patients with symptomatic spondylolysis do well with conservative treatment.43 The main goals of treatment are amelioration of pain, return to activity, and prevention of recurrence. Treatment modalities include rest, medication, and bracing, alone or in combination. Many pars interarticularis lesions heal with early care, particularly early-stage unilateral defects. Osseous healing is unnecessary to achieve an excellent clinical outcome with full return to activities, although this healing is desirable when possible.
Physical therapy has been proved quite effective in the treatment of spondylolysis. Patients with a specific and carefully managed exercise program show significant reduction in pain intensity and functional disability levels.44,45 Therapy should include exercises to increase hamstring flexibility and to strengthen deep core muscles in the abdomen and the lumbar region.46
Various studies have determined that only 9% to 15% of cases of symptomatic spondylolysis or grade 1 spondylolisthesis require surgery.42,47–49 The indications for surgery are progressive slip, intractable pain, development of neurologic defects, and segmental instability associated with pain. Pain alone can be controlled by activity modification and medication and is not an indication for surgery. Surgical treatment is directed at repairing the fracture in the pars interarticularis using bone grafting and internal fixation. Various techniques using wires and screws have been advocated. The technique by Chen and Lee,50 using a pedicle screw and laminar hook, has the advantage of not violating the facet joints, while providing excellent stabilization for healing.
Spondylolisthesis
Spondylolisthesis occurs when there is a bilateral defect in the pars interarticularis and one vertebra slips forward relative to the vertebra beneath it. The incidence of spondylolisthesis in athletes is the same as in the general population. No substantiated criteria are available for predicting which cases of spondylolysis will progressively slip, resulting in spondylolisthesis. Patients with dysplastic posterior elements have a higher risk of slip progression. Radiographic studies have shown a strong correlation between slip progression and a more vertical inclination of the superior plate of S1.51,52 Most cases of spondylolisthesis are mild, unlikely to progress, and cease to progress after growth is complete. With mild spondylolisthesis, there is no increased rate of disability and no reason to restrict participation in sports.
Symptoms associated with spondylolisthesis are dull low back pain exacerbated by activity, particularly hyperextension and rotation. Sports requiring repetitive rotation and extension under load, such as gymnastics, football, wrestling, hockey, pole vaulting, diving, and throwing sports, have been incriminated as causative factors in multiple studies.53,54 Typical of mechanical-type pain, rest tends to alleviate the pain.
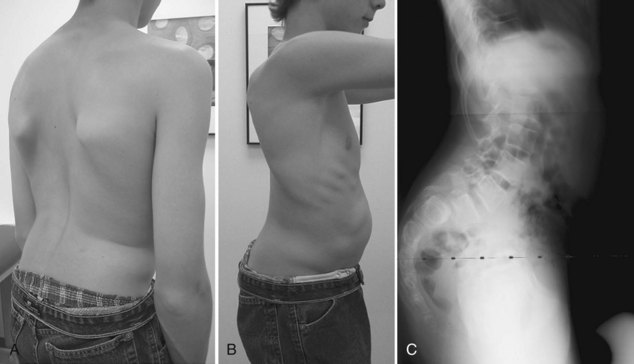
During the examination the findings of paravertebral muscle spasm, hamstring contractures, and limited flexibility may be dramatic. Kyphosis associated with severe grades of slip flattens the profile of the buttocks and creates a sagittal postural malalignment (Fig. 29–4). A step-off at the lumbosacral level may be palpable.
Weakness, loss of sensation, and a positive straight-leg raise test are usually absent, differentiating spondylolisthesis from a herniated disc. If radiculopathy is present, the L5 root is usually involved. Cauda equina syndrome has been reported in severe cases owing to nerve root stretch over the dome of the sacrum.55
The diagnosis is easily confirmed by a lateral radiograph of the lumbar spine. The severity of the slip is graded either by the quartile classification of Meyerding or, more commonly, as a percentage of displacement relative to the top of the sacrum. There is consensus that kyphosis is a more important measure of the deformity than displacement.56 The slip angle and sacral inclination are used to describe the sagittal plane deformity.
If the patient still has unremitting, disabling pain after a 6-month program of conservative treatment, certain surgical decisions are made: in situ fusion versus reduction, whether to perform decompression, whether to perform anterior and posterior fusion, and plus or minus bed rest. The debate over these issues remains. In situ fusion is the “gold standard” with well-documented long-term excellent outcomes.57 Isolated removal of the laminar fragment, or Gill procedure, is contraindicated because further progression is common after that procedure.
Absolute indications for decompression are motor deficit and bowel or bladder dysfunction.56 Some surgeons do not perform decompression even with motor or sensory signs because these signs tend to improve with a solid fusion.58 Many surgeons perform a decompression at the time of fusion if weakness, sensory loss, or radicular pain is present, particularly in instances of severe slip. With severe degrees of slip, anterior fusion with or without reduction of the kyphotic deformity can be done using pedicle screw fixation and anterior interbody cages.
Lumbar Scheuermann Disease (Juvenile Disc Disease)
The classic radiographic criteria for the diagnosis of Scheuermann disease is kyphosis of the thoracic spine with wedging of 15 or more degrees over three vertebrae.59 Scheuermann disease is associated with endplate changes such as irregularity of the apophyseal ring and Schmorl nodes. The causes of Scheuermann disease, which has been attributed to juvenile osteoporosis, are controversial. This condition affects 0.4% to 8.3% of the general population and causes irregularities in ossification and endochondral growth in the thoracic spine in adolescents and young adults.59 The disease leads to various pathologic changes at the junction of the vertebral body and the intervertebral disc, resulting in pronounced wedging of the vertebral bodies and progressive kyphosis in severe cases. According to various studies, it causes back pain in 20% to 60% of cases and occasionally causes severe deformity of the spine.59
An increased frequency of radiologic abnormalities of the thoracolumbar spine has been reported among young athletes in various sports, such as soccer, gymnastics, water-ski jumping, or wrestling, compared with nonathletes.60–70 Although the origins of typical Scheuermann disease71 have been a matter of controversy,67,72 atypical Scheuermann disease is considered to be strongly associated with trauma or excessive loading of the spine, especially in the flexed posture and during growth spurts.60,67,73 Axial compression forces apparently cause vertebral endplate bulging, whereas compression of the immature spine in flexion is considered to cause anterior intravertebral disc herniation (marginal Schmorl nodes).61,66,67,72–75 Abnormalities of the vertebral ring apophysis are thought to be the result of failure in tension shear, analogous to Osgood-Schlatter avulsion at the knee (Fig. 29–5).68
In 1985, Greene and colleagues72 described back pain and vertebral changes in the lumbar spine similar to changes seen in Scheuermann disease of the thoracic spine. These changes were accompanied by mechanical low back pain. In 1994, Heithoff and colleagues76 saw similar changes on MRI and coined the term juvenile discogenic disease. Their group detected evidence of thoracolumbar Scheuermann disease and multilevel disc disease of the lower lumbar spine in 9% of the subjects studied. The patients ranged in age from 7 to 66, but most were young: Slightly less than half of the patients were younger than 30; 9% were younger than 21. Males outnumbered females 3 : 1. Disc degeneration was found most frequently at the L5-S1 level, followed in order by L4-5 and L3-4. Of patients, 80% showed evidence of substantial degeneration at more than one lumbar level, and 53% had disc herniations involving at least one lower lumbar level.
Heithoff and colleagues76 suspected that a substantial number of young adults have a combination of painful multilevel disc degeneration and lumbar spine changes typical of Scheuermann disease. In their view, both conditions may be caused by an underlying genetic defect in disc structure. It has been estimated that 80% of young patients requiring disc surgery have a genetic predisposition to disc degeneration.76 Juvenile discogenic disease has been statistically associated with athletic activity and repetitive trauma. Most patients can be treated nonoperatively, but a subset have concurrent spinal stenosis, which may require decompression.77
Herniated Nucleus Pulposus
Acute disc herniation, or HNP, is relatively rare in children and adolescents compared with adults. Reports suggest that only 0.5% to 4% of surgically managed HNP occurs in patients younger than 18.78–82 Despite the low incidence, approximately 10% of severe back pain in skeletally immature patients is due to disc herniation.83,84 High-risk activities include weightlifting and collision sports such as football.84 HNP has also been associated with injuries sustained during gymnastics, basketball, baseball, and wrestling.85 Nearly 95% of herniations occur from L4 to S1 and are fairly evenly distributed between L4-5 and L5-S1.80,85 The L3-4 level is affected in only 5% of patients.85
The presenting symptoms of HNP in children differ from the symptoms seen in adults. The profile of an adolescent with HNP includes the presence of tension signs and sciatic scoliosis, without localizing neurologic signs. Most patients present with low back pain, with or without leg pain.84,85 Associated leg pain is seen far less often than in adults (<20% of the time).74 In children, the herniation is thought to be more central and the volume of extruded disc material less than in adults.79,84 Actual rupture of the disc is rare in children.86
Physical examination often reveals an abnormal gait or scoliosis owing to paraspinal muscle spasm.84,85 Nerve tension signs, such as a positive straight-leg raise test, are present in greater than 80% to 90% of patients, and the crossed-leg raise test is positive in more than 50%.79,84,85,87 Objective motor weakness may be present in 40%, with the extensor hallucis longus most commonly affected, and deep tendon reflexes at the knee and ankle are decreased in approximately 40% of patients.85
MRI is a very effective way to image the disc, spinal cord, and nerve roots and because of its noninvasive nature is a commonly used imaging technique. MRI has been shown to detect 100% of symptomatic herniations (Fig. 29–6).88 Herniation is associated with endplate changes, with marrow signal intensity changes on MRI, and with increased cartilage in the material removed during surgery. There is a correlation of marrow signal intensity changes on MRI and the biology of the removed material. Avulsion-type disc herniation is common.89
Conservative treatment is as outlined for nonspecific low back pain. The literature suggests, however, that the overall outcomes of conservative treatment are generally poor. Recommendations suggest a 2- to 4-week trial of conservative management followed by surgical excision of the disc if symptoms have not resolved.85
Indications for surgical excision of the disc include persistent symptoms despite conservative management, cauda equina syndrome, progressive neurologic deficits, and reinjury.84,85 Many authors have reported greater than 90% good to excellent results after surgical excision.80,82,85,90 After surgical excision, low back pain and leg pain resolved within 3 weeks, and neurologic findings resolved after 3 months.80 Long-term follow-up studies show excellent outcomes, including absence of pain and no activity limitations.80,82,90
Apophyseal Ring Fracture
Bone fragments at the posterior vertebral endplate have been given numerous names, such as posterior marginal node; limbus fracture; fracture of the vertebral rim, ring, or endplate; epiphyseal dislocation; and apophyseal ring fracture.91 This condition is unique to adolescents84 and was first described by Skobowytsh-Okolot in 1962.81,92 Endplate fracture was discovered in 20% of patients younger than 21 years and in 33% of patients younger than 17 who were undergoing lumbar disc surgery.93 The overall prevalence is only 0.07% of all patients of all ages undergoing disc surgery. There is a strong male predominance, with 85% of cases occurring in boys; 66% of cases are related to a traumatic event such as weightlifting, heavy work, or sports injury.81 Associations have also been found with Scheuermann disease.94
Hyperextension of the lumbar spine95 and rapid flexion together with axial compression to the vertebral column such as occurs with weightlifting are two proposed mechanisms of apophyseal ring injury.81,84,96 The presenting symptoms of an apophyseal ring fracture are similar to the symptoms seen with HNP—back, buttock, and posterior thigh pain. Symptoms are worse with coughing, sneezing, sports, and prolonged sitting.84 Pain may radiate down one or both legs. The straight-leg raise test is positive, and contralateral straight-leg raise is frequently positive. Paraspinal muscle spasm, lumbar tenderness, scoliosis, intermittent claudication, paraparesis, and cauda equina syndrome have been reported.81,84
Plain radiographs can be useful and show the avulsed fragment in approximately 40% of cases.81,91 This fragment appears as an arcuate or wedge-shaped bone fragment posterior to the vertebral body or disc space. Alternatively, it can appear as a bony ridge on the posterior surface of the vertebral body. MRI may show a defect in the posterior vertebral rim. The fragment may be seen as a low signal area lying posteriorly but can be difficult to distinguish from cortical bone and posterior longitudinal ligament. MRI may be diagnostic in only 22% of cases.91 CT is an excellent imaging study for these fractures because it can define the bony fragment, any associated disc prolapse, vertebral defect, and severity of any associated stenosis in approximately 75% of cases. CT should be considered if MRI fails to show an expected HNP or ring fracture.91
A trial of short-term rest, use of nonsteroidal anti-inflammatory drugs, and physical therapy is indicated. If symptoms fail to resolve after 2 to 4 weeks or if there is progressive neurologic involvement or cauda equina syndrome, surgical excision of the fragment and any associated disc material should be performed.84 Good to excellent results have been reported after surgical excision in nearly all pediatric cases of avulsed ring fracture.
Cervical Spine Injuries
Traumatic neck injuries in young athletes may be to bone, nerve, or soft tissue. The order of incidence is as follows97:
Field Treatment of Cervical Fractures
Lifting an individual high enough to insert a backboard beneath requires a chief who carefully links the head to the chest and six additional people to lift. If a team has not practiced or there are not six individuals immediately trained and available, the athlete should not be moved until there is adequate assistance to immobilize and transport him or her without incurring additional damage. Instructions for the prehospital care of a spinal cord injury on an athletic field are published online by an interdisciplinary task force.98
Prevention of Catastrophic Injuries to the Cervical Spine in Football
According to Cantu and Mueller99 of the National Center for Catastrophic Sport Injury Research, prevention is related to teaching and enforcing good technique in blocking and tackling and the proper use of well-fitted equipment. Cantu and Mueller99 noted, “The football helmet is not the cause of cervical spine injuries. Poorly executed tackling and blocking technique are the major problems.” The neck should be kept upright, avoiding use of the helmet and facemask as the initial and primary contact point in blocking and tackling. Rules against spearing should be strongly enforced, and athletes should strengthen their necks for further protection in the event of a miss-hit. Cantu and Mueller99–104 stated that being prepared for the treatment and transport of a player with a major spine injury can mean the difference between life and death. That means having a plan and practicing the teamwork necessary for a successful transport.
Cervical Peripheral Nerve Injuries
Stingers or Burners
Symptoms are a severe burning or searing pain in the shoulder and arm associated with loss of sensation and weakness of the arm. The pain may be decreased by abducting the shoulder; this can be achieved by asking the athlete to place a hand on the top of the head. Spurling maneuver is a diagnostic test that reproduces the compression mechanism of injury. The patient’s neck is extended, laterally flexed to the involved side, and rotated to the involved side with axial loading applied while in that position. The burning or searing pain is reproduced. Extension-compression mechanisms are most common, followed by brachial stretch and direct blow mechanisms.105
Initial treatment for this injury is removal from participation and rest, followed by strengthening exercises of the neck and, finally, careful stretching and restoration of range of motion. Because the pain, paresthesias, and weakness typically last only a few seconds or minutes, these injuries fall into the Seddon classification of neurapraxia. Occasionally, athletes with more severe injuries experience a prolonged recovery period that may last hours to several weeks and may lead to a prolonged loss of time from competition.106–113 Return to play criteria include full range of motion of the neck associated with complete return of arm strength and sensation.
Quan and Bird114 proposed a classification of peripheral nerve injuries that correlates well with electrodiagnostic studies and prognoses, based on earlier classifications by Seddon114a and Sunderland.114b This classification scheme is useful for diagnosis and advice in individual cases (Table 29–2).
| Type of Injury | Mode of Recovery | Time to Recovery |
|---|---|---|
| Conduction block (neurapraxia) | Remyelination of focal segment involved | 2-12 wk |
| Limited axonal loss | Collateral sprouting from surviving motor axons | 2-6 mo |
| Intermediate axonal loss | Collateral sprouting and axonal regeneration from site of injury | 2-6 mo |
| Severe axonal loss | Axonal regeneration | 2-18 mo |
| Complete nerve discontinuity | No recovery without nerve grafting | 2-18 mo |
Data from Quan D, Bird SJ: Nerve conduction studies and electromyography in the evaluation of peripheral nerve injuries. Univ Pa Orthop J 12:45-51, 1999.
Cervical Stenosis
Congenital cervical stenosis is a risk factor for cervical spine injuries.115 Two studies have analyzed the relationship of burners to cervical stenosis in college football players at the University of Iowa and Tulane University.105,116 Burners were more common in players with spinal stenosis as defined by the Torg ratio, especially the occurrence of repeated episodes of neurapraxia. The Torg ratio is defined as the ratio of the spinal canal width to the width of the vertebral body at the same level and is most narrow at C7. These studies suggest that a Torg ratio of 0.7 to 0.8 or lower is high risk. For players with cervical stenosis, the risk of burners is three times that of players without stenosis (Fig. 29–7).
Transient Spinal Cord Compression
Torg and colleagues117 described the syndrome of transient quadriplegia, considered to represent a “neurapraxia of the cervical spinal cord.” This syndrome includes bilateral upper extremity and lower extremity neurologic involvement with no associated fracture or dislocation. It usually resolves within 36 hours. The transient quadriplegia was associated with developmental spinal stenosis, either as an isolated entity or associated with congenital abnormalities, cervical instability, or intervertebral disc disease. The authors noted statistically significant spinal stenosis in all patients who incurred episodes of transient quadriparesis.117,118 They also noted that there was “no evidence that the occurrence of neurapraxia of the cervical spinal cord predisposes an individual to permanent neurological injury.”117
Fracture
Fracture of the Thoracolumbar Spine
Fracture or dislocation of the thoracolumbar spine is unusual. The typical mechanism is an axial load, as from a fall onto the buttocks from a height or at a relatively rapid speed. The injury is usually a relatively benign compression fracture occurring in the lower thoracic spine or at the thoracolumbar junction. Some compression fractures are not easily seen on plain radiographs (Fig. 29–8). When there is significant pain or tenderness using spot radiographs, CT or MRI can aid in identification and localization of the fracture. Any neurologic findings require special evaluation.
Iliac Apophysitis
The typical athlete affected is an adolescent runner. Clancy and Foltz119 described a series of 21 young distance runners, in all of whom pain resolved with alteration of training and rest. As the apophysis closes at the end of growth, even the most recalcitrant cases resolve, similar to Osgood-Schlatter disease of the knee. There are a couple of case reports of avulsion of the apophysis in older teenagers that was surgically repaired, but this is rare.120,121
Tumor
Spine cancers in children are rare. Children 7 to 15 years old with spine infection or tumor tend to present with back, pelvic, or abdominal pain.122 Intradural spinal metastasis pain is a characteristically cramping pain. The physician should take note of back pain that increases with recumbency and keeps the patient awake at night. Progressive pain is characteristic of tumors, not trauma-induced pain. The pain of cancer tends to be constant.
Neoplasia of the spine may originate in either the neural or the osseous elements. Most bony spine tumors of childhood are benign, but they usually cause pain or an irritative scoliosis (Fig. 29–9). Osteoid osteoma is a small, sclerotic, irritative lesion of the posterior spinal elements. The pain is worse at night and is relieved by aspirin or other anti-inflammatory drugs. Although the natural history is for spontaneous resolution of the pain over years, patients do not often tolerate long-term pain well.
Key Points
1 Bono CM. Low back pain in athletes. J Bone Joint Surg Am. 2004;86:382-396.
2 Brodke DS, Ritter SM. Nonoperative management of low back pain and lumbar disc degeneration. J Bone Joint Surg Am. 2004;86:1810-1818.
3 Ginsburg GM, Bassett GS. Back pain in children and adolescents: Evaluation and differential diagnosis. J Am Acad Orthop Surg. 1997;5:67-78.
4 McGill SM. Low back exercises: Evidence for improving exercise regimens. Phys Ther. 1998;78:754-765.
5 Salminen JJ, Erkintalo MO, Pentti J, et al. Recurrent low back pain and early disc degeneration in the young. Spine. 1999;24:1316-1321.
6 Standaert CJ, Herring SA. Spondylolysis: A critical review. Br J Sports Med. 2000;34:415-422.
1 Fredrickson B, Baker D, McHolick WJ, et al. The natural history of spondylolysis and spondylolisthesis. J Bone Joint Surg Am. 1984;66:699-707.
2 Langewitz W, Denz M, Keller A, et al. Spontaneous talking time at start of consultation in outpatient clinic: Cohort study. BMJ. 2002;325:682-683.
3 Rydevik B. Neurophysiology of cauda equina compression. Acta Orthop Scand Suppl. 1993;251:52-55.
4 Waddell G, McCulloch JA, Kummel E, et al. Nonorganic physical signs in low-back pain. Spine. 1980;5:117-125.
5 Ala-Kokko L. Genetic risk factors for lumbar disc disease. Ann Med. 2002;34:42-47.
6 Solovieva S, Leino-Arjas P, Saarela J, et al. Possible association of interleukin 1 gene locus polymorphisms with low back pain. Pain. 2004;109:8-19.
7 Tolonen J, Gronblad M, Virri J, et al. Oncoprotein c-Fos and c-Jun immunopositive cells and cell clusters in herniated intervertebral disc tissue. Eur Spine J. 2002;11:452-458.
8 Wang YJ, Lu WJ, Shi Q, et al. Gene expression profile of degenerated cervical intervertebral disc tissues in rats. Chin J Traumatol. 2004;7:330-340.
9 Van Tulder MW, Assendelft WJ, Koes BW, et al. Spinal radiographic findings and nonspecific low back pain: A systematic review of observational studies. Spine. 1997;22:427-434.
10 Iwamoto J, Abe H, Tsukimura Y, et al. Relationship between radiographic abnormalities of lumbar spine and incidence of low back pain in high school and college football players: A prospective study. Am J Sports Med. 2004;32:781-786.
11 Auerbach JA. Towards an evidence-based approach for imaging in evaluation of back pain in children. Ottawa: POSNA; 2005.
12 Brodke D, Ritter S. Nonoperative management of low back pain and lumbar disc degeneration. J Bone Joint Surg Am. 2004;86:1810-1818.
13 van Tulder MW, Jellema P, van Poppel MN, et al: Lumbar supports for prevention and treatment of low back pain. Cochrane Database Syst Rev CD001823, 2000.
14 Meade TW, Dyer S, Browne W, et al. Low back pain of mechanical origin: Randomised comparison of chiropractic and hospital outpatient treatment. BMJ. 1990;300:1431-1437.
15 Ramos G, Martin W. Effects of vertebral axial decompression on intradiscal pressure. J Neurosurg. 1994;81:350-353.
16 Saal JA, Saal JS. Nonoperative treatment of herniated lumbar intervertebral disc with radiculopathy: An outcome study. Spine. 1989;14:431-437.
17 Bridger RS, Orkin D, Henneberg M. A quantitative investigation of lumbar and pelvic postures in standing and sitting: Interrelationships with body position and hip muscle length. Int J Indust Ergonom. 1992;9:235-244.
18 McGill SM, Norman RW. Low back biomechanics in industry in the prevention of injury. In: Grabiner M, editor. Current Issues in Biomechanics. Champaign, IL: Human Kinetics Publishers, 1992.
19 Alaranta H, Luoto S, Heliovaara M, et al. Static back endurance and the risk of low-back pain. Clin Biomech (Bristol, Avon). 1995;10:323-324.
20 Dowzer CN, Reilly T, Cable NT. Effects of deep and shallow water running on spinal shrinkage. Br J Sports Med. 1998;32:44-48.
21 Dowzer CN, Reilly T, Cable NT, et al. Maximal physiological responses to deep and shallow water running. Ergonomics. 1999;42:275-281.
22 Reilly T, Dowzer CN, Cable NT. The physiology of deep-water running. J Sports Sci. 2003;21:959-972.
23 McGill SM. Low back exercises: Evidence for improving exercise regimens. Phys Ther. 1998;78:754-765.
24 McGill S. Low back exercises: Prescription for the healthy back and when recovering from injury. Resource Manual for Guidelines for Exercise Testing and Prescription, 7th ed. Indianapolis: American College of Sports Medicine. 2005.
25 McGill SM. The biomechanics of low back injury: Implications on current practice in industry and the clinic. J Biomech. 1997;30:465-475.
26 Nutter P. Aerobic exercise in the treatment and prevention of low back pain. Occup Med. 1988;3:137-145.
27 Adams MA, Dolan P. Recent advances in lumbar spinal mechanics and their clinical significance. Clin Biomech (Bristol, Avon). 1995;10:3-19.
28 Potvin J, Norman R. Can fatigue compromise lifting safety? Chicago. Proceedings of the Second North American Congress on Biomechanics. August 24-28, 1992:513-514.
29 Frost H, Lamb SE, Doll HA, et al. Randomised controlled trial of physiotherapy compared with advice for low back pain. BMJ. 2004;329:708.
30 Loud KJ, Micheli LJ. Common athletic injuries in adolescent girls. Curr Opin Pediatr. 2001;13:317-322.
31 Nachemson AL. Advances in low-back pain. Clin Orthop Relat Res. 1985;201:266-278.
32 Andersson G. The epidemiology of spinal disorders. In: Frymoyer J, Weinstein J, Ducker T, et al, editors. The Adult Spine: Principles and Practice. Philadelphia: Lippincott-Raven; 1991:107-146.
33 Szpalski M, Gunzburg R, Balague F, et al. A 2-year prospective longitudinal study on low back pain in primary school children. Eur Spine J. 2002;11:459-464.
34 Adams MA, Dolan P, Hutton WC, et al. Diurnal changes in spinal mechanics and their clinical significance. J Bone Joint Surg Br. 1990;72:266-270.
35 Snook SH, Webster BS, McGorry RW, et al. The reduction of chronic nonspecific low back pain through the control of early morning lumbar flexion: A randomized controlled trial. Spine. 1998;23:2601-2607.
36 Cyron BM, Hutton WC. The fatigue strength of the lumbar neural arch in spondylolysis. J Bone Joint Surg Br. 1978;60:234-238.
37 Herman MJ, Pizzutillo PD, Cavalier R. Spondylolysis and spondylolisthesis in the child and adolescent athlete. Orthop Clin North Am. 2003;34:461-467.
38 Jackson DW, Wiltse LL, Cirincoine RJ. Spondylolysis in the female gymnast. Clin Orthop Relat Res. 1976;117:68-73.
39 Soler T, Calderon C. The prevalence of spondylolysis in the Spanish elite athlete. Am J Sports Med. 2000;28:57-62.
40 El-Rassi G, Takemitsu M, Glutting J, et al. Clinical outcome and return to athletics after nonoperative treatment of spondylolysis in children Poster Exhibit. Buenos Aires: Scoliosis Research Society. 2004.
41 Bono CM. Low-back pain in athletes. J Bone Joint Surg Am. 2004;86:382-396.
42 Logroscino G, Mazza O, Aulisa G, et al. Spondylolysis and spondylolisthesis in the pediatric and adolescent population. Childs Nerv Syst. 2001;17:644-655.
42a Leono A, Cianfoni A, Cerase A, et al. Lumbar spondylolysis: a review. Skeletal Radiol. May 2010. (Epub ahead of print)
43 Cavalier R, Herman MJ, Cheung EV, et al. Spondylolysis and spondylolisthesis in children and adolescents: I. Diagnosis, natural history, and nonsurgical management. J Am Acad Orthop Surg. 2006;14:417-424.
44 McNeely ML, Torrance G, Magee DJ. A systematic review of physiotherapy for spondylolysis and spondylolisthesis. Man Ther. 2003;8:80-91.
45 O’Sullivan PB, Phyty GD, Twomey LT, et al. Evaluation of specific stabilizing exercise in the treatment of chronic low back pain with radiologic diagnosis of spondylolysis or spondylolisthesis. Spine. 1997;22:2959-2967.
46 Salminen JJ, Erkintalo MO, Pentti J, et al. Recurrent low back pain and early disc degeneration in the young. Spine. 1999;24:1316-1321.
47 Standaert CJ, Herring SA. Spondylolysis: A critical review. Br J Sports Med. 2000;34:415-422.
48 Dubousset J. Treatment of spondylolysis and spondylolisthesis in children and adolescents. Clin Orthop Relat Res. 1997;337:77-85.
49 Cheung EV, Herman MJ, Cavalier R, et al. Spondylolysis and spondylolisthesis in children and adolescents: II. Surgical management. J Am Acad Orthop Surg. 2006;14:488-498.
50 Chen JF, Lee ST. A physiological method for the repair of young adult simple isthmic lumbar spondylolysis. Chang Gung Med J. 2000;23:92-98.
51 Labelle H, Roussouly P, Berthonnaud E, et al. Spondylolisthesis, pelvic incidence, and spinopelvic balance: A correlation study. Spine. 2004;29:2049-2054.
52 Curylo LJ, Edwards C, DeWald RW. Radiographic markers in spondyloptosis: Implications for spondylolisthesis progression. Spine. 2002;27:2021-2025.
53 Berk RH. [Lumbar spine injuries in pediatric and adolescent athletes]. Acta Orthop Traumatol Turc. 2004;38(Suppl 1):S58-S63.
54 Wimberly RL, Lauerman WC. Spondylolisthesis in the athlete. Clin Sports Med. 2002;21:133-145.
55 Teitz CC, Cook DM. Rehabilitation of neck and low back injuries. Clin Sports Med. 1985;4:455-476.
56 Burkus JK, Lonstein JE, Winter RB, et al. Long-term evaluation of adolescents treated operatively for spondylolisthesis: A comparison of in situ arthrodesis only with in situ arthrodesis and reduction followed by immobilization in a cast. J Bone Joint Surg Am. 1992;74:693-704.
57 Lonstein JE. Spondylolisthesis in children: Cause, natural history, and management. Spine. 1999;24:2640-2648.
58 Zindrick MR, Wiltse LL, Doornik A, et al. Analysis of the morphometric characteristics of the thoracic and lumbar pedicles. Spine. 1987;12:160-166.
59 Sorensen K. Scheuermann’s Juvenile Kyphosis: Clinical Appearances, Radiography, Aetiology and Prognosis. Copenhagen: Mundsgaard; 1964.
60 Commandre F, Gagnerie G, Zakarian M. The child, the spine and sports. J Sports Med Phys Fitness. 1988;28:11-19.
61 Goldstein J, Berger P, Windier G. Spine injuries in gymnasts and swimmers: An epidemiologic investigation. Am J Sports Med. 1991;19:463-468.
62 Hellstrom M, Jacobsson B, Sward L. Radiologic abnormalities of the thoraco-lumbar spine in athletes. Acta Radiol. 1990;31:127-132.
63 Matheson G, Clement D, McKenzie D. Stress fractures in athletes: A study of 320 cases. Am J Sports Med. 1987;15:46-58.
64 Micheli L. Low back pain in the adolescent: Differential diagnosis. Am J Sports Med. 1979;7:362-364.
65 Ohlen G, Wredmark T, Spangfort E. Spinal sagittal configuration and mobility related to low-back pain in the female gymnast. Spine. 1989;14:847-850.
66 Sward L, Hellstrom M, Jacobsson B. Back pain and radiologic changes in the thoraco-lumbar spine of athletes. Spine. 1990;15:124-129.
67 Sward L, Hellstrom M, Jacobsson B. Disc degeneration and associated abnormalities of the spine in elite gymnasts: A magnetic resonance imaging study. Spine. 1991;16:437-443.
68 Sward L, Hellstrom M, Jacobsson B. Vertebral ring apophysis injury in athletes: Is the etiology different in the thoracic and lumbar spine? Am J Sports Med. 1993;21:841-845.
69 Tall R, DeVault W. Spinal injury in sport: Epidemiologic considerations. Clin Orthop Relat Res. 1993;12:441-448.
70 Tsai L, Wredmark T. Spinal posture, sagittal mobility, and subjective rating of back problems in former female elite gymnasts. Spine. 1993;18:872-875.
71 Scheuermann V. Kyphosis juvenilis (Scheuermann’s Krankheit). Fortschr Rontgenstr. 1936;53:1-16.
72 Greene T, Hensinger R, Hunter L. Back pain and vertebral changes simulating Scheuermann’s disease. J Pediatr Orthop. 1985;5:1-7.
73 Sward L, Eriksson B, Peterson L. Anthropometric characteristics, passive hip flexion, and spinal mobility in relation to back pain in athletes. Spine. 1990;15:376-382.
74 Schmorl G. Zur Kenntnis der Wirbelkorperepiphyse und der an ihr vorkommenden Verletzungen. Arch Klin Chir. 1928;153:35-45.
75 Siffert R. Classification of the osteochondroses. Clin Orthop Relat Res. 1981;158:10-18.
76 Heithoff KB, Gundry CR, Burton CV, et al. Juvenile discogenic disease. Spine. 1994;19:335-340.
77 Dimar JR2nd, Glassman SD, Carreon LY. Juvenile degenerative disc disease: A report of 76 cases identified by magnetic resonance imaging. Spine J. 2007;7:332-337.
78 Durham SR, Sun PP, Sutton LN. Surgically treated lumbar disc disease in the pediatric population: An outcome study. J Neurosurg. 2000;92:1-6.
79 Epstein JA, Epstein NE, Marc J, et al. Lumbar intervertebral disk herniation in teenage children: Recognition and management of associated anomalies. Spine. 1984;9:427-432.
80 Ishihara H, Matsui H, Hirano N, et al. Lumbar intervertebral disc herniation in children less than 16 years of age: Long-term follow-up study of surgically managed cases. Spine. 1997;22:2044-2049.
81 Martinez-Lage JF, Poza M, Arcas P. Avulsed lumbar vertebral rim plate in an adolescent: Trauma or malformation? Childs Nerv Syst. 1998;14:131-134.
82 Parisini P, Di Silvestre M, Greggi T, et al. Lumbar disc excision in children and adolescents. Spine. 2001;26:1997-2000.
83 Ikata T, Morita T, Katoh S, et al. Lesions of the lumbar posterior end plate in children and adolescents: An MRI study. J Bone Joint Surg Br. 1995;77:951-955.
84 Sassmannshausen G, Smith BG. Back pain in the young athlete. Clin Sports Med. 2002;21:121-132.
85 DeLuca PF, Mason DE, Weiand R, et al. Excision of herniated nucleus pulposus in children and adolescents. J Pediatr Orthop. 1994;14:318-322.
86 Shillito JJr. Pediatric lumbar disc surgery: 20 patients under 15 years of age. Surg Neurol. 1996;46:14-18.
87 Ginsburg GM, Bassett GS. Back pain in children and adolescents: Evaluation and differential diagnosis. J Am Acad Orthop Surg. 1997;5:67-78.
88 Gibson J, Waddell G: Surgery for degenerative lumbar spondylosis. Cochrane Database Syst Rev CD001352, 2005.
89 Hassard GH, Carmack WL, Dixon J, et al. Rehabilitation: A team approach to total patient care. The rehabilitation team. J Pract Nurs. 1978;28:22-25.
90 Papagelopoulos PJ, Shaughnessy WJ, Ebersold MJ, et al. Long-term outcome of lumbar discectomy in children and adolescents sixteen years of age or younger. J Bone Joint Surg Am. 1998;80:689-698.
91 Beggs I, Addison J. Posterior vertebral rim fractures. Br J Radiol. 1998;71:567-572.
92 Skobowytsh-Okolot B. “Posterior apophysis” in L.IV—the cause of neuroradicular disturbance. Acta Orthop Scand. 1962;32:341-351.
93 Banerian KG, Wang AM, Samberg LC, et al. Association of vertebral end plate fracture with pediatric lumbar intervertebral disk herniation: Value of CT and MR imaging. Radiology. 1990;177:763-765.
94 Dietemann JL, Runge M, Badoz A, et al. Radiology of posterior lumbar apophyseal ring fractures: Report of 13 cases. Neuroradiology. 1988;30:337-344.
95 Keller RH. Traumatic displacement of the cartilaginous vertebral rim: A sign of intervertebral disc prolapse. Radiology. 1974;110:21-24.
96 Lippit A. Fracture of the vertebral body end plate and disk protrusion causing subarachnoid block in an adolescent. Clin Orthop Relat Res. 1974;11:112-115.
97 Proctor MR, Cantu RC. Head and neck injuries in young athletes. Clin Sports Med. 2000;19:693-715.
98 Kleiner D, Almquist J, Bailes J, et al. Prehospital care of the spine-injured athlete: A document from the Inter-Association Task Force for Appropriate Care of the Spine-Injured Athlete. Dallas, National Athletic Trainers Association. 2001.
99 Cantu RC, Mueller FO. Catastrophic spine injuries in football (1977-1989). J Spinal Disord. 1990;3:227-231.
100 Cantu RC, Mueller FO. Catastrophic football injuries: 1977-1998. Neurosurgery. 2000;47:673-675. discussion 675-677
101 Cantu RC, Mueller FO. Catastrophic spine injuries in American football, 1977-2001. Neurosurgery. 2003;53:358-362. discussion 362-363
102 Cantu RC, Mueller FO. Brain injury-related fatalities in American football, 1945-1999. Neurosurgery. 2003;52:846-852. discussion 852-843
103 Mueller FO, Cantu RC. Catastrophic injuries and fatalities in high school and college sports, fall 1982-spring 1988. Med Sci Sports Exerc. 1990;22:737-741.
104 Mueller FO, Cantu RC. The annual survey of catastrophic football injuries: 1977-1988. Exerc Sport Sci Rev. 1991;19:261-312.
105 Meyer SA, Schulte KR, Callaghan JJ, et al. Cervical spinal stenosis and stingers in collegiate football players. Am J Sports Med. 1994;22:158-166.
106 Albright JP, McAuley E, Martin RK, et al. Head and neck injuries in college football: An eight-year analysis. Am J Sports Med. 1985;13:147-152.
107 Albright JP, VanGilder J, el-Khoury GY, et al. Head and neck injuries in sports. In: Scott WN, Nisonson B, Nicholas JA, editors. Principles of Sports Medicine. Baltimore: Williams & Wilkins; 1984:40-86.
108 Bergfeld JA, Hershman E, Wilbourn A. Brachial plexus injury in sports: A five year follow-up. Orthop Trans. 1988;12:743-744.
109 Clancy WGJr, Brand RL, Bergfield JA. Upper trunk brachial plexus injuries in contact sports. Am J Sports Med. 1977;5:209-216.
110 Funk FF, Wells RE. Injuries of the cervical spine in football. Clin Orthop Relat Res. 1975;109:50-58.
111 Rockett FX. Observations on the “burner”: Traumatic cervical radiculopathy. Clin Orthop Relat Res. 1982;164:18-19.
112 Speer KP, Bassett FH3rd. The prolonged burner syndrome. Am J Sports Med. 1990;18:591-594.
113 Watkins RG. Neck injuries in football players. Clin Sports Med. 1986;5:215-246.
114 Quan D, Bird SJ. Nerve conduction studies and electromyography in the evaluation of peripheral nerve injuries. Univ Pa Orthop J. 1999;12:45-51.
114a Seddon HJ. Three types of nerve injuries. Brain. 1943;66:237.
114b Sunderland SA. A classification of peripheral nerve injuries producing loss of function. Brain. 1951;74:491-516.
115 Eismont FJ, Clifford S, Goldberg M, et al. Cervical sagittal spinal canal size in spine injury. Spine. 1984;9:663-666.
116 Castro FPJr, Ricciardi J, Brunet ME, et al. Stingers, the Torg ratio, and the cervical spine. Am J Sports Med. 1997;25:603-608.
117 Torg JS, Pavlov H, Genuario SE, et al. Neurapraxia of the cervical spinal cord with transient quadriplegia. J Bone Joint Surg Am. 1986;68:1354-1370.
118 Pavlov H, Torg JS, Robie B, et al. Cervical spinal stenosis: Determination with vertebral body ratio method. Radiology. 1987;164:771-775.
119 Clancy WGJr, Foltz AS. Iliac apophysitis and stress fractures in adolescent runners. Am J Sports Med. 1976;4:214-218.
120 Doral MN, Aydog ST, Tetik O, et al. Multiple osteochondroses and avulsion fracture of anterior superior iliac spine in a soccer player. Br J Sports Med. 2005;39:e16.
121 Pointinger H, Munk P, Poeschl GP. Avulsion fracture of the anterior superior iliac spine following apophysitis. Br J Sports Med. 2003;37:361-362.
122 Dormans JP, Moroz L. Infection and tumors of the spine in children. J Bone Joint Surg Am. 2007;89(Suppl 1):79-97.