Chapter 10. The hip
CHAPTER CONTENTS
Summary247
SUMMARY
Pain in the hip region can be incorrectly attributed to the lumbar spine and/or sacroiliac joint, while the bursae in the area may not be considered, and can evade diagnosis. Groin strain and hamstring injury are familiar to the clinician, though worthy of mention to enhance effective treatment.
This chapter describes the anatomy relevant to common lesions in the hip region to which orthopaedic medicine principles of treatment can be applied. A commentary follows, highlighting the relevant points of the history and suggesting a methodical sequence for objective examination. Lesions are then discussed with treatment alternatives and overall management.
ANATOMY
Inert structures
The hip joint is a synovial joint formed between the head of the femur and the acetabulum of the innominate bone. The head of the femur is slightly more than half a sphere and faces anteriorly, superiorly and medially to articulate with the acetabulum forming a ball-and-socket joint. This articulation offers great stability and provides sufficient mobility for gait. The close packed position of the hip joint is full extension, with a degree of abduction and medial rotation (Hartley 1995, Standring 2009).
The acetabulum is deepened by the fibrocartilaginous acetabular labrum and all articular surfaces are covered by articular cartilage. The fibrous capsule, lined with synovium, surrounds most of the neck of the femur, attaching above to the acetabular rim, below to the intertrochanteric line anteriorly and 1 cm above the inter-trochanteric crest posteriorly. Both the joint capsule and the articular cartilage tend to be thicker anterosuperiorly, which is the region of most stress in weight-bearing. Synovial plicae (folds or reflections of the synovial membrane) have been identified by Fu et al (1997), found mainly on the external surface of the lower medial part of the acetabular labrum (labral plicae) but also at the base of the ligament of the head of the femur and on the base of the femoral neck. The labral plicae may potentially be a source of pain if injured or thickened since, in the normal state, these have been seen to slip between the articular surfaces of the femoral head and acetabulum during medial rotation and to return to their original position during lateral rotation.
Three ligaments reinforce the articular capsule and control movement. All three are taut in extension and relaxed in flexion. The iliofemoral ligament has strong medial and lateral bands which form a Y-shape, passing from the anterior inferior iliac spine to the intertrochanteric line. The pubofemoral ligament passes from the superior pubic ramus to blend distally with the capsule and the medial border of the iliofemoral ligament. The ischiofemoral ligament passes from the ischium and winds superiorly and laterally to the upper part of the femoral neck, blending with the capsule of the hip joint and supporting it posteriorly.
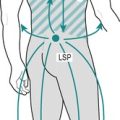
The psoas bursa (L2–L3; Cyriax 1982) is 5–7 cm long and 2–4 cm wide in its normal collapsed state (Underwood et al 1988, Toohey et al 1990, Flanagan et al 1995, Zimmermann et al 1995). In 15% of cadaveric specimens, the psoas bursa was seen to communicate with the hip joint via an aperture between the iliofemoral and pubofemoral ligaments (Flanagan et al 1995). It may be a simple bursa or multiloculated with well-defined thin walls (Meaney et al 1992).
The psoas bursa lies beneath the musculotendinous junction of the iliopsoas muscle and the front of the capsule of the hip joint (Fig. 10.1). It cushions the ilio-psoas tendon as it winds round the front of the hip joint to its posteromedial insertion on the lesser trochanter. It is related anteromedially to the femoral artery and anteriorly to the femoral nerve (Canoso 1981). Its point of location is just distal to the midpoint of the inguinal ligament, deep to the femoral artery.
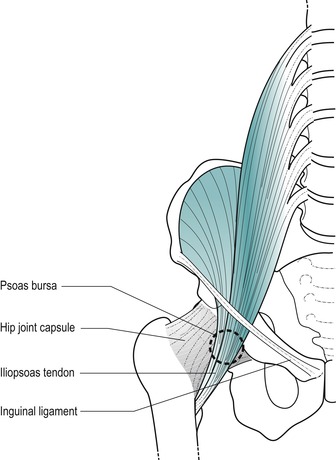 |
| Figure 10.1
Position of the psoas bursa.
|
The gluteal bursa (L4–L5; Cyriax & Cyriax 1993) is not a single entity, but for clinical purposes is considered to be so. At least four separate bursae lie between the different planes of the gluteal muscles as they attach to or pass over the greater trochanter, collectively forming the gluteal bursa.
Two bursae are associated with gluteus maximus: a large trochanteric bursa (Fig. 10.2), separating it from the lateral aspect of the greater trochanter, and a gluteofemoral bursa, lying between it and vastus lateralis (Standring 2009). The trochanteric bursa of gluteus medius lies between its tendon and the anterosuperior aspect of the greater trochanter. The trochanteric bursa of gluteus minimus separates its insertion from the medial part of the greater trochanter (Standring 2009). One further bursa may be present, the ischial bursa, lying between the ischial tuberosity and the lower part of gluteus maximus.
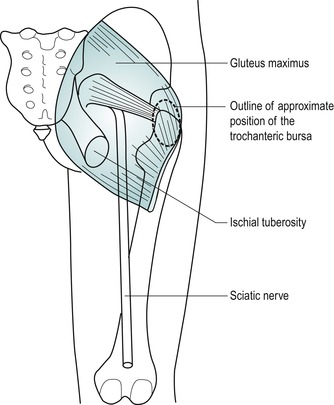 |
| Figure 10.2
Position of trochanteric bursa.
|
Contractile structures
Anterior muscles are flexors of the hip, although they may also assist other hip movements. Some pass over the knee where they also have an effect. Resisted flexion of the hip tests mainly psoas major; with the knee flexed it is also testing rectus femoris.
Psoas major (ventral rami L1–L3) has its origin from the lumbar spine. It descends to pass under the centre of the inguinal ligament receiving the fibres of iliacus on its lateral side. The iliopsoas tendon crosses the front of the hip joint where it is cushioned by the underlying psoas bursa. The combined tendon winds posteriorly to insert into the lesser trochanter of the femur.
Sartorius (femoral nerve L2–L3) passes from the anterior superior iliac spine to cross the thigh medially, inserting into the upper medial aspect of the tibia. It marks the lateral border of the femoral triangle.
Rectus femoris (femoral nerve L2–L4) is part of the quadriceps mechanism and has its main effect at the knee. However, its origin above the hip makes it a two-joint muscle and it also acts as a powerful hip flexor, being most efficient when the knee is flexed (Kapandji 1987). It has two heads of origin: a straight head from the anterior inferior iliac spine and a reflected head from just above the acetabular rim. It joins the rest of the quadriceps to insert into the patellar tendon.
Posterior muscles are extensors of the hip. Gluteus maximus acts principally as a hip extensor while the hamstrings assist hip extension, but their main effect is in flexing the knee. Since the hamstring muscles run over two joints, their efficiency in extending the hip increases if the knee is locked into extension (Kapandji 1987).
Gluteus maximus (inferior gluteal nerve L5, S1–S2) is the largest and most superficial of the gluteal muscles. It passes from behind the posterior gluteal line on the blade of the ilium to the iliotibial tract and upper femur. The large trochanteric bursa separates the insertion of gluteus maximus from the lateral aspect of the greater trochanter.
Biceps femoris (sciatic nerve L5, S1–S2) is the lateral hamstring with two heads of origin. A long head arises from an inferomedial facet on the ischial tuberosity (which it shares with semitendinosus) and a short head from the lateral lip of the linea aspera. Its fibres converge into a fusiform muscle belly and its tendon of insertion attaches to the head of the fibula.
Semitendinosus and semimembranosus are the medial hamstrings. Semitendinosus (sciatic nerve L5, S1–S2) takes origin from the inferomedial facet on the ischial tuberosity. Its muscle belly ends in the middle of the thigh and its long tendon of insertion lies on semimembranosus before winding around to the medial aspect of the upper tibia. Semimembranosus (sciatic nerve L5, S1–S2) takes origin from the superolateral facet on the ischial tuberosity and has its main insertion onto the posterior aspect of the medial tibial condyle into the tuberculum tendinis.
Functionally, the small, deep muscles of the hip are responsible for lateral rotation.
Piriformis (L5, S1–S2) originates in the pelvis, exiting through the greater sciatic foramen to attach to the upper border of the greater trochanter.
Obturator externus (posterior branch of the obturator nerve L3–L4) and obturator internus (nerve to obturator internus L5, S1) pass posteriorly to the hip joint and insert into the medial surface of the greater trochanter and trochanteric fossa.
Gemelli (L5, S1) pass from the ischial spine and ischial tuberosity to the medial aspect of the greater trochanter.
Quadratus femoris (nerve to quadratus femoris L5, S1) passes from the ischial tuberosity to the quadrate tubercle in the middle of the trochanteric crest.
Lateral muscles are abductors and lateral rotators. Gluteus medius is the main hip abductor while medius and minimus together are responsible for maintaining the position of the opposite side of the pelvis in single-leg stance. Weakness of the hip abductors produces a positive Trendelenburg sign. Tensor fascia lata and the anterior fibres of gluteus medius and minimus also produce medial rotation and flexion because they lie anterior to the frontal plane of the hip joint. Lying posteriorly, some fibres of gluteus medius and minimus are responsible for lateral rotation and extension (Kapandji 1987).
Gluteus medius (superior gluteal nerve L5, S1) is partially overlapped by maximus and lies in a slightly deeper plane. It originates from the blade of the ilium between posterior and anterior gluteal lines and inserts into the lateral aspect of the greater trochanter.
Gluteus minimus (superior gluteal nerve L5, S1) is the deepest gluteal muscle and arises between the anterior and inferior gluteal lines, inserting into the medial part of the anterior trochanteric surface.
Tensor fascia lata (superior gluteal nerve L4–L5) arises from the anterior 5 cm of the outer lip of the iliac crest and the anterior superior iliac spine. It passes downwards and laterally to insert into the anterior border of the ilio-tibial tract.
The adductor muscles originate in the pelvis and pass to the medial aspect of the thigh.
Functionally, the medial muscles are responsible for adduction of the hip. Medial rotation at the hip is a secondary function of gluteus medius, minimus and tensor fascia lata; adductor magnus, longus and pectineus may also contribute to this movement.
Gracilis (obturator nerve L2–L3) is the most medial hip adductor. It passes from the lower half of the body of the pubis, the inferior pubic ramus and the adjacent ischial ramus, to run vertically downwards to just below the medial tibial condyle.
Pectineus (femoral nerve L2–L3) passes from the pecten pubis running posterolaterally to a line joining the lesser trochanter to the linea aspera.
Adductor longus (obturator nerve L2–L4) is the most superficial adductor. It passes from the body of the pubis, in the angle between the crest and the symphysis pubis, to descend posterolaterally to the middle third of the linea aspera.
Adductor brevis (obturator nerve L3) lies deep to adductor longus, passing from the lower aspect of the body of the pubis and the inferior pubic ramus to its attachment on the femur, between the lesser trochanter and the linea aspera.
Adductor magnus (upper fibres, obturator nerve; lower fibres, tibial branch of the sciatic nerve, L2–L4) is the largest and deepest adductor muscle. It is considered to have two separate portions, one an adductor portion and the other a hamstring portion, each with its own separate nerve supply. It takes origin from the inferior pubic ramus, the adjacent ischial ramus and the infero-lateral aspect of the ischial tuberosity. Its upper fibres pass mainly horizontally to the linea aspera of the femur and form the adductor part of the muscle. Its lower fibres pass more vertically to the adductor tubercle on the medial femoral condyle and form the hamstring part.
A GUIDE TO SURFACE MARKING AND PALPATION
Pelvis region
Palpate the iliac crest, which should be obvious in most people as no muscles attach to its superior border. The highest point of the crest lies just posterior to the midpoint and gives an approximate indication of the level of the spinous process of L4.
Palpate the anterior superior iliac spine which is sub-cutaneous and located at the anterior end of the iliac crest. It marks the lateral attachment of the inguinal ligament and the origin of the sartorius muscle.
Palpate the posterior superior iliac spine which is situated at the posterior end of the iliac crest. It is not as readily palpable as the anterior spine, but lies under a dimple in the upper buttock, approximately 4 cm lateral to the spinous process of S2. It gives attachment to the sacro-tuberous ligament. Imagine a line drawn from the posterior superior iliac spine to the spinous process of S2; this line crosses the centre of the sacroiliac joint and gives an indication of the joint’s position.
Consider the position of the anterior and posterior inferior iliac spines which lie below the superior spines and are not as readily palpable. The anterior inferior spine gives origin superiorly to the long head of rectus femoris and inferiorly to part of the iliofemoral ligament.
Locate the position of the pubic tubercle at the medial end of the inguinal crease, lying at the same level as the top of the greater trochanter. It marks the medial attachment of the inguinal ligament.
Palpate the bony ischial tuberosity, which lies in the buttock approximately 5 cm lateral to the midline just above the gluteal fold. In the sitting position, body weight is supported by the ischial tuberosities. Each is most easily palpated with the patient in side-lying and the hip placed in flexion, to bring the ischial tuberosity out from under the bulk of gluteus maximus.
Lateral aspect of the thigh
In side-lying palpate the greater trochanter, which is a large quadrangular bony prominence situated at the upper lateral shaft of the femur, approximately one hand’s breadth below the iliac crest. Grasp the greater trochanter with your thumb, index and middle fingers (Fig. 10.3), lifting the leg passively into abduction to relax the iliotibial tract. The greater trochanter will be a useful bony landmark for some of the injection techniques around the hip.
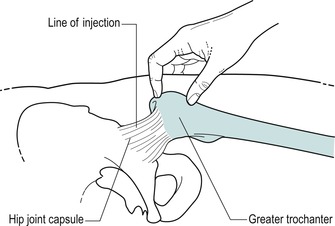 |
| Figure 10.3
Location of hip joint for the injection by grasping the greater trochanter.
|
Anterior aspect of the thigh
Consider the position of the femoral triangle on the anterior thigh (Fig. 10.4). Place the leg into the FABER position – a combination of Flexion, ABduction and External (lateral) Rotation of the hip – to give you an indication of the borders of the triangle. The inguinal ligament forms the base of the triangle, sartorius its lateral border and adductor longus its medial border. Iliopsoas and pectineus lie in the floor of the femoral triangle.
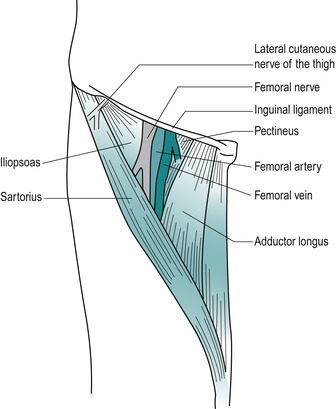 |
| Figure 10.4
Femoral triangle, also showing emerging lateral cutaneous nerve of thigh.
|
Consider the position of the lateral femoral cutaneous nerve of the thigh (L2–L3) as it passes under or through the inguinal ligament, just medial to the anterior superior iliac spine. It may be compressed here, causing a condition called meralgia paraesthetica, which produces paraesthesia and pain in the nerve’s distribution on the lateral side of the thigh. It is found in obese patients and those who wear tight-fitting clothes or belts (Adkins & Figler 2000).
Palpate for the femoral artery which passes down through the middle of the triangle with the femoral vein situated medially and the femoral nerve laterally. You will locate a strong pulse just distal to the midpoint of the inguinal ligament.
Locating the femoral pulse will prove a useful landmark for the structures passing deep to it. From superficial to deep these are the iliopsoas tendon, which is en route to its insertion into the lesser trochanter, the psoas bursa, and the hip joint.
Posterior aspect of buttock and thigh
Consider the position of the sciatic nerve in the buttock (Fig. 10.5). You can locate its approximate position by marking a point midway between the posterior superior iliac spine and the greater trochanter, which identifies the position of the nerve as it leaves the pelvis via the greater sciatic foramen, emerging under piriformis. Join this to another mark at a point just medial to the midpoint between the greater trochanter and the ischial tuberosity. This indicates the position of the nerve as it continues to exit the buttock under the lower border of gluteus maximus (Standring 2009).
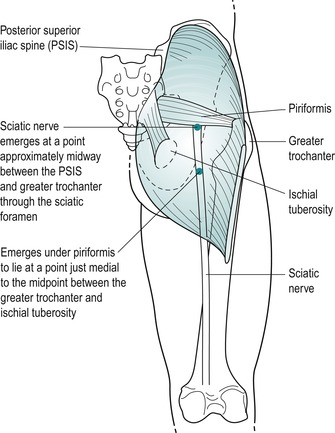 |
| Figure 10.5
Approximate course of the sciatic nerve in the buttock and thigh.
|
COMMENTARY ON THE EXAMINATION
Observation
A general observation is made of the patient’s face and overall posture, but particular attention is paid to the gait. Since the function of the hip joint is to support body weight, lesions involving the joint mechanics tend to cause alterations in the gait pattern. An uneven stride will indicate restricted movement, as found in arthritis, or may be due to pain on weight-bearing. Excessive lateral rotation on walking may indicate a slipped epiphysis in the young or may be present with pain or advanced capsular contracture in the elderly, indicating an arthrosis with a marked capsular pattern. A Trendelenburg gait will indicate weak abductor muscles.
Pain in the hip joint region may originate in the lumbar spine and a detailed history will help to eliminate a lesion in the area.
History (subjective examination)
The age, occupation, sports, hobbies and lifestyle of the patient may alert the examiner to the possible cause of the lesion.
The age of the patient is relevant to conditions at the hip. Degenerative osteoarthrosis typically presents in the middle to older age group, although it is not uncommon to find it in younger athletes, especially road runners. Muscle lesions and bursitis affect the middle age group, while loose bodies can present as a complication of osteo-arthrosis in the older group or as osteochondritis dissecans in adolescents.
Children can develop hip problems which if misdiagnosed can be potentially serious, and an orthopaedic opinion should always be sought. ‘Irritable hip’ is a non-specific diagnosis for groin pain, limited movement and a limp. Perthes’ disease affects boys aged 3–10 and is an osteochondritis of the femoral epiphysis. Slipped epiphysis is either sudden or gradual slipping of the superior epiphyseal plate which may produce a lateral rotation deformity. It tends to occur in overweight adolescents (10–16) and is more common in boys, who present with pain on exercise. Transient synovitis is of unknown aetiology and affects children under 10 years with an acute onset (Gough-Palmer & McHugh 2007). Juvenile chronic arthritis usually begins in other joints, but it can also affect the hip joints. Emms et al (2002) remind us that, although it is well known that knee pain in children may be referred from the hip, it must not be forgotten that hip pathology may masquerade as knee pain in adult patients as well.
Excessive muscle contraction, as involved in explosive sports changing rapidly from running to jumping (hurdling, etc.), can lead to avulsion fractures and chronic apophysitis in adolescents, most commonly at the origin of the long head of rectus femoris at the anterior inferior iliac spine (Brukner & Khan 2007).
Occupation, sports, hobbies and lifestyle will certainly indicate the aggravating factors of the condition and allow the clinician to formulate a programme of treatment and advice, tailored to the patient’s individual needs.
Specific sports-related conditions should be considered. Stress fracture of the femoral neck may be encountered in young adults who are involved in endurance and high-intensity sports; initially anterior hip pain occurs late into the sporting activity but progresses to limit activity, occurring during any weight-bearing episode and even at rest. It should also be suspected in women with the female athletic triad of amenorrhoea, eating disorder and osteo-porosis. Diagnosis is essential to prevent progression to avascular necrosis of the femoral head (O’Kane 1999, Adkins & Figler 2000).
Osteitis pubis, a poorly understood pathological condition involving the pubic bone and symphysis pubis, presents with groin pain which may be bilateral. The symptoms may be aggravated by exercise, twisting, turning and kicking. Pain is provoked by resisted adduction (the ‘squeeze test’) which is usually accompanied by weakness, and there is tenderness to palpation over the pubic tubercles and symphysis pubis (Brukner & Khan 2007). The so-called ‘sports hernias’ should also be considered as a cause of anterior hip pain. These are thought to be responsible for activity-related hip pain, particularly in football, rugby and ice hockey players (O’Kane 1999). Inguinal hernia presents as a lump in the groin that goes away when the patient lies down. The lump reappears or increases on coughing and is not usually painful (Jenkins & O’Dwyer 2008). ‘Gilmore’s groin’ is not a hernia but should be considered in the differential diagnosis of groin pain, particularly in the sporting male. It is a disruption of the external oblique aponeurosis causing dilatation of the superficial inguinal ring, torn conjoined tendon and dehiscence between the inguinal ligament and the torn conjoined tendon (Williams & Foster 1995, Tibor & Sekiya 2008) (see p. 272).
The site and spread of pain may be local, indicating a superficial or less irritable lesion such as a muscle strain, or diffuse, indicating a larger lesion or gross inflammation.
Referred pain may originate from the lumbar spine. The sensory nerve supply to the hip joint is mainly through the femoral nerve L2–L3; therefore the joint itself refers pain into these dermatomes depending on the size of the lesion. Part of the L2 and L3 dermatomes covers the upper buttock and a hip lesion may present as low back pain only. Lesher et al (2008) looked at pain referral patterns arising from the hip joint. Of the 51 patients assessed, 55% of patients had referral to the groin and 57% to the thigh; 22% experienced pain in the lower limb distal to the knee, and occasionally to the foot, but the most common area for referral was buttock pain, experienced by 71% of patients. The most common referral combination was buttock pain with thigh referral, which occurred in 20% of subjects. This pattern of referral is similar to both the lumbar spine and sacroiliac joint and differential diagnosis can be difficult on the basis of pain referral alone. Other factors from the history and the objective examination will help towards clinical diagnosis and it is not unusual for the initial diagnosis to be modified following consideration of treatment outcomes.
Groin pain or pain referred to the knee in the child or adolescent without obvious cause must be considered serious and a specialist opinion sought for the possibility of the conditions mentioned above.
The onset of the symptoms may be gradual or sudden.
In osteoarthrosis the pain has a gradual onset, initially during weight-bearing activities, progressing to hip pain without weight-bearing, and present at rest (Cailliet 1990). A history of previous trauma such as fracture, which alters joint biomechanics, can predispose the joint to degenerative changes.
Relatively minor trauma can fracture the pelvis in the elderly, producing severe pain of sudden onset. Loose bodies present suddenly, as do traumatic muscular lesions. Muscles around the hip joint can be easily strained, since many are two-joint muscles, and a sudden explosive contraction such as that seen in sprinting may produce overstretching (Hartley 1995). Overuse or repetitive movements may produce chronic contractile lesions or bursitis.
The duration of symptoms indicates the stage of the lesion in the inflammatory process. Degenerative osteo-arthrosis will present a typical history of gradually worsening episodes of pain. Bursitis tends to give a gradual onset of aching pain and therefore is often present for many months before the patient seeks treatment. A severe pain which gradually increases in intensity, and remains so, is indicative of a serious lesion. This, coupled with other findings in the history, may be indicative of the ‘sign of the buttock’ (see p. 274).
The symptoms and behaviour need to be considered. The behaviour of the pain gives an indication of the nature of the lesion. For example, osteoarthrosis at the hip joint may be aggravated by activity or weight-bearing, or inflamed bursae and muscle sprains are worse with use and eased by rest.
The other symptoms described by the patient may give essential clues to diagnosis. Bursae produce pain on activities which squeeze or compress them, e.g. lying on the side or sitting. Loose bodies tend to produce twinging pain and a sensation of giving way on weight-bearing. Similar symptoms may be associated with labral tears or anterior acetabular chondral defects where clicking or locking may also be present (Neumann et al 2007). Arthritis tends to produce morning pain and stiffness due to accumulation of intracapsular swelling overnight (Hartley 1995). Degenerative osteoarthrosis, in its early stage, often produces night pain. Unrelenting pain should be considered serious, especially if the patient is unwell with a fever, night sweats and rigors.
To determine if the pain is coming from the lumbar spine, the patient is questioned about the presence of paraesthesia and pain produced by a cough or sneeze.
An indication of past medical history, other joint involvement and medications may give a clue to diagnosis and will establish whether contraindications to treatment techniques exist. Patients should be asked about any unexpected recent weight loss, indicative of more serious lesions, such as secondary deposits which are common in the hip and pelvis (Paice 1995). Differential diagnosis should also consider the exclusion of hip pain associated with pathology of the abdominal and pelvic organs as well as femoral or inguinal hernias. In addition to past medical history, establish any ongoing conditions and treatment. Explore other previous or current musculoskeletal problems with previous episodes of the current complaint, any treatment given and the outcome of treatment.
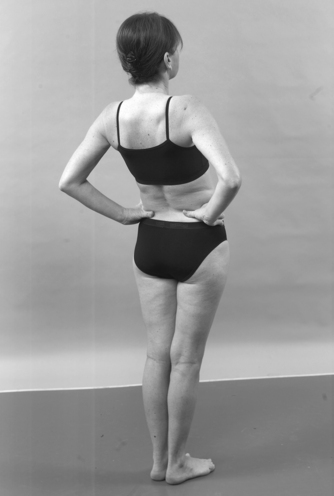
Inspection
An inspection of the general posture in weight-bearing will indicate any bony deformity. Look for general postural asymmetry which may be relevant, the position of the buttock creases, posterior superior iliac spines, anterior superior iliac spines, level of the iliac crests, any leg length discrepancy and the position of the feet.
Colour changes and swelling are not expected at the hip because it is such a deep joint, but they may be associated with trauma, bruising and abrasions. If redness and swelling are present in the buttock area without a history of trauma, the ‘sign of the buttock’ (see p. 274) may be suspected.
Muscle wasting may be seen in the glutei associated with a lumbar lesion, or in the quadriceps associated with degenerative osteoarthrosis of the hip or a lumbar lesion.
State at rest
Before any movements are performed, the state at rest is established to provide a baseline for subsequent comparison.
Examination by selective tension (objective examination)
The suggested sequence for the objective examination will now be given, followed by a commentary including the reasoning in performing the movements and the significance of the possible findings. Comparison should always be made with the other side.
Eliminate the lumbar spine
• Active lumbar extension (Fig. 10.6)
 |
| Figure 10.6
Active extension.
|
• Extension repeated with foot on stool if indicated (Fig. 10.7)
 |
| Figure 10.7
Active extension with hip flexed to differentiate between hip and lumbar spine as the cause of pain.
|
• Active lumbar right side flexion (Fig. 10.8)
 |
| Figure 10.8
Active right side flexion.
|
• Active lumbar left side flexion (Fig. 10.9)
 |
| Figure 10.9
Active left side flexion.
|
• Active lumbar flexion (Fig. 10.10)
 |
| Figure 10.10
Active flexion.
|
• Straight leg raise (Fig. 10.11)
 |
| Figure 10.11
Straight leg raise.
|
Supine lying
• Passive hip flexion (Fig. 10.12)
 |
| Figure 10.12
Passive flexion.
|
• Passive hip medial rotation for end-feel (Fig. 10.13)
 |
| Figure 10.13
Passive medial rotation.
|
• Passive hip lateral rotation (Fig. 10.14)
 |
| Figure 10.14
Passive lateral rotation.
|
• Passive hip abduction (Fig. 10.15)
 |
| Figure 10.15
Passive abduction.
|
• Passive hip adduction (Fig. 10.16)
 |
| Figure 10.16
Passive adduction.
|
• Resisted hip flexion (Fig. 10.17)
 |
| Figure 10.17
Resisted flexion.
|
• Resisted hip abduction (Fig. 10.18)
 |
| Figure 10.18
Resisted abduction.
|
• Resisted hip adduction (Fig. 10.19)
 |
| Figure 10.19
Resisted adduction.
|
• Resisted hip extension (Fig. 10.20)
 |
| Figure 10.20
Resisted extension.
|
Prone lying
• Femoral stretch test (Fig. 10.21)
 |
| Figure 10.21
Femoral stretch test.
|
• Passive hip extension (Fig. 10.22)
 |
| Figure 10.22
Passive extension.
|
• Passive hip medial rotation for range (Fig. 10.23)
 |
| Figure 10.23
Passive medial rotation.
|
• Resisted hip medial rotation (Fig. 10.24)
 |
| Figure 10.24
Resisted medial rotation.
|
• Resisted hip lateral rotation (Fig. 10.25)
 |
| Figure 10.25
Resisted lateral rotation.
|
• Resisted knee flexion (Fig. 10.26)
 |
| Figure 10.26
Resisted knee flexion.
|
• Resisted knee extension (Fig. 10.27)
 |
| Figure 10.27
Resisted knee extension.
|
Accessory test for the psoas bursa
• Passive hip flexion and adduction (Fig. 10.28)
 |
| Figure 10.28
Combined flexion and adduction to compress the psoas bursa.
|
Accessory test for the ‘sign of the buttock’
• Straight leg raise (Fig. 10.29)
 |
| Figure 10.29
Straight leg raise, accessory test for ‘sign of the buttock’.
|
Palpation
• Once a diagnosis has been made, the structure at fault is palpated for the exact site of the lesion
The routine for the examination of the hip is conducted in the above order as it allows all tests in each position of standing, supine and prone to be completed.
The lumbar spine is first assessed by the four active movements. If active lumbar extension reproduces the pain, it should be repeated with the hip joint eliminated by placing it into flexion with the foot up on a stool. If extension is still painful, the lesion lies in the lumbar spine and a more thorough investigation of this must then be made. The straight leg raise and femoral stretch tests are applied within the examination sequence to test for neural involvement. The straight leg raise does stretch the hamstrings, which needs to be considered within clinical reasoning, and is part of an accessory test to look for serious pathology in the hip or pelvis (see below).
Tests for sacroiliac joint involvement may also be included at this stage, as indicated by the history, and are described in Chapter 14.
The passive hip movements test the inert structures for pain, range of movement and end-feel. Limited movement may be typical of the capsular pattern of limitation due to arthritis. Normally, passive flexion has a ‘soft’ end-feel while passive medial rotation, lateral rotation and extension have an ‘elastic’ end-feel. It is not possible to appreciate the end-feel of the capsule on passive abduction and adduction as the tension in the overlying soft tissue structures provides the end of range of these movements before the capsule can be stressed. Abduction may still be limited as part of the capsular pattern nonetheless. A bursitis or a loose body in the joint produces a non-capsular pattern of movement.
The resisted movements test the contractile structures for pain and power. At the hip, muscle lesions are commonly found in the adductors, quadriceps and hamstrings, but positive resisted tests may also be an accessory sign in bursitis. Resisted flexion tests mainly psoas, but since the knee is flexed it also tests rectus femoris. Resisted abduction tests mainly gluteus medius, while resisted adduction tests the adductor muscles, particularly adductor longus. Resisted extension tests mainly gluteus maximus, but since the knee is extended, this also tests the hamstrings. Resisted rotation tests the medial and lateral rotators of the hip, resisted knee flexion tests the hamstring muscles and resisted knee extension tests the quadriceps muscle group.
Accessory tests can be applied if indicated. Combined hip flexion and adduction can be applied to compress the psoas bursa to confirm its diagnosis, and a straight leg raise can be included if the ‘sign of the buttock’ is suspected as an indicator of serious pathology in the hip or pelvis (see p. 274).
CAPSULAR LESIONS
The movements limited in the capsular pattern have a characteristically ‘hard’ end-feel. The capsular pattern of the hip is most limitation of medial rotation, less limitation of flexion and abduction and least limitation of extension. Klässbo et al (2003) supported medial rotation, flexion and abduction as the three most limited movements but found it difficult to identify the exact proportions lost to be able to establish an ordering or pattern of limitation. The capsular patterns at all the joints are intended as a clinical guide and it may not be appropriate to expose them to too rigorous investigation. The limitation of medial rotation is clinically the most useful component of the pattern. If, on examination, the capsular pattern exists at the hip joint, then an arthritis is present which, at the hip, can be degenerative osteo-arthrosis, traumatic arthritis, rheumatoid arthritis and any of the spondyloarthropathies.
Arthritis at the hip is commonly degenerative osteo-arthrosis, usually occurring over the age of 60 in 50% of the population (Kumar & Clark 2002). It may be sub-divided into primary athritis which has no recognizable predisposing cause although subtle secondary factors may be present, or secondary arthritis due to predisposing factors including occupational overuse, previous fracture or altered biomechanics, e.g. leg length discrepancies, and congenital or developmental abnormalities. Men and women are equally affected (Dieppe 1995, Sims 1999). However, Kersnic et al (1997) suggest that, as women have a significantly smaller femoral head radius and a larger acetabular diameter than men, contact stress on the articular surfaces is increased. The female femoral and pelvic shape may predispose women to osteoarthrosis, especially in association with increased body weight. Intrinsic factors such as altered biomechanics or extrinsic factors such as hardness of the floor, and the influence of sporting and leisure activities, may also contribute to degenerative change (Sims 1999).
Sims (1999) presents a hypothesis that the neuromuscular system plays a role in the development of degenerative osteoarthrosis. Strong contraction of the hip abductor mechanism prevents dropping of the contralateral pelvis in single-leg standing which produces an increase of four to five times body weight distributed through the hip joint. This is further increased during fast walking and running. Any alteration in the abductor mechanism, therefore, may lead to an uneven distribution of stress, resulting in articular cartilage degeneration. Dynamic loading of the hip occurs during the impact of heel strike and may involve single or repetitive loads. The impact load through the hip can exceed eight times body weight during a stumble (Bergmann et al, cited in Sims 1999).
Abnormal loading may also occur as a result of alteration in the centre of gravity such as that which occurs during an antalgic gait pattern, for example. Although this reduces the compressive forces of the abductor muscles as the centre of gravity shifts towards the stance limb, the load is transferred to the superior aspect of the femoral head where it becomes concentrated, leading to cartilage destruction. An abnormal gait pattern may be the result of pathology anywhere in the lower limb kinetic chain, from the lumbar spine to the foot, and need not be confined to the hip. The articular surfaces of the hip are slightly incongruent such that the apex of the acetabulum is a non-contact area allowing lubrication of the articular cartilage. The joint becomes more congruent during the ageing process, so reducing lubrication and possibly contributing further to degenerative change.
Neumann et al (2007) looked at the prevalence of labral tears and cartilage loss in patients with mechanical symptoms of the hip using magnetic resonance arthro-graphy. They concluded that cartilage loss, labral tears and bone marrow oedema appear to be interrelated and may represent important risk factors for the development and progression of osteoarthritis in the hip joint.
McGory & Endrizzi (2000) detail a case report of adhesive capsulitis of the hip, a diagnosis based on clinical findings with no evidence of bony changes on X-ray. The patient concerned had a history of hypothyroidism and had previously been diagnosed with bilateral adhesive capsulitis of the shoulder. They postulate that the involvement of the three separate joints gives credibility to the theory that adhesive capsulitis is a systemic rather than a local condition. Adhesive capsulitis of the hip follows a similar course to that demonstrated at the shoulder, and also responds to manual treatment and/or injection in a similar way.
The pain of osteoarthrosis usually has a gradual onset and may be felt in the upper buttock, groin and anterior thigh, up to or beyond the knee. Pain is associated with activity in the early stages, but as the condition advances, pain is also present at rest. Joint stiffness and loss of movement, such as difficulty in reaching to put on shoes and socks, are also presenting factors. X-ray changes are not a good indicator of symptoms as joint pathology can be present long before symptoms present and vice versa.
After diagnosis, the condition may stabilize and the prognosis can be good. Osteoarthrosis usually progresses with periods of exacerbation and periods of remission (Dieppe 1995). However, patients referred for surgery usually have a fairly rapid deterioration and severe symptoms progress over a period of 1–2 years.
Treatment for osteoarthrosis depends on the stage and activity of the disease as indicated by the severity/irritability of the lesion. It can be divided into early, middle and late stages (stages I, II or III) for the application of appropriate treatment.
Early stage osteoarthrosis of the hip (stage I)
This is usually the initial phase of diagnosis of the condition. At this stage, the key findings are as follows:
• The patient complains of buttock or groin pain associated with weight-bearing activities and the pain sometimes disturbs sleep.
• On examination, the patient has a mild capsular pattern of limited medial rotation, flexion and perhaps abduction, with extension not yet affected.
• The limited movements have an abnormal ‘hard’ end-feel due to muscle spasm, but some elasticity remains.
The principle of treatment, applied during this early stage, is to stretch the capsular adhesions using a Grade B capsular stretching technique in conjunction with heat applied to the joint. The aim of treatment is to relieve pain, allowing a greater range of pain-free movement to be established.
Grade B mobilization for early osteoarthrosis (Saunders 2000)
The movements limited in the capsular pattern are stretched using peripheral Grade B mobilization. However, functional benefit is often gained by stretching flexion alone.
To stretch flexion, position the patient in supine-lying with counter-pressure on the other leg to stabilize it and to ensure that maximum stretch is applied to the affected hip joint capsule (Fig. 10.30). Place one hand under the patient’s lower thigh, to avoid involving the knee and to give a little distraction, which makes the manoeuvre more comfortable. Place the patient’s foot against your shoulder to assist with stretching and to help guide the movement. After stretching flexion, slide the patient’s leg over your shoulder and return the leg steadily to the bed under some distraction to reduce discomfort (Fig. 10.31).
 |
| Figure 10.30
Grade B mobilization, stretching flexion.
|
 |
| Figure 10.31
Grade B mobilization, returning leg under some distraction.
|
To stretch extension, reverse the position described above for stretching flexion, with pressure applied to stretch extension of the affected leg (Fig. 10.32).
 |
| Figure 10.32
Grade B mobilization, stretching extension.
|
To stretch abduction, fix the good leg over the edge of the couch and position the affected leg in as much abduction as possible (Fig. 10.33). Increase this range of movement periodically as creep occurs and the range of movement increases.
 |
| Figure 10.33
Grade B mobilization, stretching abduction.
|
To stretch medial rotation, position the patient in prone-lying with the knee flexed to 90°. Fix the opposite buttock and apply the pressure carefully to the medial aspect of the knee. Take care with this manoeuvre as it may apply a strong torsion force to the neck of the femur and may also affect the knee (Fig. 10.34).
 |
| Figure 10.34
Grade B mobilization, stretching medial rotation.
|
Treatment aims to provide symptomatic relief, but it relies on the patient continuing with a self-management programme.
Initially the patient is seen regularly to assess the effect of the capsular stretching and to teach the patient home management. Clinical judgment should be used to guide how long each session of stretching should last. The pain may be aggravated for 2–4h and this should be explained to the patient. Treatment continues until either a plateau is reached or patients are confident to continue with their own stretching exercises and management.
In this early stage of the disease the patient may experience anxiety over the diagnosis and possible prognosis. Treatment must also include education of the patient, reassurance to relieve anxiety and encouragement to empower the patient to manage the condition (Dieppe 1995). Advice should be given about appropriate exercise, encouraging regular use and mobilization to prevent the further deterioration that immobilization would induce. A balance must be achieved between sufficient weight-bearing and rest and avoiding prolonged overloading of the joint.
Although there is no evidence that diet changes the progressive nature of the disease, the overweight patient should be encouraged to lose weight. Obesity may increase the load on the weight-bearing surfaces, progressing the degenerative process more rapidly (Dieppe 1995). Sticks and other walking support may be appropriate to aid daily living.
Although capsular stretching in the early stage may relieve pain and increase the range of movement, the patient may also require assistance from analgesics. Paracetamol and low-dose ibuprofen may be appropriate in the early stages of the disease (Dieppe 1995). If non-steroidal anti-inflammatory drugs (NSAIDs) are needed to control pain they should be prescribed for short periods of time during acute phases of the disease. The risks of gastro-intestinal disturbance and renal insufficiency from NSAIDs are well documented and patients with osteoarthrosis fall into the older age group which is particularly susceptible to these side-effects (Dieppe 1995, Rang et al 2003). Other forms of pain relief, such as acupuncture, may be effective (McIndoe et al 1995), although Klaber Moffett et al (1996) demonstrated no specific effectiveness for the use of pulsed short wave for osteoarthritic hip or knee pain.
Middle stage osteoarthrosis of the hip (stage ll)
Here the patient’s symptoms and signs indicate a progression of the disease. Pain may be present at rest as well as exacerbated by weight-bearing activities. On examination, a moderate to severe capsular pattern is found and the limited movements have a ‘hard’ end-feel. Capsular stretching may no longer provide benefit and the treatment of choice in the short term may be injection.
A lateral approach is advocated for reasons of safety. Leopold et al (2001) conducted a study of 30 cadaver hips to test the hypothesis that, using anatomical landmarks, the anterior and lateral injection approaches to the hip joint result in reproducibly correct intra-articular needle placement and avoid important periarticular neurovascular structures. The success rate of intra-articular injection was 60% using the anterior approach and 80% using the lateral approach. During the anterior approach the needle passed significantly closer to neurovascular structures than the lateral approach, which was never within 25 mm of any such structures. The study concluded that the lateral approach under fluoroscopy or ultrasound would be the safest and most effective method for injecting the hip joint. It is certainly becoming common practice to perform hip injections with image guidance to ensure intra-articular placement (Robinson et al 2007).
A minimum dose 40 mg of triamcinolone acetonide is recommended but support for a larger dose of 80 mg is provided by a study conducted by Robinson et al (2007) who compared the outcome of infiltration with 40 mg and 80 mg methylprednisolone, using fluoroscopic guidance and an anterior approach. For the 40 mg dose there was statistical improvement in pain and stiffness, but not disability, at week 6 and only the improvement in stiffness remained at 12 weeks. For the 80 mg dose, there was significant improvement in pain, stiffness and disability at week 6 that was maintained at 12 weeks.
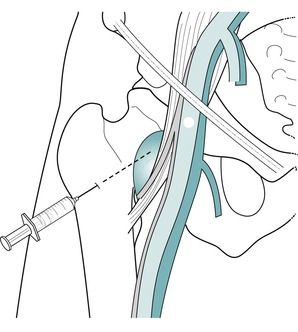
Position the patient in side-lying with the painful leg uppermost and supported in a neutral position on a pillow. Locate the greater trochanter by grasping it between thumb, index and middle fingers; the index finger should be resting on the top of the trochanter. To test you are in the correct position, move the leg passively into some abduction (Fig. 10.35), to relax the iliotibial tract, and you should feel your index finger sink in over the top of the trochanter.
 |
| Figure 10.35
Abducting the hip to locate the hip joint line.
|
The capsule of the hip joint almost completely surrounds the neck of the femur. By inserting the needle just above the index finger, i.e. above the greater trochanter, and aiming vertically downward towards the neck of the femur, the needle should be intracapsular once you gently make contact with bone (Fig. 10.36). You will feel a resistance as the needle pierces first the fascia lata, then the capsule before reaching bone (Fig. 10.37). Deliver the injection as a bolus. The patient is advised to maintain a period of relative rest for approximately 2 weeks following injection.
 |
| Figure 10.36
Injection of the hip joint.
|
 |
| Figure 10.37
Injection of the hip joint showing direction of approach and needle position.
|
Controversy exists concerning repeated steroid injections into weight-bearing joints and the risk of steroid arthropathy (Cameron 1995). Therefore, as a general precaution, repeated corticosteroid injections into the hip joint have not been recommended and it has been advised that no more than two a year should be given without monitoring the degenerative condition of the joint with X-ray investigation. Raynauld et al (2003) conducted a study on repeated injections into the knee joint and established no harmful effects (see Ch. 11), although reassurance for hip injections on the basis of this study cannot be assumed.
Kaspar & de Van de Beer (2005) conducted a retrospective study of 40 patients who had had injections prior to hip arthroplasty and 40 who had not. The hip injections had all been given under sterile theatre conditions with the same dosages of corticosteroid and local anaesthetic but the study found a significantly increased rate of postoperative infection in those hips that had had previous injection. No firm explanation could be given and there was no mention of the length of time after the injection that the hip replacements took place. The outcome of the study does beg for further research to be conducted since, as the authors suggest, previous injection into the hip joint could be considered to be a contraindication to arthroplastic procedures. In contrast to this finding, a similar study to establish the influence of corticosteroid injections on the incidence of infection following total knee arthroplasty found no link between previous injection and subsequent postoperative infection (Horne et al 2008) (see Ch. 11). Further studies are needed to clarify whether previous corticosteroid injection should provide a bar to subsequent replacement surgery. Clinicians should seek the opinion of their local hip surgeons prior to injecting the hip.
Late stage osteoarthrosis of the hip (stage lll)
Conservative management no longer controls the patient’s pain and functional disability may now be serious. Surgery is probably indicated, but there are no agreed criteria or guidelines for electing to perform hip surgery (Dieppe 1995). Pain, age and disability, as well as psychological factors, should all be taken into consideration by the patient and surgeon. Hip resurfacing restores the normal anatomy and biomechanics of the hip joint and provides proximal femoral anatomy and loading to near normal. It allows greater activity levels and tends to be preferred by the younger, fitter population (Heilpern et al 2008).
Injection may be given for pain relief during this stage, as described above.
Rheumatoid arthritis
This may affect the hip joint and symptomatic relief may be gained from intra-articular injection, given as described above.
NON-CAPSULAR LESIONS
Loose body
A loose body in the hip joint causes twinges of pain felt in the groin or radiating down the front of the leg. These twinges may be associated with a momentary sensation of locking or giving way and an inability to weight-bear. This history suggests a loose body in the joint which periodically becomes impacted between the joint surfaces. The loose body may be associated with the rare condition osteochondritis dissecans in adolescents, but most commonly occurs secondary to the onset of degenerative osteoarthrosis at the joint (Cyriax & Cyriax 1993, Saotome et al 2006, Tibor & Sekiya 2008). Loose bodies associated with arthrosis can be chondral, osteochondral or osseous. They can increase in size and progressively worsen the damage to the joint surfaces as well as the clinical symptoms (Bianchi & Martinoli 1999). To avoid this they should be removed arthroscopically (Tibor & Sekiya 2008).
Differential diagnosis should exclude labral tears which are found in the young adult. Labral pathology is often associated with traumatic incidents which may be minor twisting, repetitive flexion or hyperextension injuries. Pain is usually felt in the groin with clicking, locking and/or giving way (O’Kane 1999, Hickman & Peters 2001, Neumann et al 2007). A short stance phase in gait may be evident, or a Trendelenburg gait, and impingement tests, combining forced flexion, adduction and medial rotation, or flexion, abduction with lateral rotation, may reproduce pain (Martin et al 2008, Tibor & Sekiya 2008). There may also be pain at the extremes of movement. Magnetic resonance imaging (MRI) can be used to confirm the tear (Bharam 2006). However, in looking at the diagnostic accuracy of clinical examination in determining intra-articular pain for potential hip arthroscopy candidates, Martin et al (2008) found that even if a labral tear is present on MRI it may not be responsible for the patient’s symptoms and the whole clinical presentation should therefore be considered.
Capsular laxity is an emerging and controversial concept. The laxity may result from acute dislocation or without specific trauma and can occur as a consequence of overuse or repeated axial loading, e.g. in golfers. It may be a cause of anterior hip pain (Tibor & Sekiya 2008).
Signs of a loose body consist of a non-capsular pattern, commonly with pain at the end of range of full passive hip flexion and lateral rotation. If the range of movement demonstrates limitation, a springy end-feel may be appreciated. The principle of treatment applied is to reduce the loose body using strong traction together with Grade A mobilization. If successful, the loose body will be moved to a position within the joint where it no longer causes these typical symptoms.
Two mobilization techniques will be described (Cyriax 1984, Cyriax & Cyriax 1993).
Loose-body mobilization technique 1
Position the patient in supine on the couch with an assistant applying counter-pressure at the anterior superior iliac spines; padding may make it more comfortable for the patient. The assistant must start by applying pressure in an anterior–posterior direction and be prepared to change to apply cephalad pressure towards the end of the manoeuvre.
Your choice of manoeuvre with either lateral or medial rotation will depend on the physical findings during examination and the least painful rotation is attempted first: this is usually medial rotation.
Mobilization 1a: with medial rotation
Stand on the end of the couch, at its lowest height, with your feet close together and parallel to the edge. If local regulations or couch weight safety limits do not allow you to stand on the couch itself, the technique can be adapted and performed whilst standing on the floor. Face the direction of medial rotation and apply a butterfly grip with the thumbs parallel on the lateral aspect of the lower leg, taking care to avoid undue pressure around the malleoli (Fig. 10.38). The hands are wrapped comfortably around the talus and calcaneus to provide anchorage points and pull the ankle into a degree of dorsiflexion, to prevent undue movement at the ankle joint. The forearm rests against the lateral border of the patient’s foot, helping to direct the movement towards medial rotation.
 |
| Figure 10.38
Loose-body mobilization 1a for the hip, showing hand position for mobilization into medial rotation.
|
Next, take your distal leg off the couch and lean out to apply traction with your elbows straight (Fig. 10.39). Maintain the traction throughout the rest of the man-oeuvre, which is to rotate the patient’s leg back and forth towards medial rotation while simultaneously stepping down off the couch; this automatically takes the hip from flexion, towards extension. Re-examine the patient and decide on the next manoeuvre.
 |
| Figure 10.39
Loose-body mobilization 1a for the hip, showing body positioning and assistant’s counter-pressure.
|
Mobilization 1b: with lateral rotation
The manoeuvre is exactly the same as that described above, but in reverse.
Face the movement of lateral rotation and rotate the patient’s leg under strong traction, back and forth towards lateral rotation (Figure 10.40 and Figure 10.41).
 |
| Figure 10.40
Loose-body mobilization 1b for the hip, showing hand position for mobilization into lateral rotation.
|
 |
| Figure 10.41
Loose-body mobilization 1b for the hip, showing body positioning and assistant’s counter-pressure.
|
Loose-body mobilization technique 2 (Cyriax 1984, Cyriax & Cyriax 1993)
Mobilization 2a: with medial rotation
Position the patient in supine on the couch. An assistant applies counter-pressure to the anterior superior iliac spines. Padding may make it more comfortable for the patient (Fig. 10.42). Alternatively a seat belt can be used to maintain the patient’s position on the couch.
 |
| Figure 10.42
Loose-body mobilization 2a for the hip, showing assistant’s hand position.
|
Put your caudal foot up on the couch, beside and below the patient’s buttock. Flex the patient’s knee so that the crook of their knee (popliteal fossa) is placed over your thigh (Fig. 10.43). Take care to avoid pressure on the gastrocnemius muscle as it is uncomfortable.
 |
| Figure 10.43
Loose-body mobilization 2a of the hip, showing application of traction before the thrust into medial rotation.
|
Place one hand on the lateral aspect of the patient’s knee and the other on the medial aspect of the patient’s ankle. An assistant comfortably anchors the patient’s pelvis on the bed. To apply traction, plantarflex your foot on the couch to lift the patient’s leg while simultaneously pushing down on the patient’s ankle. Maintain this traction as you rotate the patient’s leg smartly towards medial rotation of the hip, using the patient’s leg as a lever. Reexamine the patient and decide on the next manoeuvre. Alternatively the patient’s leg may be rotated smartly to and fro as for mobilization.
Mobilization 2b: with lateral rotation
The manoeuvre is exactly the same as that described above, but reverse the hand positions to enable the patient’s leg to be smartly rotated towards lateral rotation (Fig. 10.44). Alternatively the patient’s leg may be rotated smartly to and fro as for mobilization.
 |
| Figure 10.44
Loose-body mobilization 2a of the hip, showing application of traction and the thrust into lateral rotation.
|
Bursitis
Psoas, trochanteric or occasionally ischial bursitis may be a cause of pain at the hip, although these conditions are difficult to diagnose definitively and may be overlooked. They present a muddled clinical picture and may be misdiagnosed as a tendinopathy. However, because of the close anatomical relationship of bursae to tendons, bursitis may coexist with tendinopathy.
The patient commonly presents with a gradual onset of pain, often with no obvious cause. Although it is possible to induce a bursitis by direct trauma, it is usually the result of overuse activity, with the pain increased by activity and better for rest.
On examination, a muddled clinical picture emerges of a non-capsular pattern with some resisted tests and some passive tests reproducing the pain. This may mimic that of tendinopathy. Tendinopathy usually produces a predictable clinical picture of pain on the appropriate resisted test and pain on passive stretching in the opposite direction. In contrast, a bursitis may produce pain when passively squeezed under a contracted muscle or tendon and thus this muddle emerges.
Psoas bursitis
Psoas bursitis produces a local groin pain, but can cause pain to be referred into the L3 dermatome. It has a gradual onset of pain with the patient unable to recall the precipitating factors. It may be associated with overuse or repetitive movements and exacerbated by hip flexion movements, e.g. bending to put on shoes and socks, rising from sitting with hips flexed, walking up stairs or hills, brisk walking, jogging or kicking (Broadhurst 1995a). The pain may produce a shortened gait stride and, through underuse, a secondary capsulitis.
Primary effusion of the bursa is possible, but its communication with the hip joint makes it a reservoir for joint effusion. Therefore psoas bursitis is often associated with hip joint involvement, especially rheumatoid arth-ritis (Armstrong & Saxton 1972, Meaney et al 1992).
On examination, a non-capsular pattern exists with a combination of passive hip flexion and adduction, squeezing the bursa and producing pain, which may be used as a comparable sign. Other signs could include pain on passive lateral rotation, passive extension and resisted flexion of the hip. However, clinically, resisted flexion is usually found to be pain-free (Cyriax 1982).
Some enlarged bursae have been reported to produce a palpable mass in the groin, causing extrinsic pressure on adjacent neurovascular structures (Underwood et al 1988, Toohey et al 1990, Meaney et al 1992). On diagnostic scanning these enlarged bursae have been shown to contain solid components consisting of various debris, e.g. cellular debris, osteocartilaginous plaques, fibrin, clot and calcium deposits (Meaney et al 1992).
Differential diagnosis should exclude lumbar spine involvement and other pelvic and hip joint pathology such as stress and avulsion fractures, as well as so-called ‘Gilmore’s groin’, a disruption of the external oblique aponeurosis causing dilatation of the superficial inguinal ring, torn conjoined tendon and dehiscence between the inguinal ligament and the torn conjoined tendon. Males are more commonly affected. It presents as a gradual onset of groin pain in athletes, particularly footballers. The pain is increased by sporting activity, on getting out of bed, especially the day after a game, and on sudden movement, e.g. sprinting or coughing. On examination there are no physical findings. Diagnosis is made by the examining doctor inverting the scrotum and examining the superficial inguinal ring. On the symptomatic side the ring is dilated and tender and there may be a cough impulse. This condition may require surgical repair (Gilmore 1995, Williams & Foster 1995).
Treatment for psoas bursitis is a large-volume, low-dose local anaesthetic plus an appropriate amount of corticosteroid.
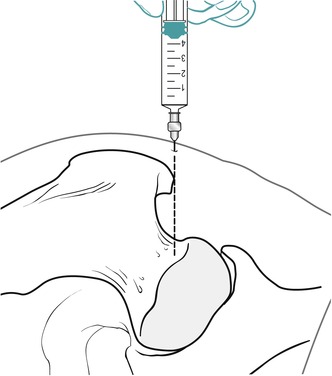
Position the patient in supine on the couch. Locate the psoas bursa by palpating for the femoral pulse just distal to the midpoint of the inguinal ligament. This is the surface marking point for the position of the psoas bursa; mark this point. Move approximately 5 cm laterally and 5 cm distally, marking both of these points. If you draw an imaginary line to connect these three points you will form an inverted right-angled triangle (Fig. 10.45). This now gives you the angle of insertion which is to follow the direction of the hypotenuse, aiming to pass deeply, in order to traverse under the neurovascular bundle in the femoral triangle, to reach the deeply located psoas bursa (Fig. 10.46).
 |
| Figure 10.45
Surface markings for injection of psoas bursitis.
|
 |
| Figure 10.46
Injection of psoas bursitis.
|
Once the needle tip makes contact with bone it should be located in the region of the hip joint anteriorly. Withdraw it slightly into the overlying psoas bursa and inject at this point (Fig. 10.47). It may be possible to inject as a bolus but, more commonly, a peppering technique is required to cover the extent of this large bursa, fanning out to cover an area approximately the size of a golf ball (Cyriax & Cyriax 1993). The patient is advised to maintain a period of relative rest for approximately 2 weeks following injection.
 |
| Figure 10.47
Injection of psoas bursitis showing direction of approach and needle position.
|
Trochanteric bursitis
Trochanteric bursitis involves inflammation of the bursae associated with the gluteal muscles and their insertion into the greater trochanter. Although several bursae around the hip region are prone to inflammation, trochanteric bursitis is the most common (Adkins & Figler 2000).
The cause is occasionally traumatic through direct injury, but more commonly due to overuse through occupational or sporting activities. It may be associated with a tight ilio-tibial band where the bursa may be irritated by direct friction, or secondary to altered biomechanics of gait, leg length discrepancy, low back pain or sacroiliac dysfunction (Haller et al 1989, Collée et al 1991, Norris 1998, Caruso & Toney 1994). Differential diagnosis should also include piriformis syndrome which presents with pain in a similar distribution and is associated with tenderness to palpation at the sciatic notch and greater trochanter (Brukner & Khan 2007, Tibor & Sekiya 2008) (see Ch. 14).
Trochanteric bursitis is common in obese, middle-aged women (Rasmussen & Fano 1985, Allwright et al 1988, Gerber & Herrin 1994). It may also be secondary to arthritis of the hip joint and it is not uncommon to find the bursa tender after total hip replacement (Dennison & Beverland 2002).
The pain is usually a diffuse ache or burning pain felt over the lateral aspect of the hip and/or referred down the lateral aspect of the leg.
Aggravating factors are walking, climbing stairs, standing for prolonged periods, crossing the legs in sitting and lying on the affected side.
On examination the typical muddled clinical picture of bursitis may emerge with some or all of the following involved: a non-capsular pattern of pain on passive hip flexion, abduction and lateral rotation as the bursa is squeezed – these movements in combination may be positive (FABER test), passive adduction which may compress the bursa, and resisted abduction which may produce the pain as the bursa is compressed by the contraction of adjacent muscles (Little 1979, Cyriax & Cyriax 1993, Dennison & Beverland 2002). Frequently, diagnosis depends on the typical history of presentation and pain referral, an absence of physical signs, and tenderness to palpation of the greater trochanter.
Palpation will reveal the area of inflammation, typically over the superolateral aspect of the greater trochanter. Care should be taken in palpation, to compare with the un-affected side, as trigger points are commonly found in the buttock, which can be misleading. Differential diagnosis should include iliotibial band syndrome, with which trochanteric bursitis can coexist. Iliotibial band syndrome presents with a similar pattern of lateral hip and/or knee pain, but is painful on provocative testing using Ober’s test as follows: with the patient in side-lying, the hip neutral and the knee flexed, extend the hip and adduct the femur. Iliotibial band tightness and/or lateral thigh pain will be demonstrated as the knee will extends as when the femur is adducted (Adkins & Figler 2000, Brukner & Khan 2007).
Once diagnosis is established, the treatment of choice is an injection of low-dose, large-volume local anaesthetic with an appropriate amount of corticosteroid.
Suggested needle size: 21G × 1½ in (0.8 × 40 mm) or 21G × 2 in (0.8 × 50 mm) green needle
Dose: 20 mg triamcinolone acetonide in a total volume of 3–5 mL
Position the patient comfortably in side-lying and palpate for the area of tenderness over the superolateral aspect of the greater trochanter where gluteus maximus inserts into the iliotibial tract (Fig. 10.48). Deliver the injection by a bolus technique if no resistance is felt, or, if this is not possible due to synovial folds and adhesions within the bursa, redirect the needle and use a series of smaller injections to infiltrate the area of tenderness (Fig. 10.49). The patient is advised to maintain a period of relative rest for approximately 2 weeks following injection.
 |
| Figure 10.48
Injection of the trochanteric bursa.
|
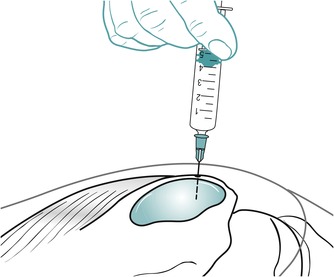 |
| Figure 10.49
Injection of the trochanteric bursa showing direction of approach and needle position.
|
Gluteal bursitis
Injection of the more common trochanteric bursa has been described above, but any of the bursae associated with the gluteal muscles may be affected. The patient presents with a muddle of signs as described above and palpation will indicate the area involved. Once the area of tenderness has been identified it can be injected using a series of small bolus injections by redirecting the needle with small insertions and withdrawals to infiltrate the whole area of tenderness.
Ischial bursitis
An ischial bursitis (weaver’s bottom) involves the ischial bursa of gluteus maximus. It produces pain on prolonged sitting, especially on hard surfaces; the pain is relieved by standing. Pain may be reproduced near the end of range of the straight leg raise (Broadhurst 1995b). It is a rare cause of buttock pain but the principles of treatment can be applied.
Complicated bursitis
Septic bursitis has been described, more commonly occurring in the olecranon and prepatellar bursae, where Staphylococcus aureus was usually the infective organism (Hoppmann 1993, Zimmermann et al 1995). A case of tuberculosis of the trochanteric bursa has also been described (Rehm-Graves et al 1983). Bursitis has also been reported as a cause of hip pain associated with rheumatoid arthritis (Raman & Haslock 1982). Pain referred from the lumbar spine and sacroiliac joint may produce a similar pattern of signs and symptoms and has been described by Traycoff (1991) as pseudotrochanteric bursitis. Occasionally bursitis may be complicated by calcification, making it resistant to normal conservative management (Gerber & Herrin 1994).
Sign of the buttock
The sign of the buttock is pain produced on straight leg raise which increases on flexing the knee and hip (Cyriax & Cyriax 1993, Hattam & Smeatham 2010). An empty end-feel is appreciated as more range of movement is available, but any attempt to produce more hip flexion is abruptly stopped by voluntary muscle spasm and the patient puts out the hand to stop the movement.
A positive sign indicates a major lesion in the buttock or hip region. The history will usually reveal an unwell patient, who looks ill and may have a fever with night sweats and rigors. The pain may be unrelenting in the buttock, hip or leg. It is not eased by rest and therefore night pain is a feature.
On examination, a non-capsular pattern of movement at the hip, and often the lumbar spine, is discovered. Pain may be increased by lumbar flexion and resisted tests at the hip, but the cardinal feature of this condition is the positive sign of the buttock.
Possible causes of the sign of the buttock are neoplasm of the upper femur or ilium, fracture of the sacrum, ischiorectal abscess, sepsis, either septic bursitis or arthritis, or osteomyelitis of the upper femur (Cyriax & Cyriax 1993). Urgent medical attention and further investigation are required.
CONTRACTILE LESIONS
The mode of onset of contractile lesions around the hip may be sudden through strain, gradual through overuse or traumatic through direct injury, causing muscle contusion. Lesions commonly affect the hamstrings, quadriceps and adductor longus muscles. Less common lesions of the psoas and sartorius are not described, although the principles of diagnosis and treatment would equally apply to any muscle lesion in the region.
Hamstrings
The hamstrings act to extend the hip and flex the knee and commonly present as strained, perhaps due to their relative weakness in comparison to the quadriceps (Sutton 1984). As two-joint muscles, they are susceptible to injury, because there is a greater potential for overuse. Injury can occur at the tendinous origin at the ischial tuberosity, within the muscle belly, or at the musculotendinous junction.
The onset is usually sudden, e.g. on a sudden stretch or a rapid contraction against resistance such as the ballistic action of sprinting, which produces acute pain, further increased by activity, swelling and bruising. The vulnerable phase in the running cycle appears to be at the end of the swing phase, where peak muscle lengths occur, and the beginning of the stance phase. Biceps is more susceptible as its peak length exceeds that of the medial hamstrings (Hunter & Speed 2007).
Symptoms may include stiffness, muscle cramps and spasms in the posterior aspect of the distal thigh or weak knee flexion. Patients with a complete distal hamstring tear may also report a sensation of instability at the knee and diagnostic imaging may be required as an adjunct to clinical examination to aid decision-making in the management of more severe lesions (Lempainen et al 2007).
Precipitating factors have been put forward as altered posture, poor condition, inadequate warm-up and fatigue (Sutton 1984, Worrell 1994). In exploring various established and speculative management approaches, Hoskins & Pollard (2005) were unable to find conclusive evidence for a wider range of specific factors leading to hamstring injury, namely muscle strength and balance, warm-up, fatigue, flexibility, body mechanics, sports-specific activities, psychosocial factors or running technique. Hunter & Speed (2007) reviewed this list of possible factors and also looked at age and previous injury. From their own review they found that only age and previous injury had confident support as risk factors.
Croisier et al (2008) have since looked at the role of muscle imbalance in hamstring injury. Pre-season isokinetic concentric and eccentric testing was performed on 687 professional soccer players to monitor strength imbalances. Follow-up was obtained in 462 players within whom 35 hamstring injuries were recorded and it was demonstrated that players with untreated muscle imbalances were four to five times more likely to sustain a hamstring injury than those recorded as normal.
The patient may report tightness or pain in the posterior thigh some time before the acute onset. Gradual onset due to overuse is possible and injuries may occur in dancers following sustained stretching at warm-up, whilst dancing, or during cool-down (Askling et al 2006). Askling et al observed 18 sprinters and 15 dancers and noted that, although injuries of sudden onset were functionally worse initially, they tended to return to pre-injury levels more quickly than the slower onset injuries, with an average of 16 weeks for the former group and 50 weeks for the latter. Re-injury is relatively common at 12–17% and Askling et al implicate early or over-zealous stretching as a contributing factor.
Chronic hamstring strain is more commonly the result of a previous acute episode which may have healed during a period of relative immobilization. Consequent tightness or shortening of the muscle belly makes it vulnerable to repeated injury. Koulouris et al (2007) conducted a study to identify whether any MRI-identifiable parameters could be predictive of athletes at risk of sustaining a recurrent hamstring injury within the same playing season. The only statistically significant risk factor for recurrent hamstring strain was a history of anterior cruciate ligament injury. However, it was noted that reinjured muscles presented with an increased length of tear and of the imaged parameters the measured length of the strain had the strongest correlation with a repeat strain.
On examination the patient has pain on resisted knee flexion and pain on passive straight leg raising. In most clinic situations, testing for hamstring strain is conducted statically in a non-weight-bearing position. In reality the hamstrings function, and are most often injured, in dynamic weight-bearing situations. This is an important point to remember for full rehabilitation of any muscle lesion in the region.
Palpation reveals the site of the lesion, with muscle belly strains commonly occurring deeply in the mid-thigh region. Chronic overuse strain occurs at the origin from the ischial tuberosity. Treatment of the origin may be by deep transverse frictions or injection.
Transverse frictions to the origin of the hamstrings
Position the patient into side-lying on the unaffected side with the hips and knees flexed to 90° to expose the ischial tuberosity from under the lower border of gluteus maximus (Fig. 10.50). Stand behind the patient’s waist facing across the couch. Frictions can then be applied transversely across the fibres using the fingers of one hand reinforced with the other hand to maintain pressure back against the origin, and rocking body weight downwards and upwards through straight arms. Start gently, then apply deep transverse frictions for 10 min after the analgesic effect is achieved. Relative rest is advised where functional movements may continue, but no overuse or stretching until the muscle is pain-free on resisted testing.
 |
| Figure 10.50
Transverse frictions to the origin of the hamstrings.
|
An alternative position involves positioning the patient in prone-lying with the knee supported over the edge of the bed on a stool to place the hip and knee into flexion and to expose the ischial tuberosity (Fig. 10.51). Apply transverse frictions by using one thumb reinforced with the other, directed firstly up against the ischial tuberosity and then transversely across the fibres.
 |
| Figure 10.51
Transverse frictions to the origin of the hamstrings, alternative position.
|
Use either position adopted for transverse frictions of the hamstrings’ origin. Locate the area of tenderness over the ischial tuberosity and insert the needle perpendicular to it (Fig. 10.52). Deliver the injection by a peppering technique into the teno-osseous junction (Fig. 10.53). The patient is advised to maintain a period of relative rest for approximately 2 weeks following injection.
 |
| Figure 10.52
Injection of the origin of the hamstrings.
|
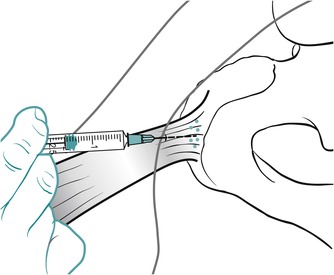 |
| Figure 10.53
Injection of the origin of the hamstrings showing direction of approach and needle position.
|
Transverse frictions for acute muscle belly
Apply the principles of treatment for acute lesions, with protection, rest, ice, compression and elevation (PRICE) being applied as soon as possible after the onset and for 2–3 days following injury. Treatment is conducted on a daily basis and transverse frictions applied gently to maintain the muscle belly function. Position the patient in prone-lying with the knee flexed, to place the muscle belly in the shortened position; this allows the muscle fibres to be moved transversely by the frictions (Fig. 10.54). Apply the transverse frictions gently and, once some analgesia has been achieved, apply approximately six deeper sweeps. Follow this immediately with Grade A mobilization, encouraging an active muscle contraction within the pain-free range to broaden the fibres. Teach the patient to use a normal heel–toe gait, with the aid of crutches if necessary.
 |
| Figure 10.54
Transverse frictions to the hamstring muscle bellies.
|
After approximately 5 days (depending upon irritability) the depth of transverse frictions and Grade A mobilizations can be increased until a full range of pain-free movement is achieved. Treating an acute muscle belly lesion in this way should avoid shortening of the muscle fibres and the need to apply stretching techniques.
Home stretching exercises can be given to support this approach but taking care to avoid overstressing the healing fibres by avoiding pain. In support of this, Malliaropoulos et al (2004) looked at the role of stretching in the rehabilitation of hamstring injuries, dividing 80 athletes with hamstring strains into two groups. The groups were taught to apply static stretches within the pain-free range for 30 s and to perform four repetitions. One group was directed to apply the regime once a day and the other four times a day. In the study, the group applying the stretch more frequently achieved full movement and returned to activity more quickly.
Transverse frictions for chronic muscle belly
Apply the transverse frictions with the muscle belly in a relaxed position and once the analgesic effect is achieved, apply deeper transverse frictions for 10 min (Figure 10.54 and Figure 10.55). Follow this with vigorous Grade A exercises to maintain the mobility gained.
 |
| Figure 10.55
Transverse frictions to the hamstring muscle bellies, alternative technique (chronic).
|
It is important that the hamstrings are not undertreated and, to prevent recurrence of symptoms, transverse frictions should be continued for approximately 1 week after cessation of symptoms. If the muscle is tight, traditional stretches can be applied once the resisted tests are pain-free but the stretches themselves should never go further than nudging into pain.
Rehabilitation following hamstring lesions
In either the acute or the chronic situation, once the hamstrings have been rendered pain-free by transverse frictions and Grade A mobilizations, a full rehabilitation programme can be implemented, including stretching to lengthen the muscle if appropriate. Mason et al (2008) support the use of graded stretching exercises within the pain-free range and also advise that consideration should be given to the lumbar spine, sacroiliac and pelvic alignment and postural control mechanisms in the rehabilitation of hamstring injuries. Attention should be paid to the dynamic rather than the static function of the hamstrings and weight-bearing sport-specific activities and rehabilitation under speed are important considerations (Coole & Gieck 1987). Hunter & Speed (2007) summarize that the aim of rehabilitation is to cause adaptation in the muscle tendon unit of the hamstrings and the adjacent supporting tissues, to allow the entire system to absorb sufficient energy and to facilitate a full return to functional activity.
Quadriceps
The mechanism of injury of the quadriceps is similar to that of the hamstrings and the principles of treatment and rehabilitation can be applied in much the same way. The patient presents with anterior thigh pain, pain on resisted knee extension and pain on resisted hip flexion (if rectus femoris is involved). As a two-joint muscle, rectus femoris is the most susceptible to injury. Palpation reveals the site of the lesion, which may be within the tendon of rectus femoris from the anterior inferior iliac spine, or in the belly of the muscle, usually mid-thigh (see Ch. 11).
Transverse frictions to the origin of rectus femoris (Cyriax 1984, Cyriax & Cyriax 1993)
Position the patient in half-lying to allow the hip flexors to relax. Locate the origin of rectus femoris and apply two fingers to the tendon (Fig. 10.56). Push down onto the tendon and apply transverse frictions across the fibres. Since the lesion is usually chronic, 10 min transverse frictions are applied after the analgesic effect is achieved. Relative rest is advised where functional movements may continue, but no overuse or stretching until the muscle is pain-free on resisted testing.
 |
| Figure 10.56
Transverse frictions to the origin of rectus femoris.
|
Adductor longus
Adductor longus is the most common adductor muscle to be strained at the hip. It is sometimes known as a ‘rider’s strain’ due to overuse of adductor longus in working a horse while riding.
The patient has groin or medial thigh pain, often presenting as a dull ache, with pain on resisted adduction and passive abduction (Tibor & Sekiya 2008). The lesion is in one of two sites: either the origin from the pubis or the musculotendinous junction. Treatment of the origin is by either transverse frictions or injection. The musculotendinous junction usually responds well to transverse frictions and injection is not usually necessary.
Transverse frictions to adductor longus
Teno-osseous site
Position the patient in supine with the leg in a degree of abduction and lateral rotation, supported on a pillow. With an index finger reinforced by the middle finger, locate the area of tenderness at the teno-osseous junction (Fig. 10.57). Apply the frictions firstly in a direction down onto the bone, then transversely across the fibres, for 10 min after gaining analgesia. This may be an embarrassing treatment for the patient and it may be more appropriate to teach patients to do the transverse frictions themselves.
 |
| Figure 10.57
Transverse frictions to the origin of adductor longus.
|
Musculotendinous site
Position the patient as above and locate the area of tenderness at the musculotendinous junction. The transverse frictions may be imparted by a pinching manoeuvre (Fig. 10.58) (Cyriax 1984, Cyriax & Cyriax 1993), or by pressure directed firstly down against the tendon and then transversely across the fibres (Fig. 10.59). Apply the transverse frictions for 10 min after gaining analgesia.
 |
| Figure 10.58
Transverse frictions to adductor longus, musculotendinous site.
|
 |
| Figure 10.59
Transverse frictions to adductor longus, musculotendinous site, alternative hand position.
|
Relative rest is advised where functional movements may continue, but no overuse or stretching until the muscle is pain-free on resisted testing.
Position the patient as for the transverse frictions. Insert the needle into the origin of adductor longus, which is situated in the angle between the symphysis and the obturator crest (Fig. 10.60). Once in the teno-osseous junction and in contact with bone, deliver the injection by the peppering technique (Fig. 10.61). The patient is advised to maintain a period of relative rest for approximately 2 weeks following injection.
 |
| Figure 10.60
Injection of the origin of adductor longus.
|
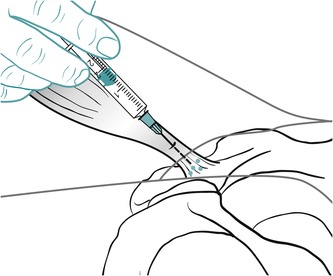 |
| Figure 10.61
Injection of the origin of adductor longus showing direction of approach and needle position.
|
REFERENCES
Adkins, S.B.; Figler, R.A., Hip pain in athletes, Am. Fam. Phys. 61 (7) ( 2000) 2109–2118.
Allwright, S.J.; Cooper, R.A.; Nash, P., Trochanteric bursitis: bone scan appearance, Clin. Nucl. Med. 13 (1988) 561–564.
Armstrong, P.; Saxton, H., Ilio-psoas bursa, Br. J. Rheumatol. 45 (1972) 493–495.
Askling, C.; Saartok, T.; Thorstensson, A., Type of acute hamstring strain affects flexibility, strength and time to return to pre-injury level, Br. J. Sports Med. 40 (2006) 40–44.
Bharam, S., Labral tears, extra-articular injuries and hip arthroscopy in the athlete, Clin. Sports Med. 25 (2006) 279–292.
Bianchi, S.; Martinoli, C., Detection of loose bodies in joints., Radiol. Clin. N. Am. 37 (4) ( 1999) 679–690.
Broadhurst, N., Iliopsoas tendinopathy and bursitis, Aust. Fam. Phys. 24 (1995) 1303.
Broadhurst, N., Ischial bursitis, Aust. Fam. Phys. 24 (1995) 1121.
Brukner, P.; Khan, K., Clinical Sports Medicine. 3rd edn ( 2007)McGraw Hill, Sydney.
Cailliet, R., Soft Tissue Pain and Disability. 2nd edn ( 1990)F A Davis, Philadelphia.
Cameron, G., Steroid arthropathy – myth or reality?J. Orthop. Med. 17 (1995) 51–55.
Canoso, J.J., Bursae, tendons and ligaments., Clin. Rheum. Dis. 7 (1981) 189–221.
Caruso, F.A.; Toney, M.A.O., Trochanteric bursitis – a case report of plain film, scintigraphic and MRI correlation, Clin. Nucl. Med. 19 (1994) 393–395.
Collée, G.; Dijkmans, B.A.C.; Vandenbroucke, J.P.; et al., Greater trochanteric pain syndrome trochanteric bursitis in low back pain, Scand. J. Rheumatol. 20 (1991) 262–266.
Coole, W.; Gieck, J.H., An analysis of hamstring strains and their rehabilitation, J. Orthop. Sports Phys. Ther. 9 (1987) 77–85.
Croisier, J-Louis.; Ganteaume, S.; Binet, J.; et al., Strength imbalances and prevention of hamstring injury in professional soccer players, Am. J. Sports Med. 36 (8) ( 2008) 1469–1475.
Cyriax, J., 8th ednTextbook of Orthopaedic Medicine. vol 1 ( 1982)Baillière Tindall, London.
Cyriax, J., 11th ednTextbook of Orthopaedic Medicine. vol 2 ( 1984)Baillière Tindall, London.
Cyriax, J.; Cyriax, P., Cyriax’s Illustrated Manual of Orthopaedic Medicine. ( 1993)Butterworth Heinemann, Oxford.
Dennison, J.; Beverland, D.E., An audit of trochanteric bursitis in total hip arthroplasty and recommendations for treatment., J. Orthop. Nurs. 6 (1) ( 2002) 5–8.
Dieppe, P., Management of hip osteoarthritis, Br. Med. J. 311 (1995) 853–857.
Emms, N.W.; O’Connor, M.; Montgomery, S.C., Hip pain can masquerade as knee pain in adults, Age Ageing 31 (2002) 67–69.
Flanagan, F.L.; Sant, S.; Coughlan, R.J.; et al., Symptomatic enlarged iliopsoas bursae in the presence of a normal plain hip radiograph., Br. J. Rheumatol. 34 (1995) 365–369.
Fu, Z.; Peng, M.; Peng, Q., Anatomical study of the synovial plicae of the hip joint, Clin. Anat. 10 (4) ( 1997) 235–238.
Gerber, J.M.; Herrin, S.O., Conservative management of calcific trochanteric bursitis, J. Manip. Physiol. Ther. 17 (1994) 250–252.
Gilmore, O.J.A., Gilmore’s groin, Physiother. Sport 18 (1995) 14–15.
Gough-Palmer, A.; McHugh, K., Investigating hip pain in a well child, Br. Med. J. 334 (2007) 216–1217.
Haller, C.C.; Coleman, P.A.; Estes, N.C.; et al., Traumatic trochanteric bursitis, Kans. Med. 90 (1989) 17–22.
Hartley, A., Practical Joint Assessment – Lower Quadrant. 2nd edn ( 1995)Mosby, London.
Hattam, P.; Smeatham, A., Special Tests in Musculoskeletal Examination. ( 2010)Churchill Livingstone, Edinburgh.
Heilpern, G.N.A.; Shah, N.N.; Fordyce, M.J.F., Birmingham hip resurfacing arthroplasty., J. Bone Joint Surg. 90 (9) ( 2008) 1137–1142.
Hickman, J.M.; Peters, C.L., Hip pain in the young adult, Am. J. Orthop. 30 (6) ( 2001) 459–467.
Hoppmann, R.A., Diagnosis and management of common tendinopathy and bursitis syndromes., J. S. C. Med. Assoc. 89 (1993) 531–535.
Horne, G.; Devane, P.; Davidson, A.; et al., The influence of steroid injections on the incidence of infection following total knee arthroplasty, N. Z. Med. J. 121 (1268) ( 2008) 1–11.
Hoskins, W.; Pollard, H., The management of hamstring injury – Part 1: Issues in diagnosis, Man. Ther. 10 (2) ( 2005) 96–107.
Hunter, D.G.; Speed, C.A., The assessment and management of chronic hamstring/posterior thigh pain., Best Pract. Res. Clin. Rheumatol. 21 (2) ( 2007) 261–277.
Jenkins, J.T.; O’Dwyer, P.J., Inguinal hernias, Br. Med. J. 336 (2008) 269–272.
Kapandji, I.A., 5th ednThe Physiology of the Joints: Lower Limb. vol 2 ( 1987)Churchill Livingstone, Edinburgh.
Kaspar, S.; de Van de Beer, J., Infection in hip arthroplasty after previous injection of steroid, J. Bone Joint Surg. 87-B (2005) 454–457.
Kersnic, B.; Iglic, A.; Kralj-Iglic, V.; et al., Increased incidence of arthrosis in women could be related to femoral and pelvic shape, Arch. Orthop. Trauma. Surg. 116 (6–7) ( 1997) 345–347.
Klaber Moffett, J.A.; Richardson, P.H.; Frost, H.; et al., A placebo controlled double blind trial to evaluate the effectiveness of pulsed short wave therapy for osteoarthritic hip and knee pain., Pain 71 (2) ( 1996) 121–127.
Klässbo, M.; Harms-Ringdahl, K.; Larrson, G., Examination of passive ROM and capsular patterns in the hip, Physiother. Res. Int. 8 (1) ( 2003) 1–12.
Koulouris, G.; Connell, D.A.; Brukner, P.; Schneider-Kolsky, M., Magnetic resonance imaging parameters for assessing risk of recurrent hamstring injuries in elite athletes, Am. J. Sports Med. 35 (9) ( 2007) 1500–1506.
Kumar, P.; Clark, M., Clinical Medicine. 5th edn ( 2002)Baillière Tindall, London.
Lempainen, L.; Sarimo, J.; Mattila, K.; et al., Distal tears of the hamstring muscles: review of the literature and our results of surgical treatment, Br. J. Sports Med. 41 (2) ( 2007) 80–83.
Leopold, S.S.; Battista, V.; Oliverio, J.A., Safety and efficacy of intra-articular hip injection using anatomic landmarks, Clin. Orthop. Relat. Res. 391 (2001) 192–197.
Lesher, J.M.; Dreyfuss, P.; Hager, N.; et al., Hip referral patterns: a descriptive study, Pain Med. 9 (1) ( 2008) 22–25.
Little, H., Trochanteric bursitis: a common cause of pelvic girdle pain, Can. Med. Assoc. J. 120 (1979) 456–458.
McGory, B.J.; Endrizzi, D.P., Adhesive capsulitis of the hip after bilateral adhesive capsulitis of the shoulder., Am. J. Orthop. 29 (6) ( 2000) 457–460.
McIndoe, A.K.; Young, K.; Bone, M.E., A comparison of acupuncture with intra-articular steroid injection as analgesia for osteoarthritis of the hip., Acupuncture Med. 13 (1995) 67–70.
Malliaropoulos, N.; Papalexandris, S.; Papalada, A.; et al., The role of stretching in rehabilitation of hamstring injuries: 80 athletes follow-up., Med. Sci. Sports Med. 36 (5) ( 2004) 756–759.
Martin, R.L.; Irrgang, J.J.; Sekiya, J.K., The diagnostic accuracy of clinical examination in determining intra-articular hip pain for potential hip arthroscopy candidates., J. Arthroscopic Relat. Surg. 24 (9) ( 2008) 1013–1018.
Mason, D.L.; Dickens, V.; Vail, A., Rehabilitation for hamstring injuries. Cochrane Database Syst. Rev. (1)CP004575, Coch. Database Syst. Rev. ( 4) ( 2008).
Meaney, J.F.; Cassar-Pullicino, V.N.; Ethrington, R.; et al., Ilio-psoas bursa enlargement, Clin. Radiol. 45 (1992) 161–168.
Neumann, G.; Mendicuti, A.D.; Zou, K.H.; et al., Prevalence of labral tears and cartilage loss in patients with mechanical symptoms of the hip: evaluation using MR arthrography, Osteoarthr. Cartil. 15 (2007) 909–1017.
Norris, C.M., Sports Injuries: Diagnosis and Management for Physiotherapists. 2nd edn ( 1998)Butterworth Heinemann, Oxford.
O’Kane, J.W., Anterior hip pain, Am. Fam. Phys. 60 (6) ( 1999) 1687–1696.
Paice, E., Pain in the hip and knee, Br. Med. J. 310 (1995) 319–322.
Raman, D.; Haslock, I., Trochanteric bursitis – a frequent cause of ‘hip’ pain in rheumatoid arthritis, Ann. Rheum. Dis. 41 (1982) 602–603.
Rang, H.P.; Dale, M.M.; Ritter, J.M.; et al., Pharmacology. 5th edn ( 2003)Churchill Livingstone, Edinburgh.
Rasmussen, K.-J.E.; Fano, N., Trochanteric bursitis: treatment by corticosteroid injection, Scand. J. Rheumatol. 14 (1985) 417–420.
Raynauld, J.-P.; Buckland-Wright, C.; Ward, R.; et al., Safety and efficacy of long-term intraarticular steroid injection in osteoarthritis of the knee, Arthritis Rheum. 48 (2) ( 2003) 370–377.
Rehm-Graves, S.; Weinstein, A.J.; Calabrese, L.H.; et al., Tuberculosis of the greater trochanter bursa, Arthritis Rheum. 26 (1983) 77–81.
Robinson, P.; Keenan, A.-M.; Conaghan, P.G., Clinical effectiveness and dose of image-guided intra-articular corticosteroid injection for hip osteoarthritis., Rheumatology 46 (2) ( 2007) 285–291.
Saotome, K.; Tamai, K.; Osada, D.; et al., Histologic classification of loose bodies in osteoarthrosis., J. Orthop. Sci. 11(6) (2006) 607–613.
Saunders, S., Orthopaedic Medicine Course Manual. ( 2000)Saunders, London.
Sims, K., The development of hip osteoarthritis: implications for conservative management, Man. Ther. 4 (3) ( 1999) 127–135.
Standring, S., Gray’s Anatomy: the Anatomical Basis of Clinical Practice. 14th edn ( 2009)Churchill Livingstone, Edinburgh.
Sutton, G., Hamstrung by hamstring strains: a review of the literature, J. Orthop. Sports Phys. Ther. 5 (1984) 184–195.
Tibor, L.M.; Sekiya, J.K., Differential diagnosis of pain around the hip join., Arthroscopy 24 (12) ( 2008) 1407–1421.
Toohey, A.K.; LaSalle, T.L.; Martinez, S.; et al., Iliopsoas bursitis: clinical features, radiographic findings, and disease associations, Semin. Arthritis Rheum. 20 (1990) 41–47.
Traycoff, R.B., ‘Pseudotrochanteric bursitis’: the differential diagnosis of lateral hip pain, J. Rheumatol. 18 (1991) 1810–1812.
Underwood, P.L.; McLeod, R.A.; Ginsburg, W.W., The varied clinical manifestations of iliopsoas bursitis, J. Rheumatol. 15 (1988) 1683–1685.
Williams, P.; Foster, M.E., Gilmore’s groin – or is it?Br. J. Sports Med. 29 (3) ( 1995) 206–208.
Worrell, T.W., Factors associated with hamstring injuries – an approach to treatment and preventative measures, Sports Med. 17 (1994) 338–345.
Zimmermann, B.; Mikolich, D.J.; Ho, G., Septic bursitis, Semin. Arthritis Rheum. 24 (1995) 391–410.