2 The Fetal Echocardiogram
Background
A variety of maternal or fetal disorders may place a fetus at increased risk for congenital heart disease (CHD) (Table 2-1). If present, a fetal echocardiogram is indicated, and timely referral is recommended. Combined, approximately 5% of pregnancies are referred for in utero evaluation. Abnormal or unsatisfactory (the inability to establish normal) cardiac views obtained as part of an obstetric anatomic survey account for more than 20% of all referrals for in utero evaluation and lead to more than half of all prenatal diagnoses. The anatomic survey, a nearly universal mid-pregnancy ultrasound scan, includes a four-chamber (4C) view of the heart and, if possible, views of both outflow tracts. A positive family history accounts for another nearly 20% of all referrals. However, these are the source of less than 5% of all prenatal diagnoses.
| Maternal Indications | Fetal Indications |
|---|---|
| Family history of CHD including prior child or pregnancy with CHD | Abnormal obstetric screening ultrasound |
| Metabolic disorders (e.g., diabetes) | Extracardiac abnormality |
| Exposure to teratogens | Chromosomal abnormality |
| Exposure to prostaglandin synthetase inhibitors (ibuprofen) | Arrhythmia |
| Infection (rubella, coxsackie virus, parvovirus B19) | Hydrops |
| Autoimmune dx (e.g., Sjögren syndrome, SLE) | Increased first trimester nuchal translucency |
| Familial inherited disorder (Marfan, Noonan syndromes) | Multiple gestation and suspicion for twin-twin transfusion syndrome |
| In vitro fertilization |
Cardiac Embryology and In Utero Physiology
Cardiac Embryology
Overview
A complete fetal echocardiogram includes two-dimensional (2D) evaluation of cardiac anatomy, spectral and color Doppler interrogation, and an assessment of cardiac function and rhythm. The components of a comprehensive evaluation are listed in Table 2-2, although not all may be visualized in every fetus at every examination. Similar to transthoracic imaging, fetal echocardiography depends on the ability to obtain standard views and evaluate structures in orthogonal views. The fetus may be very active, and the examiner may need to piece together many partial images to form a composite picture, particularly in the presence of complex CHD.
| Overview |
Study Protocol
2D Images
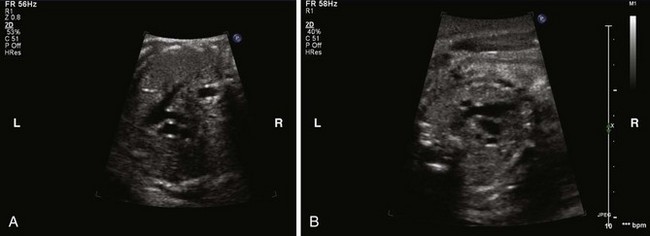
Abdominal and Cardiac Situs
The Four-Chamber View
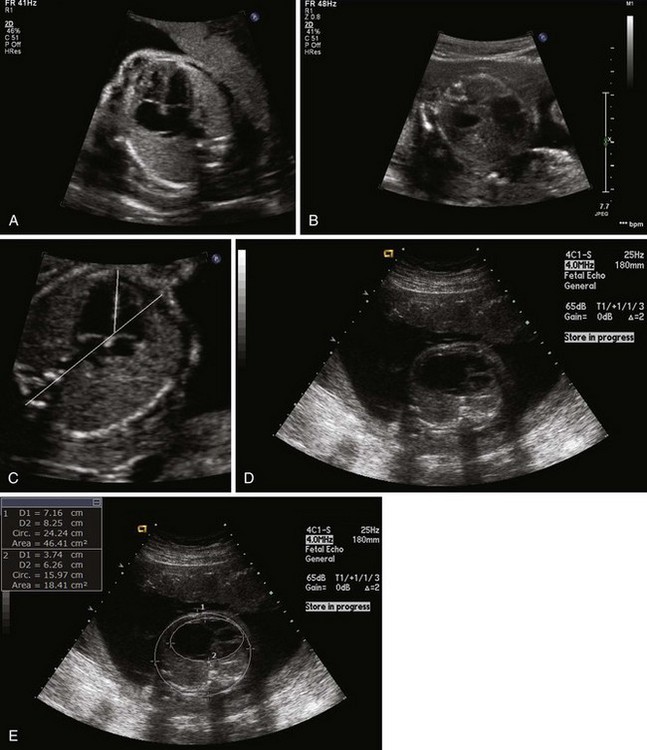
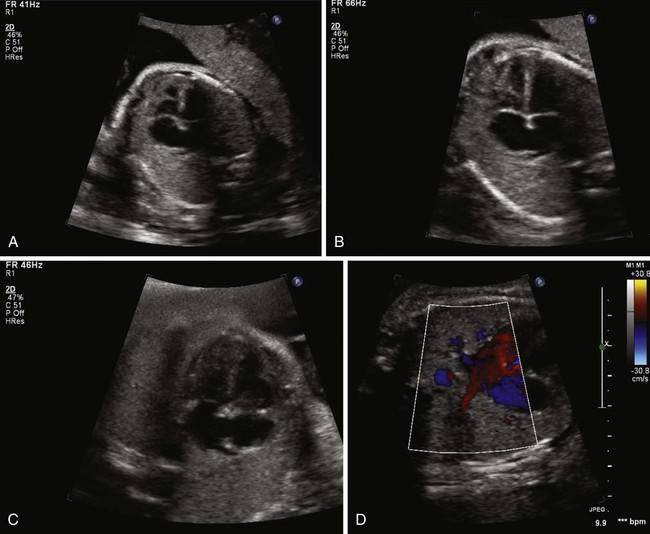
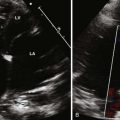
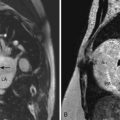
The 4C view is the most important in a comprehensive examination of the fetal heart (Fig. 2-2A). The image is obtained in a transverse scanning plane (cross section). Once an acceptable image is obtained, cardiac position, axis, and size are assessed. Cardiac position can be influenced by the presence of extracardiac abnormalities that displace the heart within the thorax. Examples include congenital cystic adenomatoid malformations, diaphragmatic hernia (see Fig. 2-2B), and intrathoracic pulmonary sequestration. Normal cardiac axis can be confirmed by visually drawing a line from the spine to the sternum. The interventricular septum intersects that line at an approximately 45-degree angle (see Fig. 2-2C). Axis deviation can be seen in a variety of congenital heart lesions such as Ebstein’s anomaly of the TV (see Fig. 2-2D). Normally the fetal heart occupies about one third of the thorax. If there is any doubt on visual inspection, the circumference of each can be measured and compared (the cardiac-to-thoracic ratio). A normal cardiac-to-thoracic ratio is 0.55 ± 0.05 (see Fig. 2-2E).
The Outflow Tracts
Aortic and Ductal Arches
Systemic and Pulmonary Venous Return
Doppler Evaluation
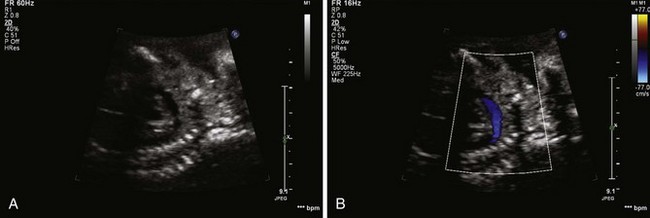
Color Doppler
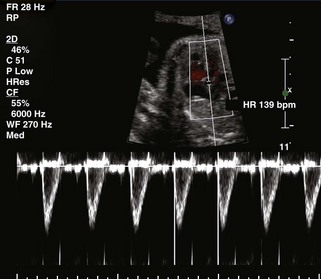
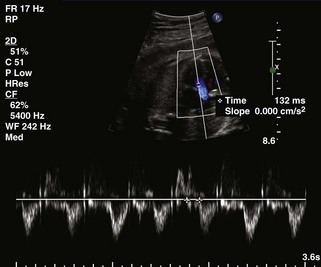
PW Doppler
Function
Rate and Rhythm Assessment
1 Friedberg M, Silverman N, Hornberger L, et al. Prenatal detection of congenital heart disease. J Pediatr. 2009;155:26-31.
2 Wimalasundera RC, Gardiner HM. Congenital heart disease and aneuploidy. Prenat Diagn. 2004;24:1116-1122.
3 Pajkrt E, Chitty LS. Fetal cardiac anomalies and genetic syndromes. Prenat Diagn. 2004;24:1104-1115.
Fetal Circulation and Neonatal Transition
1 Rychik J. Fetal cardiovascular physiology. Pediatr Cardiol. 2004;25:201-209.
1 Yagel S, Cohen SM, Achiron R. Examination of the fetal heart by five short-axis views: a proposed screening method for comprehensive cardiac evaluation. Ultrasound Obstet Gynecol. 2001;17:367-369.
2 Allan LD, Paladini D. Prenatal measurement of cardiothoracic ratio in evaluation of heart disease. Arch Dis Child. 1990;65:20-23.
3 Schneider C, McCrindle BW, Carvalho JS, Hornberger LK, et al. Development of Z-scores for fetal cardiac dimensions from echocardiography. Ultrasound Obstet Gynecol. 2005;26:599-605.
4 Al-Ghazali W, Chapman MG, Allan JG. Doppler assessment of the cardiac and uteroplacental circulations in normal and abnormal fetuses. Br J Obstet Gynaecol. 1988;95:575-580.
5 Api O, Carvalho J. Fetal dysrhythmias. Best Pract Res Clin Obstet Gynaecol. 2008;22:31-48.
Recent review of fetal dysrhythmias and their management.
6 Pasquini L, Gardiner HM. PR Interval: A comparison of electrical and mechanical methods in the fetus. Early Hum Dev. 2007;83:231-237.
7 Huhta J. Fetal congestive heart failure. Semin Fetal Neonatal Med. 2005;10:542-552.