CHAPTER 25 The Failed Uni
 Despite advances in prosthetic component design, newly developed instrumentation and surgical technique, and appropriate patient selection, failure after unicompartmental knee arthroplasty can occur. As the number of unicompartmental knee arthroplasties performed continues to rise, so too will the number of failures.
Despite advances in prosthetic component design, newly developed instrumentation and surgical technique, and appropriate patient selection, failure after unicompartmental knee arthroplasty can occur. As the number of unicompartmental knee arthroplasties performed continues to rise, so too will the number of failures. The current recommendation for management of the failed unicompartmental arthroplasty is conversion to total knee arthroplasty. In the majority of cases, the conversion of unicondylar arthroplasty to total knee arthroplasty can successfully be performed with the same approach used in primary total knee arthroplasty.
The current recommendation for management of the failed unicompartmental arthroplasty is conversion to total knee arthroplasty. In the majority of cases, the conversion of unicondylar arthroplasty to total knee arthroplasty can successfully be performed with the same approach used in primary total knee arthroplasty. Failure mode can be predictive of complexity of the conversion of unicompartmental arthroplasty to total knee arthroplasty. Failure modes have included polyethylene wear, progression of arthritis, patellofemoral symptoms, aseptic loosening, malpositioned implants, medial tibial collapse, poor patient selection, and technical factors.
Failure mode can be predictive of complexity of the conversion of unicompartmental arthroplasty to total knee arthroplasty. Failure modes have included polyethylene wear, progression of arthritis, patellofemoral symptoms, aseptic loosening, malpositioned implants, medial tibial collapse, poor patient selection, and technical factors. Polyethylene wear, with or without loosening, and progressive arthritis have been the most common failure modes reported with contemporary unicompartmental knee arthroplasty designs. When unicompartmental knees fail through these modes, the revision procedures are straightforward with minimal bone loss.
Polyethylene wear, with or without loosening, and progressive arthritis have been the most common failure modes reported with contemporary unicompartmental knee arthroplasty designs. When unicompartmental knees fail through these modes, the revision procedures are straightforward with minimal bone loss. When failure occurs in unicompartmental knee arthroplasty due to early collapse of the medial tibial plateau, there are more significant bone defects, and revisions are technically more demanding than that seen with other aseptic failure mechanisms such as polyethylene wear.
When failure occurs in unicompartmental knee arthroplasty due to early collapse of the medial tibial plateau, there are more significant bone defects, and revisions are technically more demanding than that seen with other aseptic failure mechanisms such as polyethylene wear. Early failure is typically related to inappropriate patient selection, infection, medial tibial collapse, or poor surgical technique leading to ligament instability, malpositioning of the implant, or component loosening. The more common modes of failure include polyethylene wear, progression of tricompartmental arthritis, or component loosening, and will occur late after the first or second decade.
Early failure is typically related to inappropriate patient selection, infection, medial tibial collapse, or poor surgical technique leading to ligament instability, malpositioning of the implant, or component loosening. The more common modes of failure include polyethylene wear, progression of tricompartmental arthritis, or component loosening, and will occur late after the first or second decade. In general, late failures are less demanding and can usually be converted using a cruciate-retained or posterior-stabilized primary total knee arthroplasty, without supplemental stabilization or constraint.
In general, late failures are less demanding and can usually be converted using a cruciate-retained or posterior-stabilized primary total knee arthroplasty, without supplemental stabilization or constraint. The surgical approach follows the same principles of primary total knee arthroplasty using standard primary total knee arthroplasty instrumentation. One of the most important technical aspects of the procedure is to leave the unicompartmental arthroplasty implants intact as long as possible.
The surgical approach follows the same principles of primary total knee arthroplasty using standard primary total knee arthroplasty instrumentation. One of the most important technical aspects of the procedure is to leave the unicompartmental arthroplasty implants intact as long as possible.Introduction
The popularity of unicompartmental knee arthroplasty has continued to grow over the last decade and is one of the main treatment alternatives for isolated degenerative arthritis of the knee.1–3 Since its introduction, unicondylar arthroplasty has been an alternative to total knee arthroplasty or high tibial osteotomy for the treatment of unicompartmental knee arthritis. The benefits of this procedure are attributed to the ability to provide a more rapid rehabilitation time, greater range of motion, preservation of bone stock, and more normal knee kinematics with the retention of both the anterior and posterior cruciate ligaments. With improvements in component design, surgical technique, and patient selection criteria, improved clinical outcomes have been reported in the literature. Berger et al. reported on a prospective study of 62 unicompartmental knee arthroplasties with a mean follow-up of 12 years.3 They noted no loose components or periprosthetic osteolysis, with a 10-year survival rate of 98%. Price et al. also noted a 93% 10-year survival using the Oxford unicompartmental knee implant.4 Because of these encouraging results, the prevalence of unicompartmental knee arthroplasty has increased significantly over the years. Between 1996 and 1997, unicondylar knee arthroplasty comprised only 1% of the U.S. total knee market.5 This increased to 6% of all total knees performed in the United States between 2000 and 2001. Between 1998 and 2005, there has been a 10% per year increase in the number of unicompartmental knee arthroplasty procedures performed in the United States alone.6 This growth rate is approximately three times that for total knee arthroplasty, and presently it is estimated that 12% of all total knees performed in the United States are unicompartmental knee arthroplasties.
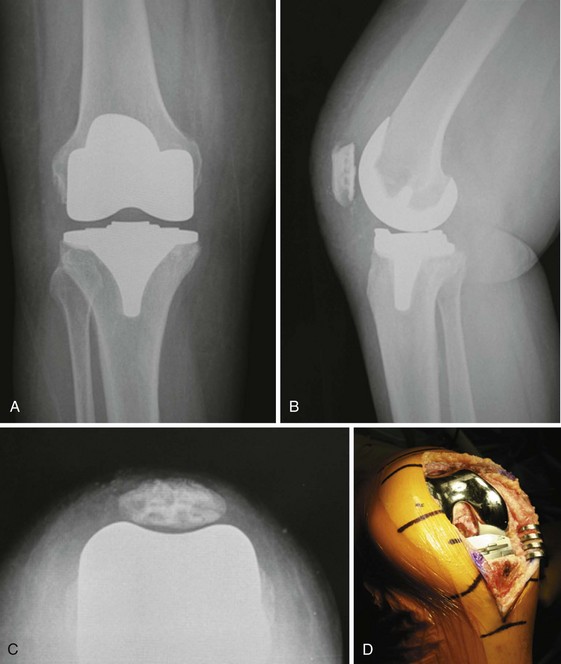
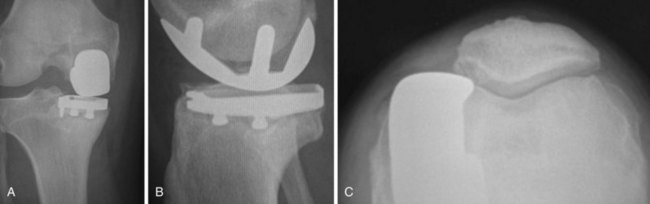
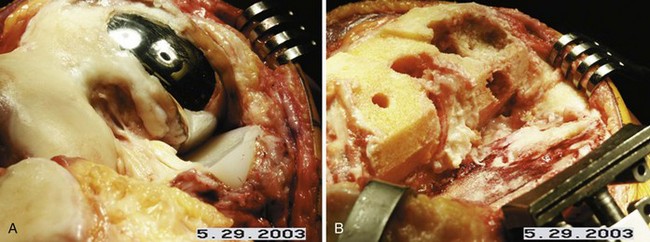
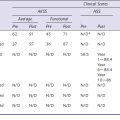
Although early midterm studies cite a high rate of satisfactory results after unicompartmental knee arthroplasty, long-term survivorship and outcome continue to be a concern. Long-term survivorship of unicompartmental knee arthroplasty has been improving with the advancement in prosthetic component design, newly developed instrumentation and surgical technique, and appropriate patient selection. Despite advances, failure after unicompartmental knee arthroplasty can occur. When compared with total knee arthroplasty as an index arthroplasty procedure, however, the cumulative revision rate for unicompartmental knee arthroplasty tends to be higher.7,8 Gioe et al. evaluated more than 5000 total knee arthroplasties in a community registry and noted that unicondylar arthroplasty was 7.2 times as likely to fail compared to an all-polyethylene cemented total knee arthroplasty.9 The Norwegian Arthroplasty Registry echoed some of these same concerns, noting two times the revision rate with unicompartmental arthroplasty versus total knee arthroplasty in their evaluation of more than 2200 unicondylar knees.10 In the Swedish Registry, Lindgren et al. found a greater than 10% cumulative revision rate at 10 years for unicondylar arthroplasty, with only a 5% cumulative revision rate for total knee arthroplasty.11 In the Australian Registry, results were equally concerning with their 5-year revision rate of 8.9%.12 As the number of unicompartmental knee arthroplasties performed continues to rise, so too will the number of failures. Early investigations reported technical difficulty during conversion of unicompartmental knee arthroplasty to total knee arthroplasty, citing substantial bone loss requiring bone grafting, stemmed revision components, or the need for custom implants.8,13 More recently, with improvement in surgical technique and prosthetic designs, conversion of unicompartmental knee arthroplasty to total knee arthroplasty has been described as less technically demanding than a revision total knee arthroplasty with results comparable to the results of primary total knee arthroplasty, in terms of both function and survivorship14 (Figs. 25–1 and 25–2).
Clinical Evaluation and Preoperative Planning
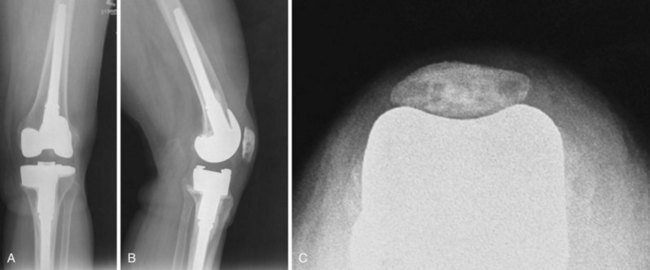
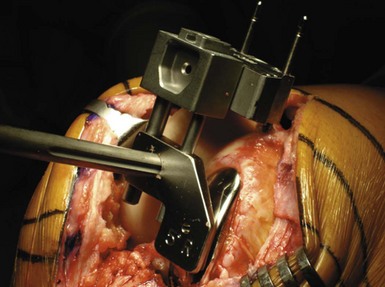
The current recommendation for management of the failed unicompartmental arthroplasty is conversion to total knee arthroplasty.15 In the majority of cases, the conversion of unicondylar arthroplasty to total knee arthroplasty can successfully be performed with the same approach used in primary total knee arthroplasty. Primary total knee arthroplasty components and instrumentaion can be used. In most cases, however, it is essential to be prepared for any technical difficulties that may arise requiring stem fixation, metal augments, bone grafting, or a more constrained component (Figs. 25–3 and 25–4). Preoperative evaluation is critical in the planning process. Berend et al. have shown that the mode of failure is predictive in determining complexity of conversion and can assist in the planning for special instrumentation, or more complex reconstructive options.15
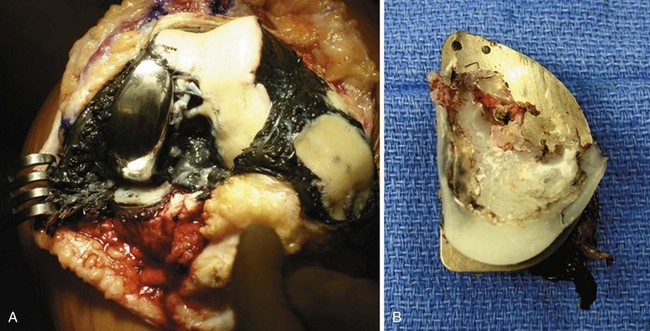
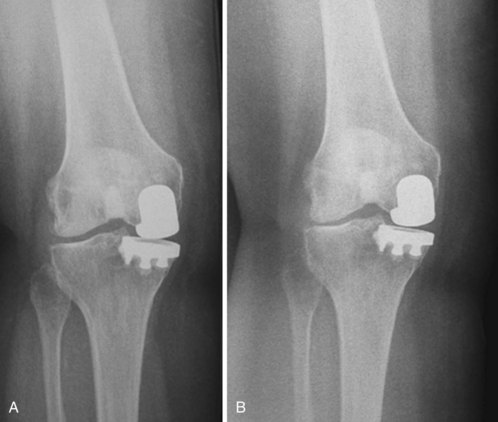
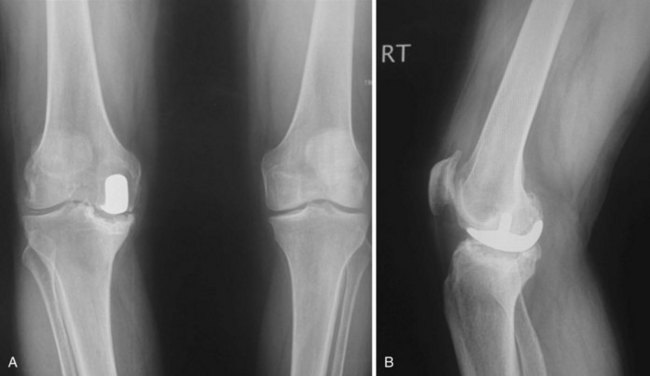
Factors leading to unicompartmental knee arthroplasty failure have been shown to differ based on whether failure has occurred early or late. Early failure is typically related to inappropriate patient selection, infection, medial tibial collapse, or poor surgical technique leading to ligament instability, malpositioning of the implant, or component loosening. The more common modes of failure include polyethylene wear, progression of tricompartmental arthritis, or component loosening, and will occur late after the first or second decade16 (Fig. 25–5). In general, late failures are less demanding and can usually be converted using a cruciate-retained or posterior-stabilized primary total knee arthroplasty, without supplemental stabilization or constraint.17 If failure occurs secondary to medial tibial collapse or excessive resection of tibial bone, a more complex reconstruction will typically be required. Aleto et al., in a retrospective review of 32 knees converted to total knee arthroplasty, found that the most common mode of failure was related to medial tibial collapse (47% of the study group)16 (see Fig. 25–1). Of these, 87% were an all-polyethylene design, and 7 of 15 failed in less than 16 months and required a more complex reconstruction with stems, augments, and screws. In addition, they also found tibial component slope to be associated with the direction of the collapse of the implant into the tibia. Excessive posterior tibial component slope, with a mean of 12.0°, was associated with posterior failure. When failure mode is related to medial tibial collapse, more significant bone loss can be expected, and most likely will require a more complex reconstruction (Fig. 25–6).
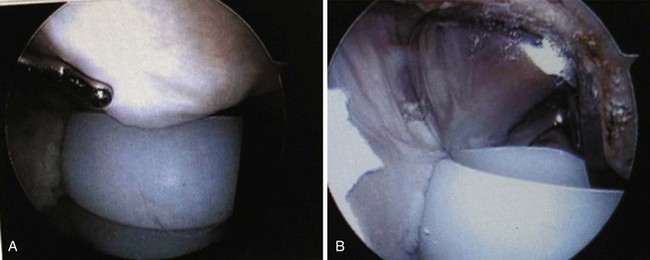
A thorough evaluation prior to surgery should be undertaken with all patients to accurately determine the cause of failure. This should include a detailed history, physical examination, radiographic evaluation, knee fluid analysis, and appropriate laboratory assessment. As in all knee arthroplasty patients, with any type of failure, it is important to consider septic arthritis until proven otherwise. Initial screening methods should be performed as in total knee arthroplasty with joint fluid analysis, including cell count, culture and sensitivity, Gram stain, and assessment for crystals. Peripheral blood evaluation should also be performed, including complete blood count, erythrocyte sedimentation rate, and C-reactive protein, as well as bone scan and sulfur colloid technetium bone scanning if indicated. A detailed physical examination should also be conducted to rule out elements of instability, with particular reference to the anterior cruciate ligament as well as the collateral ligaments. Injury or deficiency of the anterior cruciate ligament or medial collateral ligament can compromise function of the knee in the setting of unicompartmental knee arthroplasty. Lateral joint line tenderness with associated joint effusion may indicate meniscal pathology involving the opposite compartment and sometimes can be addressed with arthroscopic methods alone. Similarly, intra-articular scarring may cause impingement within the joint space, which can contribute to persistent postoperative pain and many times can be treated successfully with knee arthroscopy (Fig. 25–7).
It is important to note that the diagnosis of meniscal pathology, or intra-articular scarring, is based on history and clinical examination alone. It is therefore essential to first rule out all other causes for persistent pain and failure of unicompartmental arthroplasty. Standing weight-bearing radiographs are essential for evaluation of the femoral tibial joint space, which should include a standing bilateral anteroposterior view, a 45° flexion posteroanterior weight-bearing view, and lateral and skyline views. A long-leg standing weight-bearing (1.37 cm) axial alignment radiograph is also necessary to further evaluate the anatomic and mechanical axis of the knee (Fig. 25–8). Any progressive change of alignment may be an indication of medial tibial collapse, or possible progressive degeneration of the opposite compartment. Radiographic evaluation is also important in order to determine any evidence of radiolucent lines or concerns for component loosening or wear of polyethylene (Fig. 25–9). Serial comparison of radiographs over time is extremely helpful as changes in alignment, collapse of the tibia, or progression of arthritis can occur gradually, and sometimes can only be appreciated with prior comparison views (Fig. 25–10). Assessment of bone loss, on either the femoral or tibial side, is also important in planning the need for a more complex reconstruction requiring metal augments, stems, or a more constrained revision component. Templating the level of resection on radiographs can help in this planning process to more accurately predict the need for augmentation.
Setup and Technique
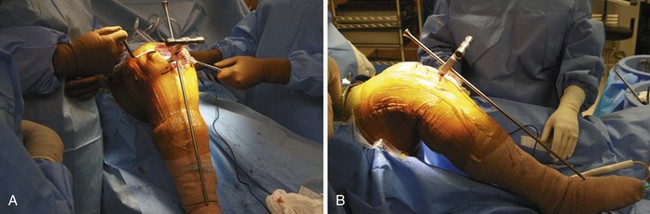
After confirmation of the preoperative plan, examination under anesthesia should be performed first. This will allow for further assessment of passive range of motion and collateral ligament stability, as well as the integrity of the anterior and posterior cruciate ligaments. The procedure is approached in a manner similar to that of primary total knee arthroplasty utilizing general or regional anesthesia. A short-acting spinal anesthetic with light sedation is preferable, as this will allow for a more successful approach with pain management. This has also been very beneficial in initiating early weight bearing and recovery of quadriceps muscle function within hours after the procedure. After induction of anesthesia, the patient is positioned in the supine position, with a small bolster placed at the foot of the bed to allow for knee flexion between 70° and 90° (Fig. 25–11). A specific leg holder is not necessary, and many times can cause further constraints of the tibia, affecting internal and external rotation during the surgical procedure.
Resection of the patella can be performed first in order to facilitate the exposure to the distal femur. This will also avoid eversion of the patella, which will minimize the soft tissue trauma to the extensor mechanism. Patellar resection is performed using the same principles followed in total knee arthroplasty with a measured resection approach. Using a towel clip, the patella can be easily everted and stabilized for preparation (Fig. 25–12). Removing the surrounding synovial tissue from the periphery of the patella is helpful in accurately identifying the level of resection. Once the periphery of the patella is cleared of synovial tissue to define its margins, a measured resection can be performed. It is important to restore the native patellar thickness to avoid overstuffing the patellofemoral joint, which can affect patellar articulation, patellar tracking, and range of motion. The patella should be measured using calipers in all four quadrants in order to retain the normal patellar height in the most accurate manner, and to avoid an oblique level of resection (Fig. 25–13). Transverse patellar osteotomy can be performed utilizing a freehand method or instrument method, depending on the surgeon’s preference (Fig. 25–14). The resection level should be parallel, and once again, assessment should be made with the caliper in all four quadrants to avoid the risk of an oblique cut, and any abnormality with patellar tracking (Fig. 25–15). Sizing of the patella can then be performed in the usual manner, taking care to medialize the patella to prevent any overhang beyond the margins of the bone (Fig. 25–16). The thickness of the patella should then be reassessed following insertion of the prosthetic component trial. Ideally the goal is to have the thickness of the remaining patella and the patellar prosthesis equal to the appropriate patellar thickness.
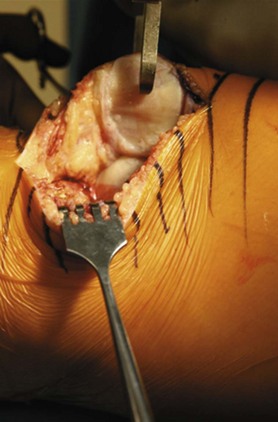
Figure 25–13 Patellar thickness is measured with the caliper, with assessment of both the medial and lateral facets.
Once the patella has been appropriately prepared, it can be easily displaced into the lateral gutter, thereby avoiding eversion of the patella with much less surgical trauma or injury to the quadriceps extensor mechanism. A custom-designed patellar retractor has been developed to facilitate the retraction of the patella, as well as protect the resected surface throughout the procedure (Fig. 25–17). The knee is then flexed and held in a position between 70° and 90° of flexion to provide excellent exposure of the distal femur and proximal tibia. It is important to note that hyperflexion should be avoided as this can cause greater difficulties with exposure of the distal femur due to the increased tension that is applied across the extensor mechanism the further the knee is flexed. If a modular tibial component is present, then removal of the tibial polyethylene component should be performed first. This will facilitate exposure and preparation of the distal femur. If an all-polyethylene tibial component is present, then removal should be delayed until after resection of the distal femur. Removal of an all-polyethylene tibial component can be achieved more easily and more accurately once the distal femoral resection is complete (Fig. 25–18).
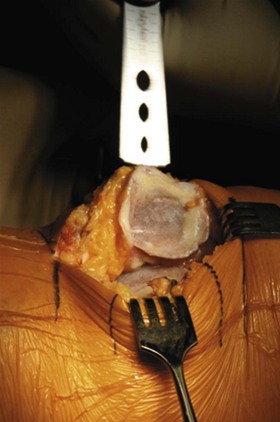
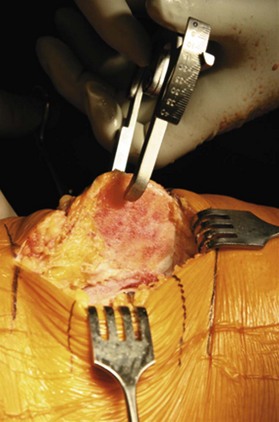
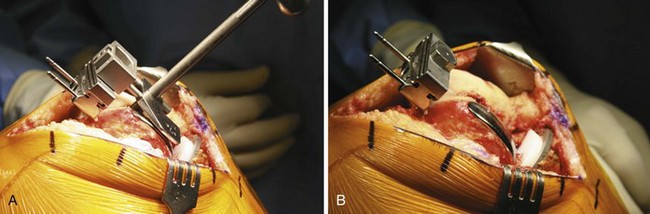
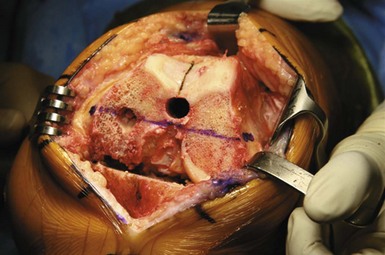
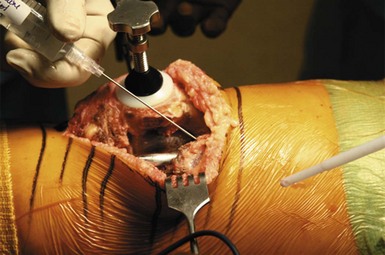
Distal femoral resection is performed next. It is extremely important to leave the femoral component intact on the distal femur. This is a critical step, and will allow for more accurate assessment of the joint line for preparation of the distal femur. With the femoral component intact, the intramedullary canal can be entered for insertion of the distal resection guide, referencing off of the medial femoral condyle with the existing component in place (Fig. 25–19). Reference should also be made to the resection level of the lateral compartment with an angel wing to further verify the appropriate level of distal femoral resection. With the distal resection guide in place, and the femoral component left intact, the majority of the distal resection can be performed. A small ( -inch) osteotome can be used next to carefully, and meticulously, disrupt the bone-cement interface of the femoral component. It is extremely important to address the entire periphery of the prosthesis as well as the posterior condylar area in order to minimize any significant bone loss during implant removal (Fig. 25–20). Once the femoral component has been removed, the distal resection of the femur can be completed in the usual manner (Fig. 25–21). Frequently this will create a resection level with minimal or no deficiencies of bone in the distal femoral condyle. Bone loss in the distal femoral condyle can usually be addressed with simple bone grafting techniques. Loss of bone in the posterior condyle of the femur is common, but rarely will require bone grafting or augmentation.
-inch) osteotome can be used next to carefully, and meticulously, disrupt the bone-cement interface of the femoral component. It is extremely important to address the entire periphery of the prosthesis as well as the posterior condylar area in order to minimize any significant bone loss during implant removal (Fig. 25–20). Once the femoral component has been removed, the distal resection of the femur can be completed in the usual manner (Fig. 25–21). Frequently this will create a resection level with minimal or no deficiencies of bone in the distal femoral condyle. Bone loss in the distal femoral condyle can usually be addressed with simple bone grafting techniques. Loss of bone in the posterior condyle of the femur is common, but rarely will require bone grafting or augmentation.
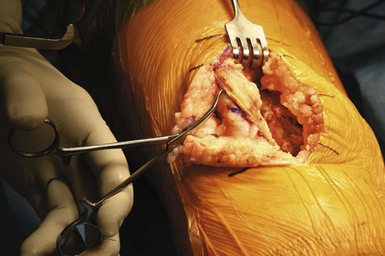
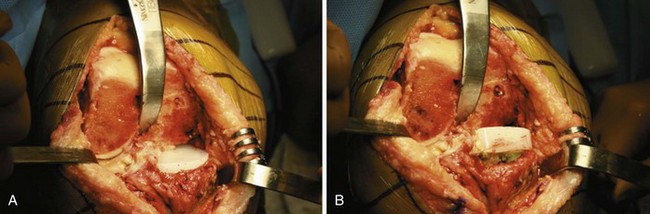
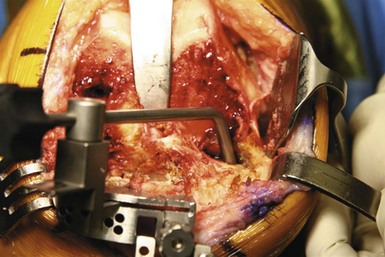
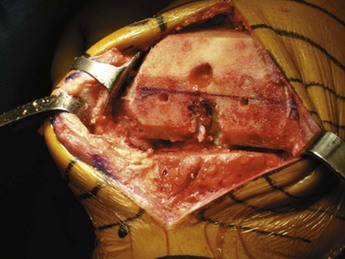
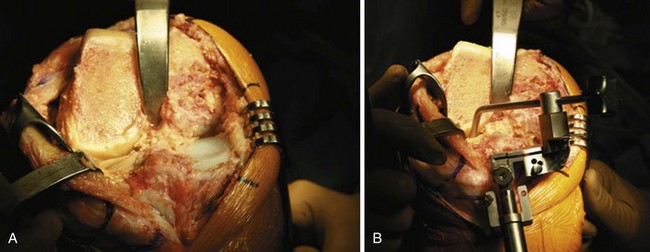
Once the distal femoral resection is complete, exposure of the proximal tibia is significantly easier to achieve. If the anterior cruciate ligament is still intact, this should be incised first to facilitate anterior displacement of the proximal tibia and improve exposure. A Hohmann retractor carefully placed into the intercondylar notch on the posterior tibia will provide excellent exposure of the proximal tibia. A Z retractor is placed behind the patellar tendon at the level of the joint line in order to protect the tendon and to further displace the patella into the lateral gutter and improve exposure (Fig. 25–22). A Hohmann retractor placed at the midlevel of the lateral tibial plateau may also be necessary for adequate exposure depending on the anatomy. Attention can now be directed toward removal of the tibial component. Once again, careful and meticulous disruption of the cement-mantle interface is critical in order to minimize any significant bone loss. A reciprocating saw should be used first to disrupt the bone-cement interface, followed by the use of a small osteotome. As with the femoral component removal, it is very important to carefully disrupt the bone-cement interface around the entire periphery of the prosthesis, with particular attention to the posterior aspect of the tibial component to avoid loss of bone in this area. Removal of an all-polyethylene tibial component can be easily accomplished using an oscillating saw to disrupt the cement-implant interface first. The polyethylene pegs and retained cement can be addressed in the final preparation of the tibia.
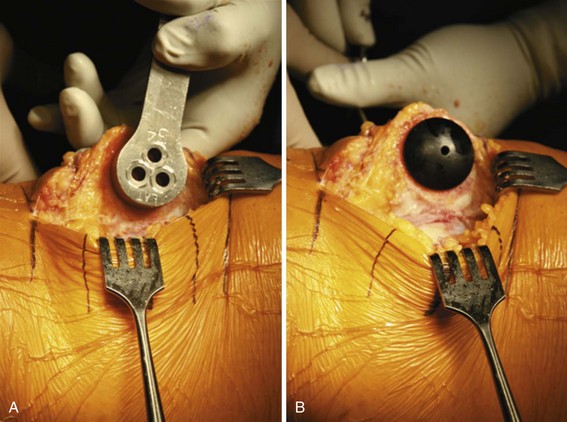
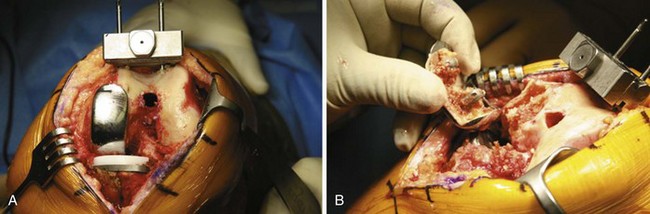
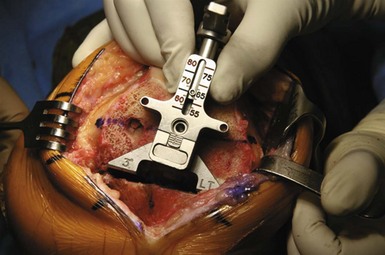
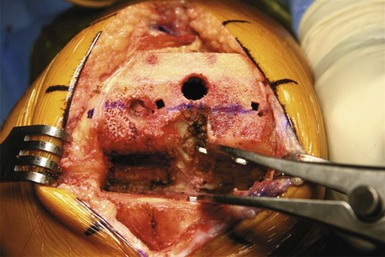
Once the tibial component is removed, the tibial resection guide can be positioned using the same reference points used in primary total knee arthroplasty. Depth of tibial resection will be the more critical assessment to be made at this time. Reference should be made off the intact lateral bone, which will allow for the most conservative resection of bone (Fig. 25–23). Appropriate slope, as well as varus-valgus alignment, should also be verified. It is extremely important not to reference the deficient area of bone, as this will frequently cause over-resection of the proximal tibia. After the resection of the proximal tibia is complete, assessment of any medial bone deficiency can now be evaluated more accurately. If the defect is less than 6 mm and is contained, then bone grafting or screws and cement can be used successfully to restore the level of the medial compartment to the level of the lateral compartment resection. However, if there is a deficiency of 6 mm or greater, then medial augmentation with stem preparation should be carried out at this time (Fig. 25–24).
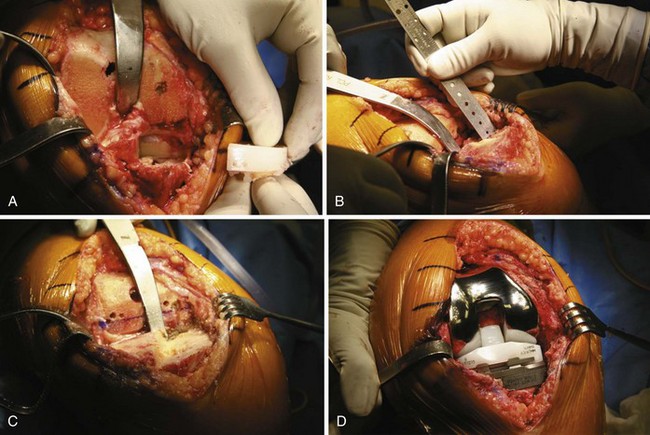
Figure 25–24 (A) Intra-operative view after removal of an all-polyethylene tibial component with a significant medial defect.
(C) The tibia has been prepared for a medial augment and the appropriate stem fixation.
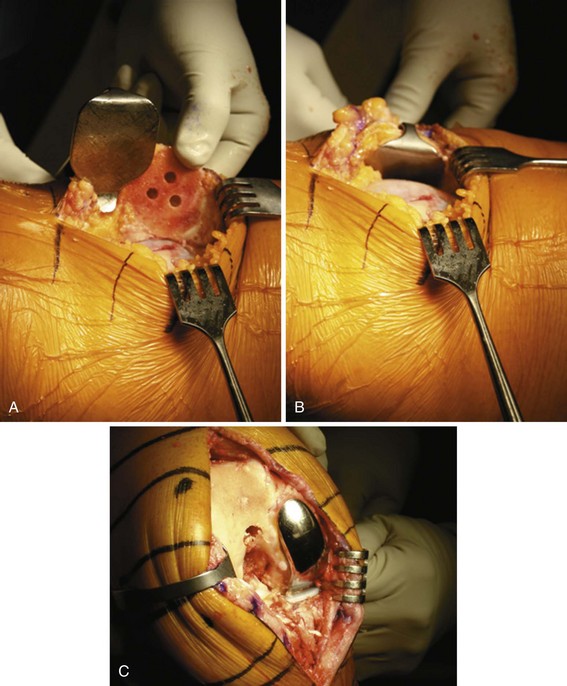
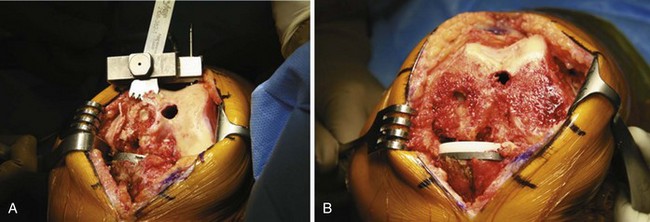
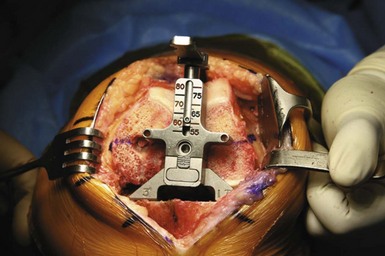
With the tibial resection completed, attention can be redirected toward the final preparation of the distal femur. It is essential at this time to identify and mark both Whiteside’s line and the transepicondylar axis. When converting a medial unicondylar arthroplasty, bone loss from the posteromedial femoral condyle is not uncommon and will cause posterior condylar referencing for rotational alignment and sizing to be unreliable (Fig. 25–25). Excess external rotation of the femoral component will occur if these reference points are not identified (Fig. 25–26). The femoral sizing and rotation guide can now be easily applied and accurately positioned utilizing these two reference points. With the guide positioned in appropriate external rotation, two reference drill holes can be made for accurate placement of the 4-in-1 guide (Figs. 25–27 and 25–28). Once the femoral resection is complete, the medial posterior femoral condyle can be evaluated for bone loss, and the need for augmentation can be determined. Once again, because of improved component designs, posterior augmentation of the femur is rarely required (Fig. 25–29).

Figure 25–28 The 4-in-1 femoral resection guide can be positioned accurately for final preparation of the femur.
With the completion of all bone cuts, both on the femur and tibia, ligament balance as well as flexion-extension gap balance can be evaluated. Spacer block technique should then be performed, and is a critical step to verify that appropriate mechanical alignment has been restored, as well as appropriate balance and stability of the flexion and extension space (Fig. 25–30). Using a laminar spreader, with the knee flexed at 90°, the posterior compartment can be evaluated for any debris, meniscal remnants, or residual posterior osteophytes (Fig. 25–31). Trial reduction is then performed, assessing appropriate stability, range of motion, and the integrity of the posterior cruciate ligament. If there is deficiency of the posterior cruciate ligament, then a more constrained posterior-stabilized component can be utilized. Patellar tracking should be assessed utilizing a “no-thumbs technique” to assure that there is no lateral subluxation or dislocation that occurs throughout range of motion. Patellar malalignment or maltracking should be addressed, which should include a reevaluation of femoral component rotational alignment. This should be performed before routinely performing a lateral retinacular release. The final evaluation should show central tracking of the patella, with full extension of the limb, and appropriate stability and balance of the posterior cruciate ligament in both extension and flexion. In addition, there should be appropriate stability with anterior and posterior drawer testing.
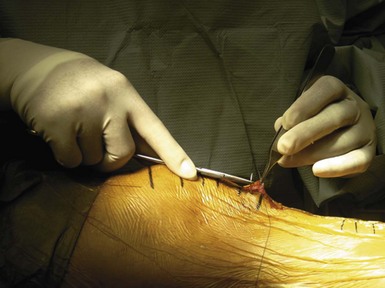
Preparation is then performed in the usual manner utilizing appropriate cement technique. The affected bone surfaces are prepared with a jet lavage system to accurately remove any blood and debris for cementation. Cement is applied first to the tibial surface with digital pressurization in order to achieve an appropriate bone-cement mantle, as well as to the undersurface of the tibial component.18 Following application of the tibial tray, the femoral component is then cemented. Cement is applied to all surfaces with the exception of the posterior condylar surface to avoid the introduction of excess cement into the posterior compartment.19 Cement is applied to all surfaces of the backside of the femoral component, including the posterior condylar surface. Following insertion and cement clearing of the femoral component, the tibial bearing surface is then applied and the knee is reduced and placed in full extension. The patellar component is then cemented last and pressurized with a clamp. The deep capsular tissues medially and laterally are injected with a “pain cocktail,” as is the subcutaneous layer, prior to closure20 (Fig. 25–32). The deep capsule is closed with an absorbable suture. Skin closure is accomplished with 4-0 absorbable running subcutaneous suture closure (Fig. 25–33). This can avoid the irritation and wound complications that have been identified with the use of staples.
Special Considerations
Retaining the femoral component for preparation of the distal femur is a critical step (Fig. 25–36). This will allow for more accurate restoration of the joint line and also avoid overresection of the distal femur. Attention to femoral rotation is also critical. Identifying the transepicondylar axis and longitudinal axis (Whiteside’s line) should be performed in all cases (see Figs. 25-24 and 25-35). The deficiency of the posteromedial femoral condyle (posterolateral for lateral unicompartmental knee arthroplasty) will create excess external rotation (or internal rotation for lateral unicompartmental knee arthroplasty) in preparing the femur if not recognized (see Fig. 25–26). The most conservative tibial resection should be performed initially, with an assessment of flexion and extension gap in order to help determine the need for a medial (or lateral) augment. Spacer block technique, which can allow for the assessment of ligament balance as well as alignment and stability, has also been helpful (see Figs. 25-30 and 25-31). The use of a cruciate-retained or a posterior-stabilized prosthetic component can be determined at the time of surgery, depending on the integrity of the posterior cruciate ligament. Success has been reported with both types of components.14 With attention to detail and a stepwise approach to the technical aspects of the surgical procedure, high clinical success can be achieved comparable to the success that has been achieved with primary total knee arthroplasty.
Postsurgical Follow-Up
Postoperative recovery is similar to that utilized for primary total knee arthroplasty. A preemptive multimodal approach to pain management is utilized in the early postoperative phase in order to restore quadriceps function and to prevent shutdown of the extensor mechanism. An intra-articular injection is performed at the time of surgery with a pain cocktail, which can significantly minimize pain in the early postoperative phase.20 Quadriceps isometric exercises, straight leg raises, and range-of-motion exercises are started on the day of surgery. Full weight bearing is permitted immediately, and patients are encouraged to begin weight bearing on the day of surgery with the use of crutches, walker, or a cane. Ketorolac (Toradol) 15 mg intravenously has been extremely helpful in controlling the inflammatory response when given preoperatively, in addition to every 6 hours for the first 24 hours in patients without allergy to nonsteroidal anti-inflammatories. It is important that physical therapy is not too aggressive in the early phase, as this will contribute to excessive soft tissue swelling and progressive limitation of motion, quadriceps muscle weakness, increased wound drainage, and possible wound healing complications. A continuous passive motion machine during hospitalization may be used at the surgeon’s discretion. Thromboembolism prophylaxis is used similar to total knee arthroplasty with coumadin (Warfarin) being utilized during the hospital stay. The majority of patients will continue with enteric-coated aspirin (325 mg, twice daily) for 4–6 weeks, unless there is an increased risk for thromboembolism or increased bleeding tendency where aspirin cannot be utilized. In these situations, coumadin is used for 2 weeks. Intravenous antibiotics are used for the first 24 hours in order to prevent infection. When quadriceps strength returns, patients are allowed to progress with unrestricted activities, with recommendation to avoid excessive loading and deep flexion, and high-impact activities.
Conclusion
In the past, conversion of unicompartmental knee arthroplasty to total knee arthroplasty has created some concerns for a more technically demanding procedure requiring a more complex reconstructive approach necessitating the use of bone grafting, augments, and stemmed revision components.21 With newer prosthetic designs and more conservative surgical techniques, the conversion of unicompartmental arthroplasty to total knee arthroplasty has improved significantly, with results that are comparable to the results of primary total knee arthroplasty. Johnson et al. reported on a series of 35 patients who had undergone conversion of unicompartmental knee replacement to total knee replacement with 91% survivorship at 10 years of follow-up.14 This study also demonstrated that the conversion of a unicompartmental knee arthroplasty to a total knee arthroplasty is a much less demanding procedure than revision total knee arthroplasty, with results comparable to those of primary total knee arthroplasty. Only 3 of the 35 cases in this series required a stem or augmentation device. Studies on clinical outcome comparing unicompartmental knee arthroplasty conversion to primary total knee arthroplasty are rare. Miller et al. found that unicompartmental knee arthroplasty patients had a higher complication rate with inferior clinical results compared to primary total knee arthroplasty patients.22 Jarvenpaa et al. noted that the knee scores were improved in patients who underwent conversion to a posterior cruciate ligament substituting design.23 Saragaglia et al. evaluated the radiologic and clinical results of medial unicompartmental arthroplasty converted to total knee arthroplasty.24 When comparing their results to the literature, they suggested that conversion of unicompartmental arthroplasty would give better results than revision total knee arthroplasty.
As previously reported, failure mode can be predictive of complexity of the conversion of unicompartmental knee arthroplasty to total knee arthroplasty.15 Failure modes have included polyethylene wear, progression of arthritis, patellofemoral symptoms, aseptic loosening, malpositioned implants, medial tibial collapse, poor patient selection, and technical factors. Of these, polyethylene wear, with or without loosening, and progressive arthritis have been the most common failure modes reported with contemporary unicompartmental knee arthroplasty designs. Both McAuley et al. and Levine et al. demonstrated that, when unicompartmental knees fail through these modes, the revision procedures are straightforward with minimal bone loss.25,26 In all cases, primary femoral components were used, and on the tibial side, the defects encountered were easily dealt with using autogenous nonstructural bone graft, augments, and stems, where indicated.16 Aleto et al. found that the more significant bony defects were encountered in knees that failed by medial tibial collapse, and required increased implant requirements as compared to other failure modes.16 In this review of 32 knees, 13 of the 15 required screws and cement and/or augments, and 10 of the 15 required stems on the tibial side. This suggests that, when failure occurs in unicompartmental knee arthroplasty due to early collapse of the medial tibial plateau, there are more significant bone defects, and revisions are technically more demanding than those seen with other aseptic failure mechanisms such as polyethylene wear. Furthermore, of the failures that occurred in this series as a result of medial tibial collapse, 87% of the 15 knees were of all-polyethylene design, which was highly significant compared to metal-backed components (Fig. 25–37). Using a three-dimensional finite element model to evaluate contact stresses, Morra and Greenwald found a strikingly different polyethylene loading pattern for fixed-bearing, all-polyethylene unicompartmental knee arthroplasty designs versus metal-backed designs.27 In particular, the fixed-bearing designs showed much higher contact stresses in the polyethylene, with highly localized contact points in the anterior and medial locations. Based on the clinical data, coupled with finite element analysis estimations, it can be concluded that an all-polyethylene, fixed-bearing, low-conformity unicompartmental knee arthroplasty would be most susceptible to excessive peripheral or localized edge loading resulting in cancellous bone overload and medial tibial collapse.16 Understanding these failure modes not only will help in the planning for conversion of the failed unicompartmental knee arthroplasty, but hopefully will also allow for improvements in understanding the technical factors required in achieving long-term clinical success. The ultimate goal in converting a unicompartmental knee arthroplasty to a total knee arthroplasty is to achieve the clinical result of a primary total knee arthroplasty, in terms of both function and survivorship.
Tips and Pearls
1 Kozinn SC, Marx C, Scott RD. Unicompartmental knee arthroplasty: a 4.5 to 6 year follow up study with a metal backed tibial component. J Arthroplasty. 1989;4(Suppl):S1-S9.
2 Cobb AG, Kozinn SC, Scott RD. Unicondylar or total knee replacement: the patient’s preference. J Bone Joint Surg [Br]. 1990;72:166.
3 Berger RA, Meneghine RM, Jacobs JJ, et al. Results of unicompartmental knee arthroplasty at a minimum of ten years of follow-up. J Bone Joint Surg [Am]. 2005;87:999-1006.
4 Price AJ, Waite JC, Svärd U, Long-term clinical results of the medial Oxford unicompartmental knee arthroplasty. Clin Orthop Relat Res, 435, 2005, 171-180.
5 U.S. Markets for Reconstructive Devices 2001. Toronto, Ontario, Canada: Millennium Research Group, 2002.
6 U.S. Markets for Reconstructive Devices 2002. Toronto, Ontario, Canada: Millennium Research Group, 2003.
7 Goie TJ, Killeen KK, Hoeffel DP, et al, Analysis of unicompartmental knee arthroplasty in a community-based implant registry. Clin Orthop Relat Res, 416, 2003, 111-119.
8 Dudley TE, Goie TJ, Sinner P, Mehle S, Registry outcomes of unicompartmental knee arthroplasty revisions. Clin Orthop Relat Res, 466, 2008, 1666-1670.
9 Goie TJ, Killeen KK, Grimm K, et al, Why are total knee replacements revised? Analysis of early revision in a community knee implant registry. Clin Orthop Relat Res, 428, 2004, 100-106.
10 Furnes O, Espehaug B, Lie SA, et al. Early failures among 7,174 primary total knee replacements: a follow-up study from the Norwegian Arthroplasty Register 1994–2000. Acta Orthop Scand. 2002;73:117-129.
11 Lidgren L, Knutson K, Robertsson O. Swedish Knee Arthroplasty Register: 2003 Annual Report. Lund: Swedish Knee Arthroplasty Register; 2003.
12 Australian Orthopaedic Association National Joint Registry. Annual Report. Adelaide, Australia: Australian Orthopaedic Association; 2007.
13 Bohm I, Landsiedl F. Revision surgery after failed unicompartmental knee arthroplasty: a study of 35 cases. J Arthroplasty. 2000;15:982-989.
14 Johnson S, Jones P, Newman JH. The survivorship and results of total knee replacements converted from unicompartmental knee replacements. Knee. 2007;14:154-157.
15 Berend K, George J, Lombardi A. Unicompartmental knee arthroplasty to total knee arthroplasty conversion: assuring a primary outcome. Orthopedics. 2009;32:684.
16 Aleto TJ, Berend ME, Ritter MA, et al. Early failure of unicompartmental knee arthroplasty leading to revision. J Arthroplasty. 2008;23:159-163.
17 Springer BD, Scott RD, Thornhill TS, Conversion of failed unicompartmental knee arthroplasty. Clin Orthop Relat Res, 446, 2006, 214-220.
18 Vanlommel J, Luyckx JP, Labey L, et al. Cementing the tibial component in total knee arthroplasty: which technique is the best? J Arthroplasty. 2010. April 7. [Epub ahead of print]
19 Vaninbroukx M, Labey L, Innocenti B, Bellemans J. Cementing the femoral component in total knee arthroplasty: which technique is the best? Knee. 2009;16:265-268.
20 Busch CA, Shore BJ, Bhandari R, et al. Efficacy of periarticular multimodal drug injection in total knee arthroplasty: a randomized trial. J Bone Joint Surg [Am]. 2006;88:949-963.
21 Padgett DE, Stern SH, Insall JN. Revision total knee arthroplasty for failed unicompartmental replacement. J Bone Joint Surg [Am]. 1991;73:186-190.
22 Miller M, Benjamin JB, Marson B, Hollstein S. The effect of implant constraint on results of conversion of unicompartmental knee arthroplasty to total knee arthroplasty. Orthopedics. 2002;25:1353-1357.
23 Jarvenpaa J, Kettunen J, Miettinen H, Kroger H. The clinical outcome of revision knee replacement after unicompartmental knee arthroplasty versus primary total knee arthroplasty: 8–17 years follow-up study of 49 patients. Presented at the International Orthopaedics (SICOT) meeting, 2009.
24 Saragaglia D, Estour G, Nener C, Colle PE. Revision of 33 unicompartmental knee prostheses using total knee arthroplasty: strategy and results. Int Orthop. 2009;33:969-974.
25 McAuley JP, Engh GA, Ammeen DJ, Revision of failed unicompartmental arthroplasty. Clin Orthop Relat Res, 392, 2001, 279-282.
26 Levine WN, Ozuna RM, Scott RD, et al. Conversion of failed modern unicompartmental arthroplasty to total knee arthroplasty. J Arthroplasty. 1996;11:797.
27 Morra EA, Greenwald AS. The effects of walking gait on UHMWPE damage in unicompartmental knee systems: a finite element study. Presented at the Annual Meeting of the American Academy of Orthopedic Surgeons, 2003.
Ansari S, Newman JH, Ackroyd CE. 10 year survivorship analysis of medial sled arthroplasty. Acta Orthop Scand. 1997;68:430-434.
Barrett WP, Scott RD. Revision of failed unicondylar unicompartmental knee arthroplasty. J Bone Joint Surg [Am]. 1987;69:1328.
Cartier P, Cheaib S. Unicondylar knee arthroplasty: 2–10 years of follow-up evaluation. J Arthroplasty. 1987;2:157-162.
Chakrabarty G, Newman JH, Ackroyd CE. Revision of unicompartmental arthroplasty: clinical and technical considerations. J Arthroplasty. 1998;13:191-196.
Fehring TK, Odum SM, Masonis JL, Springer BD. Early failures in unicondylar arthroplasty. Orthopedics. 2010;33:11.
Knutson K, Lindstrand A, Lidgren L. Survival of knee arthroplasties: a nation-wide multicentre investigation of 8000 cases. J Bone Joint Surg [Br]. 1986;68:795.
Kozinn SC, Scott RD. Current concepts review: unicondylar knee arthroplasty. J Bone Joint Surg [Am]. 1989;71:145.
Lai C, Rand J, Revision of failed unicompartmental total knee arthroplasty. Clin Orthop Relat Res, 267, 1993, 193.
Laurencin CT, Zelicof SC, Scott RD, Ewald FC, Unicompartmental versus total knee arthroplasty in the same patient. Clin Orthop Relat Res, 273, 1991, 151-156.
Lewold S, Robertsson O, Knutson K, Lidgren L. Revision of unicompartmental knee arthroplasty: outcome in 1135 cases from the Swedish Knee Arthroplasty study. Acta Orthop Scand. 1998;69:469-474.
Mackinnon J, Young S, Bailey RAJ. The St. Georg sledge for unicompartmental replacement of the knee. J Bone Joint Surg [Br]. 1988;70:217.
Murray DW, Goodfellow JW, O’Connor JJ. The Oxford medial unicompartmental knee arthroplasty: a ten-year survival study. J Bone Joint Surg [Br]. 1998;80:983-989.
Newman JH, Ackroyd CE, Ahmed S. The early results of prospective randomised study of unicompartmental or total knee arthroplasty. J Bone Joint Surg [Br]. 76(Suppl 57), 1994.
Newman JH, Ackroyd CE, Shah NA. Unicompartmental or total knee replacement? Five year results of a prospective, randomised trial of 102 osteoarthritic knees with unicompartmental arthritis. J Bone Joint Surg [Br]. 1998;80:862-865.
Svärd UC, Price AJ. Oxford medial unicompartmental knee arthroplasty: a survival analysis of an independent series. J Bone Joint Surg [Br]. 2001;83:191-194.