The eyes and visual system
An examination of the eyes and the visual system can prove helpful in patients with no visual or ocular symptoms. This section will first describe examination of the eye generally, then examination of the pupils, visual function, acuity, visual fields and fundoscopy. Eye movements are discussed on pages 18–19.
Remember false eyes can be cosmetically effective – a pitfall in exams.
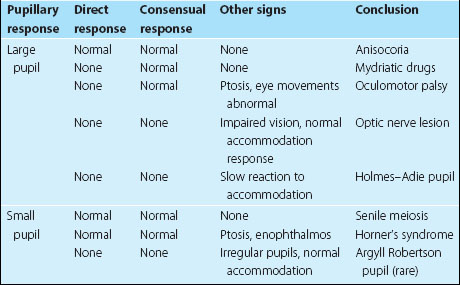
Examination of the pupils
Ask the patient to look into the distance and shine a light twice in each eye in turn. First, look at the response in the eye into which you are shining the torch (the direct response), and then at the response in the other eye (the consensual response). Then ask the patient to look at your finger held 15 cm from the patient’s face and look at the pupils for brisk constriction – the accommodation response. If no response is obtained from shining a light into the eye, but there is a normal response on accommodation, this is called an afferent pupillary defect and indicates significant optic nerve disease. Other abnormalities are summarized in Table 2.
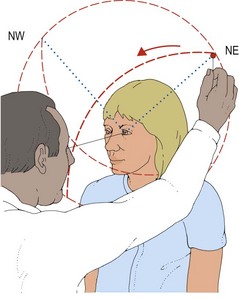
Examination of visual fields
The visual fields are examined by covering one of the patient’s eyes, asking the patient to fixate on your opposite eye and then bringing an object in from the periphery to find the edge of the patient’s vision (Fig. 1). This is done slightly differently depending on the type of object at which the patient is asked to look. The visual field for a large moving object is normally much larger than for a small red object. It is easiest to screen the visual fields using a crude stimulus, for example a wiggling finger, and then refine any defect with a smaller object, usually a small, red hat-pin head.
More detailed examination
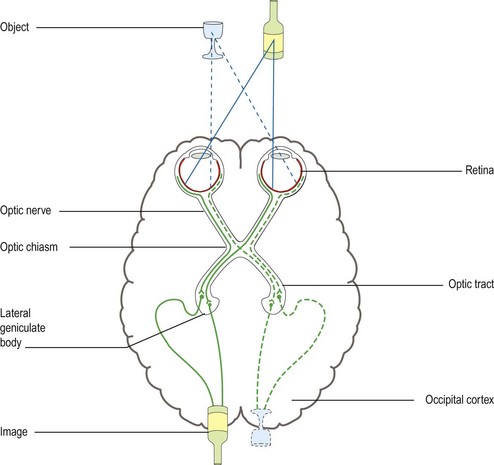
The location of a lesion producing a field defect can be deduced from the anatomy and organization of the visual system (Fig. 2; Table 3) (see p. 56).
| Site of lesion | Possible associations | |
|---|---|---|
| Unilateral visual field loss | Optic nerve or retina | Loss of pupillary responses, reduced acuity |
| Bitemporal hemianopia | Optic chiasm | Pituitary abnormalities, hypersecretion with or without hypopituitarism |
| Superior homonymous quadrantanopia | Temporal lobe | Hemisensory loss, mild hemianopia |
| Inferior homonymous quadrantanopia | Parietal lobe | Sensory agnosias (see p. 13) |
| Congruent homonymous hemianopia or quadrantanopia | Occipital lobe | Patients often have limited awareness of the defect |
| Incongruent homonymous hemianopia | Optic tract |
Occipital lobe lesions are associated with highly congruent fields.