2 The Eyelids
NORMAL ANATOMY
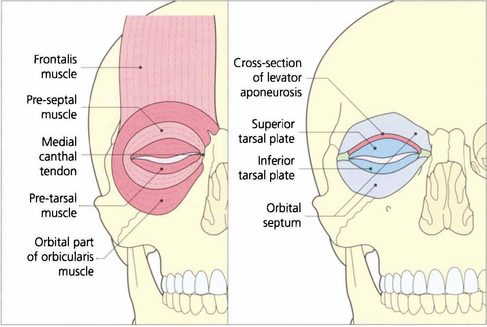
Fig. 2.1 Diagrammatic view of the structures of the normal eyelid. The orbicularis muscle can be divided into the pretarsal, the preseptal and orbital parts although these are not separate anatomically. The pretarsal and preseptal parts together form the palpebral section of the orbicularis muscle which is responsible for blinking and facilitates the drainage of tears (see Ch. 20) and the orbital part is responsible for forced lid closure. The grey line is where orbicularis oculi meets the lid margin. This visible line lies anterior to the meibomian gland orifices and posterior to the eyelashes. It is the plane at which the anterior and posterior lamella can be separated during surgery. Removal of the orbicularis muscle exposes the underlying tarsal plates and orbital septum. The levator aponeurosis is the tendon of the levator muscle which inserts between the orbicularis muscle bundles and is responsible for the eyelid skin crease.
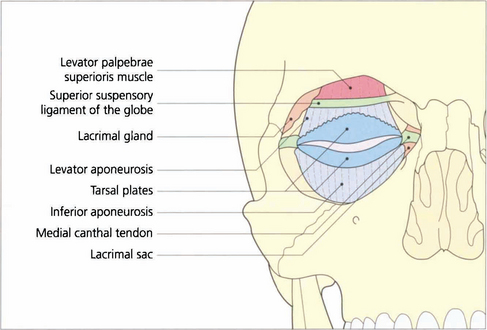
Fig. 2.2 The pre-aponeurotic fat pad lies behind the orbital septum. If it is elevated, the levator palpebrae superioris muscle with its aponeurosis is seen. Whitnall’s ligament (the superior suspensory ligament of the globe) is a thickening in the aponeurosis that helps to support the aponeurosis and the upper lid retractors. It runs from the periosteum of the lacrimal gland fossa to the trochlea of the superior oblique muscle. The inferior aponeurosis is the forward extension of the connective tissue from Lockwood’s ligament (the inferior suspensory ligament of the globe) and is continuous posteriorly with the sheath around the inferior rectus muscle (see Fig. 2.5).
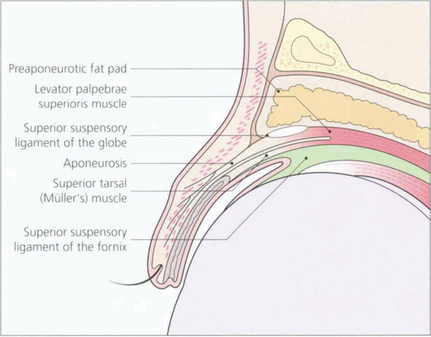
Fig. 2.3 The upper lid structures can be compared in diagrammatic and histological vertical sections. The levator palpebrae superioris muscle inserts into the anterior lamella and the posterior lamella (Müller’s muscle), both of which are responsible for lifting the eyelid. The connective tissue between the levator muscle and the superior rectus muscle (the common sheath) extends forward to support the upper conjunctival fornix (superior suspensory ligament of the fornix).
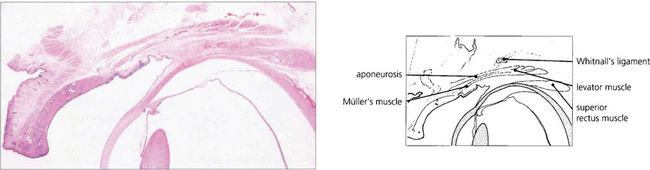
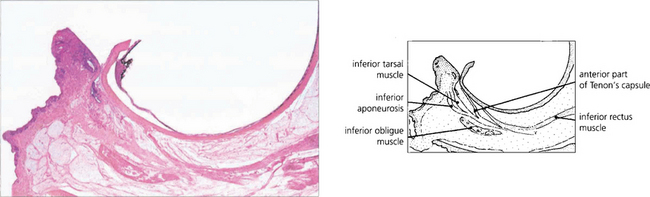
Fig. 2.4 Histological section of the upper lid corresponding to the cross-sectional diagram of Fig. 2.3.
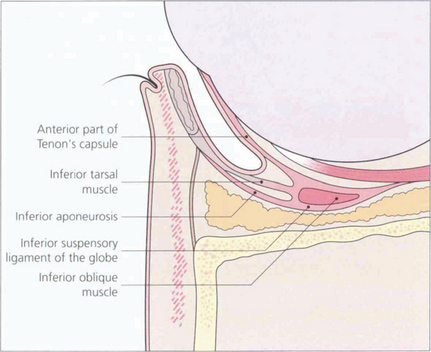
Fig. 2.5 Sections of the lower lid show the arrangement of the lower lid retractors. A condensation of fascia around the inferior oblique muscle forms the inferior suspensory ligament of the globe (Lockwood’s ligament). This is analogous to Whitnall’s ligament in the upper eyelid. It is attached medially and laterally in the region of the canthal tendons and can support the globe if the orbital floor is removed. The inferior aponeurosis extends forwards from Lockwood’s ligament with the inferior tarsal muscle (analogous to Müller’s muscle in the upper lid). These are the lower lid retractors which are responsible for depressing the lower eyelid on downgaze due to their connection with the inferior rectus muscle. A forward extension of the connective tissue associated with the lower lid retractors forms the inferior suspensory ligament of the fornix and anterior part of Tenon’s capsule.
CONGENITAL EYELID ABNORMALITIES
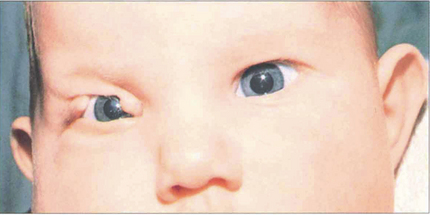
Fig. 2.7 Congenital lid colobomas are the result of a failure of normal development of the eyelid and closure of the facial clefts. Urgent repair is required only if the defect is so severe that the cornea is likely to suffer permanent damage from exposure.
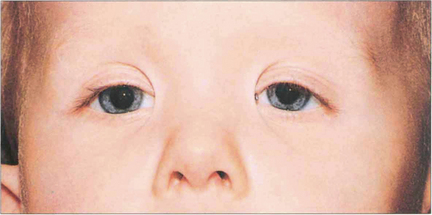
Fig. 2.8 Epicanthic folds are abnormal folds of skin at the medial canthus. They are common in childhood, especially in children of oriental origin, but they may also be acquired as a result of tissue loss from trauma. Congenital epicanthic folds frequently give an appearance of pseudostrabismus (see Ch. 18). They usually become less obvious with age but, if they persist, both congenital and acquired folds can be treated by a variety of plastic surgery procedures.
EYELID MALPOSITION
All forms of eyelid malposition may be congenital or acquired.
ENTROPION

Fig. 2.10 Horizontal lower lid laxity is assessed by grasping the lower lid skin and applying gentle traction away from the globe. (a) The extent to which the lid can be lifted off the globe is measured in millimetres; more than 6 mm is considered abnormal. (b) Laxity of the medial canthal tendon is assessed by gently pulling the lid laterally. The position of the punctum in relation to the limbus or pupil in primary gaze is then recorded. Lack of a lower lid skin crease in downgaze implies disinsertion of the inferior retractors.

Fig. 2.11 Congenital lower lid entropion is caused by hypertrophy of the skin and underlying orbicularis muscle. A mild degree of this hypertrophy is common in young children (epiblepharon) and, rarely, the eyelid margin itself inverts (congenital entropion). Should this fail to improve with age and cause irritation of the eye, it is corrected by the excision of the hypertrophic skin and underlying orbicularis muscle.
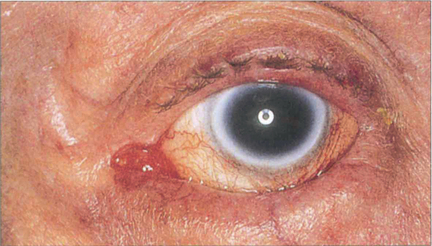
Fig. 2.12 Involutional entropion is a common condition caused by ageing changes affecting the orbicularis muscle, the lower lid retractors, the tarsal plate, the medial and lateral canthal tendons and the orbital fat. A variety of operations has been described to correct various combinations of these defects. These include sutures or incisions designed to prevent the upward movement of the preseptal muscle, tightening the lower lid retractors, eversion of the upper border of the tarsal plate and horizontal lid and canthal tendon shortening procedures.
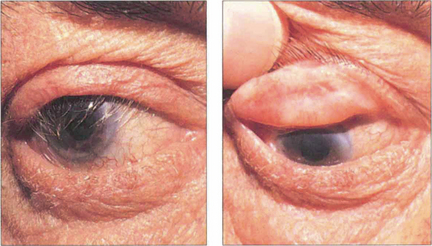
Fig. 2.13 Cicatricial changes can affect the posterior lamella of either the upper or lower lid and lead to entropion. This patient has scarring and shrinkage of the tarsal plate and conjunctiva. Common causes include trauma, acid and alkali burns, trachoma and other chronic conjunctival inflammations such as chronic staphylococcal lid disease, ocular pemphigoid or Stevens–Johnson syndrome. It may be possible to correct a cicatricial entropion with an everting procedure and rotation of the tarsal plate but if there is a marked degree of lid retraction a posterior lamellar graft will be required to lengthen the posterior lamella.
ECTROPION

Fig. 2.14 Congenital ectropion in neonates and very young children may be caused by crying and spasm of the orbicularis muscle. This does not usually require any treatment. If there is a shortage of skin, as in the case illustrated here, skin replacement is necessary with a graft or flap.
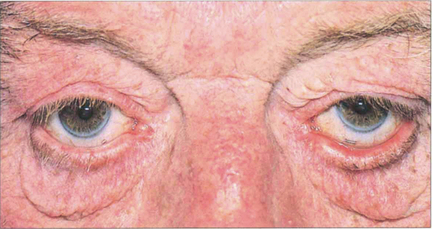
Fig. 2.15 Involutional lower lid ectropion is caused by a generalized laxity of all the lid tissues aggravated by gravity. Various operations have been described to correct the condition; most of these involve a horizontal shortening procedure of one or both lamellae or tightening of the canthal tendons with or without the removal of excess skin and orbital fat. Chronic exposure may cause conjunctival keratinization, punctal stenosis and chronic infection.
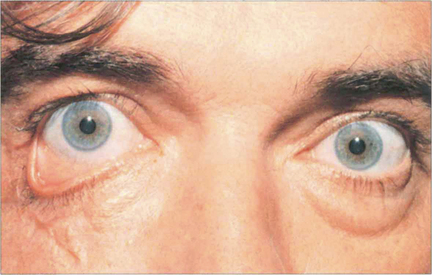
Fig. 2.16 Cicatricial lower lid ectropion may be caused by any condition that leads to a shortage of skin. This patient fell off his bicycle and lost skin; the resultant scarring caused a cicatricial ectropion. Surgical correction involves excision of the scar tissue, and replacement skin grafting. The lid must be shortened at the same operation if it has been stretched excessively by the scarring.
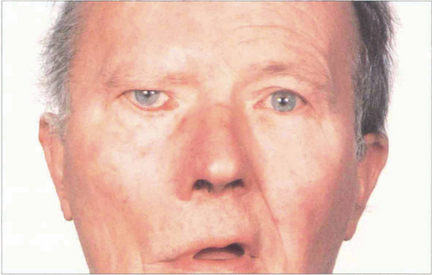
Fig. 2.17 Paralytic ectropion is caused by weakness of the orbicularis muscle (seventh nerve palsy) and subsequent lid laxity. Corneal exposure may be a problem, particularly if there is reduced trigeminal sensation (e.g. with a cerebellar pontine angle tumour such as acoustic neuroma). Bell’s phenomenon protects the cornea on forced eyelid closure, but is not always present. The cornea can be protected by transient ptosis induced by botulinum toxin if recovery of the seventh nerve palsy is expected. Medial canthalplasty and a lateral canthal sling may help, and a variety of other procedures such as fascia lata slings may be useful. The loss of brow wrinkling indicates this patient has a lower motor neurone seventh nerve palsy.
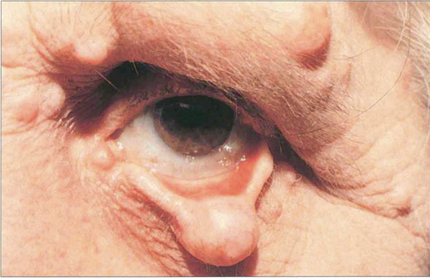
Fig. 2.18 Any form of lump on the lower lid can lead to a mechanical ectropion. The patient illustrated here has a localized neurofibroma of the lower lid. Treatment involves the excision of the tumour and correction of any induced horizontal laxity of the lid.
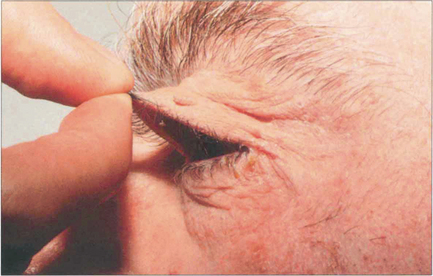
Fig. 2.19 The characteristics of the floppy eyelid syndrome are easy evertion of the upper lid and a chronic papillary conjunctivitis (which is caused by the mechanical abrasion of the upper tarsal conjunctiva on the lower lid lashes). It is associated with obesity and sleep apnoea and is a risk factor for cardiovascular and cerebrovascular disease. Patients need investigation for these underlying conditions.
PTOSIS
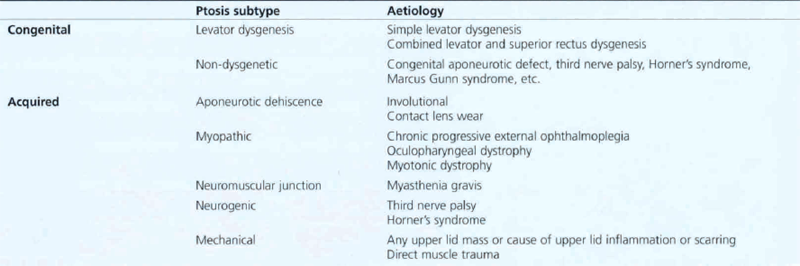
Blepharoptosis (ptosis) is a reduction in the vertical palpebral aperture due to descent of the upper lid as a result of pathology involving the eyelid retractors. A useful classification of ptosis can be made by considering pseudoptosis and congenital or acquired ptosis (Table 2.1). Pseudoptosis is associated with such problems as orbital volume deficiency, excess lid skin or hypotropia. Congenital ptosis is usually due to a dysgenesis of the levator palpebrae muscle which may be either unilateral or bilateral and may also affect the superior rectus, causing poor elevation of the eye. Acquired causes include myopathic, neurogenic, mechanical or aponeurotic defects. A careful history and examination is required for each patient paying special attention to such features as duration, progression or variability, associated symptoms such as diplopia and systemic muscle weakness and factors such as birth trauma, head or orbital injury and contact lens wear.
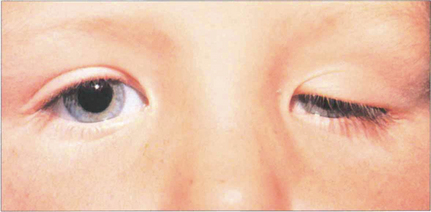
Fig. 2.20 Congenital ptosis. If the visual axis is not occluded by the eyelid it is reasonable to delay correction of a congenital ptosis until the child is old enough for a more accurate assessment when definitive surgery may be performed, usually around the age of 4 years. Congenital ptosis is also frequently associated with refractive errors that need correcting to prevent anisometropic amblyopia.

Fig. 2.21 Lid position on downgaze should be examined. Congenital dystrophy of the levator produces hang-up in downgaze because the levator does not relax properly and tethers the lid. This is accentuated by asking the patient to adopt a chin-up head posture. The skin crease position of both upper lids should be noted.
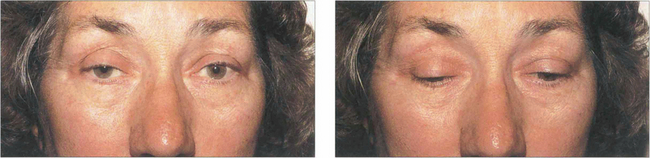
Fig. 2.22 Aponeurotic disinsertion is one of the commonest causes of ptosis. It is characterized by an elevated skin crease and increased ptosis on downgaze in the presence of normal levator function. This is frequently compensated for by overaction of the frontalis. This patient shows bilateral ptosis, worse on the right than the left, with high skin creases and bilateral frontalis overaction. The right upper lid is more ptotic on downgaze. Caution is required as identical changes can be seen in myasthenia gravis.
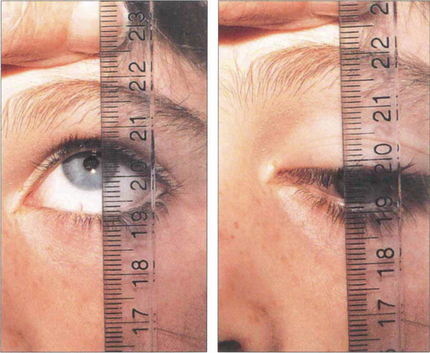
Fig. 2.23 The type of operation is governed primarily by the degree of remaining levator function which is assessed by measurement of the excursion of the upper lid from full downgaze to full upgaze. The frontalis muscle is prevented from acting by pressure over the brow. If levator function is 4 mm or better, the muscle can be shortened. Poorer levator function requires an alternative method of elevation such as a brow suspension.
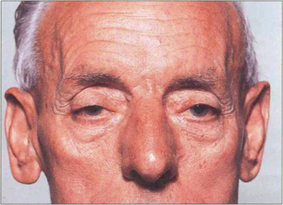
Fig. 2.24 Ocular myopathy usually presents as a bilateral progressive and symmetrical ptosis with a poor range of ocular movement, slow saccades on rapid gaze and weakness of the orbicularis. Most cases are due to a mitochrondrial myopathy but myasthenia gravis needs to be excluded in all cases. Ocular myopathy may be associated with systemic features such as generalized muscle weakness, swallowing difficulty and heart block. Surgical correction must be approached with caution as these patients usually have a poor Bell’s phenomenon and corneal exposure may result. Surgery is feasible only under local anaesthesia and the patient must be prepared to have the eyelid level adjusted at a later stage if the myopathy deteriorates. Ptosis props may be useful. Note the bilateral frontalis overaction in this patient and the loss of upper facial expression.
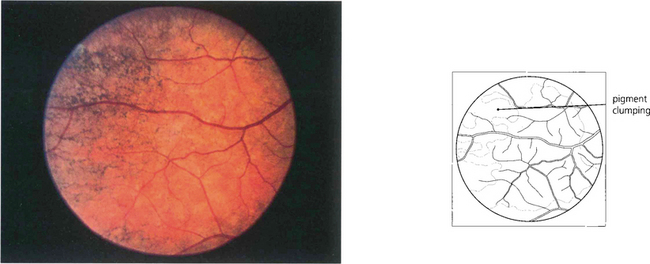
Fig. 2.25 This fundus photograph shows a mild peripheral pigmentary retinopathy in a patient with an ocular mitochondrial myopathy. The changes are often subtle and are not as florid as in retinitis pigmentosa. The ERG may be abnormal.
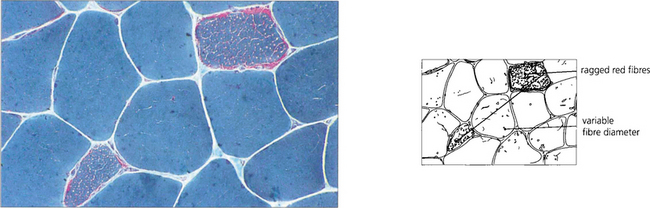
Fig. 2.26 Mitochondrial abnormalities are best demonstrated in a skeletal muscle biopsy by the presence of ‘ragged red fibres’ as seen in Gomori’s trichome stained sections.
By courtesy of Dr P H McKee.

Fig. 2.27 With a third nerve palsy, the eye deviates downwards and outwards as a result of the remaining action of the lateral rectus and superior oblique muscles. Depending on the cause of the palsy, the pupil may or may not be involved. Signs of aberrant regeneration should be looked for in all patients (see Ch. 19). This elderly woman has a complete ptosis. On elevating the lid it can be seen that she cannot adduct the eye; notice, too, that the pupil is not enlarged which suggests that the palsy is likely to be due to microvascular ischaemia, a common cause in the elderly.

Fig. 2.28 The sympathetic supply to the superior tarsal muscle (Müller’s muscle) is disrupted in Horner’s syndrome (see Ch. 19); this results in a ptosis of the upper lid of 1–2 mm. Miosis and ‘inverse ptosis’ of the lower lid may also be seen. In this case, hypopigmentation of the affected right iris suggests a congenital or extremely long-standing aetiology. In acute lesions hyperaemia of the conjunctiva and loss of sweating on the same side of the face may be seen. An anatomical localization of the neurological defect is important as preganglionic lesions are frequently associated with malignancy in the chest.

Fig. 2.29 Marcus Gunn (jaw-winking) ptosis is a congenital syndrome characterized by elevation of the ptotic lid when the mouth is opened or when the jaw is moved laterally, usually to the side opposite the ptosis. The eyelid may even become retracted as in this patient. The anomaly is due to a synkinesis between the levator and the medial and lateral pterygoid muscles.

Fig. 2.30 Excessive upper-lid skin (dermatochalasis) is usually the result of involutional changes involving the skin and may present as pseudoptosis and occasionally as visual field loss. The excess skin can be removed with a blepharoplasty. This patient has marked brow elevation and frontalis overaction on both sides.
EYELID RETRACTION
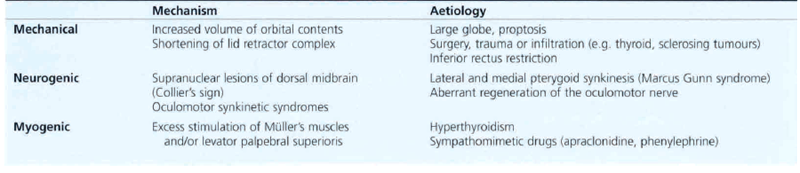
The height of the upper lid in relation to the limbus is dependent on mechanical forces such as the globe to orbital volume, the neural activity of the eyelid retractors and pathology of the ocular muscles or levator. Eyelid retraction must be differentiated from conditions such as proptosis and high myopia, as well as from contralateral ptosis. Scleral show on downgaze confirms the presence of primary lid retraction; if lid retraction is secondary to inferior rectus restriction, the retraction lessens in downgaze. The most common cause of upper and lower lid retraction is dysthyroid eye disease (Table 2.2). Treatment depends on the cause. The vertical height of the palpebral aperture can be reduced by excising Müller’s muscle, recessing the upper lid retractors or inserting a graft of material such as hard palate, ear cartilage or artificial spacer material.

Fig. 2.31 This patient has bilateral upper and lower lid retraction resulting from dysthyroid eye disease (see Ch. 20).
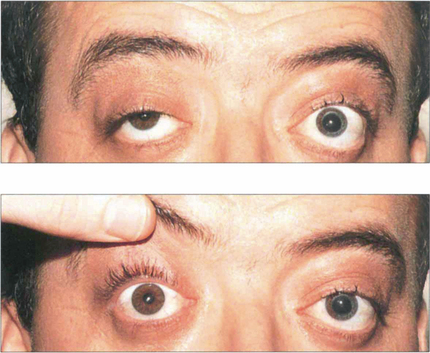
Fig. 2.32 Patients with a unilateral ptosis may have an apparent retraction of the contralateral upper lid due to increased neuronal stimulation of this levator, according to Herring’s law. When the ptotic lid is elevated the excessive neuronal stimulation is relieved and after a few minutes the retracted lid falls to a normal level.
EYELID TUMOURS
BENIGN LID TUMOURS

Fig. 2.33 Xanthelasmas are infiltrates of lipid-laden histiocytes in the dermis. They may be either idiopathic or associated with hyperlipidaemia. Local treatment consists of excision or argon laser ablation. Patients should be investigated for hyperlipidaemia.
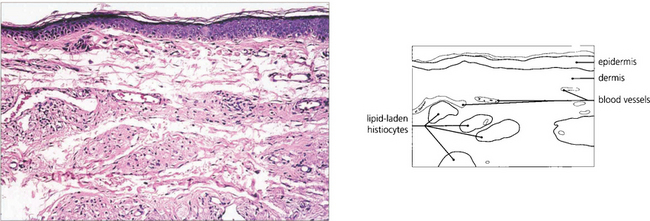
Fig. 2.34 Histological examination shows aggregations of lipid-laden histiocytes in the dermis in relation to blood vessels.
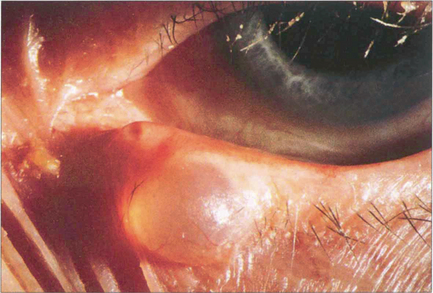
Fig. 2.35 Cysts of Moll are retention cysts of the apocrine glands of Moll. They occur at the lid margin and appear translucent because they are filled with clear fluid. They are treated by excision or marsupialization.
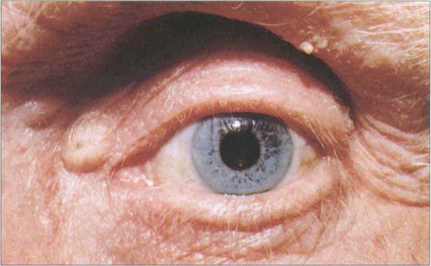
Fig. 2.36 Sebaceous cysts appear as yellowish-white lumps in the skin and have a central occluded punctum. They are caused by blockage of pilosebaceous units and contain retained cheesy yellow keratin. They can be treated by simple excision.
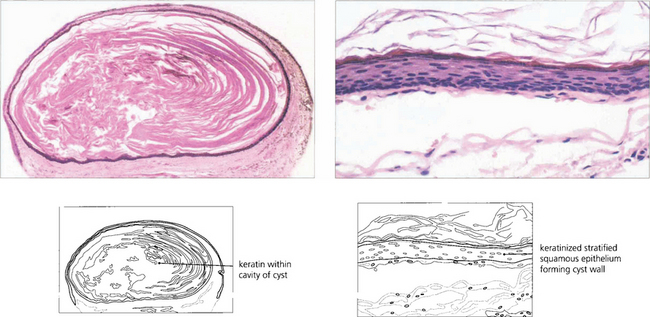
Fig. 2.37 Sebaceous cysts contain keratin and are lined by keratinized stratified squamous epithelium. Low (left) and high (right) magnification.

Fig. 2.38 Cysts of Zeis arise from the glands of Zeis in the same way as sebaceous cysts arise elsewhere. Like sebaceous cysts, they contain keratin. They can be incised.

Fig. 2.39 Meibomian cysts (chalazions) are not true cysts. They are due to granulomatous inflammation caused by retained sebaceous secretion leaking into the stroma of the lid following blockage of the meibomian glands in the tarsal plate. Clinically they sometimes present in the acute stage as a red, tender swelling within the tarsal plate of the upper or lower eyelid (left). This either resolves completely or leaves a firm nodule (right). Alternatively, they can present as a painless, non-inflamed lump in the tarsal plate. Treatment is initially conservative with heat and local antibiotics, but if resolution does not occur incision and curettage are performed.
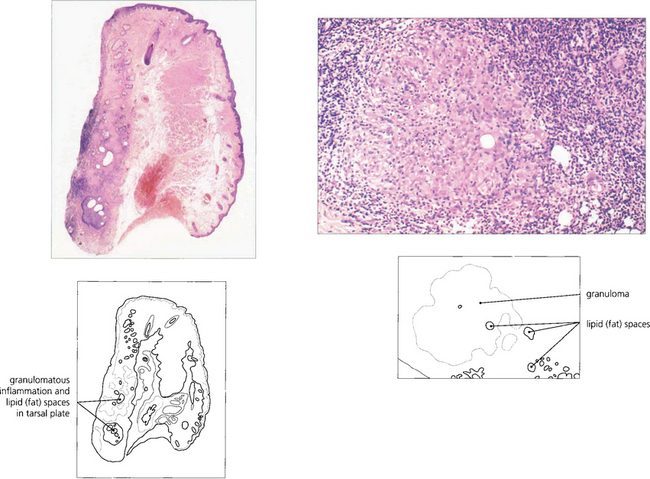
Fig. 2.40 This eyelid shows a localized lesion in the tarsal plate; higher magnification shows a granulomatous inflammatory reaction to lipid which has been leached during processing to leave empty spaces (fat spaces).

Fig. 2.41 Capillary haemangiomas are one of the commonest lid tumours seen in infancy. They have a predilection for the upper lid and, if large enough, may cause amblyopia. They may become more prominent when the child cries. Many involute spontaneously, as in this child over 2 years, but intralesional steroid injections may speed up the process.
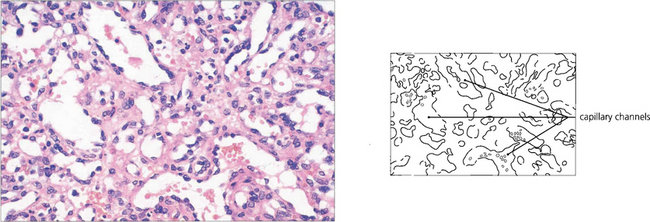
Fig. 2.42 Histological examination shows irregular capillary channels of varying size in the dermis and subcutaneous tissue.

Fig. 2.43 An eyelid neurofibroma may be diffuse, as in this patient, or localized (Fig. 2.18). Localized lesions may be excised, but large lesions require careful debulking. Plexiform neurofibromas are usually seen with type 1 neurofibromatosis. This child also has partial hemihypertrophy of the face, ectropion uveae and sphenoidal wing dysplasia.
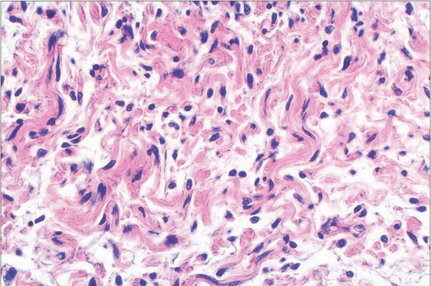
Fig. 2.44 Histological examination of a neurofibroma shows proliferation of Schwann cells, fibroblasts and nerve axons with wavy collagen fibres.
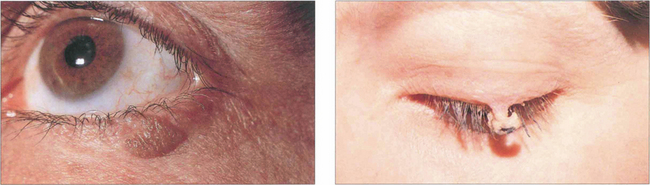
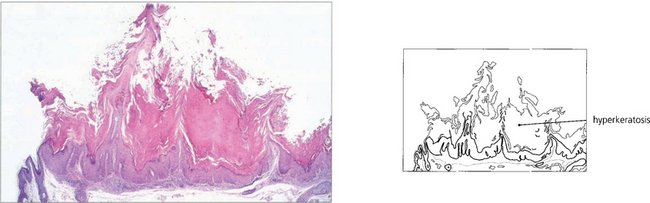
Fig. 2.45 A simple squamous cell papilloma is a benign overgrowth of squamous epithelium commonly found on the lids or lid margin with a typical raspberry-like appearance (left). Keratin may build up on the surface of a squamous papilloma to form a cutaneous horn (right). The lesion can be simply excised or cauterized.
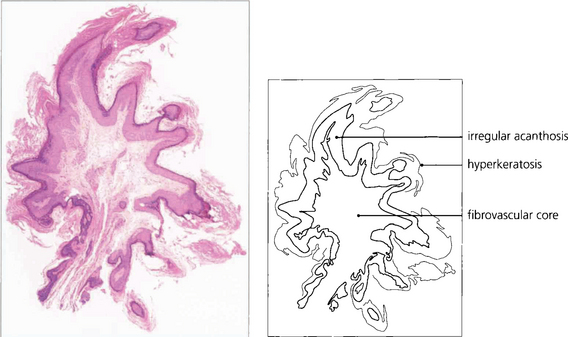
Fig. 2.46 This example shows a fibrovascular core with overlying irregular acanthosis (thickened squamous cell layer) and hyperkeratosis.

Fig. 2.47 Seborrhoeic keratosis (seborrhoeic wart, basal cell papilloma) occurs in the elderly as a benign, discrete and often rather greasy and pigmented raised lesion. Other lesions are frequently present elsewhere on the body.

Fig. 2.48 Histologically seborrhoeic keratoses are epidermal thickenings consisting mainly of basal cells. A characteristic feature is the abrupt transition from basal cells to squamous cells and keratin production with the formation of keratin-filled cysts (horn cysts). The amount of surface keratin is variable and the pigmentation seen clinically is due to melanin in the basal cells.

Fig. 2.49 A keratocanthoma is a rapidly growing, dome-shaped lesion with a central core of keratin, most commonly seen on the lower lid. It usually grows vigorously over a 3-month period and then involutes spontaneously. Should involution not occur, however, the lesion should be excised in its entirety for histological identification as a small number may be confused with squamous cell carcinoma.
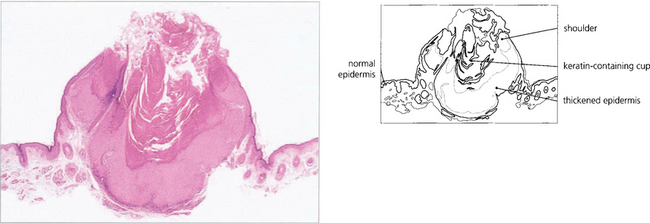
Fig. 2.50 The histological diagnosis of a keratoacanthoma depends largely upon an adequate clinical history as the appearance can resemble a well-differentiated squamous cell carcinoma. Microscopy shows epidermal thickening with a sharp transition from normal to abnormal epidermis. There is well-marked shoulder formation and a central keratin-containing cup.
LID TUMOURS WITH MALIGNANT POTENTIAL

Fig. 2.51 In clinical practice actinic (solar or senile) keratosis is the most common precancerous skin lesion. It relates to excessive solar radiation rather than age. It presents as a dry, scaly and slightly raised lesion with excess keratin, mainly in elderly people with fair skins who have been exposed to excessive sun. There is an underlying squamous dysplasia that may eventually proceed to invasive squamous cell carcinoma (see Figs 2.53 and 2.54). Lesions can be treated by excision or cryotherapy, depending on size and location.
MALIGNANT LID TUMOURS
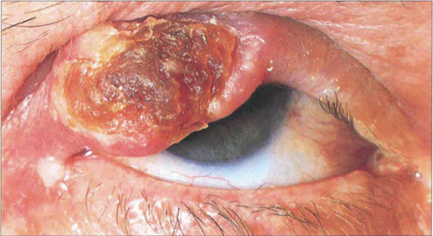
Fig. 2.53 Squamous cell carcinoma may arise de novo or from a pre-existing actinic keratosis or Bowen’s disease (carcinoma in situ), and is especially common in the rare syndrome of xeroderma pigmentosum. The tumour has an everted edge and is relatively more common on the upper eyelid. It may metastasize to the regional lymph nodes. Treatment is usually by surgical excision.
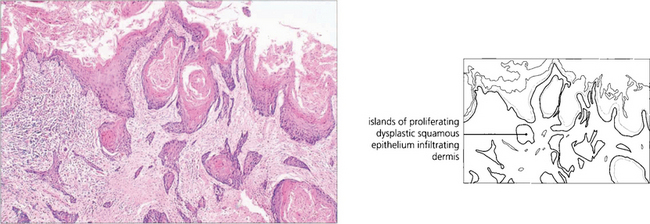
Fig. 2.54 Microscopy shows downward proliferation of dysplastic squamous epithelium with invasion into the dermis.
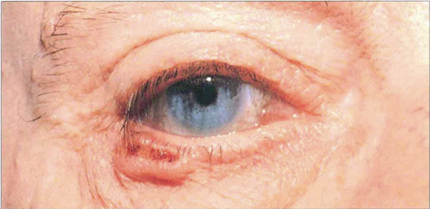
Fig. 2.55 Basal cell carcinoma is the most common malignant eyelid tumour. It usually arises on the lower eyelid or at the medial canthus. Nodular, ulcerating and sclerosing (morpheic) types are seen. Treatment is by surgery, radiotherapy or cryotherapy depending on the site of the lesion and the physician’s preference. Surprisingly, of tumours that are incompletely excised, only about 25 per cent will recur clinically. This is an example of a relatively benign type of basal cell carcinoma with a classical pearly margin laced with blood vessels and a central shallow ulcerated base.
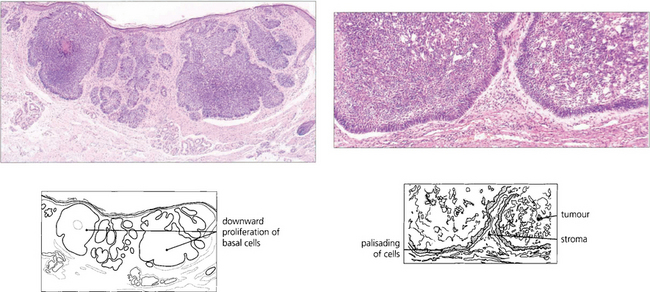
Fig. 2.56 The tumour arises from the pluripotential germinative cells that form the basal layer of the epidermis. Areas of glandular or squamous differentiation can be seen in some tumours. Palisading of cells at the periphery of tumour lobules is a common feature (right).

Fig. 2.57 This example of basal cell carcinoma shows a sclerosing (morpheic) tumour with a less clearly defined margin. At operation it is difficult to define the tumour margins, and this type of lesion is best excised by Mohs’ micrographic surgical technique to ensure complete removal.
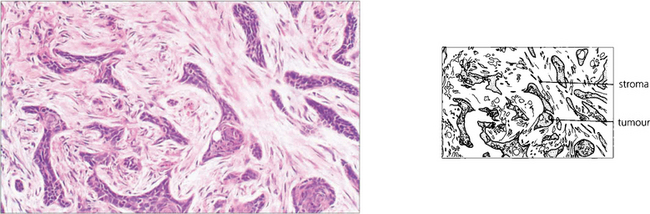
Fig. 2.58 Histological examination shows elongated strands of tumour cells embedded in a dense fibrous stroma.

Fig. 2.59 Basal cell carcinomas spread by direct extension and may be highly invasive, although they do not metastasize. Local invasion is a particular problem of tumours at the inner canthus as these may involve the lacrimal drainage apparatus or nasal sinuses.
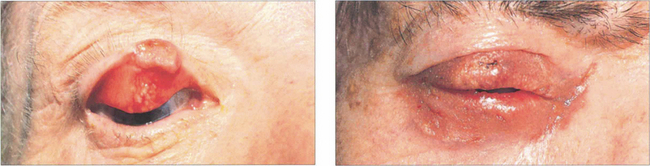
Fig. 2.60 Meibomian gland carcinoma may occur in either a localized or a more generalized form. When the carcinoma is relatively localized, it often presents as a persistent and recurrent meibomian cyst. These localized tumours, shown on the left, can be excised surgically. The more generalized form (right) often presents as a severe unilateral and persistent chronic blepharitis. Diffuse disease normally carries a poor prognosis and requires treatment with a combination of radiotherapy and surgery.
PIGMENTED EYELID LESIONS
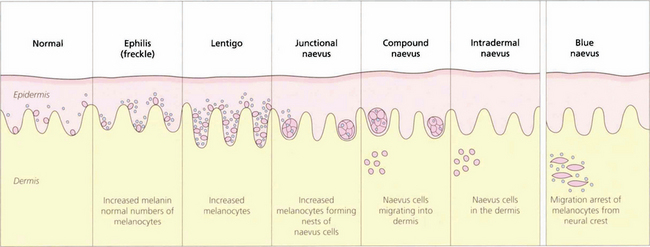
Fig. 2.61 All melanocytes are derived from the neural crest. Epidermal melanocytes can form naevus cells and so lead to the development of junctional, compound and intradermal naevi. In contrast, dermal melanocytes can form blue naevi.
Pigmented lid lesions with malignant potential
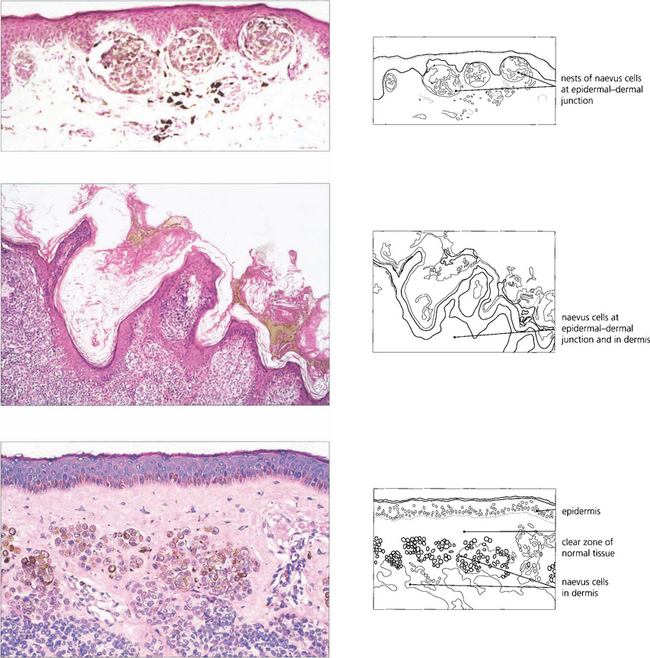
Fig. 2.62 It is difficult to diagnose the naevus type by the clinical appearances. Junctional naevi can occur at the lid margin and are usually flat and well circumscribed; the naevus cells lie at the epidermal–dermal junction (top). Compound naevi are raised, pigmented or warty lesions occasionally with hairs on the surface. Histological examination shows, as in this example (middle), naevus cells at the epidermal–dermal junction and within the dermis; there may also be a papillary configuration. Intradermal naevi present as dome-shaped nodules, papillomatous lesions or skin tags; they are frequently devoid of pigment and are often excised as ‘papillomas’; naevus cells are found only within the dermis; a clear zone of normal tissue separates them from the epidermis (bottom).
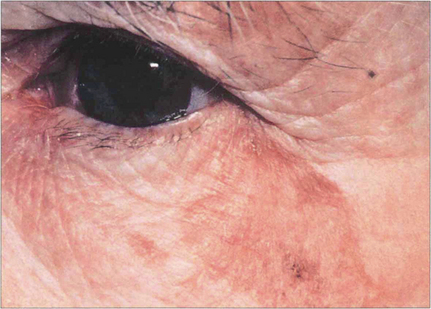
Fig. 2.63 Lentigo maligna presents as an irregular, flat, tan-brown, variably pigmented patch, ranging in size from a few millimetres to several centimetres. It has the potential of evolving into a fully invasive malignant melanoma; the development of a papular darker area often coincides with the histological findings of invasion. Macules enlarge slowly over 5–10 years. Between 10 and 25 per cent of all head and neck melanomas arise from lentigo maligna.
By courtesy of Dr C M Lawrence.
Malignant pigmented lid lesions

Fig. 2.64 A malignant melanoma can arise de novo or from a pre-existing junctional or compound naevus. Warning signs of malignant change in a naevus are a rapid increase in size, satellite lesions, ulceration or haemorrhage, but any pigmented eyelid lesion that is growing should be excised. These examples show early malignant change in a pre-existing naevus (left) and an advanced malignant melanoma (right).
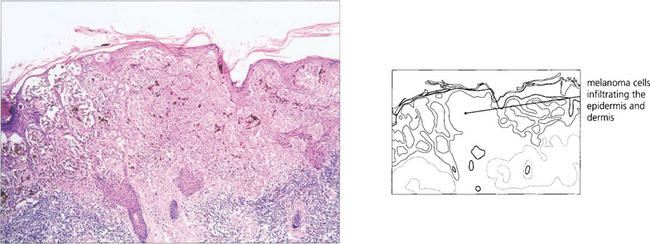
Fig. 2.65 Malignant melanoma comprises about 1 per cent of eyelid malignancies. Melanoma cells can be seen infiltrating both the epidermis and dermis in this specimen. Tumours involving the lid margin and those that are more than 0.75 mm in thickness carry a poorer prognosis; spread occurs through the lymphatics or bloodstream.
EYELID TRAUMA

Fig. 2.66 Full-thickness loss of eyelid tissue, as in this case following a caustic burn, may result in corneal exposure and requires sophisticated techniques of lid reconstructive surgery. Conjunctival damage is often present, creating problems of symblepharon and loss of ocular motility, dry eye or damage to the lacrimal drainage system.
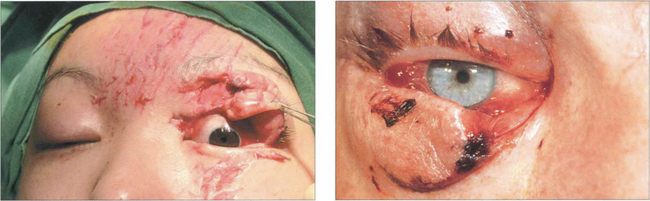
Fig. 2.67 Lateral traction injury to the eyelid may avulse it from the medical canthal tendon, lacerating the lacrimal drainage apparatus without loss of lid tissue.
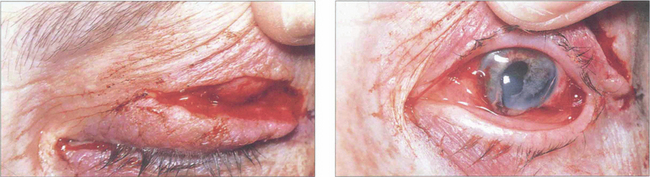
Fig. 2.68 Upper lid lacerations need to be explored carefully and the levator repaired if cut. A search should be made for a foreign body within any perforating lid injury, and the globe must always be visualized and the fundus examined. This patient had a full-thickness lid laceration with perforation of the globe from a broken bottle injury.
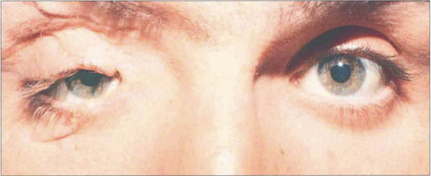
Fig. 2.69 In this patient, severe injuries around the right orbit have caused orbital wall fractures and avulsion of the medial canthal tendon, resulting in a traumatic telecanthus. Such a severe injury may also cause ptosis as in this case, either from direct injury to the levator complex, injury to the nerve supply, or by causing enophthalmus following a blow-out fracture.
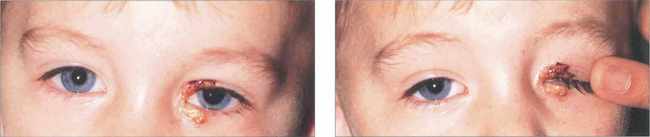
Fig. 2.70 Nonaccidental injury. This child was burned on the lids with a cigarette. In suspected cases of nonaccidental injury, the child should be formally assessed for retinal haemorrhages from throttling, skeletal injuries and healing fractures by a paediatrician experienced in the medico-legal implications of diagnosis.