Chapter 7
The Eye1
Who would believe that so small a space could contain the images of all the universe? O mighty process!
Leonardo da Vinci (1452–1519)
Historical Considerations
The eyes are the windows to the world. Most of the sensory input to the brain comes from the eyes. For centuries, the eye has been considered the essence of the person, representing the “I.” In mythology and the writings of ancient times, the eye is an organ associated with mystical powers.
The eye has long been associated with mythical gods. In ancient Egypt, the eye was the symbol of the Great Mother Goddess Maat, goddess of law, morality, and justice. The Egyptians believed that Maat held the universe together. The Eye of Maat later became known as the Eye of Horus. The Eye of Horus was believed to protect against all evil and to ensure success. The “evil eye” from the myth of Medusa was an expression of envy and greed (see Fig. 27-3). To this day, people wear talismans to ward off the “evil eye.”
Another interesting association is the subconscious linking of “eyeball” with genitalia. Blindness can symbolize castration because testicles and eyeballs have the same shape and are important in the development of the sense of identity. This linking goes back to the legend of Oedipus, who pierced his eyeballs when he discovered that he had been married to his mother and had killed his father. This can be thought of as an act of self-castration, as well as a means of cutting oneself off from all worldly relationships. Throughout literature, the blinding of an individual was frequently a form of punishment for lust. The age-old notion that masturbation causes blindness further reinforces this close association of these organs.
Structure and Physiology
The external landmarks of the eye are shown in Figure 7-1, and the cross-sectional anatomy of the eye is shown in Figure 7-2.
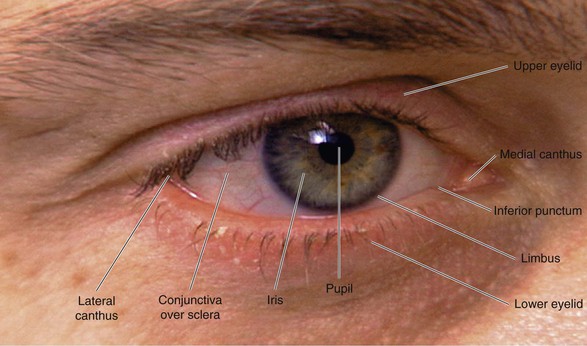
Figure 7–1 External landmarks of the eye.
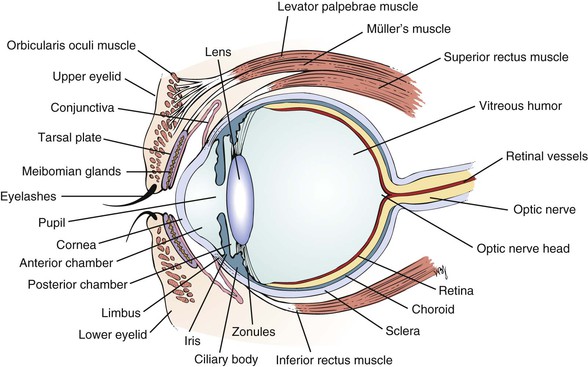
Figure 7–2 Cross-sectional anatomy of the eye.
The eyelids and eyelashes protect the eyes. The eyelids cover the globe and lubricate its surface. The meibomian glands, which are modified sebaceous glands in the eyelids, secrete meibum, an oily lubricating substance that retards evaporation. The openings of these glands are at the eyelid margins. This is illustrated in Figure 7-28B.
The orbicularis oculi muscle encircles the lids and is responsible for their closure. This muscle group is the reason we have such expressive eyes. This muscle is supplied by the facial, or seventh cranial, nerve. The levator palpebrae muscle elevates the lids and is innervated by the oculomotor, or third cranial, nerve. Müller’s muscle is a small part of the levator muscle that has sympathetic innervation.
The globe has six extraocular muscles that control its motion. There are four rectus and two oblique muscles: the medial rectus, the lateral rectus, the superior rectus, the inferior rectus, the superior oblique, and the inferior oblique muscles. These six extraocular muscles are shown in Figure 7-3.
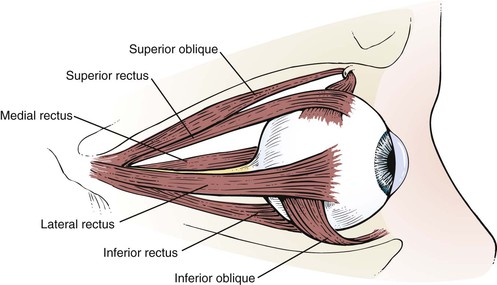
Figure 7–3 The extraocular muscles.
The extraocular muscles work in a parallel, conjugate manner to maintain single, binocular vision. When the head is turned to look left, for example, the left lateral rectus and the right medial rectus contract to turn the eyes to the left. The actions and innervations of the extraocular muscles are listed in Table 7-1, and the extraocular movements are illustrated in Figure 7-4.
Table 7–1
Actions and Innervations of the Extraocular Muscles*
| Muscle | Action | Cranial Nerve Innervation |
| Medial rectus | Adduction (eye moves nasally) | Oculomotor (III) |
| Lateral rectus | Abduction (eye moves temporally [away from the nose]) | Abducens (VI) |
| Inferior rectus | Depression (eye moves down) Extorsion (the 12 o’clock position on the cornea rotates temporally) Adduction |
Oculomotor (III) |
| Superior rectus | Elevation (eye moves up) Intorsion (the 12 o’clock position on the cornea rotates nasally) Adduction |
Oculomotor (III) |
| Superior oblique | Intorsion Depression Abduction |
Trochlear (IV) |
| Inferior oblique | Extorsion Elevation Abduction |
Oculomotor (III) |
* Remember “LR6SO4.” This mnemonic means that the lateral rectus (LR) muscle is innervated by the sixth cranial nerve, and the superior oblique (SO) muscle is innervated by the fourth cranial nerve. All the other muscles are innervated by the third cranial nerve.
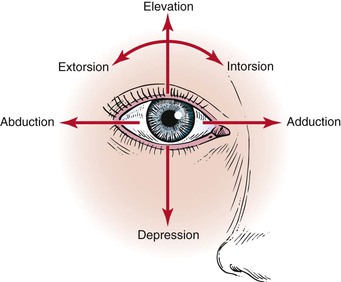
Figure 7–4 Extraocular movements.
The lateral rectus muscle, which is innervated by the abducens nerve, turns the eye laterally (abducts the eye), as do both oblique muscles. As easy way to remember the innervations is the formula LR6SO4, meaning that the lateral rectus is innervated by cranial nerve VI (abducens) and the superior oblique is innervated by cranial nerve IV (trochlear); all the other muscles are innervated by cranial nerve III (oculomotor).
The conjunctiva is a thin, vascular, transparent mucous membrane that lines the lids of the anterior portion of the globe. The palpebral portion covers the inner surface of the lids, whereas the bulbar portion covers the sclera up to the limbus, which is the corneal-scleral junction. The conjunctiva contains many small blood vessels, which, when dilated, produce the appearance of a “red” eye. There is little nervous innervation to the conjunctiva.
The lacrimal apparatus consists of the lacrimal gland, accessory tear glands, canaliculi, tear sac, and nasolacrimal duct. These are shown in Figure 7-5.
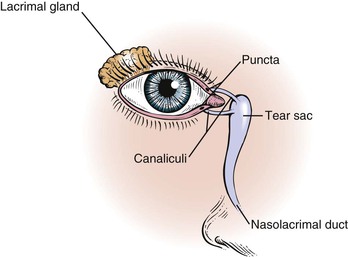
Figure 7–5 The lacrimal apparatus.
The lacrimal gland produces watery tears and is located above and slightly lateral to the globe. Secretion occurs mostly as reflex tearing or crying. Tears drain through the puncta on the lids and into the superior and inferior canaliculi. These canaliculi join and enter the tear sac, located at the medial canthus of the eye. The nasolacrimal duct drains tears from the sac to the nose. Of the lacrimal apparatus, only the puncta are visible on routine examination.
The sclera is the white, fibrous, outer coat of the globe visible just beneath the conjunctiva. The extraocular muscles insert onto the sclera.
The cornea is a smooth, transparent, avascular tissue that covers the iris and joins with the sclera and conjunctival reflection at the limbus. The cornea functions as a protective window, allowing light to pass into the eye. The cornea is richly innervated by the trigeminal, or fifth cranial, nerve and is therefore exquisitely sensitive to touch and pain.
The anterior chamber, or space between the cornea anteriorly and the iris posteriorly, is filled with clear aqueous humor. Aqueous humor is produced by the ciliary body in the posterior chamber, the area behind the iris and in front of the lens. Aqueous humor circulates from the posterior chamber through the pupil into the anterior chamber and is filtered out through the canal of Schlemm, from where it eventually enters the venous system. Pressure within the eye is regulated by this filtration. The angle is formed by the juncture of the cornea and the iris at the limbus. A section through the eye at this level is shown in Figure 7-6.
The iris is the circular, colored portion of the eye. The small, round aperture in the middle of the iris is the pupil. Because it is optically empty in the healthy eye, it appears black. The pupil functions much like the aperture of a camera, controlling the amount of light that enters the eye.
When a light is shined on one eye, both pupils constrict consensually. This constriction is the pupillary light reflex. To understand this reflex, a brief review of the neuroanatomy is in order. Figure 7-7 illustrates the pathways of the pupillary light reflex.
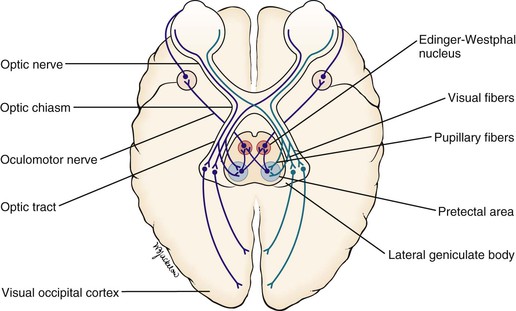
Figure 7–7 The pupillary light reflex.
The optic, or second cranial, nerves are composed of 80% visual and 20% afferent pupillary fibers. The optic nerves leave both retinas and travel a short course to where they join each other. This joining is the optic chiasm. At the optic chiasm, the nasal fibers cross and join the uncrossed fibers of the other side, forming the optic tract. The visual fibers continue in the optic tract to the lateral geniculate body, where synapses occur, the axons of which terminate in the primary visual cortex of the occipital lobe. The afferent pupillary fibers bypass the geniculate body and end in the superior colliculus and pretectal area of the midbrain.
Light impulses to the eye cause the retina to transmit nerve impulses to the optic nerve, the optic tract, the midbrain, and the visual cortex of the occipital lobes. This is the afferent limb of the light reflex. In the midbrain, the pupillary fibers diverge and are relayed by crossed fibers to the opposite Edinger-Westphal nucleus of the oculomotor, or third cranial, nerve. Some fibers remain on the same side. The third cranial nerve is the efferent limb, which goes via the ciliary body to the sphincter muscle of the iris to cause it to contract. The direct effect is the constriction of the pupil of the eye on which the light is shined (the ipsilateral eye). The consensual effect is the simultaneous constriction of the opposite pupil (the contralateral eye).
The near reflex occurs when the subject looks at a nearby target. The three parts of the near reflex are accommodation, convergence, and pupillary constriction. Accommodation is defined as the near focusing of the eye, which is effected by increasing the power of the lens by contraction of the ciliary muscle, innervated by the third cranial nerve.
There is also autonomic innervation of the eyes. The iris is supplied by sympathetic and parasympathetic fibers. When the sympathetic fibers are stimulated, the pupil dilates, and the eyelid elevates. Think of the cat stalking its prey, pupils dilated, ready to pounce in the dark. The cat needs all the light it can get. The reflex is purely sympathetic. When the parasympathetic fibers in the oculomotor nerve are stimulated, pupillary constriction occurs. When we sleep, our bodies are in a parasympathetic mode and our pupils are constricted.
The lens sits directly behind the iris. It is a biconvex, avascular, colorless structure that changes its shape to focus the image on the retina. The shape is changed by the ciliary body muscles contracting. They in turn are connected to the zonules of the lens, thereby changing its shape.
The vitreous humor is the transparent, avascular gel that is located behind the lens and in front of the retina. It occupies 80% of the volume of the eye. This clear matrix is made up of collagen, hyaluronic acid, and water. It is bounded by the posterior lens capsule anteriorly and the retina posteriorly.
The choroid is the middle, vascular layer of the globe between the sclera and the retina. It acts as a source of nourishment, as well as a heat sink, serving to remove the extreme heat produced by the light energy entering the eye. Bruch’s membrane separates the choroid from the retina. Superficial to Bruch’s membrane (closer to the retina) is the retinal pigment epithelium (RPE). The RPE is a monolayer of cells between Bruch’s membrane and the retina. Some of the important functions of the RPE are to absorb light passing through the retina and to regenerate the visual pigments.
The retina is the innermost layer, or “camera film,” of the eye. The retina is attached firmly to the underlying choroid at the optic nerve posteriorly and at the ora serrata anteriorly. Between these two points, the retina is in contact with the choroid, but it is not attached to it. The ora serrata is the junction of the retina and ciliary body. The retina is only 0.4 mm in thickness and is thinnest in the region of the macula. Histologically, the retina is made up of 10 distinct layers. Basically, the retina senses light through the rods and cones in its outer layer (closest to the RPE); performs initial signal processing in its middle layer; and encodes and transmits the data in its inner layer, the nerve fiber layer. The nerve fiber layer is directly under the inner limiting membrane of the retina, the layer closest to the vitreous. These nerve fibers course along the inner portion of the retina and aggregate to form the optic nerve. On leaving the eye, the nerve fibers become myelinated.
Within the retina are several important structures: the optic disc, the retinal vessels, and the macula. Figure 7-8 illustrates the retina of the left eye.
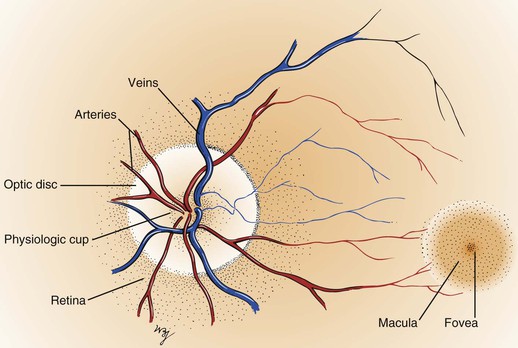
Figure 7–8 The retina of the left eye.
The optic disc is located at the nasal aspect of the posterior pole of the retina. This is the head of the optic nerve, from where the nerve fibers of the retina exit the eye. The optic disc is 1.5 mm in diameter and is ovoid. It is lighter than the surrounding retina and appears yellowish-pink. The disc margins are sharp with some normal blurring of the nasal portion. African-American patients may have pigmentation at the margins. The physiologic cup is the center of the disc, where the retinal vessels penetrate. This small depression normally occupies approximately 30% of the disc diameter.
The retinal vessels emerge from the disc and arborize on the retinal surface. The arteries are brighter red and thinner than the veins. An artery-to-vein ratio of 2 : 3 is normal.
The macula is a small, round area, approximately the size of the disc, located 3.5 mm temporal to and 0.5 mm inferior to the disc. The macula is easily seen because it is devoid of retinal vessels. In the center of the macula is the fovea, a depressed area composed only of cones. Cones provide detailed vision and color perception.
The remaining areas of the retina contain mostly rods, which compose the other neurosensory element of the retina. The rods are responsible for motion detection and night vision. It should be remembered that the image on the retina is upside down and reversed left to right: The right world is projected on the left half of the retina, and the left world is projected on the right half of the retina. An image in the superior world strikes the inferior part of the retina, and an inferiorly positioned image strikes the superior part. This concept is illustrated in Figure 7-9.
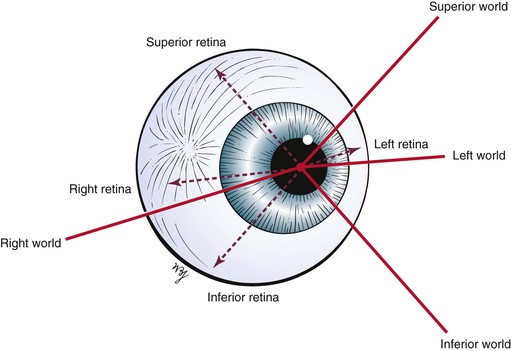
Figure 7–9 How images strike the retina.
At birth, there is little pigment in the iris, which is why many infants are born with blue eyes. By 6 months of age, the pigmentation is complete. The lens is more spherical at birth than in later life. Most infants are born hyperopic (farsighted). By 3 months after birth, the medullation process of the optic nerve is completed. As the child grows, hyperopia increases until the age of 8 years and then gradually decreases. After age 8, myopia (nearsightedness) appears to increase.
With advancing age, there is the gradual loss of elasticity of the skin around the eyes. The cornea may show an infiltration of cholesterol deposits around the limbus, which is known as an arcus senilis. The lens consistency changes from plastic to rigid, making it progressively more difficult to change its shape to focus on near objects. This condition is presbyopia. The lens may undergo changes resulting from metabolic disorders that cause its opacification; this condition is called a cataract. The vitreous humor may develop condensations, called floaters. The retinal arteries may develop atherosclerosis, with resultant retinal ischemia or infarction.
Review of Specific Symptoms
The major symptoms of eye disease are the following:
Loss of Vision
When a patient complains of loss of vision, the following two questions must be asked:
It is extremely important to ascertain the acuteness of the loss of vision and the presence or absence of pain. Sudden, painless loss of vision may result from a retinal vascular occlusion or a retinal detachment. Sudden, painful loss of vision occurs in attacks of acute narrow-angle glaucoma. Gradual, painless loss of vision commonly occurs in chronic simple glaucoma and cataracts.
Eye Pain
Eye pain may result from a variety of causes. Ask the patient the following questions:
“Did the pain come on suddenly?”
“Does the light bother your eye?”
“Do you have pain when you blink?”
“Do you have the sensation of something in the eye?”
“Do you have pain on movement of the eye?”
Pain may be experienced as “burning,” “aching,” “throbbing,” “tenderness,” or pain behind the eye. Each of these descriptions may have a range of causes. It is important to determine whether the patient has the sensation of a foreign body in the eye. Pain in the eye while blinking occurs in corneal abrasions and with foreign bodies in the eye. Photophobia is eye pain associated with light, as seen in inflammations of the uveal tract (i.e., iris, ciliary body, or choroid). Inflammations of the conjunctiva, conjunctivitis, produce a gritty sensation. Diseases of the cornea are associated with significant pain because the cornea is so richly innervated. Headaches and eye pain are common in acute narrow-angle glaucoma. Pain on motion of the eye occurs in optic neuritis. Eye pain associated with brow or temporal pain may be an indication of temporal arteritis (see Chapter 22, The Geriatric Patient). Contact lens wearers may have corneal irritation and may complain of eye pain.
Diplopia
Diplopia, or double vision, is a common complaint. Diplopia results from a faulty alignment of the eyes. Normally, when the eyes fixate on an object, the object is seen clearly, despite the fact that the two retinal images are not exactly superimposed. These slightly different images, however, are fused by the brain; it is this fusion that produces binocular vision, or the perception of depth. When the eyes are misaligned, the two images fall on different parts of the retinas, with only one falling normally on the fovea. The field of vision of the deviated eye is different, so that its image is not projected on its fovea; therefore, this second image is different and not superimposable. The patient may close one eye to relieve this distressing situation. A compensatory head posture may be used by the patient to relieve the double vision (see Fig. 7-152). Elevation or depression of the patient’s chin is used to overcome a vertical deviation. Tilting of the head is often used to counteract the torsional and vertical deviation. Suggested questions for the patient with diplopia are listed in Chapter 18, The Nervous System.
Tearing and Dryness
Excessive tearing of the eyes is a common complaint. Abnormal tearing may be caused either by overproduction of tears or by an obstruction of outflow. The eye depends on the flow of tears to provide constant moisture and lubrication to maintain vision and comfort. Tears are a combination of water, for moisture; oils, for lubrication; mucus, for even spreading of the tears; and antibodies and special proteins, for resistance to infection. These components are secreted by special glands located around the eye. Thus tears provide lubrication, reduce the risk of eye infection, wash away foreign matter in the eye, and keep the surface of the eyes smooth and clear.
When there is an imbalance in this tear system, a person may experience dry eyes. Nearly fifty-five million Americans 50 years of age and older are estimated to have dry eye, with only 17% having been diagnosed with the condition. Most patients with dry eyes are women. In the United States, it was estimated in 2000 that 14.4% of the population report symptoms of dry eyes. The prevalence increases with age: 8.4% in individuals younger than the age of 60 years and 19% in individuals older than the age of 60 years. In 2014, it is expected that there will be 20% more Medicare patients with dry eyes, and by 2010, it is anticipated that there will be 100% more Medicare patients.
The most common form of dry eyes is due to an inadequate amount of the water layer of tears. This condition, called keratoconjunctivitis sicca, is also referred to as the dry eye syndrome.
Patients suffering from the dry eye syndrome often experience:
• Dryness
• Eye pain
• Stinging or burning sensation
• Stringy discharge from the eye
• Sand in the eye; a gritty feeling
• Itching
• Redness
There are many causes of the dry eye syndrome. These include:
Gender: Women are more likely to develop dry eyes because of hormonal changes and menopause.
Environmental conditions: Exposure to pollutants such as smoke, exhaust, and smog, and arid and windy conditions can increase tear evaporation, resulting in dry eye symptoms. Failure to blink regularly, such as when staring at a computer screen for long periods, can also contribute to the dry eye syndrome. Excessive alcohol consumption is also associated with the dry eye syndrome.
Other factors: Long-term use of contact lenses can be a factor in the development of dry eyes. Refractive eye surgeries, such as laser-assisted in situ keratomileusis (LASIK),2 can cause decreased tear production and dry eyes.
Sometimes, a person with a dry eye will have excess tears running down the cheeks, which may seem confusing. This happens when the eye isn’t getting enough lubrication. The eye sends a distress signal through the nervous system for more lubrication. In response, the eye is flooded with tears to try to compensate for the underlying dryness. However, these tears are mostly watery and do not have the lubricating qualities or the rich composition of normal tears. They wash debris away, but they do not coat the eye surface properly.
Discharge
Discharge from the eye can be watery, mucoid, or purulent. A watery or mucoid discharge is often associated with allergic or viral conditions, whereas a purulent discharge occurs in association with bacterial infections. Most of the time, eye discharge is harmless. However, sometimes it can be an indication of a more serious condition. Pollen, gusty winds, dry eyes or an eyelash can cause an irritation that will lead to the discharge as well. Other, more serious causes of eye discharge can be associated with medical conditions such as conjunctivitis and corneal ulcers.
Redness
The symptom of the red eye is very common. The interviewer should ask the following questions:
“Have you had any injury to the eye?”
“Does anyone else in the family have a red eye?”
“Have you had any recent coughing spells? Vomiting?”
“Have you had any associated eye pain?”
“Does light bother your eyes?”
The eye may appear bloodshot. Redness may result from trauma, infection, allergy, or sudden increased pressure in the eye. Severe coughing spells or recurrent vomiting may cause a patient to have a subconjunctival hemorrhage. A family member or friend with viral conjunctivitis may be the source of a patient’s red eye. The combination of eye pain and red eye may indicate acute narrow-angle glaucoma, or an inflammatory condition known as scleritis or episcleritis. (Table 7-2 summarizes the differential diagnosis for the red eye.) Uveitis, inflammation of the uveal tract, which is associated with a red eye, can manifest with light sensitivity. Patients wearing contact lenses may suffer from corneal irritation and may have eye redness.
Table 7–2
Differential Diagnosis for Red Eye*
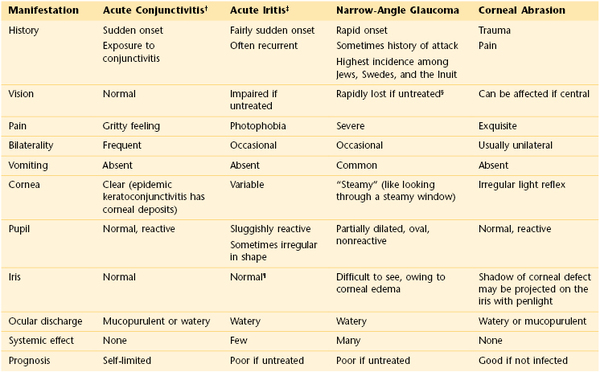
* See Figure 7-92.
† Can be viral, bacterial, or allergic.
‡ See Figure 7-67.
§ Seeing “rainbow” can be an early symptom during an acute attack.
¶ Slit-lamp examination revealing cells in anterior chamber is diagnostic.
General Suggestions
It is important to determine the medications that a patient is taking because many drugs have deleterious effects on the eye. Some antimalarial, antituberculous, antiglaucoma, and anti-inflammatory drugs can cause eye disorders. A thorough family history reveals familial disease tendencies such as glaucoma, cataracts, retinal degeneration, strabismus, or corneal dystrophies.
There are many specific symptoms related to eye disease. The common visual, nonvisual but painful, and nonvisual and painless symptoms and some possible causes are listed in Tables 7-3, 7-4, and 7-5, respectively.
Table 7–3
Common Visual Eye Symptoms and Disease States
| Visual Symptom | Possible Causes |
| Loss of vision | Optic neuritis |
| Detached retina | |
| Retinal hemorrhage | |
| Central retinal vascular occlusion | |
| Central nervous system disease | |
| Spots | No pathologic significance* |
| Flashes | Migraine |
| Retinal detachment | |
| Posterior vitreous detachment | |
| Loss of visual field or presence of shadows or curtains | Retinal detachment |
| Retinal hemorrhage | |
| Glare, photophobia | Iritis (inflammation of the iris) |
| Meningitis (inflammation of the meninges) | |
| Distortion of vision | Retinal detachment |
| Macular edema | |
| Difficulty seeing in dim light | Myopia |
| Vitamin A deficiency | |
| Retinal degeneration | |
| Colored halos around lights | Acute narrow-angle glaucoma |
| Opacities in lens or cornea | |
| Colored vision changes | Cataracts |
| Drugs (digitalis increases yellow vision) | |
| Double vision | Extraocular muscle paresis or paralysis |
* May precede a retinal detachment or may be associated with ingestion of fertility drugs.
Table 7–4
Common Nonvisual, Painful Eye Symptoms and Disease States
| Nonvisual, Painful Symptom | Possible Causes |
| Foreign body sensation | Foreign body |
| Corneal abrasion | |
| Burning sensation | Uncorrected refractive error |
| Conjunctivitis | |
| Sjögren’s syndrome | |
| Throbbing, aching | Acute iritis (inflammation of the iris) |
| Sinusitis (inflammation of the sinuses) | |
| Tenderness | Eyelid inflammation |
| Conjunctivitis | |
| Iritis | |
| Headache | Refractive errors |
| Migraine | |
| Sinusitis | |
| Drawing sensation | Uncorrected refractive errors |
Table 7–5
Common Nonvisual, Painless Eye Symptoms and Disease States
| Nonvisual, Painful Symptom | Possible Causes |
| Itching | Dry eyes |
| Eye fatigue | |
| Allergies | |
| Tearing | Emotional states |
| Hypersecretion of tears | |
| Blockage of drainage | |
| Dryness | Sjögren’s syndrome |
| Decreased secretion as a result of aging | |
| Sandiness, grittiness | Conjunctivitis |
| Fullness of eyes | Proptosis (bulging of the eyeball) |
| Aging-related changes in the lids | |
| Twitching | Fibrillation of orbicularis oculi |
| Eyelid heaviness | Fatigue |
| Eyelid edema | |
| Dizziness | Refractive error |
| Cerebellar disease | |
| Vestibular disease | |
| Excessive blinking | Local irritation |
| Facial tic | |
| Eyelids sticking together | Inflammatory disease of eyelids or conjunctivae |
Effect of Blindness on the Patient
The loss of sight is a terrifying experience. The sighted person lives mostly in a visual and auditory world illuminated by lights and colors. When blindness occurs, the person loses not only the ability to see but also their perceptual center of the world. This center must now be replaced by hearing and touch. Because light is often equated with life, the inability to see light is associated with death. The newly blinded patient must take a new place in society. He or she can no longer read ordinary books, can no longer receive visual stimuli, and is unable to appreciate the world of visual communication. This can result in a reactive depression. The clinician must show genuine care for blind patients and try to understand their feelings of discouragement and despair.
The person who is blind from birth or early childhood has little or no conception of the visual world. Having never been able to see, this patient has no visual frame of reference.
On occasion, a blind individual recovers sight as a result of a surgical procedure later in life. Many difficulties may arise owing to the reorganization of the patient’s perception. His or her frame of reference has been shifted from touch to sight. Surprisingly, many of these patients become depressed after attaining vision. Facial expressions mean nothing because only with experience can people understand them. The following quote from a case history by Gregory and Wallace illustrates the response of such an individual:
He suffered one of the greatest hardships (blindness) and yet he lived with energy and enthusiasm. When his handicap was apparently swept away, as by a miracle, he lost his peace and self-respect.
Similarly, the patient with normal vision may develop psychosomatic eye problems as a result of anxiety. Loss of vision also can accompany panic disorders. Such individuals can have either partial or complete vision loss in one or both eyes. Supportive care of the primary problem usually results in the return of vision.
In multiple sclerosis, one of the presenting symptoms may be the sudden onset of blindness caused by optic neuritis. This blindness in most cases reverses completely, in approximately 6 weeks. This is a very frightening experience for a typically young patient.
Physical Examination
The equipment necessary for the examination of the eye is as follows: an ophthalmoscope, a penlight, a pocket visual acuity card, and a 3 × 5 inch (7.6 × 12.7 cm) card.
The physical examination of the eye includes the following:
Visual Acuity
Visual acuity is expressed as a ratio, such as 20/20. The first number is the distance at which the patient reads the chart. The second number is the distance at which a person with normal vision can read the same line of the chart. Another way of describing visual acuity is as follows: if a person has 20/20 vision, that person has 20/20 or 100% vision because 20 divided by 20 equals 1 or 100% of normal vision. The abbreviation OD refers to the right eye; OS refers to the left eye; OU refers to both eyes.3
Using the Standard Snellen Chart
If a standard Snellen eye chart is available, the patient should stand 20 feet from the chart. If the patient wears glasses for distance, he or she should wear them for the examination. The patient is asked to cover one eye with the palm4 or an index card and read the smallest line possible. If the best he or she can see is the 20/200 line, the patient’s vision in that eye is 20/200; this means that at 20 feet, the patient can see what a person with normal vision can see at 200 feet. This can also be explained as 10% of normal vision in that eye. If a patient at 20 feet cannot see the 20/200 line, he or she is moved closer until the letters are recognized. If the patient can read these letters at 5 feet, the patient’s visual acuity in that eye is 5/200.
Using a Pocket Visual Acuity Card
If the standard Snellen chart is not available, a pocket visual acuity card is helpful. This is viewed at 14 inches (35.6 cm). The patient is again asked to read the smallest line possible. If neither eye chart is available, any printed material may be used. The examiner should remember that most patients older than 40 years require reading glasses. Although visual acuity cannot be quantified, the examiner can certainly determine whether the patient has any vision. In such a case, the patient is asked to cover an eye and read the smallest line possible on a given printed page.
Evaluation of Patients with Poor Vision
Patients with poor vision who are unable to read any lines of print should be tested for finger-counting ability. This crude measurement of visual acuity is obtained by the examiner’s holding up fingers in front of one of the patient’s eyes with the other eye covered. The patient is then asked how many fingers are seen. If the patient is still unable to see, the next step would be to evaluate whether he or she has any light perception. This is performed by covering one eye and directing a light at the eye in question. The examiner asks the patient whether he or she can see when the light is on and off. No light perception is the term used when a person cannot perceive light.
Evaluation of Patients Who Cannot Read
For individuals who cannot read, such as young children or illiterate patients, the use of the letter “E” in different sizes and directions is helpful. The examiner asks the patient to point in the direction of the letter: up, down, right, left.
Visual Fields
Visual field testing is useful for determining lesions of the visual pathway. Many techniques are used for this purpose. The examiner should learn to perform the technique known as confrontation visual field testing. In this technique, the examiner compares his or her peripheral vision with that of the patient.
Assess Fields by Confrontation Testing
The examiner stands or sits 3 feet in front of and at eye level with the patient. The patient is asked to close the right eye while the examiner closes his or her own left eye, each fixating on the other’s nose. The examiner holds up fists with the palms facing him or her. The examiner then shows one or two fingers on each hand simultaneously and asks the patient how many fingers he or she sees. The hands are moved from the upper to the lower quadrants, and the examination is repeated. The examination is then repeated, with the other eye of the patient and that of examiner. The fingers should be seen by both patient and examiner simultaneously. To position the patient to better advantage, the hands are held up slightly closer to the examiner. This provides a wider field for the patient. If the examiner can see the fingers, the patient can see them unless he or she has a field deficit. This technique for examining the patient’s left eye is shown in Figure 7-10.
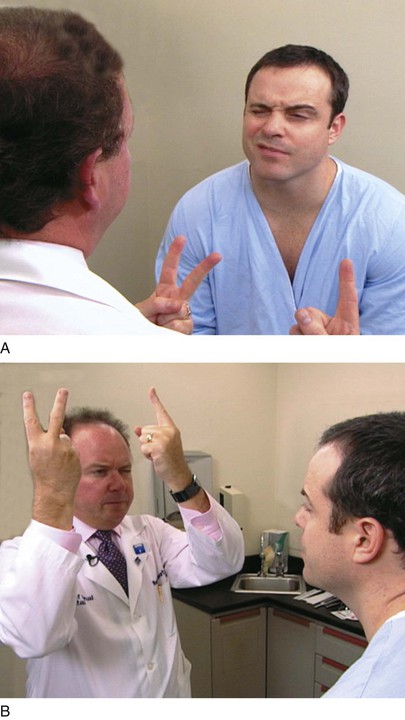
Figure 7–10 Confrontation visual field testing. A, View of the patient during examination of the lower fields of the patient’s left eye. B, Position of the examiner during examination of the upper fields of the patient’s left eye.
Because lesions along the visual pathway develop insidiously, the patient may not be aware of any changes in visual fields until late in the course of the disease. Confrontation fields, performed by the internist, may provide the first objective evidence that the patient has a lesion involving the visual pathway. An area of depressed vision is called a scotoma.
The normal central vision extends approximately 30 degrees in all directions of central fixation. The blind spot is the physiologic scotoma located approximately 15 to 20 degrees temporal to central fixation, corresponding to the optic nerve head. No sensory elements such as the rods or cones are located on the nerve head.
Assess Visual Field Abnormalities
Pathologic scotomata may be appreciated on visual field testing. Scotomata may result from primary ocular disease, such as glaucoma, or from lesions in the central nervous system, such as tumors. Figure 7-11 illustrates some of the common defects.
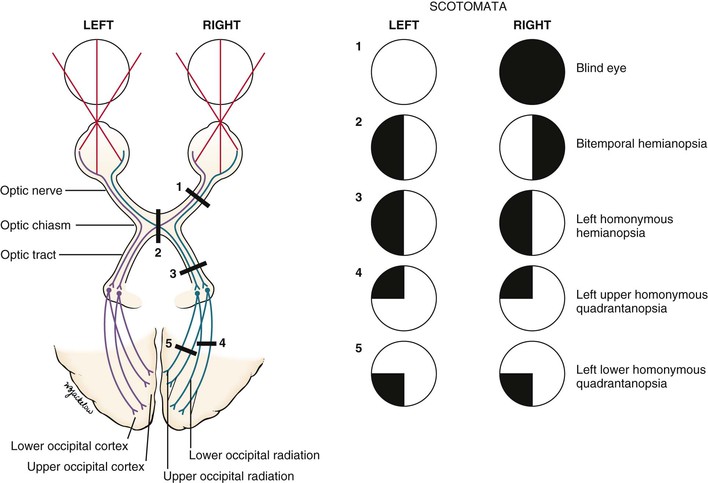
Figure 7–11 Visual field defects.
Total loss of vision in one eye constitutes a blind eye, resulting from a disease of the eye or a lesion of its optic nerve.
Hemianopsia refers to absence of half of a visual field. A defect in both temporal fields is termed bitemporal hemianopsia. It results from a lesion involving the optic nerves at the level of the optic chiasm. Pituitary tumors are common causes.
A homonymous hemianopsia results from damage to the optic tract, optic radiation, or occipital cortex. The term homonymous indicates that the visual loss is in similar fields. A patient with a left homonymous hemianopsia is unable to see the left half of the fields of both eyes. This defect occurs with damage to the right optic tract. Homonymous hemianopsia is the most common form of field loss and occurs frequently in patients with strokes.
A quadrantanopsia is a field loss in one quadrant, also known as a “pie in the sky” lesion. A patient with a left upper homonymous quadrantanopsia has damage to the right lower optic radiations or the right lower occipital region. Tunnel vision may occur in advanced glaucoma. However, the visual fields enlarge with increasing testing distance, in contrast to hysterical blindness, in which the field size typically remains the same at all times, regardless of the testing distance.
Assess Optokinetic Nystagmus
On occasion, a patient may feign blindness. They may be trying to qualify for disability insurance or some other issue of secondary gain. Alternately, they may have psychological issues. A useful test for ruling out such malingering involves optokinetic nystagmus (OKN). OKN is the rapid alternating motion of the eyes that occurs when the eyes try to fixate on a moving target. For example, observe the eyes of a person riding a train as it enters the station. The eyes move rapidly back and forth as the person tries to fixate on a station sign. The presence of OKN indicates physiologic continuity of the optic pathways from the retina to the occipital cortex. OKN may be elicited in the examining room by having the patient fixate on the numbers on a tape measure while you rapidly pull out the tape. Because OKN is involuntary, a positive response5 provides excellent verification that the patient is feigning blindness.
Ocular Movements
Ocular movements are effected by the contraction and relaxation of the extraocular muscles. This results in simultaneous movement of the eyes up or down or from side to side, as well as in convergence.
Assess Eye Alignment
Alignment of the eyes is seen by observing the location of reflected light on the cornea. The penlight should be held directly in front of the patient. If the patient is looking directly at the penlight, the light reflex should be in the center of each pupil. If the light falls in the pupillary center of one eye but is displaced away from the pupillary center in the other eye, deviation of the eye may exist.
The condition of a deviated, or crossed, eye is called strabismus, or tropia. Strabismus is the nonalignment of the eyes in such a way that the object being observed is not projected simultaneously on the fovea of each eye. Esotropia is deviation of an eye nasally; exotropia is deviation of an eye temporally; hypertropia is deviation upward. An alternating tropia is the term used to describe the condition in which either eye deviates. Figure 7-12 shows a patient with a left exotropia.
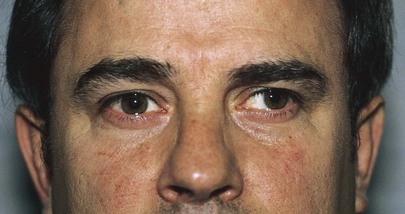
Figure 7–12 Left exotropia.
Perform the Cover Test
The cover test is useful for determining whether the eyes are aligned (if a deviated eye is present). The patient is instructed to look at a distant target. One eye is covered with a 3 × 5 inch (7.6 × 12.7 cm) card. The examiner should observe the uncovered eye. If the uncovered eye moves to take up fixation of the distant point, that eye was not straight before the other eye was covered. If the eye did not move, it was straight. The test is then repeated with the other eye.
Evaluate the Six Diagnostic Cardinal Positions of Gaze
An important cause of a deviated eye is a paretic (weak), or paralyzed, extraocular muscle or muscles. Paralysis of these muscles is detected by examination of the six diagnostic positions of gaze.
Because the rotational actions of the oblique and vertical rectus muscles cannot be easily assessed, the eye must be moved into six diagnostic gaze positions that best isolate the vertical actions of these muscles to test their innervations. The oblique muscles are tested in adduction to maximize their vertical action. In contrast, the vertical rectus muscles are tested in abduction; in these positions, the superior rectus acts now as a pure elevator and the inferior rectus as a pure depressor. These diagnostic cardinal positions of gaze are the testing positions for the muscles, and the abduction and adduction testing movements are different from the normal actions of the muscles as indicated in Table 7-1.
Hold the patient’s chin steady with your left hand, and ask the patient to follow your right hand as it traces a large H in the air. Hold your right index finger approximately 15 to 18 inches (38 to 46 cm) from the patient’s nose. From the midline, move your finger approximately 12 inches (30 cm) to the patient’s left and pause; then up approximately 8 inches (20 cm) and pause, as shown in Figure 7-13; down approximately 16 inches (40 cm) and pause; up approximately 8 inches (20 cm); and then slowly back to the midline. Switch your hands, now holding the patient’s chin with your right hand. Cross the midline and repeat the finger movements on the other side. These are the six diagnostic cardinal positions of gaze. Observe the movement of both eyes, which should follow the finger smoothly. Look for the parallel movements of the eyes in all directions.
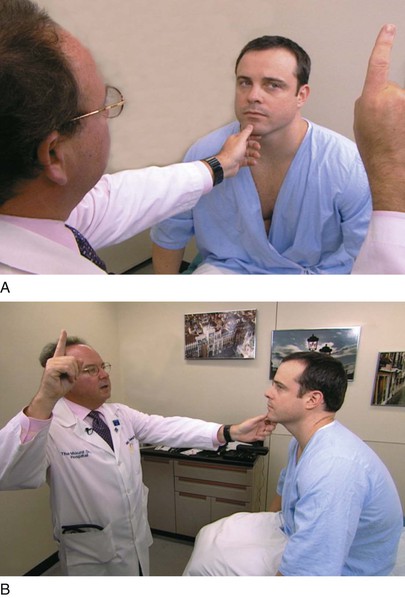
Figure 7–13 A and B, Technique for testing ocular motility.
On occasion, when looking to the extreme side, the eyes develop a rhythmic motion called end-point nystagmus. There is a quick motion in the direction of gaze, which is followed by a slow return. This test differentiates end-point nystagmus from pathologic nystagmus, in which the quick movement is always in the same direction, regardless of gaze.
If the eye and eyelid do not move together, lid lag is present.
The six diagnostic cardinal positions of gaze, with the related muscles, are illustrated in Figure 7-14, and Table 7-6 summarizes the abnormalities in ocular motility that are caused by paretic muscles.
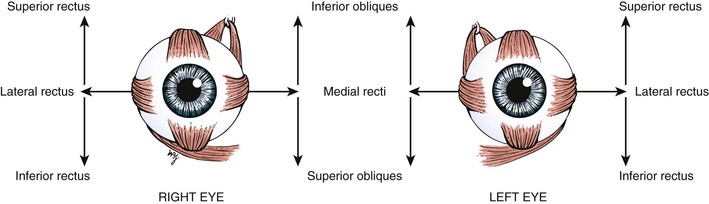
Figure 7–14 Diagnostic positions of gaze.
Table 7–6
Paretic Muscles Causing Abnormal Ocular Motility
| Paretic Muscle | Position to Which Eye Will Not Turn |
| Medial rectus | Nasal |
| Inferior oblique | Up and nasal |
| Superior oblique | Down and nasal |
| Lateral rectus | Temporal |
| Superior rectus | Up and temporal |
| Inferior rectus | Down and temporal |
The images projected on the retina may be interpreted by the brain in one of three ways: fusion, diplopia, or suppression. Fusion and diplopia have already been discussed. In children, strabismus leads to diplopia, which leads to confusion and then suppression of the image and finally to amblyopia. Amblyopia is the loss of visual acuity secondary to suppression. Amblyopia is reversible until the retinas are fully developed, at approximately the age of 7 years. Amblyopia is a phenomenon that occurs only in children. An adult who acquires strabismus secondary to a stroke, for example, cannot suppress the deviated eye’s image and will experience diplopia, which is intolerable.
Evaluate the Pupillary Light Reflex
Ask the patient to look in the distance while you shine a bright light in the patient’s eye. The light source should come from the side, with the patient’s nose acting as a barrier to light to the other eye. Observe both the direct and consensual pupillary responses. Then repeat the test on the other eye.
The swinging light test is a modification for testing the pupillary light reflex. This test reveals differences in the response to afferent stimuli of the two eyes. The patient fixates on a distant target while the examiner rapidly swings a light from one eye to the other, observing for constriction of the pupils. In some conditions, there is a paradoxical dilatation of the pupil on which the light is shined. This condition, called a Marcus Gunn defect or relative afferent pupillary defect (RAPD), is associated with an afferent limb defect in the eye being illuminated.
The most extreme example of an eye displaying the Marcus Gunn, or RAPD, phenomenon is a blind eye. When light is shined into the blind eye, there is neither a direct nor a consensual response. When the light is moved to the other eye, there is both a direct and a consensual response because both afferent and efferent pathways are normal. When the light is swung back to the blind eye, no impulses are received by the retina (afferent), and the pupil of the blind eye no longer remains constricted; it therefore dilates. There are different degrees of severity of Marcus Gunn pupils, depending on the involvement of the optic nerve.
Evaluate the Near Reflex
The near reflex is tested by having the patient look first at some distant target and then at a target placed approximately 5 inches (13 cm) away from his or her nose. When the patient focuses on the near target, the eyes should converge, and the pupils should constrict.
External and Internal Eye Structures
The examination of the external and internal eye structures includes the following:
Inspect the Orbits and Eyelids
Are the globes present in the orbits? An enucleation of his left eye is pictured in Figure 7-15. The removal of the entire globe from the orbit may be caused by trauma, surgery (as in the case of a ruptured globe), or self-induced injury by a psychotic person. Rarely one may see a case of congenital anophthalmos.

Figure 7–15 Enucleation of left eye.
Examine the eyelids for evidence of drooping, infection, erythema, swelling, crusting, masses, or other abnormalities. Have the patient open and close the eyelids. The motion should be smooth and symmetric. Do the eyes close completely?
Note the position of the eyelids. When the eye is open, the upper eyelid normally covers only the upper margin of the iris. When the eye is closed, the eyelids should approximate each other completely. The space between the upper and lower lids is the palpebral fissure. Drooping of the eyelid is known as blepharoptosis, or ptosis. Figure 7-16 depicts marked bilateral ptosis, causing narrowing of the palpebral fissure that resulted from a muscle-weakening disorder, myasthenia gravis.

Figure 7–16 Bilateral ptosis.
Figure 7-17 shows a patient with Kearns-Sayre syndrome, also known as chronic progressive external ophthalmoplegia. In this autosomal-dominant condition, there is a slowly progressive, symmetric ptosis and symmetric external ophthalmoplegia (weakness of the external eye muscles). The syndrome also is associated with retinal pigmentary degeneration and cardiac conduction defects such as complete heart block. Affected patients are frequently of short stature and may be deaf. In the patient shown in Figure 7-17, notice the arching of the brows in an effort to lift the eyelids to reduce the ptosis.
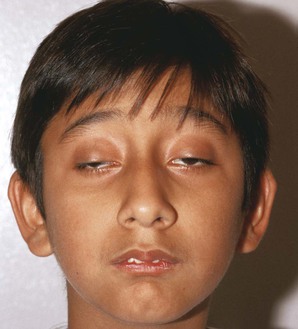
Figure 7–17 Kearns-Sayre syndrome.
Lagophthalmos is a condition, pictured in Figure 7-18, in which there is an inability to close the eyelids completely. It is seen in thyroid disease secondary to orbital infiltration caused by inflammation, as a result of autonomic stimulation, or as a consequence of ocular surgery. The name comes from the Greek word lagos, meaning “hare,” an animal believed to sleep with its eyes open.

Figure 7–18 Lagophthalmos.
Figure 7-19 shows a patient with an entropion. An entropion is a turning inward of the lid margin in such a way that the eyelashes abrade the cornea and globe. An ectropion is a turning outward of the eyelid margin. An ectropion is pictured in Figure 7-20. Both entropions and ectropions may be seen as involutional changes associated with aging and may be associated with the dry eye syndrome.
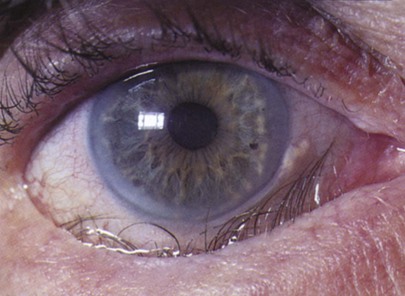
Figure 7–19 Entropion.
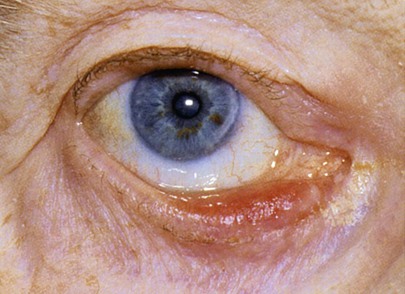
Figure 7–20 Ectropion.
A common benign lesion of the eyelid is a marginal intradermal nevus, shown in Figure 7-21. Such lesions are well differentiated, and hairs commonly grow from them. One of the associated problems is that these hairs may scratch the cornea, causing corneal abrasions like those caused by entropions.

Figure 7–21 Marginal nevus of upper eyelid.
A cutaneous horn is a clinical diagnosis referring to a conical projection above the surface of the skin that resembles a miniature horn. The base of the horn may be flat, nodular, or crateriform. The horn is composed of compacted keratin. Cutaneous horns usually arise on sun-exposed skin but can occur even in sun-protected areas. More than half of all cutaneous horns are benign. Malignancy at the base of the horn, however, is present in up to 20% of cases, with squamous cell carcinoma being the most common type. No clinical features reliably distinguish between benign and malignant lesions. Tenderness at the base and lesions of larger size favor malignancy. Figure 7-22A shows a patient with a cutaneous horn on the medial aspect of the left upper eyelid. Figure 7-22B shows a close-up of the cutaneous horn. Figure 7-23 shows another patient with a cutaneous horn above her left eyebrow.
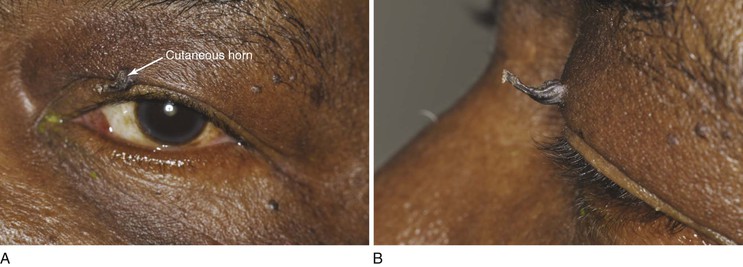
Figure 7–22 Cutaneous horn. A, Patient’s left eye with horn on medial aspect of upper eyelid. B, Close-up of lesion.

Figure 7–23 Cutaneous horn over left eyebrow.
Molluscum contagiosum is a viral infection, caused by a member of the poxvirus family, that causes raised, pearl-like, umbilicated (dimpled) papules on the skin. In most people, the growths range from about the size of a pinhead to as large as a pencil eraser (2 to 5 mm in diameter). This is a common infection in children and occurs when a child comes into direct contact with a lesion. It is frequently seen on the face, neck, armpit, arms, and hands but may occur anywhere on the body except the palms and soles. The virus can spread through contact with contaminated objects, such as towels, clothing, or toys. The virus also spreads by sexual contact. Early lesions on the genitalia6 may be mistaken for herpes or warts but, unlike herpes, these lesions are painless. Persons with an impaired immune system, such as patients with acquired immune deficiency syndrome (AIDS), may have a significantly worse case of molluscum contagiosum. Figure 7-24 shows a patient with molluscum contagiosum around the eye. Note the umbilicated lesions in this figure as well as in Figure 15-37.

Figure 7–24 Molluscum contagiosum. Note the umbilicated (dimpled) lesions; one example is indicated.
A common ocular occurrence of aging is herniation of the orbital fat, caused by progressive thinning of the orbital septum, allowing orbital fat to move forward and resulting in puffy areas around the globe. Figure 7-25 shows an example of herniated orbital fat. Note the unrelated old corneal scars and the arcus senilis, discussed later in this chapter.

Figure 7–25 Herniated orbital fat.
Figure 7-26 depicts a small hemangioma of the lower eyelid. Sturge-Weber syndrome is a congenital condition recognizable by a characteristic port wine stain, or nevus flammeus, on one side of the face that follows the distribution of one or more of the divisions of the trigeminal nerve. Hemangiomas may develop on the episclera, iris, ciliary body, and choroid. Unilateral glaucoma develops frequently on the affected side if there is extensive involvement of the eye with a uveal hemangioma. These patients should be screened for glaucoma early. Figure 7-27 shows a patient with Sturge-Weber syndrome. Notice the sharply demarcated patch of the hemangioma with the involvement of the ophthalmic and maxillary divisions of the left trigeminal nerve. The lesion, which does not blanch on pressure, tends to darken with age from red to purple (see also Fig. 21-7).

Figure 7–26 Hemangioma of lower eyelid.

Figure 7–27 Sturge-Weber syndrome.
A chalazion is a granulomatous reaction to inspissated secretions of the meibomian glands in the eyelid. It is caused by a blocked duct in one of the glands. These glands are aligned vertically in the eyelids perpendicular to the lid margin. The openings of these glands are located on the eyelid margin directly behind the eyelashes. The glands, which number approximately 30 in the upper lid and 20 in the lower lid, produce a thin, oily fluid that lubricates the eye. A chalazion may appear as a localized mass on the eyelid near the orifice of the gland, painful at first, but usually painless when chronic. Figure 7-28A shows a patient with a chalazion; Figure 7-28B illustrates the position of the meibomian glands on the lids. Figure 7-29 shows a patient with bilateral chalazions. A chalazion will often disappear without treatment within a month or so. The initial treatment is to place very hot, but not burning,7 compresses over the eyelid for 10 to 15 minutes at least 4 times a day. This tends to soften the hardened oils blocking the duct, and promote drainage and healing. Figure 7-30A shows another patient with a chalazion; Figure 7-30B shows the same patient with the lid everted. Note the chalazion distorting the lid margin and the granuloma formed on the lower inner eyelid at the proximal end of the meibomian gland.
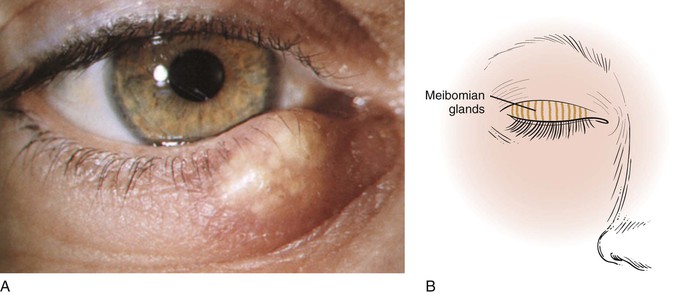
Figure 7–28 A, Chalazion. B, This illustration shows the position of the meibomian glands on the eyelids.

Figure 7–29 Bilateral chalazions.
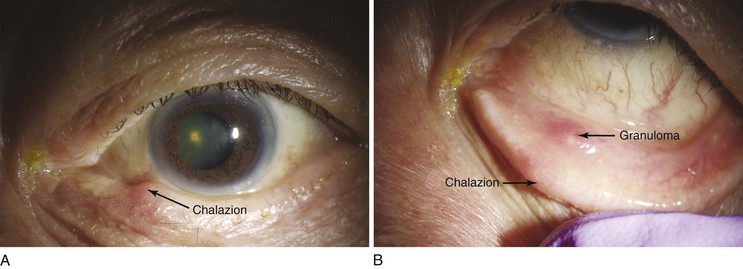
Figure 7–30 Chalazion. A, Note the lesion on the lower eyelid. B, Close-up of the lesion with the eyelid everted. Note the chalazion distorting the lid margin and the granuloma formed on the lower inner eyelid at the proximal end of the meibomian gland.
In herpes zoster ophthalmicus, rows of vesicles, ulcers, and crusted scabs are scattered along the course of one or more of the branches of the ophthalmic division of the trigeminal nerve. The vesicles contain clear fluid. These rupture, leaving ulcers that can become infected secondarily and form crusts. The eyelids become edematous and red. Pain can be excruciating. Ophthalmoplegia secondary to involvement of the extraocular muscles may also occur. Figure 7-31 shows a patient with AIDS and herpes zoster ophthalmicus at different stages of evolution (fresh and crusted vesicles) in the ophthalmic division of the trigeminal nerve. Treatment with antivirals will dramatically reduce the symptoms.

Figure 7–31 Herpes zoster ophthalmicus.
Is orbital discoloration present? One type of orbital pigmentation known as raccoon eyes is an important sign of a basilar skull fracture. This discoloration is caused by extravasated blood from the fracture of the base of the brain. This is an important sign to recognize, especially in an unconscious patient, when a history is not available. Figure 7-32 shows a patient with a basilar skull fracture. Notice also the subconjunctival hemorrhages on the lateral aspects.
Inspect the eyelids for xanthelasma. Although not specific for hypercholesterolemia, these yellowish plaques are commonly associated with lipid abnormalities and are caused by lipid deposition in the periorbital skin. Xanthelasma is shown in Figure 7-33.

Figure 7–33 Xanthelasma.
A stye, or acute external hordeolum, is a localized abscess in an eyelash follicle and is caused by a staphylococcal infection. It is a painful, red infection that looks like a pimple pointing on the lid margin where the hair follicle of the eye lash or cilia is situated. Figure 7-34 depicts a stye. Blepharitis is a chronic inflammation of the eyelid margins. The most common form is associated with small white scales around the lid margin and the eyelashes, which stick together and may fall out. There are several annoying symptoms: itching, tearing, and redness. The condition is frequently associated with seborrheic dermatitis and acne rosacea. Figure 7-35 shows a patient with blepharitis.

Figure 7–34 Stye.

Figure 7–35 Blepharitis.
Malignant tumors of the eyelids are not uncommon. Characteristics suggesting malignancy include:
Carcinoma of the eyelids has the highest incidence of any malignant ocular tumor. Men are more commonly affected than women; the average age at onset is 50 to 60 years. Of all eyelid carcinomas, 95% are of the basal cell type. The location of basal cell carcinomas are on the lower eyelid (50–60%), medial canthus (25–30%), upper eyelid (15%), and lateral canthus (5%). Figure 7-36 shows a basal cell carcinoma of the lower lid. The lesion begins growing slowly and painlessly, eventually forming the typical rodent ulcer with a raised border and an indurated base. The tumor erodes the surrounding area, forming the ulcer. Note the raised border of the lesion in Figure 7-36.
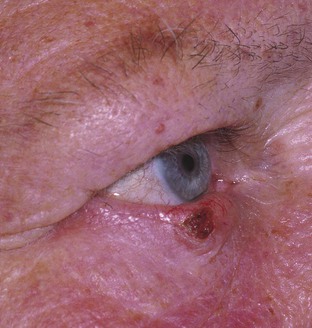
Figure 7–36 Basal cell carcinoma of the eyelid.
The remaining 5% consist of squamous cell carcinomas and meibomian gland carcinomas. Squamous cell carcinomas are 40 times less common than basal cell carcinomas and tend to be on the upper eyelid and grow faster than basal cell carcinomas. Early ulceration is common. A squamous cell carcinoma of the eyelid is shown in Figure 7-37. The base and edges of the ulcer are hard and hyperemic.
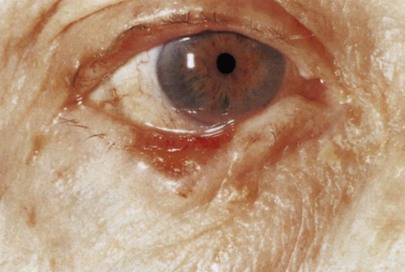
Figure 7–37 Squamous cell carcinoma of the eyelid.
Malignant melanomas are less then 1% of all malignant tumors of the eyelid.
The most common ocular manifestation of AIDS affecting the eyelids is lesions of Kaposi’s sarcoma. The initial manifestation may be subtle and may be mistaken for blepharitis or a chalazion. Refer to Figure 5-100C, which shows a patient with AIDS and Kaposi’s sarcoma of the eyelid.
Inspect the Lacrimal Apparatus
In general, there is little to be seen of the lacrimal apparatus, with the exception of the punctum. If tearing, also known as epiphora, is present, there may be some obstruction to flow through the punctum. If excessive moisture is present, check for a blockage of the nasolacrimal duct by pressing the lacrimal sac gently against the inner orbital rim. If a blockage is present, material may be expressed through the punctum. Figure 7-38 shows massive lacrimal gland enlargement as a result of sarcoidosis.
Figure 7-39 shows marked bilateral proptosis of the globe in a patient with hyperthyroidism. Note the massive lacrimal gland enlargement.
Dacryocystitis is a term describing the inflammation of the lower lacrimal passages usually seen in infants or older individuals. The causes include congenital anomalies, infection, and stenosis of the lacrimal duct. Chronic dacryocystitis, seen in Figure 7-40, is a common disorder and almost always arises secondary to ductal obstruction.
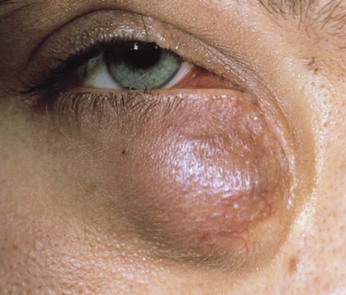
Figure 7–40 Chronic dacryocystitis.
Inspect the Conjunctiva
The conjunctivae should be examined for signs of inflammation (i.e., injection caused by dilatation of its blood vessels), pallor, unusual pigmentation, swelling, masses, and hemorrhage.
The tarsal conjunctiva may be seen by everting the eyelid. Ask the patient to keep the eyes open and look downward. Grasp gently some of the eyelashes of the upper lid. Pull the eyelid away from the globe, and press the tip of an applicator stick against the upper border of the tarsal plate. Then quickly turn the tarsal plate over the applicator stick, using it as a fulcrum. Your thumb can now be used for holding the everted lid, and the applicator stick can be removed. After inspection of the tarsal conjunctiva, have the patient look up to return the lid to its normal position.
The normal conjunctiva is transparent. Note the number of blood vessels. Normally, only a small number of vessels are seen. Ask the patient to look up, while you pull down on the lower eyelids. Compare the vascularity in the two eyes.
Conjunctivitis is the most common of all eye diseases in the Western hemisphere. The causes are numerous: bacterial, viral, chlamydial, fungal, parasitic, spirochetal, allergic, traumatic, chemical, and idiopathic. Bacterial conjunctivitis is the most frequent type and is self-limited, lasting 10 to 14 days. Figure 7-41 shows acute hemorrhagic conjunctivitis. This highly contagious ocular infection, often bilateral, is caused by the enteroviruses (members of the picornavirus family), Pneumococcus organisms, and Haemophilus influenzae. Giant papillary conjunctivitis is an ocular syndrome consisting of excessive secretion of conjunctival mucus, itching, and the development of giant papillae (1 mm or more in diameter) on the tarsal conjunctiva. This syndrome occurs mostly in patients who wear soft contact lenses, but it can occur in patients with ocular prostheses or other foreign bodies in the eye. Figure 7-42 shows a patient with giant papillary conjunctivitis.
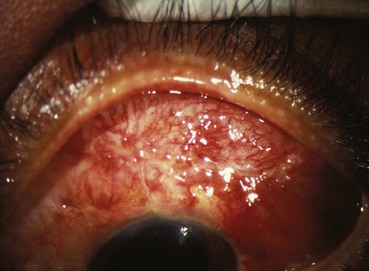
Figure 7–41 Acute hemorrhagic conjunctivitis.
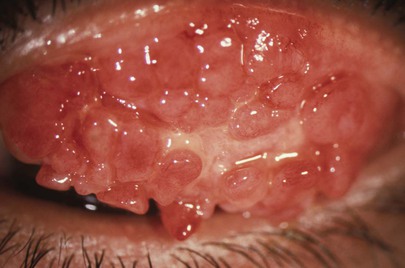
Figure 7–42 Giant papillary conjunctivitis.
Figure 7-43 shows a large subconjunctival hemorrhage. This common condition may occur spontaneously, usually in only one eye, in any age group. Because of its sudden appearance and bright red color, the patient may become alarmed. The hemorrhage is usually caused by a rupture of a small conjunctival vessel after a bout of severe coughing or sneezing. Occasionally, a subconjunctival hemorrhage may occur as a consequence of elevated blood pressure. There is no treatment, and the hemorrhage resolves within 1 to 2 weeks.

Figure 7–43 Subconjunctival hemorrhage.
The conjunctiva is attached to the episclera by loose connections. This potential space can easily be filled with fluids such as blood or serum. Chemosis is the presence of fluid in this space. Trauma, allergies, and chronic exposure, as seen in proptosis of hyperthyroidism and neurologic deficits, are important causes of chemosis. Figure 7-44 shows chemosis secondary to hay fever. An example of hemorrhagic chemosis is pictured in Figure 7-45. The patient, a 42-year-old man, had a 7-year history of progressive proptosis secondary to a melanoma.

Figure 7–45 Hemorrhagic chemosis.
Two common benign growths on the conjunctiva are the pinguecula and pterygium. A pinguecula is a whitish-yellow, triangular, nodular growth on the bulbar conjunctiva adjacent to the corneal-scleral junction (limbus), as seen in Figure 7-46; it does not cross on to the cornea. A pterygium is a more vascular growth on the bulbar conjunctiva that begins at the medial canthus and extends beyond the corneal-scleral junction to the cornea. This typically triangle-shaped fibrovascular connective tissue may cause astigmatism or even decreased vision if it extends toward or occludes the pupillary margin. The cause of the pterygium is thought to be chronic dry eyes because its frequency is higher among people living near the equator. Figure 7-47A shows a pterygium; Figure 7-47B is a close-up photograph of a pterygium in another patient. Notice the vascularity and their positions across the limbus.
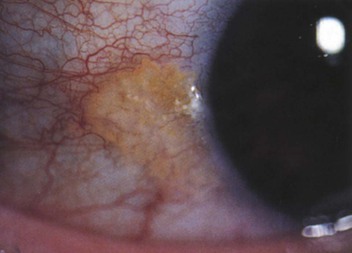
Figure 7–46 Pinguecula.
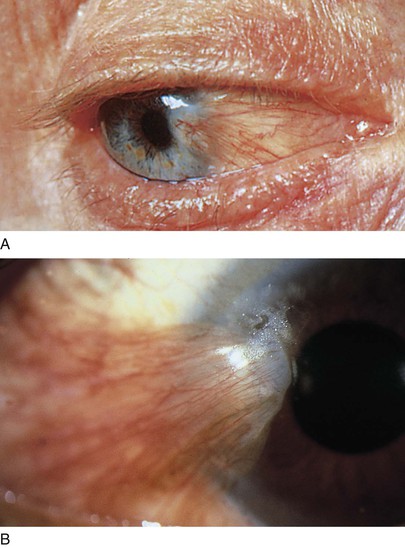
Figure 7–47 A and B, Pterygium. B, A close-up view.
Primary acquired melanosis is a unilateral condition in which melanotic pigmentation develops in the conjunctival or corneal epithelium. It starts insidiously during middle age. A biopsy is often needed to rule out a malignant melanoma. Figure 7-48 shows primary acquired melanosis. Primary acquired melanosis of the plica semilunaris in another patient is seen in Figure 7-49.
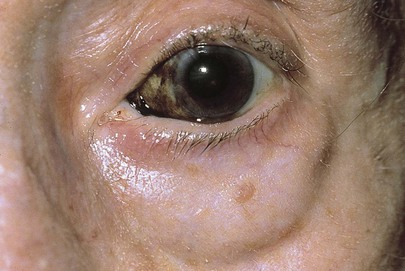
Figure 7–48 Primary acquired melanosis.
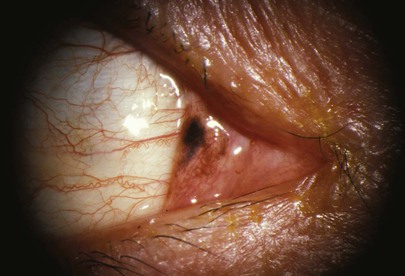
Figure 7–49 Primary acquired melanosis.
A benign pigmented tumor of the conjunctiva may be a conjunctival nevus. This is a solitary, well-defined, slightly elevated lesion. Nevi have a predilection for the limbus, plica semilunaris, caruncle, and lid margin. Most nevi are tan or brown, and many have zones of clearing within known as lacunae. Figure 7-50 shows a patient with a conjunctival nevus.

Figure 7–50 Conjunctival nevus.
A dermolipoma of the conjunctiva is a common congenital tumor, often bilateral, that usually appears as a smoothly rounded growth in the superotemporal quadrant of the bulbar conjunctiva near the lateral canthus. Figure 7-51A shows bilateral dermolipomas of the conjunctiva. A close-up of the lesion in the right eye is shown in Figure 7-51B. The yellowish color is secondary to the increased fatty deposits in the lesion. Often, fine hairs may protrude from its surface. Treatment is usually not indicated.
Inspect the Sclera
The sclera is examined for nodules, hyperemia, and discoloration. The normal sclera is white. In dark-skinned individuals, the sclera may be slightly brownish in color because of pigment migration.
Jaundice, or icterus, is a yellowish discoloration of the sclera, skin, and mucous membranes, and is caused by retention of bilirubin or its products of metabolism. Jaundice is more easily seen in the sclera of white individuals and may be missed in people of color or in dim light. Ingestion of too much carotene-containing foods, carotenoids, may cause yellowing of the skin but not of the sclera (see Fig. 14-5). Many foods are associated with high levels of carotenoids; these include carrots, sweet potatoes, tomatoes, asparagus, yellow corn, cheese, mustard, oranges, papayas, peaches, pineapple, pumpkin, and many more.
The sclera may appear bluish, normally in infants or pathologically in osteogenesis imperfecta. Osteogenesis imperfecta is a group of hereditary disorders with bone fragility. Individuals with these disorders may suffer bone fractures after mild trauma. The autosomal dominant form is most widely recognized. In this form, the sclerae are very thin and take on a blue hue because the uveal pigment shows through the sclera. Deafness is also seen in this form of the disorder. Figure 7-52 shows blue sclerae in a patient with osteogenesis imperfecta.
Episcleritis is a benign, usually painless, commonly recurring disorder frequently affecting both eyes of young adults, more commonly women. It is a noninfectious inflammation that is subconjunctival and yet superficial to the underlying sclera. The affected area may be either flat and diffuse or localized and nodular (1 to 4 mm in diameter). Although the cause in most cases is unclear, episcleritis also occurs in patients with inflammatory bowel disease, herpes zoster, collagen vascular disease, gout, syphilis, and rheumatoid arthritis. Figure 7-53 shows the classic features of episcleritis.

Figure 7–53 Episcleritis.
Scleritis is a painful, often bilateral, recurrent disorder, less common than episcleritis, that affects older age groups and occurs in women more often than in men. There is inflammation of the sclera with possible involvement of the cornea, uveal tract (i.e., iris, choroid, and ciliary body), or retina. Photophobia is common. Scleritis is usually related to a systemic disorder. It occurs much more commonly in patients with connective tissue disorders. It may be diffuse or localized and nodular. Nodular scleritis is marked by dark localized blue patches in the anterior portion of the sclera; these are seen because the choroid is visible through the translucent sclera. The condition may resolve spontaneously. Figure 7-54 shows nodular scleritis.
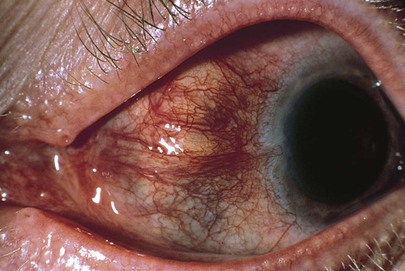
Figure 7–54 Nodular scleritis.
Scleromalacia perforans is an uncommon, painless scleral condition characterized by the appearance of one or more dehiscences in the sclera in the absence of inflammatory changes. This necrotizing scleritis without inflammation is classically seen in patients with long-standing rheumatoid arthritis. The underlying uvea is often visible, and it may bulge out, as shown in Figure 7-55. Another example of scleromalacia perforans is shown in Figure 7-56. Notice the thinning of the sclera and the underlying dark uvea, as well as the irregular border of the iris. Anterior synechiae are present, holding the iris down to the lens and causing the scalloped appearance of the iris. There is corneal disease as well.
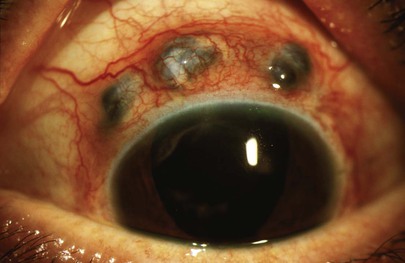
Figure 7–55 Scleromalacia perforans.
Inspect the Cornea
The cornea should be clear and without cloudiness, ulceration, or opacities.
A whitish ring at the perimeter of the cornea is probably an arcus senilis. In patients older than 40 years, this finding is usually a normal phenomenon. Although there are many false-positive findings, patients younger than 40 years may have hypercholesterolemia. An arcus senilis is seen in Figures 7-57 and 7-58.

Figure 7–57 Arcus senilis.
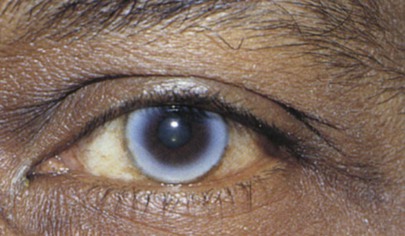
Figure 7–58 Arcus senilis.
An abnormal golden to greenish-brown ring near the limbus, most evident superiorly and inferiorly, is a Kayser-Fleischer ring. This ring is a specific and sensitive sign of Wilson’s disease, which is hepatolenticular degeneration as a result of an inherited disorder of copper metabolism. Approximately 95% of patients with Wilson’s disease who present with neurologic signs will have a Keyser-Fleischer ring. This ring is caused by deposition of copper in Descemet’s membrane of the peripheral cornea. Figure 7-59 shows a Kayser-Fleischer ring. Notice that the ring is most prominent in the vertical meridian.
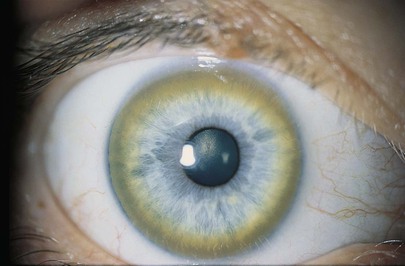
Figure 7–59 Kayser-Fleischer ring.
Corneal ulcers are extremely painful lesions caused by loss of substance from the cornea by progressive erosion and necrosis of tissue. These ulcers may be caused by a variety of agents, including bacteria, viruses, fungi, and hypersensitivity reactions. Pneumococcus organisms are common bacteria associated with corneal ulceration. Pseudomonas infection is less common but is associated with a rapid spread and corneal perforation. Herpes simplex virus (HSV) is another common cause of corneal ulceration and is the most common cause of corneal-related blindness. It is almost always unilateral and may affect any age group. The keratitis (inflammation of the cornea) is commonly accompanied by conjunctival hyperemia, tearing, and photophobia. Recurrent attacks may be less painful to painless as generalized corneal anesthesia develops. Patients with AIDS or other immunosuppressive conditions are very susceptible to this recurring infection. Figure 7-60 shows a corneal ulceration secondary to HSV infection. Marked blepharospasm is common with corneal ulceration. The most common characteristic finding of HSV-related keratitis is the dendritic ulcer on the cornea. This ulcer is the result of active viral replication in the corneal epithelial cells. Figure 7-61 shows HSV-related keratitis. The eye has been stained with rose Bengal. The devitalized, swollen cells laden with the replicating virus stain brightly with this substance. Figure 7-62 shows corneal scarring in another patient as a result of a previous herpes zoster infection. Note the discrete areas of infiltrates in the cornea, as well as the darkening of the skin on the ipsilateral side from the nose to the forehead.
Keratoconus is an acquired abnormality of the shape of the cornea. It has a gradual onset. It is usually bilateral but asymmetric. It is estimated to occur in 1 per 20,000 individuals. The cornea protrudes as a cone, with the apex becoming thin and scarred. Affected patients experience slow visual deterioration. When the patient is asked to look downward, the cone can become quite obvious, deforming the lower lid to a pointy shape as seen in Figure 7-63. This is known as Munson’s sign.

Figure 7–63 Keratoconus. Munson’s sign.
Patients with keratoconus or corneal scarring from other causes may require corneal transplantation. A recent corneal transplant is shown in a patient in Figure 7-64. Note the sutures and the mild edema. In recent years, a new treatment, corneal cross-linking, has been developed to prevent the need for corneal transplantation; corneal cross-linking causes the cornea to harden, and the cornea can then be reshaped with laser correction.

Figure 7–64 Corneal transplant.
Figure 7-65 shows a patient with a dermolipoma of the corneal limbus. It is a smoothly rounded, yellowish, benign growth (see also Fig. 7-51).
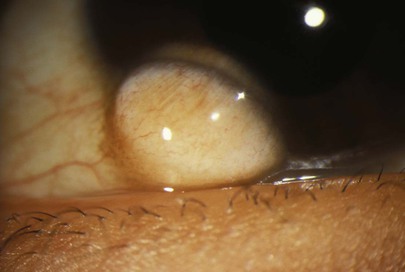
Figure 7–65 Dermolipoma of corneal limbus.
Inspect the Pupils
The pupils should be equal in size, round, and reactive to light and accommodation. In approximately 5% of normal individuals, pupillary size is not equal; this is called anisocoria. Anisocoria may be an indication of neurologic disease. Pupillary enlargement, or mydriasis, is associated with ingestion of sympathomimetic agents or with administration of dilating drops. A sluggish, mid-dilated pupil may be present with acute angle-closure glaucoma. Pupillary constriction, or miosis, occurs with ingestion of parasympathomimetic drugs, with inflammation of the iris, and with drug treatment for glaucoma. Many medications can cause anisocoria. It is therefore important to ascertain whether the patient has used any eye drops or has taken any medications.
Pupillary abnormalities may be markers of neurologic disease. The Argyll Robertson pupil is a pupil constricted 1 to 2 mm that reacts to accommodation but is nonreactive to light. It occurs in association with neurosyphilis. Horner’s syndrome is sympathetic paralysis of the eye that is caused by interruption of the cervical sympathetic chain. In addition to miosis and ptosis, anhidrosis8 is also present. A benign condition known as Adie’s tonic pupil is a pupil dilated 3 to 6 mm that constricts little in response to light and accommodation. This pupil is often associated with diminished to absent deep tendon reflexes in the extremities. It occurs more commonly in women 25 to 45 years of age, and the cause is unknown. There are no serious clinical implications. Table 7-7 lists features of these significant pupillary abnormalities.
Inspect the Iris
The iris is evaluated for its shape, color, presence of nodules, and vascularity. Normally, iris blood vessels cannot be seen unless the eye is observed with magnification.
An iris coloboma is a notch or gap in the iris. It results from failure of fusion of the embryonic tissue. The typical iris coloboma is usually part of a choroidal coloboma, which is an autosomal dominant trait. It is often bilateral, is usually located inferiorly, and involves the iris, choroid, or overlying retina (see Fig. 7-146). Visual acuity may be normal if the macula and optic nerve head are spared. Figure 7-66 shows a patient with an iris coloboma involving the ciliary body and the choroid.

Figure 7–66 Iris coloboma.
Inflammation of the iris, known as iritis or iridocyclitis, is associated with severe pain, photophobia, tearing, decreased vision, and circumcorneal congestion. This congestion is caused by injection of the deep episcleral vessels (known as ciliary flush). The dilation of the iris vessels leads to transudation of protein into the aqueous humor and deposition of inflammatory cells on the corneal endothelium, known as keratic precipitates. As a result of this deposition, the iris becomes blurred and loses its distinctive radial appearance (a “muddy iris”). There are many causes of iritis, including exogenous infection from perforating injuries; secondary infection from the cornea, sclera, or retina; endogenous infection such as tuberculosis, gonorrhea, syphilis, and viral and mycotic infections; and systemic diseases such as rheumatoid arthritis, systemic lupus erythematosus, Reiter’s disease, Behçet’s syndrome, and relapsing polychondritis. Figure 7-67 shows the classic features of an extremely severe case of acute iritis. Most of the time iritis is not visible to the naked eye and requires examination using the slit lamp.
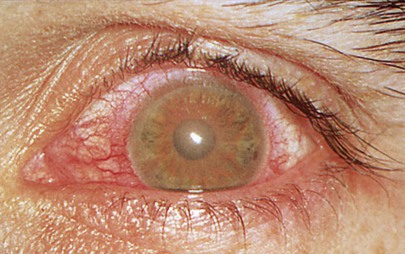
Figure 7–67 Acute iritis.
As a result of the inflammatory reaction of the iris, the iris may adhere to the cornea, forming anterior synechiae; posterior synechiae are adhesions between the iris and lens. Glaucoma is a well-known sequela of iritis and synechiae formation. Visualization of synechiae requires slit lamp examination.
Inspect the Anterior Chamber
Is the anterior chamber clear? If not, is it filled with pus or blood? Figure 7-68A shows pus in the anterior chamber, known as a hypopyon, in a patient with HSV keratitis. Another example of hypopyon, a large hypopyon together with severe conjunctival injection, is shown in Figure 7-68B.
Is there blood in the anterior chamber? This condition, known as a hyphema, is illustrated in Figure 7-69. Note the subconjunctival hemorrhage also in the patient in Figure 7-69A. A hyphema can occur as a result of significant blunt trauma to that eye causing bleeding within the eyeball. This bleeding comes from the anterior chamber angle or the iris, and therefore pupillary abnormalities are common. A hyphema can occur spontaneously also, not related to trauma. The presence of neovascularization of the iris, as can be seen in severe diabetes mellitus or after a central retinal vein occlusion, predisposes for a spontaneous hyphema. Figure 7-70 depicts an example of a “candy cane” hyphema resulting from neovascularization of the iris as a consequence of a central retinal vein occlusion. The photograph shows blood breakdown products intermingled with fresh blood.
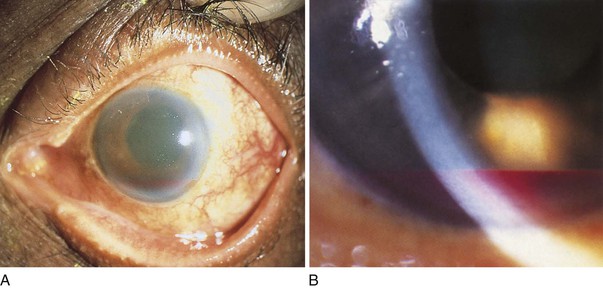
Figure 7–69 A and B, Two examples of hyphema.
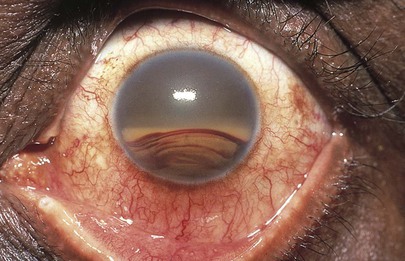
Figure 7–70 “Candy cane” hyphema.
Assess the depth of the anterior chamber. By shining a light obliquely across the eye, you can estimate the depth of the chamber. If a crescentic shadow on the far portion of the iris is visible, the anterior chamber may be shallow. Shadowing of the anterior chamber refers to the decreased space between the iris and the cornea. The technique for estimating the depth of the anterior chamber is illustrated in Figure 7-71.
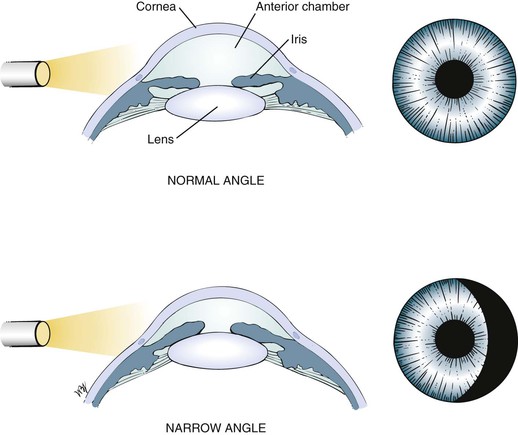
Figure 7–71 Assessing the depth of the anterior chamber.
Inspect the Lens
With oblique lighting, inspect the lens. Is the lens clear? Note any opacity that may be visible through the pupil.
The most commonly observed abnormality of the lens is opacification; the most common cause of opacification is aging. Slow, gradual vision loss is the symptom. Other causes include hereditary diseases, such as Down’s syndrome and cretinism; ocular diseases, such as high myopia, iritis, and retinal dystrophy; systemic disease, such as diabetes and hypoparathyroidism; medications, such as steroids; and trauma, such as a penetrating eye wound.
A cataract is any opacification of the lens that causes reduced visual acuity and interferes with the patient’s everyday life. Figure 7-72A shows a dense cataract of the left eye. Note the leukocoria9 related to the cataract. Figure 7-72B shows a dense nuclear, or central cataract of the left eye in another patient. Figure 7-73 is a close-up view of a dense nuclear cataract with anterior cortical spokes (opacification of the anterior cortex of the lens). The red reflex, described in the following section, “Ophthalmoscopic Examination,” is absent in all of these patients.
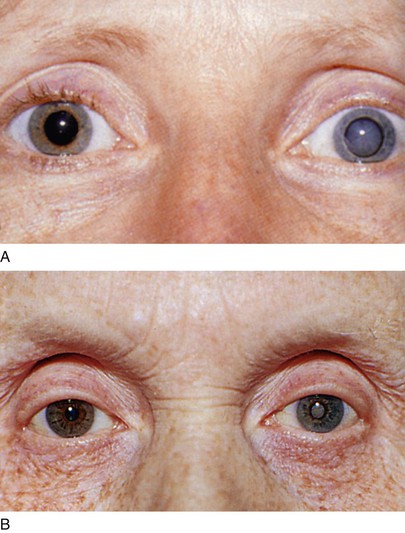
Figure 7–72 A and B, Cataract of the left eye.
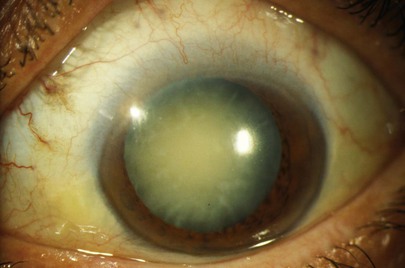
Figure 7–73 Dense nuclear cataract.
Is the lens in the normal position, or is it dislocated? The lens may be dislocated anteriorly, pressing the iris against the posterior cornea and blocking aqueous humor outflow, or it may be dislocated posteriorly. Secondary glaucoma may result. Marfan’s syndrome is an autosomal dominant condition, often with incomplete expression, in which there is increased length of the long bones; ocular complications include dislocation, or subluxation, of the lens, usually superiorly and nasally. Figure 7-74 shows a subluxated lens secondary to Marfan’s syndrome. This is the pupil of the patient’s left eye. Note the lower edge of the lens and the attached zonules that are apparent from the 3 o’clock to 7 o’clock positions (white lines). The red behind these lines is the red reflex of the retina in the background.
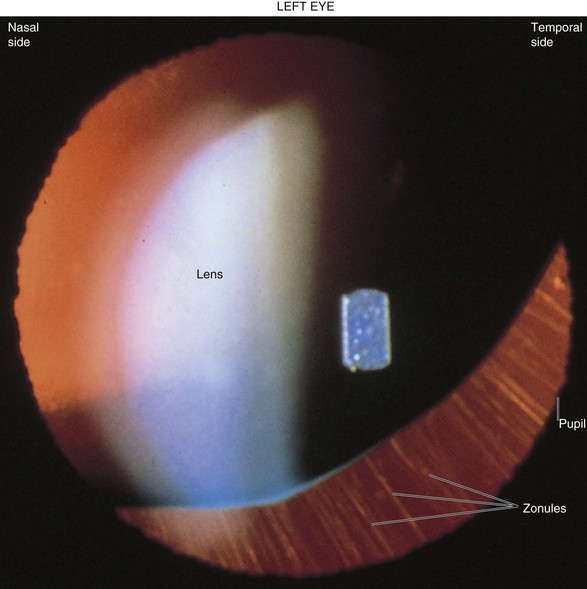
Figure 7–74 Subluxated lens (left eye) in Marfan’s syndrome.
Patients now receive intraocular lens implants after cataract surgery. Figure 7-75 shows a dislocated intraocular lens implant. Note the dislocated wire attachment.
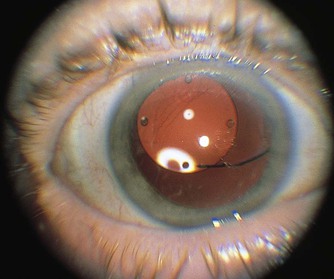
Figure 7–75 Dislocated intraocular lens implant.
Ophthalmoscopic Examination
The Ophthalmoscope
Before the examination of the optic fundus is discussed, a few words about the ophthalmoscope are in order. The ophthalmoscope is an instrument with a mirror optical system for viewing the interior anatomy of the eye. There are two dials on the ophthalmoscope: one adjusts the light apertures and filters, and the other changes the lenses to correct for the refractive errors of both the examiner and the patient.
The most important apertures and filters are the small aperture, the large aperture, and the red-free (green) filter. The small aperture is for an undilated pupil, the large aperture is for a dilated pupil, and the red-free filter excludes rays of red light and is designed for visualization of blood vessels10 and hemorrhages. With this filter, the retina appears gray, the disc appears white, the macula appears yellow, and blood appears black.
Using the Ophthalmoscope
Hold the ophthalmoscope in your right hand in front of your right eye to examine the patient’s right eye. Ask the patient to look straight ahead and fixate on a distant target. If you wear glasses, remove them for better visualization of the retina. The ophthalmoscope light is turned on, and the aperture is switched to the small aperture. Start with the lens diopter11 dial set to 0 if you do not use glasses. The myopic examiner should start with “minus” lenses, which are indicated by red numbers; the hyperopic examiner needs “plus” lenses, which are indicated by black numbers. Your index finger remains on the dial to enable easy focusing.
Place the ophthalmoscope against your forehead while your left thumb gently elevates the patient’s right upper eyelid gently against the superior orbital rim. The ophthalmoscope and your head should function as one unit. While looking through the ophthalmoscope, approach the patient at eye level from about 15 inches (38 cm) away at an angle of approximately 15 to 20 degrees lateral from center, as shown in Figure 7-76. The light should shine on the pupil. A red glow, the red reflex, can be seen in the pupil if the path of light is not obstructed by an opaque lens. Note any opacity in the cornea or lens. Because the macula is temporal to the optic disc, by shining the light 15 to 20 degrees lateral from center, little light will fall directly on the macula, and the patient will not find the light beam uncomfortable.
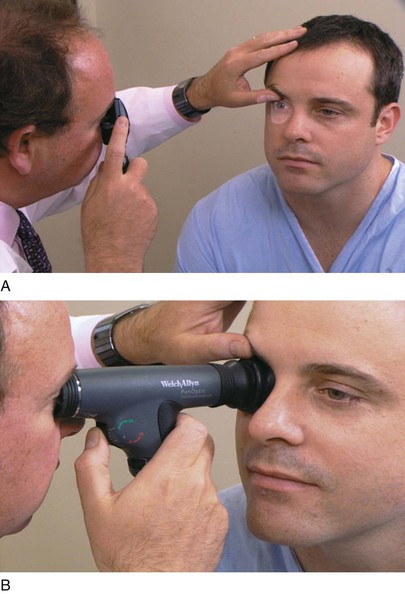
Figure 7–76 A and B, Correct positions for holding the ophthalmoscope and patient’s eye. B, The PanOptic ophthalmoscope.
By moving in toward the patient along the same 15 to 20 degree line, you begin to see the blood vessels of the retina. Move in close to the patient, bringing your hand holding the ophthalmoscope against the patient’s cheek. As contact is made with the patient, the optic disc or vessels are visible. By rotating the diopter wheel with the index finger, you bring these structures into sharp focus. Figure 7-77 shows the correct position of the examiner and patient for viewing the retina; Figure 7-78A shows a normal optic fundus in the right eye and Figure 7-78B in the left eye. Notice that the macula is temporal to the optic disc.
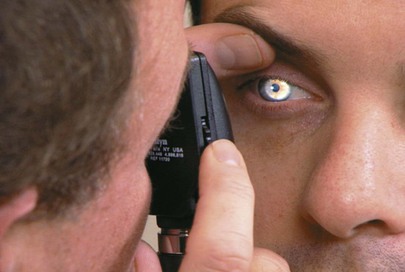
Figure 7–77 Correct position for examining the retina.
After the right eye is examined, hold the ophthalmoscope in your left hand and use your left eye to examine the patient’s left eye.
Careful assessment of the optic fundus is important for several reasons. The optic fundus is the only area where the blood vessels can be seen in vivo; it can provide an excellent picture of the state of the vasculature of other organs. In addition, the optic fundus is frequently involved with manifestations of systemic disease such as AIDS, infective endocarditis, hypertension, and diabetes; a thorough evaluation of the fundus can provide valuable clues to their diagnosis. Finally, because the eye is an extension of the central nervous system, evaluation of the optic fundus can provide information about many neurologic disorders.
The optic fundus must be assessed methodically, starting at the optic disc, tracing the retinal vessels emerging from it, inspecting the macula, and evaluating the rest of the retina.
Inspect the Optic Disc
The most conspicuous landmark of the retina is the optic disc (Fig. 7-79). The optic disc is the intraocular portion of the optic nerve and is seen with the ophthalmoscope. Its margins, color, and cup-disc ratio should be determined. The disc should be round or slightly oval with the long axis usually vertical and with sharp borders. The nasal border is normally slightly blurred. The disc is pinkish in light-skinned individuals and yellowish-orange in darker-skinned individuals. The relative pallor of the optic disc is caused by the reflection of light from the myelin sheaths of the optic nerve. In the center of the normal optic disc, there is a funnel-shaped depression known as the physiologic cup. The cup is the portion of the disc that is central, lighter in color, and penetrated by the retinal vessels. The normal ratio of the cup diameter to disc diameter varies from 0.1 to 0.5. The examiner should check the cup-disc ratio in both eyes for symmetry. Asymmetry of the physiologic cups is not typical, and the patient should be evaluated for possible early glaucoma.
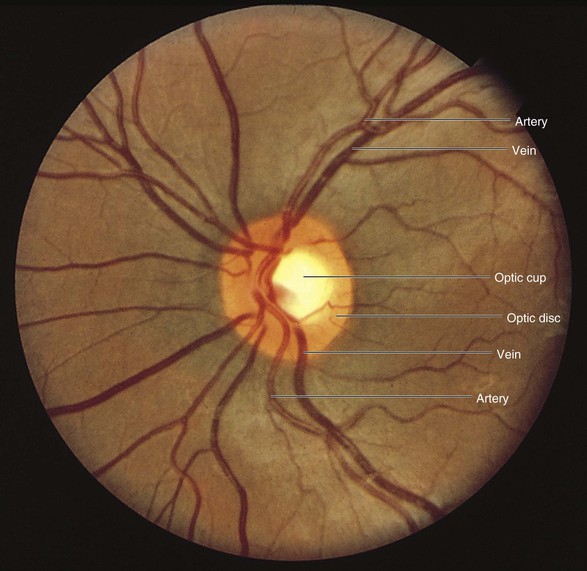
Figure 7–79 Normal optic disc, left eye.
The benign condition myelinated, or medullated, nerve fibers is seen in 0.3% to 0.6% of all individuals. In this condition, the nerve fiber layer continues to myelinate into the retina. The fibers appear as white patches with feathery borders that radiate from the optic disc and obscure the retinal vessels over which they pass. The condition can be seen soon after birth, does not change, and usually causes no visual impairment. Figure 7-80 shows the retina of a patient with myelinated nerve fibers. Another dramatic example of myelinated nerve fibers at the disc is shown in Figure 7-81. Figure 7-82 shows myelinated nerve fibers in the peripheral retina.
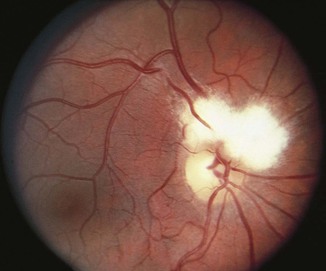
Figure 7–80 Retina with myelinated nerve fibers.
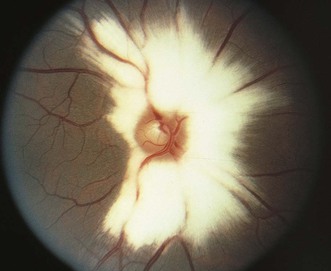
Figure 7–81 Myelinated nerve fibers at optic disc.

Figure 7–82 Myelinated nerve fibers at peripheral retina.
An optic pit is a congenital anomaly of the optic disc. It is a small depression, located temporally in 75% of cases, in the optic nerve and is usually gray or yellow. In 85% of cases, it is unilateral. Figure 7-83A shows an optic pit. Retinal tears and detachment can occur in 50% of patients with an optic pit, as shown in Figure 7-83B; this patient has an optic pit and a retinal tear involving the macula of the left eye.
Inspect the Retinal Vessels
The retinal vessels are evaluated as they arborize over the retina. The central retinal artery enters the globe through the physiologic cup. It divides within the cup and again on the surface, giving rise to four main branches that supply the superior and inferior temporal and nasal quadrants of the optic fundus. The arteries are two-thirds to four-fifths the diameter of the veins and have a prominent light reflex. This light reflex is a reflection of the ophthalmoscope’s light on the arterial wall and is normally approximately one-fourth the diameter of the column of blood. The veins exhibit spontaneous pulsations in 85% of patients. This can best be demonstrated as the retinal vein enters the optic nerve where it can be seen on end.
As all the vessels course away from the disc, they appear to narrow. The crossing of the arteries and veins occurs within two disc diameters from the disc.
The normal vessel wall is invisible with its thin light reflex. In hypertension, the vessel may have focal or generalized areas of narrowing or spasm, causing the light reflex to be narrowed. With time, the vessel wall becomes thickened and sclerotic, and there is a widening of the light reflex to greater than half of the diameter of the column of blood. The light reflex develops an orange metallic appearance called copper wiring (Figure 7-84A). When such an artery crosses over a vein, there appears to be a discontinuity of the venous column as a result of the widened, but invisible, arterial wall. This is termed arteriovenous nicking (Figures 7-84B and 7-84C). It has been postulated that, because the arteriole and venule share a common sheath, the arteriole’s thicker walls push against those of the venule forcing the venule to collapse. This makes the venule form an hourglass shape (nicking) around the arteriole.
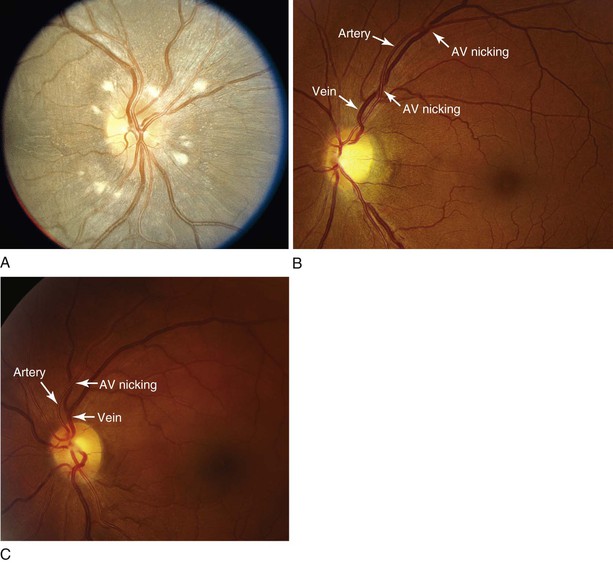
Figure 7–84 Hypertension. A, Note the “copper wiring” of the arteries and the numerous cotton-wool spots, which are exudates caused by infarctions of the nerve fiber layer. B, Notice the two areas of arteriovenous (AV) nicking in this patient’s left eye. C, A close-up of the retina of another patient showing AV nicking and marked copper wiring of the arterial wall.
Follow the vessels in all four directions: superior temporal, superior nasal, inferior nasal, and inferior temporal. Remember to move your head and the ophthalmoscope as one unit.
Inspect the Macula
When the ophthalmoscope is kept level with the disc and moved temporally approximately 1.5 to 2 disc diameters, the macula is seen. This appears as an avascular area with a pinpoint reflective center, the fovea. If the examiner has difficulty in seeing the macula, the patient can be instructed to look directly into the light; the fovea is then visible. The red-free filter is also helpful in locating the macula. Figure 7-85 shows a normal macula of the right eye.
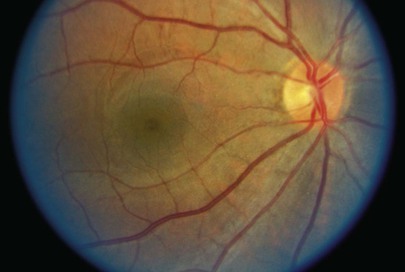
Figure 7–85 Normal macula, right eye.
Figure 7-86 shows a patient with a macular hole of the left eye; notice the punched-out appearance at the macula. Macular holes can be seen in patients with high myopia.

Figure 7–86 Macular hole.
Describe Any Retinal Lesions
When a lesion is seen, its color and shape are important in determining its cause. Is it red, black, gray, or whitish? Red lesions are usually hemorrhages. They can be located best by using the green (red-free) filter of the ophthalmoscope. Linear, or flame-shaped, hemorrhages occur in the nerve fiber layer of the retina (Fig. 7-87), whereas round hemorrhages are located in deeper intraretinal layers. Are the borders of the lesions sharp or blurred?
A common benign retinal finding is congenital hypertrophy of the RPE. This appears as a round, dramatically dark pigmented lesion, often one to several disc diameters in size. The surface is flat, and the edges are very sharp. Several small, punched-out holes are commonly present within. The retinal vessels appear normal. This is an asymptomatic lesion and is usually unilateral; it may occur in any position in the retina. Its recognition is important and should not be misdiagnosed as a malignant melanoma. Figure 7-88 shows a retina with congenital hypertrophy of the RPE.
Black lesions that are shaped like bone spicules are associated with retinitis pigmentosa (RP). In this condition, melanin tends to unsheathe the retinal vessels (see Fig. 7-148 and a discussion of this condition at the end of this chapter). A doughnut-shaped lesion is often found in chronic inactive toxoplasmosis chorioretinitis (see Figs. 7-131 and 7-132). A pigmented, raised, disc-shaped lesion is suggestive of a melanoma (see Fig. 7-145). Diffuse spotting of the retina is often a degenerative state. Flat, gray lesions are usually benign choroidal nevi (see Fig. 7-144).
White lesions may appear soft, as in cotton-wool spots, or dense, as in drusen. Soft, cotton-wool spots or exudations are caused by retinal nerve fiber layer microinfarcts (see Figs. 7-84A and 7-87). Infarcted retinal ganglion cell axons extrude their axoplasm and form these yellowish-white spots. These spots are commonly arrayed around the optic disc and along the temporal vascular arcades. Cotton-wool spots are frequently associated with hypertension or diabetes. Drusen appear in normal aging, but they may also be found in other pathologic conditions, as is discussed later in this chapter.12 The differentiation of white lesions of the retina is summarized in Table 7-8 and is discussed later in this chapter under “Clinicopathologic Correlations.”
Table 7–8
Differentiation of Whitish Lesions of the Fundus
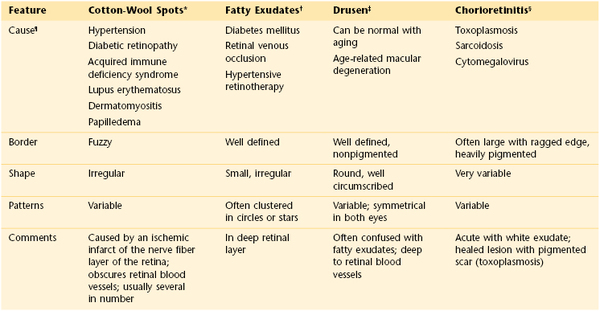
* See Figures 7-84A and 7-87.
† Also known as edema residues. See Figures 7-108 and 7-109.
‡ Also known as colloid bodies. See Figure 7-125.
§ See Figures 7-131 to 7-141.
¶ The diseases noted do not constitute a complete etiologic list. Only the most common causes are indicated.
Difficulties in Using the Ophthalmoscope
Frequently, difficulties arise in the use of the ophthalmoscope. These include the following:
The use of mydriatic drops to better visualize the retina is important. Many medical students fear that these drops will precipitate an attack of narrow-angle glaucoma. It is clear from the data that more retinal findings are missed by not dilating the pupils than when the drops precipitate such an attack, which occurs in less than 0.1% of patients. If, by some chance, this reaction occurs, the patients are in the best possible facility for treatment.
The examiner should use one drop of tropicamide (Mydriacyl) in each eye. Care should be taken to place the drop on the inside of the lower lid by pulling the lower eyelid away from the eye to make a space. The patient should be told that the drop will sting slightly and will result in everything appearing much brighter, especially if it is a sunny day. Often a drop of proparacaine hydrochloride 0.5% is instilled beforehand to cut down on the sting of the tropicamide. The duration of the mydriatic action depends primarily on the patient’s sensitivity to the medication: a more heavily pigmented iris requires more time to achieve mydriasis. The cycloplegic13 action lasts for approximately 3 to 4 hours. These drops should not be used in patients wearing contact lenses; patients need to remove the lenses first. Atropine should be avoided because its effect lasts for up to 2 weeks. The large aperture of the ophthalmoscope is used when the pupil is dilated. Record in the chart that the patient’s pupil or pupils were dilated and which medications were used.
The room should be darkened as much as possible for the easiest evaluation of the retina. Another common problem is corneal reflection. Often, light is reflected from the cornea, which makes the examination more difficult. Use of the small aperture or a polarizing filter, which many ophthalmoscopes include, may be helpful.
Patients with myopia provide the most problems for the novice examiner. In myopic eyes, the retinal image is enlarged, making it difficult sometimes to visualize the retina adequately. If the patient is severely myopic, it may be necessary for the patient to wear corrective lenses while being examined.
A mature, or advanced, cataract may not allow adequate visualization of the retina.
Clinicopathologic Correlations
There are many ophthalmoscopic conditions with which the examiner should be familiar. An image is normally focused directly on the retina. When the image is not focused on the retina, a refractive error is present. Lenses are used to correct refractive errors. The absence of a refractive error is called emmetropia. Refractive errors are extremely common. Listed here are the common refractive errors and their causes:
Hyperopia (also known as hypermetropia or farsightedness): Light is focused posterior to the retina.
Myopia (also known as nearsightedness): Light is focused anterior to the retina.
Figure 7-89 illustrates normal (emmetropic), hyperopic (hypermetropic), myopic, and astigmatic eyes.
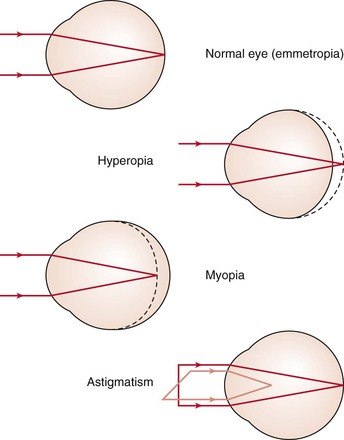
Figure 7–89 Common refractive errors.
Cataracts (see Figs. 7-72 and 7-73) are the most common cause of blindness. A cataract is a type of degenerative eye disease. One of the first symptoms that patients with cataracts experience is a “mistiness” of vision. Affected patients typically give a history in which vision has become “like looking through a dirty window.” As the lenticular opacity increases with time, there is a diminution of visual acuity in association with glare in bright light. This effect results from pupillary constriction limiting the light rays passing through the central portion of the lens, where the opacity is often most dense.
Narrow-angle glaucoma results from an obstruction to the drainage of aqueous humor at the canal of Schlemm. Patients with narrow-angle glaucoma have periodic attacks of acute elevation of intraocular pressure caused by intermittent obstruction. This is associated with pain, seeing halos, and poor vision. These attacks of glaucoma commonly occur in a darkened room, when pupillary dilatation occurs. When the pupil is dilated in a person with a narrow angle, the redundant iris folds at its base cause the increased obstruction and decreased drainage.
Primary open-angle, or chronic simple, glaucoma, in contrast, is associated with an open angle. There are many causes for simple glaucoma, which is a leading cause of slowly progressive blindness. The most important diagnostic difference from narrow-angle glaucoma is that in chronic simple glaucoma, pain is absent. Patients have reduced outflow of aqueous humor through the trabecular meshwork and into the canal of Schlemm, which results in elevated intraocular pressure. As a result, progressive cupping of the optic nerve (i.e., loss of nerve substance) occurs, accompanied by changes in the visual field. Other newer technologies14 are available to help the ophthalmologist evaluate the progression of glaucoma. Although primary open-angle glaucoma is usually bilateral, its asymmetric onset results in a difference in optic cup size between the two eyes, one of the most characteristic early signs (Fig. 7-90). Vision is increasingly impaired as progressive atrophy of the optic nerve continues, owing to the increased intraocular pressure. Late in the disease, only a small area on the nasal aspect of the nerve head may remain. Figure 7-91 shows a close-up of the optic disc of a patient with 50% to 60% cupping of the optic nerve head. Table 7-9 lists the major characteristics of both types of glaucoma.
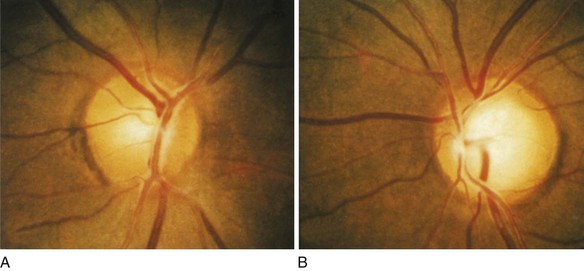
Figure 7–90 A and B, Optic cup asymmetry in glaucoma. The cup-disc ratio is approximately 30% in A (right eye) and 70% in B (left eye).
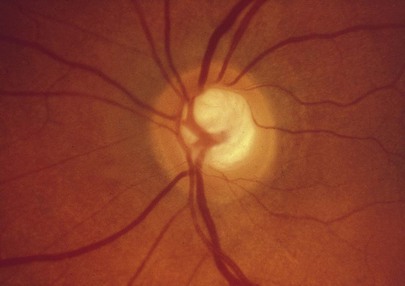
Figure 7–91 Glaucomatous cupping of the optic nerve head. The cup-to-disc ratio is approximately 50% to 60%.
Table 7–9
Characteristics of Glaucoma
| Feature | Primary Open-Angle Glaucoma | Narrow-Angle Glaucoma |
| Occurrence | 85% of all glaucoma cases | 15% of all glaucoma cases |
| Cause | Unclear* | Closed angle prevents aqueous drainage |
| Age at onset | Variable | 50 to 85 years |
| Anterior chamber | Usually normal | Shallow |
| Chamber angle | Normal | Narrow |
| Symptoms | Usually none Decreased vision, late |
Headache Seeing halos around lights Sudden onset of severe eye pain Vomiting during attack |
| Cupping of disc | Progressive if not treated (see Figs. 7-90 and 7-91) | After one or more untreated attacks |
| Visual fields | Peripheral fields are involved early Central involvement is a very late sign |
Involvement is a late sign |
| Ocular pressure | Progressively higher if not medically controlled Late: high |
Early: detected with provocative tests only |
| Other signs | Fixed, partially dilated pupil Conjunctival injection “Steamy” cornea† |
|
| Treatment | Medical Laser surgery |
Surgical |
| Prognosis | Good if recognized early Very dependent on patient compliance |
Good |
* Thought to be a defect in the trabecular network ultrastructure.
† Like looking through a steamy window.
Acute eye inflammations are common. They may be associated with local or systemic disease. The differential diagnosis of the red eye is important. The presence of pain, visual loss, and irregularities of the pupils are important signs signifying a serious, potentially blinding disorder. Figure 7-92 shows a patient with a red eye. Table 7-2 provides an approach to the diagnosis of the red eye.

Figure 7–92 Red eye.
Diabetic retinopathy is the leading cause of blindness in Americans aged 20 to 75 years. It is estimated that more than 12 million Americans have diabetes. Diabetic retinopathy is a highly specific vascular complication of type 1 and type 2 diabetes mellitus and is directly related to the duration and management of the disease. By 25 years after the onset of diabetes, nearly all patients with type 1 diabetes and 65% of patients with type 2 diabetes have some degree of retinopathy.
The retinal findings of diabetic retinopathy are the result of retinal microangiopathy, which causes increased vascular permeability that results in macular edema and decreased vision. In addition, vascular occlusive changes result in fibrovascular proliferation, hemorrhage, and scarring. The early changes of nonproliferative retinopathy are capillary microaneurysms, dilatation and tortuosity of vessels, and nonperfusion of areas of the retina. As the disease progresses to proliferative retinopathy, retinal neovascularization appears either at the optic disc (neovascularization of the disc [NVD]) or elsewhere in the retina (neovascularization elsewhere in the retina [NVE]). Neovascularization may diminish vision still further by vitreous hemorrhage or traction detachment of the retina.
Nonproliferative, or background, retinopathy is the first stage of diabetic retinopathy. An early sign is the development of microaneurysms. These usually have smooth borders and round shapes. In addition, intraretinal hemorrhages result from rupture of the microaneurysms, capillaries, and venules. The location of the hemorrhage within the retinal layers governs the shape of the hemorrhage: hemorrhages in the nerve fiber layer typically are flame-shaped with feathery borders, whereas hemorrhages in the deep areas of the retina have a fuzzy, blot-shaped appearance. Exudates may appear as clusters, streaks, or rings around the macula. These exudates result from leakage through the abnormally permeable capillary walls. Commonly, these microaneurysms, hemorrhages, and exudates occur near the macula. The retinal findings in a patient with nonproliferative diabetic retinopathy are shown in Figure 7-93. Note the hemorrhages and exudates. Figure 7-94 shows the marked tortuosity of the vessels in another patient with background retinopathy. Figure 7-95 shows the flame-shaped hemorrhages and exudates that are characteristic of nonproliferative diabetic retinopathy. Figure 7-96 shows circinate retinopathy in a diabetic patient.
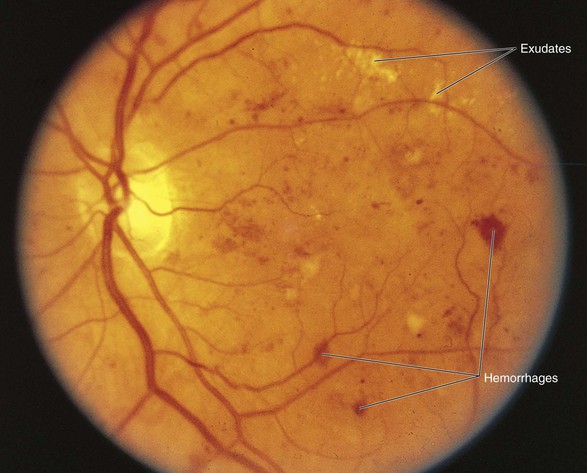
Figure 7–93 Nonproliferative diabetic retinopathy.
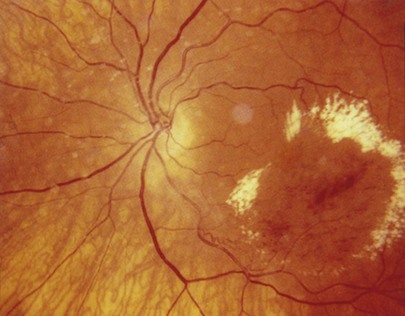
Figure 7–96 Nonproliferative retinopathy, circinate retinopathy. Note the ring of exudates around or near the macula, as well as the hemorrhages at the macula.
Proliferative diabetic retinopathy is characterized by neovascularization: that is, new blood vessels that arise from the retinal and optic disc vessels. Neovascularization appears as a fine network, known as tufts, of blood vessels that seem to bud off other vessels. NVD is shown in Figure 7-97; NVE is shown in Figure 7-98. These vessels proliferate along the retinal surface and into the vitreous humor, often with fibrous band components. The vessels are often adherent to the posterior vitreous, and preretinal hemorrhages occur as a result of vitreoretinal separation pulling on the fragile vessels. The blood resulting from a preretinal hemorrhage is trapped in the potential space between the retina and the vitreous humor (under the inner limiting membrane), forming a classic boat-shaped hemorrhage (Fig. 7-99). Further pulling on the retina can progress to retinal tears and tractional retinal detachments. Figures 7-100 to 7-102 show vitreous strands in patients with proliferative diabetic retinopathy. Figure 7-102 shows vitreous traction and a macular hole. Note the light-colored area surrounding the macula.
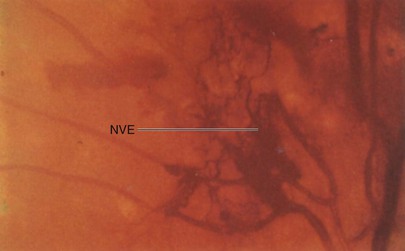
Figure 7–98 Proliferative diabetic retinopathy. Note the neovascularization elsewhere in the retina.
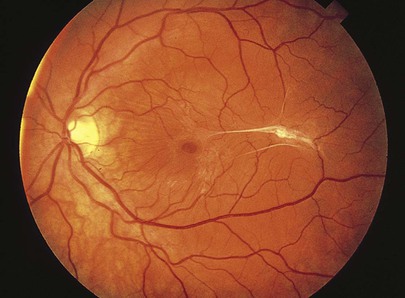
Figure 7–102 Proliferative diabetic retinopathy. Note the vitreoretinal fibrous bands and macular hole.
Figure 7-103 shows a patient with proliferative diabetic retinopathy with NVE, NVD, preretinal hemorrhage, and a fatty exudative maculopathy.

Figure 7–103 Diabetic retinopathy with neovascularization of the disc, neovascularization elsewhere in the retina, preretinal hemorrhage, and fatty macular exudates.
The therapy for proliferative retinopathy is panretinal photocoagulation (PRP) to cause regression of the neovascularization. Figures 7-104 and 7-105 show proliferative retinopathy and the laser burns of PRP. Note the PRP-treated areas that appear as round, punched-out spots with pigmentation in the center or at the margins. The treated areas first appear white or yellow, but within several weeks, pigmentation occurs. The laser burns are brought up to the vascular arcades and up to one disc diameter from the optic disc. Vitrectomy is also indicated for tractional detachments. The final stages of diabetic retinopathy, known as involutional or burned-out retinopathy, show a tangle of new vessels, hemorrhages, traction, and fibrosis.
The role of vascular endothelial growth factor (VEGF) in the growth of both regular and abnormal blood vessels was identified in the 1980s, and agents that could block the angiogenic cascade first came on the scene for cancer treatments in the early 1990s. VEGF is a signal protein produced by cells that stimulates vasculogenesis and angiogenesis. It is part of the system that restores the oxygen supply to tissues when blood circulation is inadequate. The normal function of VEGF is to create new blood vessels during embryonic development, new blood vessels after injury, and new vessels (collateral circulation) to bypass blocked vessels. When VEGF is over-expressed, it can contribute to disease.
VEGF is important in diabetic retinopathy. The microcirculatory problems in the retina of people with diabetes can cause retinal ischemia, which results in the release of VEGF. VEGF may then cause the creation of new blood vessels in the retina and elsewhere in the eye, heralding the diabetic changes that may threaten the sight. Researchers have now found a new treatment paradigm for the abnormal growth of blood vessels in the eye and the exudation of fluid from otherwise normal blood vessels: anti-VEGF agents. The use of these agents, such as pegaptanib (Macugen®), bevacizumab (Avastin®), and ranibizumab (Lucentis®), has been shown to not only slow vision loss or maintain current visual acuity, but also to offer the potential of improving and even restoring functional vision.
Hypertension also produces significant characteristic retinal features. Systemic hypertension may be reflected in the retina in terms of irregularities in arteriolar size, tortuosity of the retinal arteries, retinal edema, and changes in the arteriovenous crossings. Progressive changes of hypertension include arteriolar narrowing with increasing areas of retinal ischemia, which is evident by the development of cotton-wool exudates, hemorrhages, retinal edema, and papilledema. Figure 7-106 shows the retinal changes in a patient with hypertension. Notice in Figure 7-107 the tortuosity of the retinal vessels in another patient with hypertension; a green (red-free) filter is used to enhance the visualization of the vessels. Cotton-wool spots and flame-shaped retinal hemorrhages in another patient with hypertension are shown in Figure 7-87. As the arteriole walls thicken as a result of sustained hypertension, the arterioles lose their transparency, and noticeable changes are seen at the crossings of the arteries and veins. Veins appear to disappear abruptly on either side of an artery. Some of the arteries develop a burnishing of the red reflex.
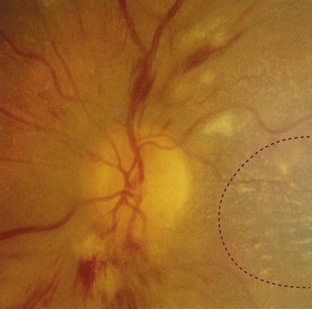
Figure 7–106 Retinal changes in a patient with long-standing hypertension. Note the cotton-wool spots and flame-shaped hemorrhages. Part of a macular star is seen on the bottom right.
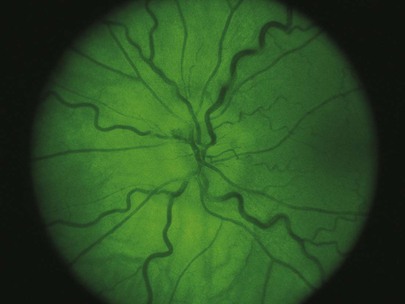
Figure 7–107 Hypertensive retinopathy. Note the markedly tortuous vessels seen through the red-free (green) filter.
Macular exudates are also common in hypertension (Fig. 7-108). These are well-defined, whitish-yellow intraretinal collections of lipids secondary to vascular leakage. A macular star is an accumulation of edema residues arranged in a stellate pattern around the macula. Macular stars are commonly seen in patients with hypertension, papilledema, papillitis, and central retinal venous occlusion (CRVO). A macular star is shown in Figure 7-109. Arteriolar dilations may also develop. These are known as arteriolar macroaneurysms and are prone to leak blood and serous fluid. A hemorrhage from a macroaneurysm is shown in Figure 7-110.
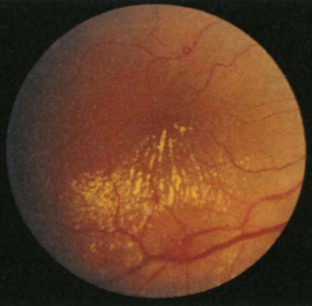
Figure 7–108 Macular exudates in a patient with hypertension.
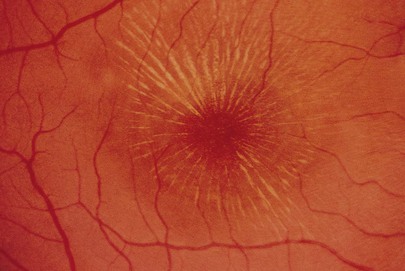
Figure 7–109 Macular star in hypertensive retinopathy.
Increased intracranial pressure, frequently secondary to a space-occupying intracranial lesion, produces a classic picture of papilledema. Papilledema is a swelling of the optic disc. It is believed that the increased pressure is transmitted to the optic nerve sheath, causing axoplasmic flow stasis in the disc. This in turn causes axonal swelling and secondary vascular congestion. The most characteristic finding is blurring of the optic disc and its margins. This occurs in association with the loss of spontaneous retinal venous pulsation, hyperemia of the disc, loss of the optic cup, hemorrhages and exudates of the disc, and dilated tortuous retinal veins. In spite of these changes, vision remains remarkably normal in the early or acute stages. Figure 7-111 is a photograph and a labeled schematic of the retinal changes in chronic papilledema. Figure 7-112 shows papilledema in another patient. Notice the blurring of the disc margins and the hyperemia of the disc. Figure 7-113 shows papilledema in yet another patient; notice the flame-shaped hemorrhages and the hyperemia of the disc. There are other causes of a blurred disc margin. Table 7-10 provides a differential diagnosis of blurred disc margins.

Figure 7–112 Papilledema. Note the hyperemia of the disc.
Table 7–10
Differentiation of Blurred Disc Margins
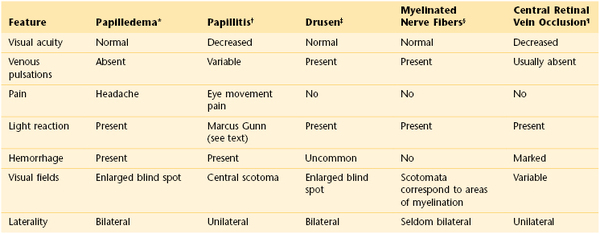
* Edema of the optic disc resulting from increased intracranial pressure. See Figures 7-111 to 7-113.
† Inflammation of the optic disc.
‡ See Figure 7-123.
§ Myelination of the optic nerve ends at the optic disc. When it continues into the retina, white, flame-shaped areas obscure the disc margins. See Figures 7-80 to 7-82.
¶ See Figure 7-121.
Blood dyscrasias are frequently diagnosed from the examination of the retina. Figure 7-114 shows the retina of a patient with leukemia. Notice the multiple hemorrhages, perivascular infiltrates of the retinal arterioles, and Roth’s spots. These spots have a clear white center and are surrounded by hemorrhage; they are believed to be areas of emboli and retinal infarcts. They are also seen in infective endocarditis and human immunodeficiency virus (HIV) retinitis.

Figure 7–114 Leukemia-related retinitis. Note the multiple hemorrhages, perivascular infiltrates, and Roth’s spots.
Occlusive disorders of the retinal circulation are dramatic. A central retinal artery occlusion (CRAO) is usually caused by an embolus from the heart or from a large artery. It results in sudden, painless loss of vision in one eye. The pupillary direct light reflex is lost, and spontaneous venous pulsations are absent. Within minutes, the retina becomes pale and milky white with narrowed arteries, and a cherry-red spot appears at the macula. This cherry-red spot appears because in the foveal area, the retina is thin, allowing visibility of the underlying choroidal circulation that is obscured elsewhere by retinal edema. This is a true ocular emergency because if it is not treated within 45 minutes, the retina may be lost. Figure 7-115 shows the left retina of a patient with a CRAO. Notice the pale retina with the cherry-red spot at the macula. Figures 7-116A and B show the retinas of two different patients with a CRAO with cilioretinal artery sparing. The cilioretinal arteries are present in 40% of normal individuals. They are derived from the posterior ciliary circulation and usually emerge from the temporal aspect of the disc to supply a small portion of the retina. Occasionally, this artery may supply enough circulation to the macula, thereby sparing central vision. Notice the area of retina that is spared as a result of perfusion by the cilioretinal artery in both images. Figure 7-116B shows the patent cilioretinal artery. Figure 7-117 shows a CRAO in another patient. In this example, the retina is also pale (ischemic and edematous), but the area of the cherry-red spot at the macula is heavily pigmented. This is the finding in dark-skinned individuals with a CRAO.
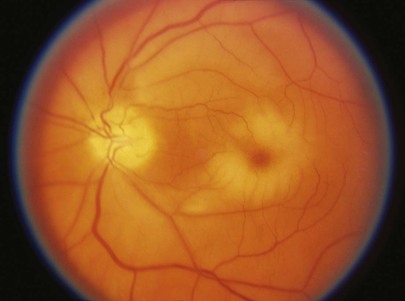
Figure 7–115 Central retinal artery occlusion.
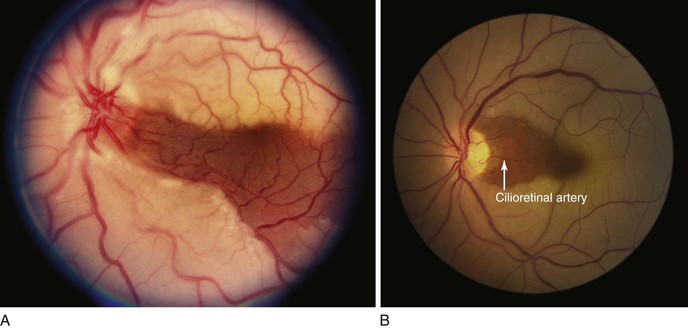
Figure 7–116 A and B, Two examples of central retinal artery occlusion with cilioretinal artery sparing. Note the patent cilioretinal artery in B.
Hollenhorst plaques are cholesterol emboli found at the bifurcation of the retinal arteries. The source of these emboli is usually the heart or the carotid arteries. These plaques are usually unilateral and occur in older adults with advanced atherosclerosis. Symptoms of fleeting alterations of vision may accompany these emboli. Figures 7-118A and B show classic examples of a Hollenhorst plaque in two different patients. Figure 7-119 shows a branch retinal artery occlusion (BRAO). Note the area of the ischemic retina and the cotton-wool spots and adjacent flame-shaped hemorrhage. Figure 7-120 shows a BRAO in another patient that involves the superior portion of the left retina. Note the superior pallor representing the ischemic retina.
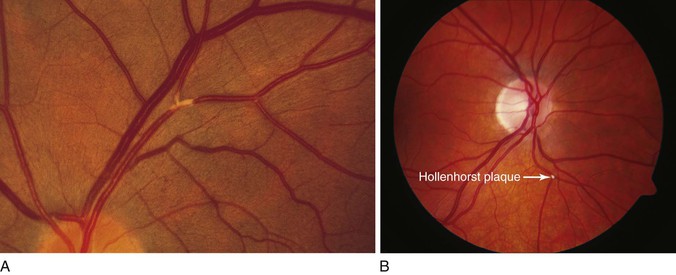
Figure 7–118 A and B, Two examples of a Hollenhorst plaque.
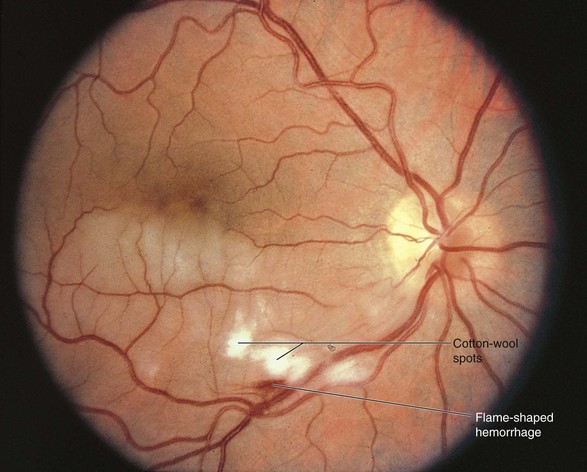
Figure 7–119 Branch retinal artery occlusion.
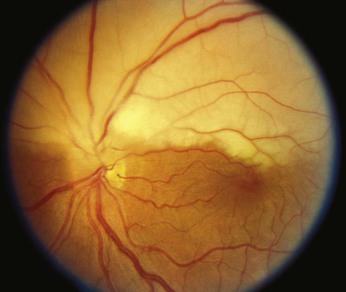
Figure 7–120 Branch retinal artery occlusion. Note the pallor of the superior left retina, resulting from occlusion of the artery supplying this area.
Venous occlusion is one of the most common retinal vascular disorders. A central retinal vein occlusion (CRVO) occurs deep within the nerve head. The patient experiences painless loss of vision in that eye. The fundus exhibits venous dilatation and tortuosity, blurred optic disc and margins caused by edema, flame-shaped hemorrhages in all quadrants, cotton-wool spots, and often a large hemorrhage at the macula. The fundus in a CRVO has been described as a “pizza thrown against a wall.” The patients are usually from 70 to 80 years of age. The causes of CRVO are many: hypertension, glaucoma, atherosclerosis, diabetes, or hyperviscosity syndromes. Figure 7-121 shows the retina of a patient with a CRVO. Notice the dark, engorged, tortuous, dusky-colored retinal veins. A branch retinal vein occlusion (BRVO) occurs at a site of retinal arteriovenous crossing. BRVO is commonly associated with systemic hypertension, although any systemic disease associated with hypercoagulability may predispose to BRVO. Distal to the site of occlusion, the retinal vein becomes engorged and tortuous with associated capillary dysfunction that leads to intraretinal edema and hemorrhage. Figure 7-122 shows two examples of the retinas of patients with a BRVO. Anti-VEGF therapy is currently being used with good results in these patients.

Figure 7–121 Central retinal vein occlusion.
Drusen of the optic disc are acellular, calcified hyaline deposits in the substance of the optic nerve that occur secondary to axonal degeneration. The disc margins are irregular or blurred. Drusen are found to be bilateral in 70% of affected patients, and the condition is transmitted as an irregular dominant trait with incomplete penetrance. Drusen occur almost exclusively in white individuals. Figure 7-123 shows optic disc drusen. Notice the scalloped appearance of the optic nerve border. Because of the irregular disc border, optic disc drusen sometimes can be confused with papilledema. The absence of optic disc hyperemia, exudates, and venous congestion as well as the presence of a normal optic cup differentiates drusen from papilledema.

Figure 7–123 Optic disc drusen.
Optic disc drusen should not be confused with retinal drusen. Diffuse retinal drusen, as shown in Figure 7-124, are not age-related phenomena and are benign. On the other hand, hard and soft retinal drusen at the level of the RPE located near the macula are part of the disorder known as age-related macular degeneration (AMD). AMD is the most common cause of blindness in patients older than 60 years in the United States. It is usually bilateral but may be asymmetric. Retinal drusen are yellowish-white, round lesions that may vary in size and are frequently concentrated at the posterior pole. Figure 7-125 shows the retina of a patient with AMD and subfoveal choroidal neovascularization. The neovascularization appears as the gray pigmentation around the drusen at the macula. This gray area represents new blood vessels grown in from the choroid between it and the RPE. Figure 7-126 is a close-up photograph of macular drusen in another patient. The growing vessels leak blood, lipids, and serum under the sensory retinal layer that stimulate the formation of a fibrous scar, further damaging the sensory retinal layers. Studies have implicated VEGF in the pathogenesis of AMD. This growth factor is naturally expressed in the retina, with high levels concentrated in the RPE. In the normal eye, VEGF may play a protective role in maintaining adequate blood flow to RPE and photoreceptors. Studies have indicated that a reduction of choroidal blood flow and oxidative stress may stimulate the initial overexpression of VEGF in the RPE and retina. This stimulates proliferation and permeability, promoting angiogenesis, increased vascular permeability, and the breakdown of the blood-retinal barrier, which are hallmarks of choroidal neovascularization and AMD. Anti-VEGF agents have been shown to be efficacious in patients with AMD. Figure 7-127 shows the retina of a patient with long-standing AMD; note that the macula has been destroyed and only a scar exists.
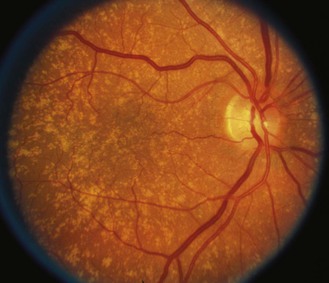
Figure 7–124 Diffuse retinal drusen that are not age related.
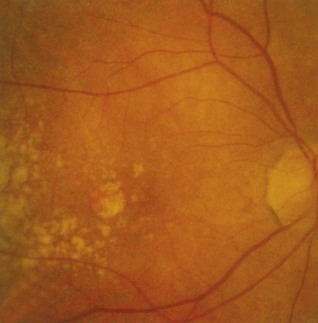
Figure 7–126 Close-up photograph of macular drusen.
Optic atrophy is a reduction in size and substance of the optic nerve caused by loss of axons and myelin sheaths. Optic atrophy may result from a lesion anywhere in the anterior visual pathway between the retina and the lateral geniculate body. The ophthalmoscopic hallmark of optic atrophy is optic disc pallor. The patient may have a loss of visual acuity, narrowed visual fields, deficit in color vision, or an afferent pupillary defect. The pallor of the disc is caused by the loss of its capillary network and by glial tissue formation. Figure 7-128 shows the right retina of a patient with optic atrophy. Note the pallor of the temporal aspect of the disc.
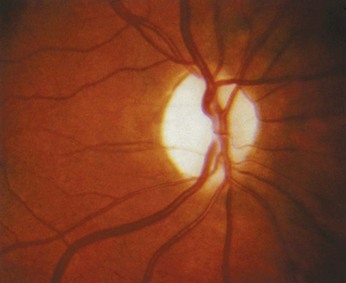
Figure 7–128 Right retina with optic atrophy. Note the marked pallor of the temporal aspect of the disc.
Anterior ischemic optic neuropathy (AION) is the most common cause of acute optic neuropathy in the older age groups. It can be nonarteritic or arteritic, the latter being associated with giant cell arteritis15 (GCA). AION is characterized by visual loss associated with pale optic disc swelling, occasionally with flame hemorrhages on the swollen disc, and sometimes with nearby cotton-wool exudates. Figure 7-129A shows a patient with AION secondary to GCA (arteritic); note the presence of pale papilledema caused by ischemia to the optic nerve. This is in sharp contrast to papilledema caused by increased intracranial pressure, which causes the disc to become hyperemic and pinkish-red. In both types of AION, visual loss is often sudden, or occurs over a few days at most, and is usually permanent; with high-dose steroid treatment, some recovery from arteritic AION may occur within the first weeks or months. Always monitor the erythrocyte sedimentation rate in patients with arteritic AION and titrate the steroid dose based on the results. As the edema resorbs, optic atrophy becomes visible as shown in the same patient 2 months later (Figure 7-129B). Figure 7-130 shows a different patient with nonarteritic AION. Note again the pale papilledema and the infarct on the nerve fiber layer. Control of blood pressure in the nonarteritic type is of paramount importance.
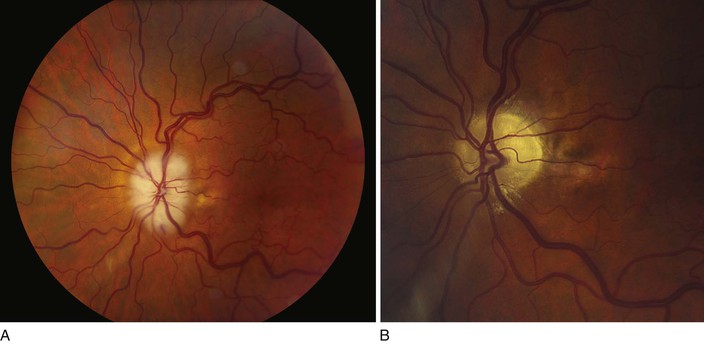
Figure 7–129 Anterior ischemic optic neuropathy—arteritic. A, Note the pale papilledema secondary to the inflammation caused by giant cell arteritis, which interferes with circulation. B, The same patient 2 months later showing optic atrophy. Note the marked pallor of the disc as the edema has been resorbed.

Figure 7–130 Anterior ischemic optic neuropathy—nonarteritic. Note the pale papilledema and the white infarct on the nerve fiber layer.
Chorioretinitis is an inflammatory process that originates in the choroid and subsequently spreads to involve the retina. Most inflammatory changes in the choroid are of endogenous origin, including tuberculosis, syphilis, Q fever, HIV, herpes zoster, cytomegalovirus (CMV), measles, sarcoidosis, histoplasmosis, Aspergillus infection, Candida infection, cryptococcosis, coccidioidomycosis, toxoplasmosis, Toxocara infection, and onchocerciasis. In acute chorioretinitis, there is blurred vision resulting from vitreous haze, and the patient sees light flashes and multiple floating spots. Loss of vision may occur if the macula is involved. In chronic chorioretinitis, there is clumping of pigment around the lesions, which are whitish owing to the presence of scar tissue and the underlying sclera that is visible because the retina and choroid have been destroyed.
Toxoplasmosis, caused by the organism Toxoplasma gondii, is most frequently a congenital condition, transmitted to the fetus from the mother during the first trimester of pregnancy. The early lesions heal once the organisms become encysted; only retinochoroidal scarring is seen on routine ophthalmoscopy. The condition may recur with the liberation of the encysted organisms and further retinal damage. The visual prognosis depends on the location of the lesion. Figure 7-131 shows the retina of the right eye of a patient with AIDS and acute toxoplasmosis chorioretinitis. The acute lesions are round with an overlying yellow-white haze as a result of a vitreitis; these acute lesions have been described as looking like a “headlight in fog.” Notice the multifocal areas of retinal involvement. This patient had similar multifocal lesions in the left eye. The multifocal areas and bilaterality are typical of acute toxoplasmosis retinitis in patients with AIDS. Figure 7-132 shows another patient with acute toxoplasmosis; notice the dense “fog” caused by the active vitreitis. Figure 7-133 shows a retina of another patient with a healed, inactive lesion of toxoplasmosis chorioretinitis at the macula. Figure 7-134 shows another patient with diffuse retinal scars secondary to inactive toxoplasmosis.

Figure 7–131 Acute toxoplasmosis chorioretinitis in a patient with acquired immune deficiency syndrome.
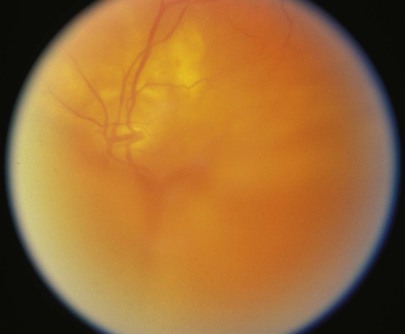
Figure 7–132 Active vitreitis secondary to acute toxoplasmosis.
The presumed ocular histoplasmosis syndrome (POHS) has a distinct retinal appearance characterized by small atrophic areas in the retina. Histoplasmosis is caused by a dimorphic yeast, Histoplasma capsulatum. It exists in humans in the yeast form and in the soil as the mold form. It is endemic in the soil along the Ohio and Mississippi River valleys and in Maryland, Florida, and Texas. Histoplasmosis enters the body through inhalation of the spores. Infection may be asymptomatic, or it may cause a mild flulike syndrome. Dissemination throughout the body may occur. Histoplasmosis infections in immunocompromised patients may cause a fulminating, life-threatening systemic infection. In POHS, there is a ring of pigmented atrophic scarring surrounding the optic nerve. The macula may also be affected. POHS is so named because the organism has never been isolated from the choroid of individuals who have been ill with histoplasmosis and have developed retinal lesions. Figure 7-135 shows the classic lesion of POHS.
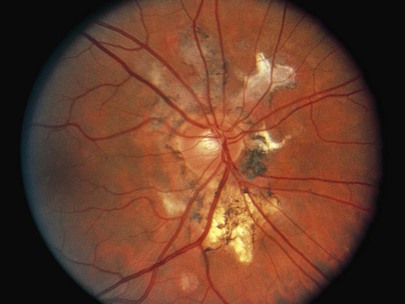
Figure 7–135 Presumed ocular histoplasmosis syndrome.
CMV chorioretinitis is the most common ocular opportunistic infection in patients with AIDS. Autopsy studies have shown that more than 95% of viral chorioretinitis in patients with AIDS is a result of CMV infection. CMV chorioretinitis is progressive and often preterminal. It appears that the patient with AIDS is at greatest risk for CMV retinitis when the CD4+ T cell count is less than 40/mm3. Figure 7-136 depicts retinal necrosis and vasculitis in a patient with AIDS and CMV chorioretinitis. Figure 7-137 shows the retina of the left eye of a patient with CMV chorioretinitis. Notice the marked retinal necrosis extending from the optic nerve superiorly and temporally. Figure 7-138 shows the retina of the right eye of another patient with CMV retinitis. There is extensive necrotizing optic neuritis with retinal necrosis and retinal vasculitis. Notice the white sheathing of the retinal vessels (especially superiorly off the disc), which is typical of vasculitis. Figure 7-139 shows the left eye of another patient with active CMV retinitis; notice the retinal vessel sheathing and extensive necrotizing optic neuritis. Figure 7-140 shows the retina of a patient with burned-out CMV retinitis. Notice the sclerosed retinal arteries and the paucity of vessels. The patient was blind as a result of the CMV infection.

Figure 7–136 Cytomegalovirus retinitis in a patient with acquired immune deficiency syndrome, right retina.
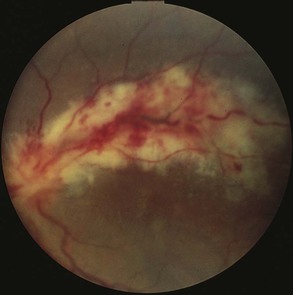
Figure 7–137 Cytomegalovirus chorioretinitis, left retina.
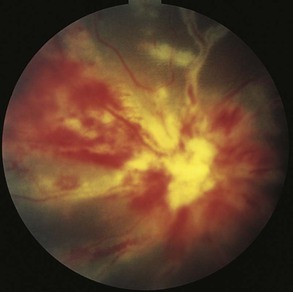
Figure 7–138 Cytomegalovirus chorioretinitis, right retina.
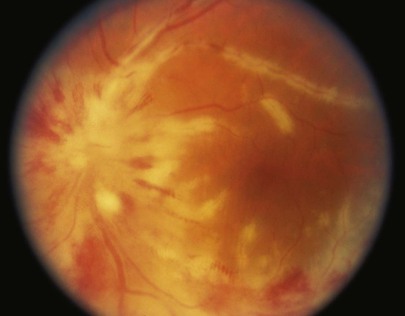
Figure 7–139 Active cytomegalovirus retinitis. Note the retinal sheathing, retinal vasculitis, and the necrotizing optic neuritis.

Figure 7–140 Burned-out cytomegalovirus retinitis.
Figure 7-141A shows the left retina of a patient with HIV chorioretinitis. Notice the cotton-wool spots and the extremely large flame-shaped hemorrhage. Figure 7-141B shows another patient with HIV chorioretinitis infection. Notice the many cotton-wool spots. Roth’s spots are commonly seen in patients with HIV chorioretinitis. Figure 7-114 shows examples of Roth’s spots in a patient with leukemia.
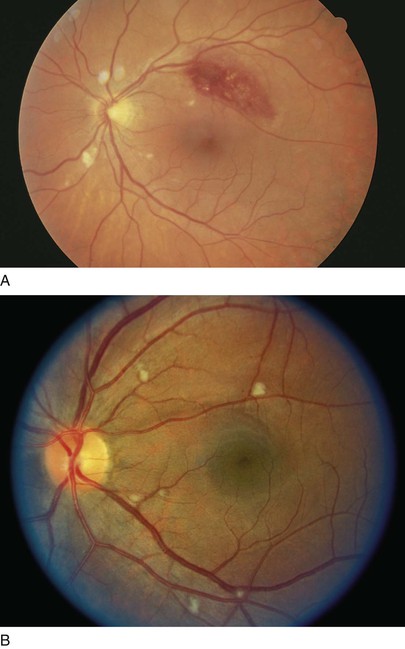
Figure 7–141 A, Human immunodeficiency virus (HIV) chorioretinitis. Note the large flame-shaped hemorrhage and the cotton-wool spots. B, Another patient with HIV chorioretinitis. Note the many cotton-wool spots.
There are several important tumors of the ocular fundus. Retinoblastoma is the most common malignant tumor of the sensory retina. It has been estimated to occur in 1 per 18,000 live births. The cancer generally is found in children younger than the age of 6; it is most commonly diagnosed in children aged 1 to 2 years. It can be sporadic or familial with an autosomal dominant mode of inheritance. The abnormal gene has been localized to the long arm of chromosome 13. Persons who inherit the gene are more likely to have bilateral retinoblastomas than are those without the gene. Children with retinoblastomas present with leukocoria, or a white pupil. Look at Figure 7-142. Leukocoria is present because most of the globe contains the large white tumor, which is often lobulated. Figure 7-143 shows the right and left retinas of a child with bilateral retinoblastomas. Note the large tumor mass in the left retina.

Figure 7–142 Leukokoria.
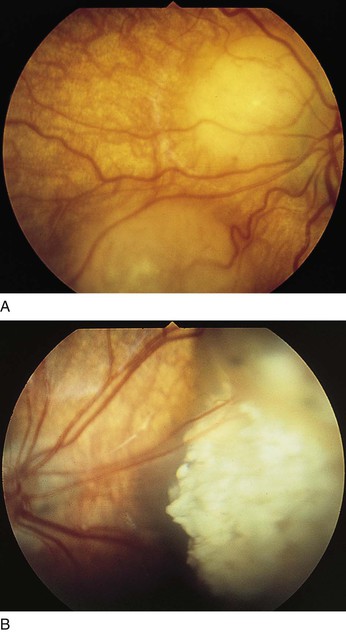
Figure 7–143 Retinoblastoma. A, Right retina. B, Left retina.
The two most important tumors of the choroid are the choroidal nevus and the choroidal melanoma. The choroidal nevus is the most common fundus tumor. It is commonly a flat, slate-gray lesion with a slightly ill-defined border. Figure 7-144 shows a choroidal nevus. A nevus must be differentiated from a choroidal melanoma. A choroidal melanoma is the most common primary intraocular malignancy. It occurs in approximately 6 per 1 million people per year. It has no sex predisposition and is usually nonfamilial. It is rare in African Americans and is most common in white persons. Unlike the choroidal nevus, the choroidal melanoma has depth and is frequently dome-shaped or mushroom-shaped. Figure 7-145 shows the retina of a patient with a choroidal melanoma.

Figure 7–144 Choroidal nevus.

Figure 7–145 Choroidal malignant melanoma.
Colobomas of the retina and choroid are congenital defects in these tissues caused by failure of the embryonic fissure to fuse properly. Colobomas appear as large white areas in which the retina or choroid is absent, and thus the white sclera is seen. Retinal vessels may cross into the lesion. Typically, colobomas are seen in the inferior aspect of the fundus because the embryonic fissure is inferonasal in the developing eye. Figure 7-146 shows the classic features of a coloboma. See also Figure 7-66, which shows an iris coloboma.
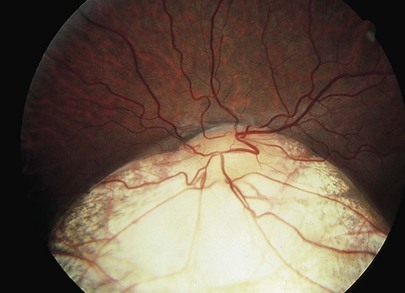
Figure 7–146 Retinal coloboma.
Retinal tears and detachments are painless. Seeing floaters or flashes is a warning sign that a person may have retinal tears. The signs of retinal tears and detachment also include reduction of vision and a shadow or curtain in the peripheral vision. Typically the shadow will move toward the center of vision over hours, days, or weeks. The patient may also experience a shower of floaters that cloud the vision. Acute retinal tears with or without flashes and floaters pose a risk because fluid can enter through the tear under the retina and lift the retina off, causing a retinal detachment. Figure 7-147 shows a giant retinal tear. A large area of bare choroid is visible through the break.
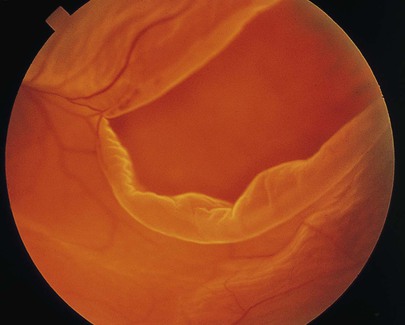
Figure 7–147 Retinal tear.
Retinitis pigmentosa (RP) is a very rare, genetically determined degenerative disease of the retina with an onset seen between the ages of 6 and 12 years. It is more common in boys than in girls and is almost always bilateral. An estimated 100,000 people in the United States have RP, mainly caused by gene mutations inherited from one or both parents. Mutated genes give the wrong instructions to photoreceptor cells, instructing them to make an incorrect protein, or too little or too much protein. Many different gene mutations exist in RP. Night blindness is the first symptom, followed by a gradually progressive constriction of the peripheral fields and eventually blurred vision. Evaluation of the retina reveals the very characteristic picture of black “bone spicule” pigmentary changes, particularly in the midperipheral retina. Macular degeneration occurs in late stages. No treatment is available, but recent studies have shown that proper vitamin A supplementation can postpone blindness by up to 10 years in certain individuals. Figure 7-148A is the classic picture of RP. A close-up photograph of the “bone spicules” is seen in Figure 7-148B.
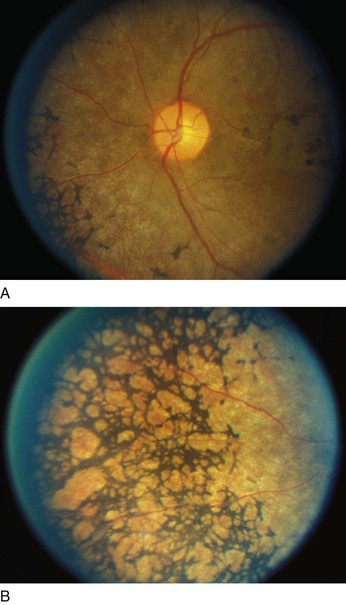
Figure 7–148 A, Retinitis pigmentosa. Note the black “bone spicules” in the midperipheral retina. B, Close-up photograph of the “bone spicules.”
A staphyloma is an outward bulging of the sclera and protrusion of intraocular contents at a point where the sclera is too thin to support the ocular structure. When present in the posterior pole, as shown in Figure 7-149, it is associated with degenerative high myopia. Macular holes, retinal tears, and retinal detachment are common. Staphylomas may be congenital or may occur after trauma or chronic inflammation that has weakened the scleral wall. In most cases, no therapy is available. In severe cases, the staphyloma gradually enlarges and enucleation may be necessary.
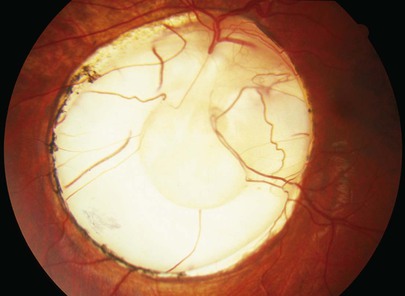
Figure 7–149 Staphyloma.
Abnormalities of gaze are not uncommon. Ophthalmoplegia is paralysis of the eye muscles. Lesions causing this paralysis may be acute, chronic, or progressive. The abnormalities of this condition are demonstrated in Figure 7-150. When the patient is asked to look straight ahead, the right eye is abducted. Notice the ptosis of the right eyelid. When the patient is asked to look to the far right, both eyes move normally, although the right ptosis is well seen. When the patient is asked to look to the far left, the right eye cannot cross the midline. This patient has an acute oculomotor paralysis secondary to a fungal lesion near the nucleus of the third cranial nerve.
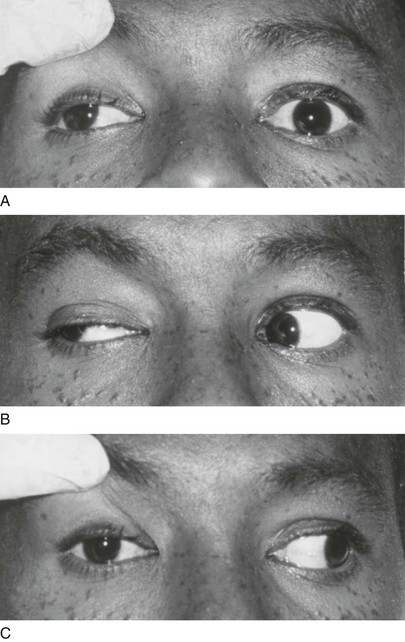
Figure 7–150 Acute right oculomotor nerve paralysis. A, When the patient is asked to look straight ahead, the right eye is turned laterally (note the position of the corneal light reflexes). The right palpebral fissure is markedly narrowed, requiring the eyelid to be elevated to visualize the position of the eye. B, When the patient is asked to look to the far right, both eyes are able to move in that direction. Note the marked ptosis of the right eyelid. C, When the patient is asked to look to the far left, the right eye cannot cross the midline.
When the patient shown in Figure 7-151 is asked to look straight ahead or to the right, both eyes move smoothly in the correct motion. However, when the patient is asked to look to the left, the left eye fails to cross the midline. Diplopia occurred as a result of a left abducens palsy secondary to carcinomatous meningitis. Another common cause of diplopia is diabetes mellitus.
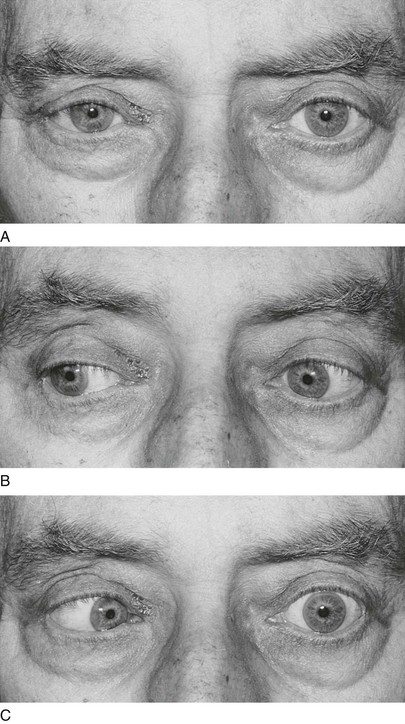
Figure 7–151 Acute left abducens paralysis. A, When the patient is asked to look straight ahead, both eyes are straight. B, When the patient is asked to look to the right, both eyes turn normally. C, When the patient is asked to look to the left, the left eye cannot cross the midline; this indicates left abducens palsy.
Head tilt may be a sign of an extraocular muscle weakness. A weakness of the superior oblique muscle, often resulting from birth trauma secondary to forceps delivery, may not be recognized until much later in life. Diplopia may develop associated with a characteristic head tilt. The head is habitually held in such a position as to avoid horizontal, vertical, or torsional diplopia. Figure 7-152 illustrates the classic head tilts associated with paralysis of the oblique muscles. With a superior oblique palsy (see Figs. 7-152A and B), the face is turned and the head is tilted to the uninvolved side; the chin is depressed. With an inferior oblique palsy (see Figs. 7-152C and D), the face is turned to the uninvolved side, the head is tilted to the involved side, and the chin is elevated. Head tilt also may be seen in paralysis of the vertical rectus muscles.
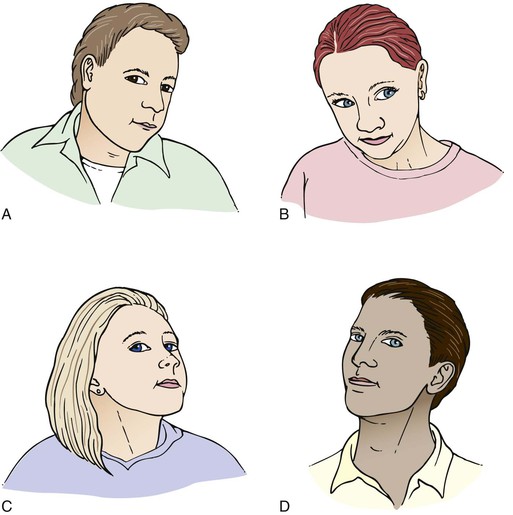
Figure 7–152 Classic head-tilt positions in patients with palsies of the oblique muscles. A, Right superior oblique. B, Left superior oblique. C, Right inferior oblique. D, Left inferior oblique.
The retinal findings of common diseases are summarized in Table 7-11. Many common diseases display their disorders at the macula of the retina. Table 7-12 provides a differentiation of some of these lesions.
Table 7–11
Retinal Characteristics of Common Diseases
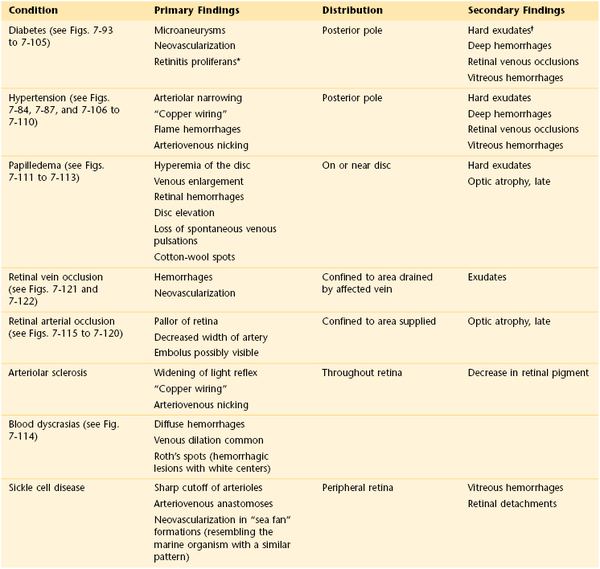
* A growth of a light-colored sheet of opaque connective tissue over the inner surface of the retina. Neovascularization of the tissue with tortuous vessels is seen. These vessels bleed easily.
† Exudate is the term used for small intraretinal lesions caused by retinal disturbances in a variety of disorders.
Table 7–12
Differentiation of Common Macular Lesions
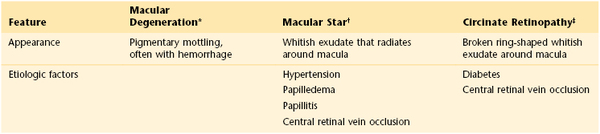
* Often bilateral in elderly patients. See Figures 7-125 and 7-127.
† See Figure 7-109.
‡ See Figure 7-96.
The bibliography for this chapter is available at studentconsult.com.
Bibliography
Albert DM, Miller JW, Azar DT. Albert and Jakobiec’s principles and practice of ophthalmology. ed 3. WB Saunders/Elsevier: Philadelphia; 2008.
Ambati J, et al. Age-related macular degeneration: etiology, pathogenesis, and therapeutic strategies. Surv Ophthalmol. 2003;48:257.
Batterbury M, Bowling B. Ophthalmology: an illustrated colour text. Churchill Livingstone: Edinburgh; 1999.
Cassirer R. The philosophy of symbolic forms. Oxford University Press: London; 1955.
Herbella FA, et al. “Raccoon eyes” (periorbital haematoma) as a sign of skull base fracture. Injury. 2001;32:745.
Kanski JJ, Nischal KK. Ophthalmology: clinical signs and differential diagnosis. Harcourt: London; 2000.
Kaufman SR. Developments in age-related macular degeneration: diagnosis and treatment. Geriatrics. 2009;64:16.
Keane P, Sadda SR. Development of anti-VEGF therapies for intraocular use: a guide for clinicians. J Ophthal. 2012 [Article ID 483034] http://www.hindawi.com/journals/jop/2012/483034/.
Kerr NM, et al. Diagnostic accuracy of confrontation visual field tests. Neurology. 2010;74:1184.
Leibowitz HM. The red eye. N Engl J Med. 2005;343:345.
Michelson JB, Friedlaender MH. Color atlas of the eye in clinical medicine. Mosby-Wolfe: London; 1996.
Mohamed Q, Gillies MC, Wong TY. Management of diabetic retinopathy. JAMA. 2007;298:902.
Rosenberg EA, Sperazza LC. The visually impaired patient. Am Fam Physician. 2008;77:1431.
Rowe S, MacLean CH, Shekelle PG. Preventing visual loss from chronic eye disease in primary care: scientific review. JAMA. 2004;291:1487.
Spaide RF. Diseases of the retina and vitreous. WB Saunders: Philadelphia; 1999.
Steinmann WC, Millstein ME, Sinclair SH. Pupillary dilation with tropicamide 1% for funduscopic screening: a study of duration of action. Ann Intern Med. 1987;107:181.
Vafadis G. When is red eye not just conjunctivitis? Practitioner. 2002;246:469.
Witmer AN, et al. Vascular endothelial growth factors and angiogenesis in eye disease. Prog Retin Eye Res. 2003;22:1.
Zadnik K. The ocular examination: measurements and findings. WB Saunders: Philadelphia; 1997.
Zarbin MA. Current concepts in the pathogenesis of age-related macular degeneration. Arch Ophthalmol. 2004;122:598.
1 The author thanks Vivian Hirshaut, MD, attending physician of ophthalmology at Mount Sinai Medical Center, New York, New York, and Albert Einstein College of Medicine, Bronx, New York, for reviewing this chapter.
2 LASIK, commonly referred to as laser eye surgery, is a procedure for the correction of refractive errors such as myopia, hyperopia, and astigmatism. LASIK surgery requires the use of an excimer laser, or microkeratome, to reshape the eye’s cornea to improve visual acuity. In most patients, LASIK surgery provides a permanent alternative to wearing eyeglasses or contact lenses.
3 Abbreviations are Latin: OD, oculus dexter; OS, oculus sinister; OU, oculus uterque.
4 Always ask a patient to cover the eye with the palm. When fingers are used to cover the eye, a patient may peek between the fingers to see the chart.
5 Positive response means that the eyes are trying to fixate on the target, indicating that vision is present.
6 See Figures 15-36 and 15-37.
7 Tell the patient to apply hot compresses to the closed eye using the hottest water he or she can stand, without burning the face.
8 Absence of sweating in this syndrome is related to interruption of the sympathetic chain. The amount of sweating is assessed by examination of the forehead or the axilla of the affected side.
9 A white pupil.
10 See Figure 7-107. Note that the blood vessels are grayish-black with this filter.
11 A unit of optical power of a lens to cause light rays to diverge or converge.
12 See Figures 7-124 to 7-127.
13 Producing paralysis of accommodation.
14 These technologies include Heidelberg retinal tomography (HRT) and optical coherence tomography (OCT). HRT is a scanning laser ophthalmoscope that is capable of acquiring and analyzing three-dimensional images of the optic nerve head and peripapillary retina. OCT is an imaging modality analogous to ultrasound.
15 The diagnosis of GCA is made definitively by biopsy of the temporal artery. If the diagnosis of temporal arteritis is confirmed, steroid therapy must be initiated immediately to avoid blindness. See also Chapter 22, The Geriatric Patient.

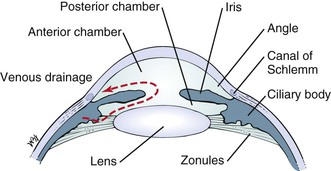










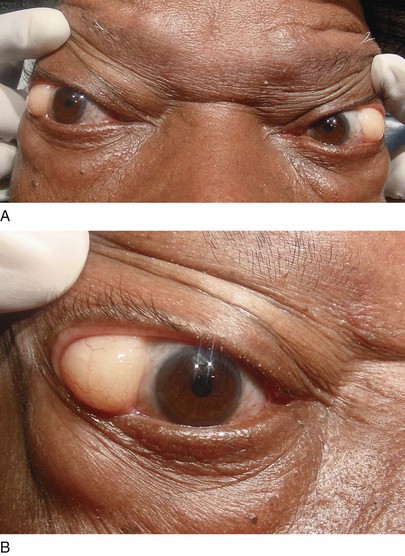

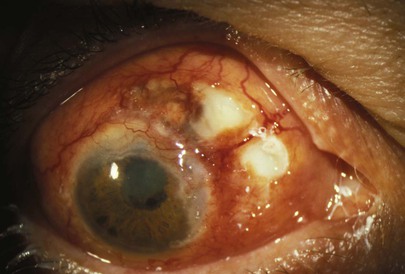



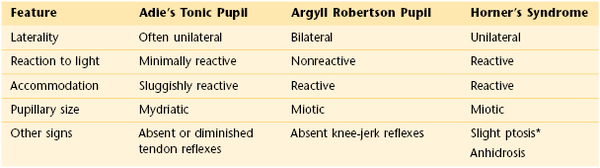
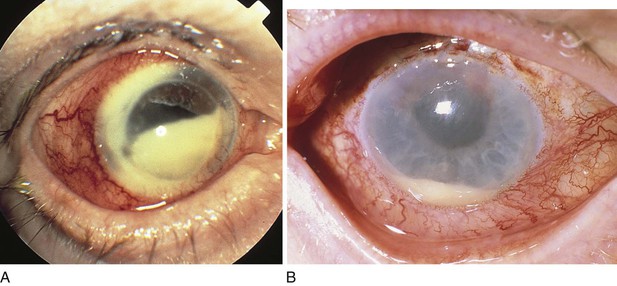

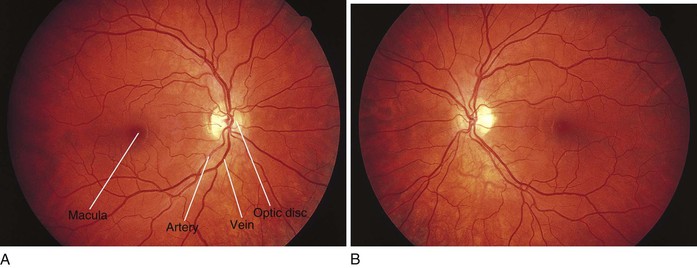

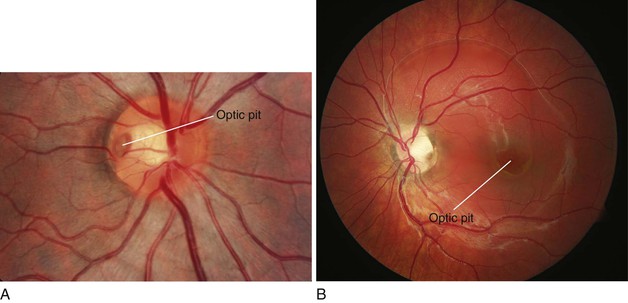





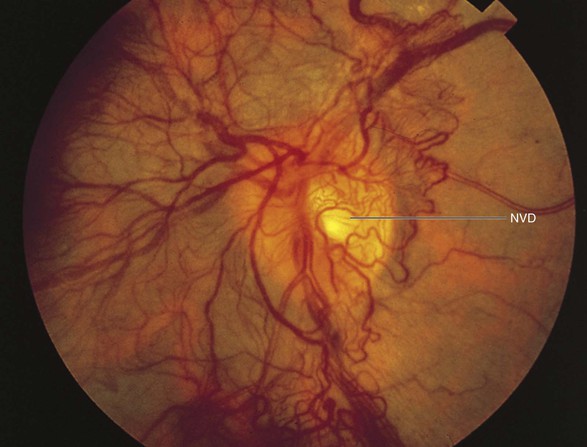
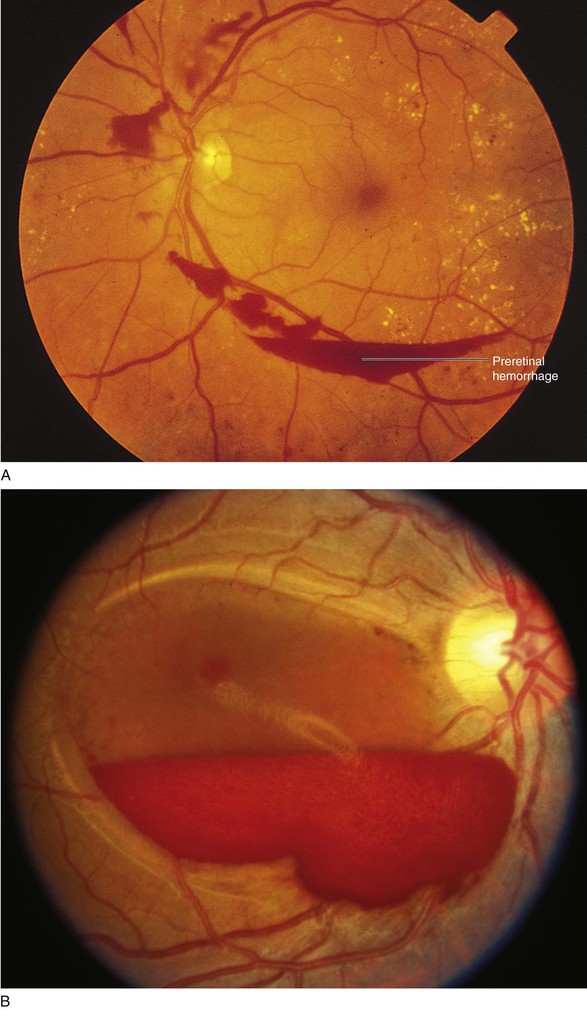
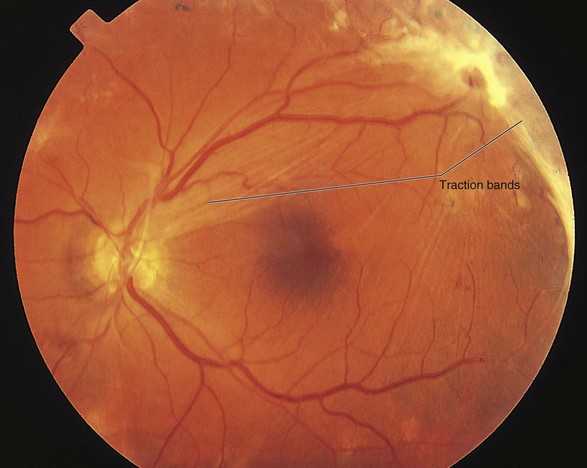
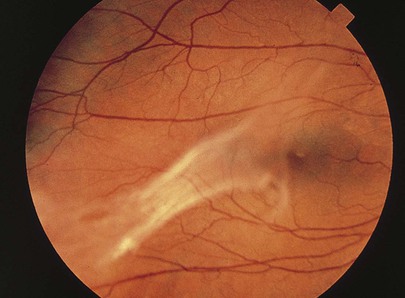

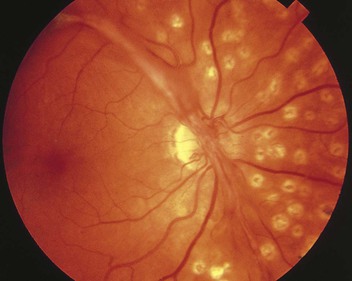
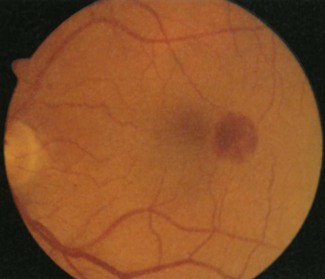
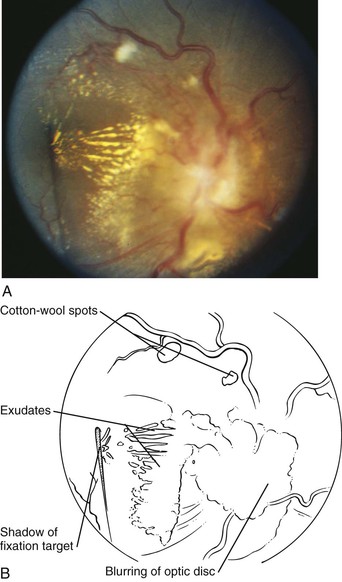
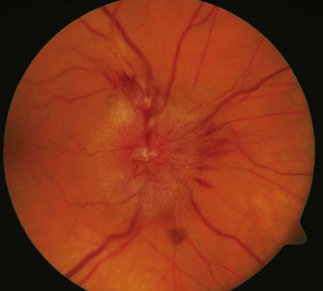

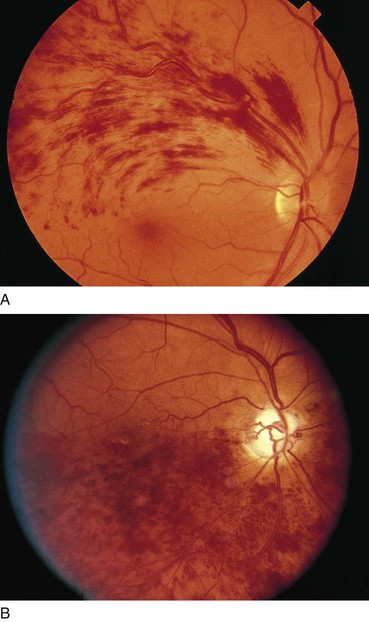
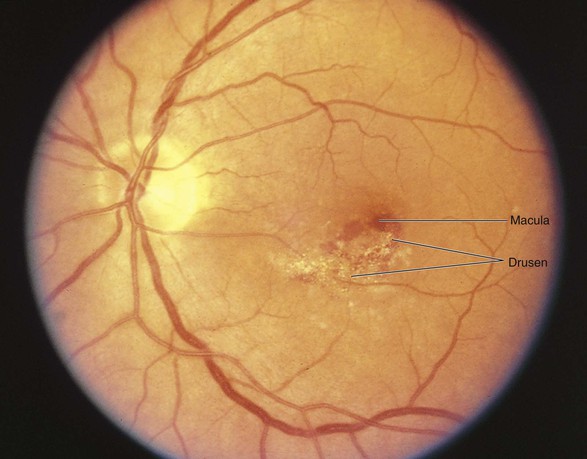
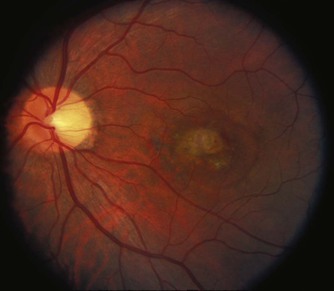
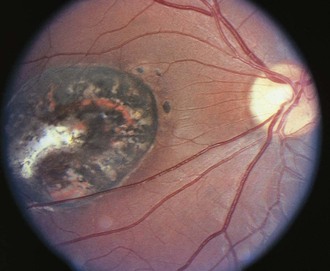
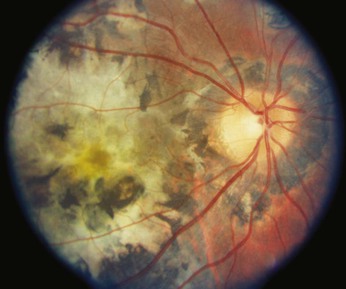
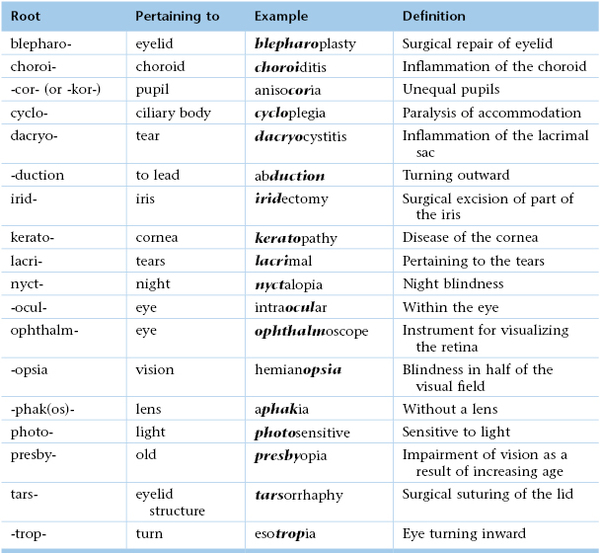
 -inch [6.35-mm] print in the newspaper at approximately 6 inches [15 cm] with his right eye. There is OS NLP. The examination of the external eye is normal. The EOMs are intact. The left optic disc margin is slightly blurred on its nasal aspect. The cup-disc ratio is normal. There are multiple, soft, cotton-wool exudates seen bilaterally. A large, flame-shaped hemorrhage is seen in the right eye at the 2 o’clock position. Arteriovenous nicking is present bilaterally.
-inch [6.35-mm] print in the newspaper at approximately 6 inches [15 cm] with his right eye. There is OS NLP. The examination of the external eye is normal. The EOMs are intact. The left optic disc margin is slightly blurred on its nasal aspect. The cup-disc ratio is normal. There are multiple, soft, cotton-wool exudates seen bilaterally. A large, flame-shaped hemorrhage is seen in the right eye at the 2 o’clock position. Arteriovenous nicking is present bilaterally.