Chapter 6. The elbow
SUMMARY
To aid diagnosis and accurate treatment, the chapter begins by outlining the relevant anatomy and provides guidelines for palpation. A commentary on the history and objective sequence follows, leading to discussion of the lesions that may be encountered, with suggestions for their effective treatment and management.
ANATOMY
Inert structures
Together with the shoulder, the elbow functions to position the hand in space. Anatomically the elbow consists of two articulations, the elbow joint proper and the superior radio-ulnar joint, both contained within the same joint capsule.
The elbow joint proper is a synovial hinge joint between the distal end of the humerus, comprising the capitulum and trochlea, and the proximal ends of the radius and ulna. The articular capsule surrounds the articular margins, originating anteriorly around the coronoid and radial fossae of the humerus and inserting into the annular ligament and anterior border of the coronoid of the ulna. Posteriorly it attaches to the olecranon fossa of the humerus and the olecranon of the ulna.
In common with other synovial hinge joints, the relatively weak articular capsule is reinforced by strong collateral ligaments. The medial collateral ligament fans out from the medial epicondyle, where it is closely related to the common flexor tendon and primarily resists valgus stresses. The lateral collateral ligament is a strong triangular band fanning out from the lateral epicondyle, where it underlies and shares a close anatomical relationship with the common extensor tendon. It runs on to blend with the annular ligament below. The radial collateral ligament stabilizes the radial head, preventing varus stresses, and the annular ligament stabilizes the superior radioulnar joint. The elbow joint has two axes of motion and thus a greater inherent stability than the shoulder (Miyasaka 1999).
The capitulum is roughly hemispherical in shape and articulates with the radial head. The trochlea is pulley- or spool-shaped and extends from the anterior aspect of the distal end of the humerus to the olecranon fossa posteriorly. Its prominent medial ridge provides a valgus tilt which contributes to the carrying angle of the elbow joint. It articulates with the trochlear notch of the ulna.
On the distal anterior surface of the humerus sit the radial and coronoid fossae, accommodating the rims of the radial head and coronoid process of ulna in full flexion. The olecranon fossa of the humerus accepts the olecranon process of the ulna in full extension. The proximal end of the radius consists of a head, neck and tuberosity. The radial head is cup-shaped superiorly for articulation with the capitulum. The periphery of the head is an articulating surface for the superior radioulnar joint, articulating with the inner surface of the annular ligament. The radial tuberosity gives insertion to the biceps tendon.
At the proximal end of the ulna is the massive, hook-shaped olecranon process. Anteriorly, the coronoid process arises with the radial notch on its medial side for articulation with the radius at the superior radioulnar joint. The elbow joint itself permits flexion and extension coupled with a small amount of adjunct rotation (Standring 2009). About 160° of passive flexion exists as the bones become almost parallel and the radial and coronoid fossae allow for extra functional movement by accommodating the flexor muscle bulk. The normal end-feel of elbow flexion is soft due to approximation of the flexor muscles. Passive extension is achieved by locking the olecranon into the olecranon fossa; it corresponds to a 180° angle and has a hard end-feel due to bone contact.
The elbow joint receives a nerve supply from the musculocutaneous, median and radial nerves anteriorly, and the ulnar and radial nerves posteriorly (C5–C8).
The superior (proximal) radioulnar joint is a uniaxial pivot joint permitting the movements of pronation and supination. These movements occur between the circumference of the radial head in the fibro-osseous ring created by the annular ligament and the radial notch of the ulna. The annular ligament is covered internally by a thin layer of articular cartilage.
Movement occurring at the superior and inferior radio-ulnar joints is rotation of the radius around the ulna to produce pronation and supination. The range of passive pronation is approximately 85° and passive supination 90°, normally with an elastic end-feel.
The carrying angle (cubitus valgus) is evident in the anatomical position. The medial end of the distal humerus projects more distally and anteriorly than the lateral, pushing the ulna laterally to produce this valgus angle. It is approximately 10–15° in men and 20–25° in women (Palastanga et al 2006). Miyasaka (1999) cites several references suggesting that the carrying angle in women is 13–16° and noting that one large study demonstrated no difference in the carrying angle between men and women.
The cubital fossa is situated on the anterior aspect of the elbow. Its proximal border is an imaginary line drawn between the two epicondyles of the humerus; its lateral border is brachioradialis and its medial border is pronator teres. On the floor of the fossa lies supinator and biceps and the roof is formed by the overlying skin and fascia. The contents of the cubital fossa, from lateral to medial, are the tendon of the biceps in the centre, the brachial artery and the median nerve.
Contractile structures
Biceps brachii (musculocutaneous nerve C5–C6) has two heads of origin. The muscle ends in a stout tendon which attaches deeply to the posterior aspect of the radial tuberosity. As the tendon passes to its insertion it twists so that its anterior surface comes to rest laterally. The tendon is separated from the anterior aspect of the radial tuberosity by the subtendinous bicipital bursa. The bicipital apo-neurosis arises anteromedially from the distal end of the tendon and sweeps medially to blend with the antebrachial fascia. Biceps is a powerful elbow flexor. Its secondary action, due to its insertion on the medial aspect of the radius, is to assist supinator in supination of the forearm, particularly with the elbow joint in 90° of flexion; it has no supinating action in the extended elbow.
Brachialis (musculocutaneous nerve C5–C6) takes origin from the anterior aspect of the lower half of the shaft of the humerus and inserts into the coronoid process of the ulna. As it crosses the elbow joint some of its deep fibres insert into the capsule of the elbow joint. Its action is to flex the elbow in either pronation or supination.
Brachioradialis (radial nerve C5–C7) passes from a long attachment on the upper two-thirds of the lateral supracondylar ridge of the humerus to the distal end of the radius just above the styloid. It flexes the elbow, being most effective in the mid-pronation–supination position.
Triceps (radial nerve C6–C8) has three heads of origin above the elbow, with its tendon inserting into the olecranon process. It is the main elbow extensor and is involved in pushing and thrusting activities as well as raising body weight on semiflexed elbows, as in getting up from a chair.
Pronator teres (median nerve C6–C7) has two heads of origin: a humeral head from just above the medial epicondyle, the coronoid process and from the common flexor tendon, and an ulnar head from the medial side of the coronoid process. It passes down and laterally to insert into a roughened area along the lateral aspect of the shaft of the radius. Its main action is to pronate the forearm, especially against resistance.
Pronator quadratus (median nerve C8, T1) binds the lower parts of the radius and ulna and is the principal pronator of the forearm.
Supinator (posterior interosseous nerve C5–C6) has its proximal attachment from the supinator crest of the ulna, lateral epicondyle of the humerus and the radial collateral and annular ligaments. It wraps round the elbow obliquely, laterally and distally, to insert into the proximal third of the radius, and supinates the forearm, bringing the palm of the hand to face upwards, whatever the degree of flexion at the elbow.
Extensor carpi radialis longus (radial nerve C6–C7) takes its main origin from the lower third of the lateral supracondylar ridge, in part deep to the origin of brachioradialis, and some origin from the common extensor tendon. It passes to the radial side of the base of the second metacarpal.
Extensor carpi radialis brevis (posterior interosseous nerve C7–C8) takes its main origin from the lateral epicondyle via the common extensor tendon, in part deep to extensor carpi radialis longus, and inserts into the radial side of the base of the third metacarpal. It is very commonly involved in tennis elbow.
Extensor carpi radialis longus and brevis extend the wrist and produce radial deviation. They work synergistically with the finger flexor tendons by holding the wrist in extension, allowing the finger flexors to form an effective grip (Palastanga et al 2006).
Other muscles which share the origin from the common extensor tendon with extensor carpi radialis brevis and are also responsible for wrist extension are extensor digitorum, extensor digiti minimi and extensor carpi ulnaris (which also produces ulnar deviation). All of these muscles are supplied by the posterior interosseous nerve (C7–C8).
Flexor carpi radialis (median nerve C6–C7) arises from the medial epicondyle via the common flexor tendon and becomes tendinous above the wrist, before passing through its own lateral compartment under the flexor retinaculum. It inserts into the bases of the second and third metacarpals.
Palmaris longus (median nerve C7–C8), often absent, arises from the medial epicondyle via the common flexor tendon and passes over, not under, the flexor retinaculum, attaching to the distal flexor retinaculum and the palmar aponeurosis.
Flexor digitorum superficialis (median nerve C7–C8, T1) lies in a slightly deeper plane than the above flexor muscles and has a humeral head from the medial epicondyle via the common flexor tendon and a small radial head. It divides to pass under the flexor retinaculum before entering the fingers to attach to the middle phalanx of each.
Flexor carpi ulnaris (ulnar nerve C7–C8) has two heads of origin: a small humeral head from the medial epicondyle via the common flexor origin and an ulnar head from the ulna. It passes over the retinaculum into pisiform.
GUIDE TO SURFACE MARKING AND PALPATION
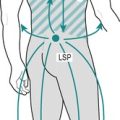
Lateral aspect (Fig. 6.1)
Palpate the lateral supracondylar ridge, which is a sub-cutaneous sharp ridge, giving part origin to extensor carpi radialis longus and brachioradialis.
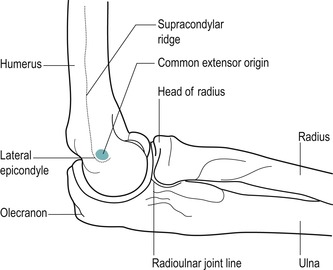 |
| Figure 6.1
Lateral aspect of the elbow in mid-position.
|
The lateral supracondylar ridge terminates in the lateral epicondyle, a small bony projection which you will palpate more easily if the elbow is flexed.
Visualize the small facet on the anterolateral aspect of the lateral epicondyle which gives origin to the common extensor tendon of the superficial wrist extensor muscles. This facet is approximately the size of the patient’s little finger nail. This appears to impose a mechanical dis-advantage, since large forces are transmitted through the common extensor tendon to this small site, leading to possible strain. The area may also be vulnerable to shearing stresses during all movements of the forearm.
Palpate the head of the radius on the lateral side of the extended forearm; it is located in a posterior depression just distal to the lateral epicondyle. Confirm the correct position by rotating the forearm to feel the radial head move under your finger.
Move proximally a short distance to palpate the radiohumeral joint line, just above the radial head. It can also be palpated by dropping into the dimple on the posterolateral aspect of the olecranon. The gap between the head of the radius and the capitulum of the humerus should be obvious; flex your elbow and feel the joint open, providing the most accessible point for an intra-articular injection. Flexion past 45° tightens the joint capsule, making the joint line less obvious. Identify brachioradialis, the most superficial forearm muscle on the lateral side of the forearm, by flexing the elbow against resistance in the mid-pronation–supination position.
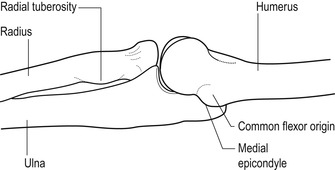
Medial aspect (Fig. 6.2)
Palpate the medial supracondylar ridge which ends in the rounded knob of the medial epicondyle. Identify the medial epicondyle, which is subcutaneous and most easily felt with the elbow in extension. Palpate the anterior aspect of the medial epicondyle, which provides the attachment for the common flexor tendon of the superficial wrist flexor muscles.
 |
| Figure 6.2
Medial aspect of the elbow in extension.
|
Visualize the position of the superficial wrist flexor muscles by placing the thenar eminence of one hand onto the opposite medial epicondyle, and spread the digits down the forearm to represent the following tendons (Fig. 6.3):
• Thumb: pronator teres
• Index: flexor carpi radialis
• Middle: palmaris longus
• Ring: flexor digitorum superficialis (deeper than the others and not so obvious)
• Little: flexor carpi ulnaris.
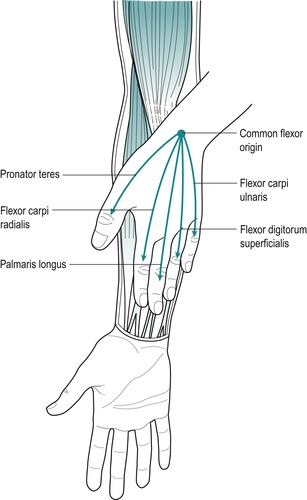 |
| Figure 6.3
The position of the muscles arising from the common flexor origin.
|
Anterior aspect
It is not possible to palpate the joint line of the elbow anteriorly because of the position of the flexor muscles, but it can be visualized approximately 1 cm below the elbow flexor crease that connects the medial and lateral epicondyles (Miyasaka 1999, Palastanga et al 2006).
Locate the tuberosity of the radius by flexing the elbow to make the tendon of the biceps more obvious. Follow the tendon down to its insertion onto the radial tuberosity. The tendon of the biceps will be easily palpable as it passes deep into the cubital fossa, but the tuberosity may not feel distinct to the palpating finger, although it is tender to deep palpation.
Place the arm in the anatomical position of elbow extension and supination and note the obvious valgus angle, known as the carrying angle. It should be symmetrical bilaterally.
Posterior aspect
COMMENTARY ON THE EXAMINATION
Observation
Before proceeding with the history, a general observation of the patient’s face, posture and gait will alert the examiner to abnormalities and serious illness. The acute elbow is usually held in a position of flexion and a degree of supination, with medial rotation at the shoulder and the patient nursing the arm in a position of comfort.
Lesions commonly found at the elbow are due to overuse when abnormalities of posture are not usually observed.
History (subjective examination)
The age, occupation, sports, hobbies and lifestyle of the patient may give an indication of the nature of the onset and cause of the injury, and will alert the examiner to possible postural or overuse problems. It may also give an indication of whether the source of the problem is in the cervical spine.
Age may be relevant, as certain conditions affect particular age groups, for example conditions such as ‘pulled elbow’ (a subluxation of the small radial head in the relatively immature annular ligament), which affects children in the 1–4 years age group. Degenerative osteo-arthrosis generally affects the elderly, while rheumatoid arthritis may involve the elbow at any age. Loose bodies can occur in adolescents, associated with osteochondritis dissecans, or in the middle-aged/elderly group, associated with degenerative changes in the articular cartilage. The overuse lesions of tennis and golfer’s elbow tend to be a problem of middle age as the ageing process causes the tendinous material to become less extensible and more prone to injury.
The elbow joint and surrounding structures are situated within the C5–C7 and T1 dermatomes. However, the site of pain is usually well localized, indicating a less severe, superficial lesion. A spread of pain would indicate a more irritable lesion and possibly referral of pain from a deeper, more proximal structure.
The patient may report local tenderness with an olecranon bursitis or, more commonly, with a tennis or golfer’s elbow, which may produce a diffuse reference of pain into the forearm, as well as point tenderness over either the lateral or medial epicondyle, respectively.
The onset of the symptoms may be sudden, due to trauma, or gradual, due to overuse or arthritis. If the onset is traumatic in nature the mechanism of injury should be deduced. Acute injuries include dislocations and fractures of the radial head, olecranon and distal humerus (Safran 1995).
Hyperextension injuries may cause a capsulitis, or a fall on the out-stretched hand may cause fracture (e.g. supracondylar, distal radius or ulna) and/or dislocation. Possible neurovascular complications, secondary to trauma, should be kept in mind.
A sudden onset of pain associated with locking of the elbow could indicate a loose body.
The duration of the symptoms may be long-standing. The most common lesions at the elbow are due to chronic overuse and result in the enthesiopathies of tennis elbow (lateral epicondylar tendinopathy) and golfer’s elbow (medial epicondylar tendinopathy). The common tendons of the forearm flexors and extensors are susceptible to excessive use because they function across two joints. The causative factors may be intrinsic overload, from the force of muscle contraction; extrinsic overload, through excessive joint torque forces stressing the connective tissue, stretching and eventually disrupting it; or a combination of intrinsic and extrinsic forces (Safran 1995).
These overuse injuries are often associated with the middle-aged racquet sports player or individuals participating in throwing activities. Throwing motions may produce a valgus stress on the medial elbow and compressive forces at the lateral elbow. Such repetitive actions may result in microtrauma to the joint or surrounding tissues (Nicola 1992).
Climber’s elbow affects brachialis, as climbing involves the use of the semi-flexed pronated forearm (Safran 1995). Overuse may cause friction between the radial tuberosity and the biceps tendon, resulting in inflammation of the biceps subtendinous bursa, or an overuse lesion in the tendon itself.
The duration of symptoms indicates the stage of the lesion in the inflammatory process and will also give an indication for the likely length of treatment, with more chronic lesions usually taking longer to resolve. The common presentation of tennis or golfer’s elbow is pain of weeks’ or even months’ duration, while the less common loose body has recurrent episodes of twinging, often resolving spontaneously. Arthritis is characterized by recurrent episodes of exacerbation of symptoms and has usually been present for months or years.
The symptoms and behaviour need to be considered. The behaviour of the pain indicates the nature of the lesion: mechanical lesions are eased by rest and aggravated by repeated movements, particularly those involved in the mechanism of the lesion. For example, tennis elbow gives an increase of pain on gripping activities – simple things such as lifting a cup or pulling up bedclothes. Patients often report that knocking the lateral aspect of the elbow can give excruciating pain and it is very tender to touch. Other symptoms described by the patient could include twinges of pain with locking of the elbow, usually just short of full extension, which would indicate a possible loose body. A twinge of pain in the forearm on gripping is also associated with a tennis elbow, causing the patient to drop the object and giving an apparent feeling of muscle weakness.
Paraesthesia may be indicative of nerve involvement and the exact location of these symptoms should be ascertained. Paraesthesia may be referred distally from the cervical spine, but as the ulnar nerve lies in an exposed location behind the medial epicondyle, it is occasionally subject to direct trauma.
Both the posterior interosseous nerve (passing between the two heads of supinator) and the median nerve (passing between the two heads of pronator teres) are susceptible to muscular compression. This may complicate the clinical presentation of either tennis or golfer’s elbow and may be a reason for a poor response to treatment.
An indication of past medical history, other joint involvement and medications will establish whether contraindications to treatment exist, or that the lesion is part of an ongoing inflammatory arthritis. As well as past medical history, establish any ongoing conditions and treatment. Explore other previous or current musculoskeletal problems with previous episodes of the current complaint, any treatment given and the outcome of treatment.
Inspection
An inspection is conducted in standing with the upper limb resting in the anatomical position, if this can be achieved. Assess the overall posture from above down, looking for any bony deformity, noting the position of the head, the lordosis in the cervical spine, the position of both shoulders and the scapulae. Assess the carrying angle in the anatomical position, comparing it with the other side for symmetry.
Inspect for colour changes, including contusions and abrasions which are associated with direct trauma. These may be located at the point of the elbow or over either epicondyle. Bruising over the biceps or triceps muscles can occur in contact sports where a direct blow is possible. Abrasions may be a site of entry for bacteria, with septic olecranon bursitis being a possible result of such infection.
Muscle wasting may be evident in the forearm if a patient has a long or recurrent history of tennis elbow. Other muscle wasting would be unusual and would probably be a neurological sign associated with cervical pathology.
Swelling is usually associated with trauma. It may be diffuse, engulfing the elbow area, in which case the elbow will be fixed in the position of ease, to accommodate the swelling with minimal pain. The dimples seen at the back of a flexed elbow are obliterated if swelling is present, as here the capsule is lax and usually accommodates excess fluid.
Immediate swelling indicates bleeding and a possible haemarthrosis. Swelling developing 6–24 h after trauma indicates synovial irritation and capsular involvement. Local swellings are associated with direct trauma. A localized soft, boggy, fluctuating swelling may be seen over the point of the elbow and is indicative of an olecranon bursitis. Occasionally patients complain of swelling over the lateral epicondyle in tennis elbow, but this is not always evident clinically.
Palpation
Since the elbow is a peripheral joint, the joint is palpated for signs of activity. Heat indicates an active inflammation (Fig. 6.4), as does synovial thickening which is most easily palpable over the radial head in the more chronic state (Fig. 6.5). Swelling is usually most apparent in the dimples at the back of the elbow and may be palpated in that area. Other swellings such as that associated with olecranon bursitis or nodules can also be palpated to assess whether they are hard or soft.
 |
| Figure 6.4
Palpation for heat.
|
 |
| Figure 6.5
Palpation for synovial thickening.
|
State at rest
Before any movements are performed, the state at rest is established to provide a baseline for subsequent comparison.
Examination by selective tension (objective examination)
The suggested sequence for the objective examination will now be given, followed by a commentary including the reasoning in performing the movements and the significance of the possible findings. Comparison should always be made with the other side.
It is important to screen other joints that may refer symptoms to the region. The 5th, 6th and 7th dermatomes pass over the elbow joint region and symptoms of cervical and/or shoulder origin should be considered and ruled out as necessary. Consider too the widespread area of referral associated with cardiac pathology.
The elbow joint and the superior radioulnar joint are assessed by four passive movements looking for pain, range and end-feel. In the normal patient passive flexion has a ‘soft’ end-feel and passive extension has a ‘hard’ end-feel. At the superior radioulnar joint, passive pronation and supination have an ‘elastic’ end-feel. The signs elicited will establish whether or not the capsular pattern exists.
Elbow and superior radioulnar joints
• Passive elbow flexion (Fig. 6.6)
 |
| Figure 6.6
Passive elbow flexion.
|
• Passive elbow extension (Fig. 6.7)
 |
| Figure 6.7
Passive elbow extension.
|
• Passive pronation of the superior radioulnar joint (Fig. 6.8)
 |
| Figure 6.8
Passive pronation.
|
• Passive supination of the superior radioulnar joint (Fig. 6.9)
 |
| Figure 6.9
Passive supination.
|
• Resisted elbow flexion (Fig. 6.10)
 |
| Figure 6.10
Resisted elbow flexion.
|
• Resisted elbow extension (Fig. 6.11)
 |
| Figure 6.11
Resisted elbow extension.
|
• Resisted pronation (Fig. 6.12 a–c)
 |
 |
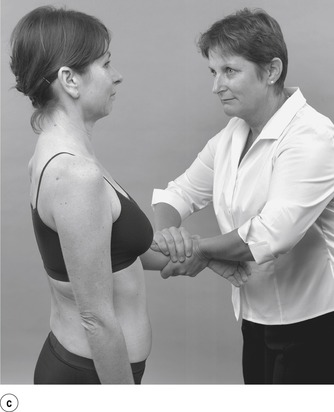 |
| Figure 6.12
(a–c) Hand and body positioning for resisted pronation and supination.
|
• Resisted supination (Fig. 6.12 a–c)
Pain provocation tests for tennis and golfer’s elbow
• Resisted wrist extension for tennis elbow (Figure 6.13 and Figure 6.15)
 |
| Figure 6.13
Resisted wrist extension.
|
• Resisted wrist flexion for golfer’s elbow (Figure 6.14 and Figure 6.15)
 |
| Figure 6.14
Resisted wrist flexion.
|
 |
| Figure 6.15
Examples of further provocative tests: (a) resisted wrist extension from the flexed position; (b) resisted wrist flexion from the extended position.
|
Palpation
• Once a diagnosis has been made, the structure at fault is palpated for the exact site of the lesion
A loose body in the elbow joint produces a non-capsular pattern of movement with either limitation of passive flexion, or extension, but not both. The limited movement has an abnormal ‘springy’ end-feel.
The resisted tests are conducted for the muscles around the elbow, looking for pain and power. Resisted elbow flexion tests biceps and resisted elbow extension tests triceps. Resisted pronation tests pronator quadratus and pronator teres, but since pronator teres takes origin from the common flexor tendon, this may be an accessory sign in golfer’s elbow. Resisted supination tests biceps, since it is assessed with the elbow flexed, and supinator.
Two provocative resisted tests are conducted at the wrist to assess the common extensor and common flexor tendons for tendinopathy. Resisted wrist extension and resisted wrist flexion are assessed with the elbow joint fully extended. Since they are not required to stabilize the elbow in this close packed or locked position, they contract strongly to resist the wrist movements and allow minor lesions to be detected. To provoke pain, further provocative tests can be applied for tennis elbow, e.g. passive wrist flexion, resisted wrist extension from the flexed position, resisted radial deviation and resisted middle finger extension. For golfer’s elbow, resisted wrist flexion can be assessed from the extended position.
CAPSULAR LESIONS
The capsular pattern indicates the presence of arthritis in the joint which, at the elbow, is frequently rheumatoid arthritis. Degenerative osteoarthrosis is of itself symptom-free, but traumatic arthritis may be secondary to overuse or trauma of a restricted joint. Treatment of choice is a corticosteroid injection into the elbow joint.
Sit the patient with the elbow flexed to approximately 45° and the forearm pronated (Fig. 6.16). Locate the radiohumeral joint line on the posterolateral aspect of the elbow. Insert the needle between the head of the radius and the capitulum (Fig. 6.17). Once intra-articular, deliver the injection as a bolus. The patient is advised to maintain a period of relative rest for approximately 2 weeks following injection.
 |
| Figure 6.16
Injection of the elbow joint.
|
 |
| Figure 6.17
Injection of the elbow joint, showing direction of approach and needle position.
|
Traumatic arthritis can be treated with other physio-therapeutic modalities.
NON-CAPSULAR LESIONS
Loose body
Osteochondritis dissecans occurs in adolescents and can give rise to loose body formation, particularly with activities such as gymnastics, throwing and racquet sports. Repeated compressive forces cause microtrauma between the radial head and capitulum and focal degeneration results in fragmentation and the formation of loose bodies (Patten 1995). Surgical removal is advisable in this age group. Joji et al (2001) present a case report to demonstrate osteochondritis dissecans occurring in the medial aspect of the distal humerus of a 17-year-old baseball pitcher, which is deemed to be less common than osteochondritis with loose body formation found in the lateral aspect.
Loose bodies can also be encountered in the middle-aged or elderly group and may be associated with degenerative changes. They may be a fragment or fragments of cartilage or bone, or both (osteochondral), and can be associated with degenerative osteoarthrosis in the older adult (Saotome et al 2006). They can be stable, fixed in a synovial recess or bursa, or attached to synovial membrane, where they tend not to be displaced. Unstable loose bodies can move freely in the joint where they can become trapped at irregular intervals between the articular bone ends, causing intermittent symptoms and joint derangement (Bianchi & Martinoli 1999).
Characteristically, the patient complains of a history of twinging pain, with the elbow giving way under pressure or locking, usually just short of full elbow extension. The history alone may be the only diagnostic evidence available since the loose body may spontaneously reduce. Sometimes diagnostic imaging may be necessary to identify and localize loose bodies before arthroscopic removal (Ho 1995).
On examination, a non-capsular pattern may exist with either a small degree of limitation of flexion or extension, but not both. The end-feel to the limited movement is abnormally springy.
The treatment of choice to reduce a loose body is strong traction together with Grade A mobilization, theoretically aiming to shift the loose body to another part of the joint and to restore full, pain-free movement.
There are two possible manoeuvres, both working towards elbow extension. The choice of starting man-oeuvre is random and sometimes it may be necessary to try both and repeat the most successful, although sometimes one manoeuvre is sufficient. As with all mobilization techniques, the patient is reassessed after every man-oeuvre and a decision made about the next, based on the outcome.
Mobilization for loose body in the elbow joint (Saunders 2000)
Towards extension and supination
Position the patient against the raised head of the couch, with the arm resting against a pillow and the elbow in approximately 90° of flexion. Use a butterfly grip with the thumbs placed on the flexor surface of the forearm, over the radius (Fig. 6.18). Face the direction of the supination movement and lift the leg farthest from the patient off the ground, leaning out to establish traction with straight arms. Step forwards, taking the elbow joint towards extension (not full range), while simultaneously rotating the forearm with several flicking movements towards supination (Fig. 6.19). The manoeuvre is easier to perform if you begin the rotation from a position of some pronation.
 |
| Figure 6.18
Hand position for mobilization for loose body in the elbow joint, towards extension and supination.
|
 |
| Figure 6.19
Body position for mobilization for loose body in the elbow joint, towards extension and supination: step forwards.
|
Towards extension and pronation
The patient’s position is the same. Face the movement of pronation, placing the thumbs on the extensor surface of the forearm, over the radius (Fig. 6.20). Establish the traction as above and step backwards, simultaneously rotating the forearm with several flicking movements towards pronation (Fig. 6.21). The manoeuvre is easier to perform if you begin the rotation from a position of some supination.
 |
| Figure 6.20
Hand position for mobilization for loose body in the elbow joint, towards extension and pronation.
|
 |
| Figure 6.21
Body position for mobilization for loose body in the elbow joint, towards extension and pronation: step backwards.
|
The patient may need to be reviewed to assess the success of the treatment. Generally speaking, the manoeuvre is usually successful, but there are no guarantees that the condition will not recur. Excessive recurrences of the condition may need referral for surgery.
Olecranon bursitis
Swelling and inflammation of the olecranon bursa can occur due to repeated pressure and friction, or to direct trauma of the bursa. The bursa is the most vulnerable structure to trauma on the posterior surface of the elbow and septic bursitis is not uncommon (Nicola 1992, Hoppmann 1993). The patient may present with an obvious swelling over the olecranon which is boggy and fluctuating. Provided sepsis is not present, conservative management includes aspiration, ice and non-steroidal anti-inflammatory drugs (Nicola 1992). Any physio-therapeutic modality may be applied and corticosteroid injection may be given in the absence of infection.
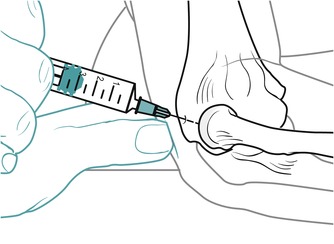
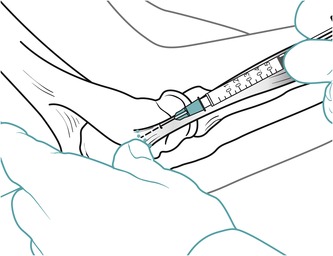
Seat the patient with the elbow supported in a degree of flexion. Palpate the obvious swollen bursa and mark a convenient point for inserting the needle. Insert the needle into the bursa (Figure 6.22 and Figure 6.23). Aspirate first to check for the presence of infection and, if clear, the injection can be delivered as a bolus. The patient is advised to maintain a period of relative rest for approximately 2 weeks following injection.
Suggested needle size: 21G × 1½ in (0.8 × 40 mm) green needle
Dose: 10 mg triamcinolone acetonide in a total volume of 2 mL
 |
| Figure 6.22
Injection of olecranon bursitis.
|
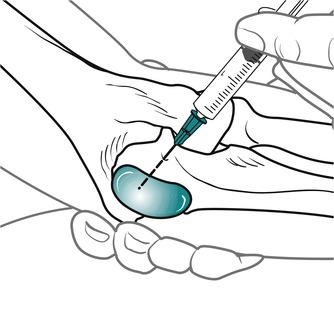 |
| Figure 6.23
Injection of olecranon bursitis, showing direction of approach and needle position.
|
Pulled elbow
This condition usually presents to the general practitioner’s surgery or the casualty department. Typically the child is aged between 1 and 4 years old and has a sudden onset of pain in the arm, followed by a reluctance to use the arm. The child is unhappy and holds the arm in elbow flexion and pronation. The arm is pain-free provided it is not moved.
There may be a history of the child stumbling or falling or it may occur if the child grabs the cot rails or other stationary object while falling. Frequently the child is accompanied by a guilty parent, if pulling a resistant toddler or lifting the child by the arms and swinging them in play was the cause.
The mechanism is thought to be a distal subluxation of the radial head through the annular ligament (Hardy 1978, Kohlhaas & Roeder 1995); however, X-rays taken before and after reduction show no evidence of displacement (Hardy 1978). An X-ray is therefore of little value unless the nature of the trauma is significant when a fracture dislocation of the elbow must be ruled out (Brukner & Khan 2007).
Reduction of a pulled elbow involves supporting the child’s elbow with one hand, feeling the radial head and providing counterpressure to axial compression. Quickly pronate the forearm through a small range while maintaining axial compression until a click is felt. The reduction is confirmed by immediate use of the arm by the child, to the subsequent relief of the parent.
Adeniran & Merriam (1994) reported a case of ‘pulled elbow’ in a 21-year-old woman, as an exception to the usual age group of the condition. Spontaneous reduction occurred as the patient was positioned into supination for X-ray.
CONTRACTILE LESIONS
Tennis elbow
Tennis elbow is the term commonly applied to a strain of the wrist extensor muscles at the site of their common origin from the anterolateral aspect at the lateral epicondyle of the humerus. In the past it has been commonly referred to as ‘lateral epicondylitis’, but the absence of inflammatory cells at the site of the lesion has led to this terminology being dropped. It is commonly a chronic lesion of more than 3 months’ duration. Tendinopathy is a more appropriate description unless excision biopsy has been performed and the specific histopathological features of the specimen can be described, to be able to distinguish between tendinopathy and tendinosis (Khan & Cook 2000). It most commonly involves the extensor carpi radialis brevis tendon and is by far the most common lesion treated at the elbow, being five to eight times more common than golfer’s elbow (Coonrad & Hooper 1973, Gellman 1992, Gabel 1999). The condition may be resistant to treatment and is prone to recurrence.
Tennis elbow was first described in 1898 by Runge as ‘writer’s cramp’ (Gellman 1992, Verhaar et al 1993). Of all diagnosed cases, 35–64% are associated with work-related activities, with tennis players representing 8% of the total diagnosed. Repetitive loading seems to be a factor, with low-load activities such as keyboarding possibly representing the majority of patients. Workplace stress contributes to psychosocial factors (Gabel 1999). Repetitive wrist movements and unaccustomed activities are often blamed. However, competitive tennis players are susceptible to tennis elbow, 50% of them experiencing at least one episode (Noteboom et al 1994). Altered biomechanics, particularly of the backhand stroke, predisposes tennis players to the condition (Schnatz & Steiner 1993).
The condition occurs in middle age, with incidence of the condition peaking between the ages of 35 and 54 and with a duration of an average episode of between 6 months and 2 years (Assendelft et al 1996, Ernst 1992, Katarincic et al 1992). It affects the dominant arm most commonly, with epidemiological studies showing a prevalence of 1% in men and 4% in women (Verhaar et al 1993, Noteboom et al 1994).
The patient complains of a gradually increasing pain felt on the lateral aspect of the elbow and posterior aspect of the forearm, sometimes referred to the wrist and into the dorsum of the hand. The condition is so common that patients often make the diagnosis themselves. There is a constant ache which is aggravated by repeated gripping actions, together with rotation of the forearm. The gripping action is often related to occupational or sporting activities and rarely is tennis elbow related to direct trauma or a traumatic incident. The possibility of acute onset has been reported, however, in which case inflammatory changes might be present (Nirschl and Maffuli et al cited in Greenfield & Webster 2002).
Point tenderness is present over the lateral epicondyle and the patient will often experience excruciating pain when the elbow is knocked. An apparent muscle weakness may be reported, as pain is often accompanied by a severe twinge which causes the patient to drop relatively light objects (e.g. coffee cup). Pienimäki et al (2002) demonstrated similar subjective pain reports in tennis and golfer’s elbow, but a greater reduction in grip strength associated with tennis elbow.
On examination there is usually a full range of pain-free movement at the elbow joint with pain on resisted wrist extension. Most authors seem to be in agreement that pain on resisted extension of the wrist and tenderness to palpation over the lateral epicondyle at the insertion of extensor carpi radialis brevis are pathognomic of the condition.
Greenfield & Webster (2002) conducted a survey of outpatient physiotherapists, seeking their opinion on current practice of tennis elbow, and identified 15 diagnostic tests, with the above two tests being used most commonly. Passive wrist flexion stretches the common extensor tendon and other resisted tests which may be positive include resisted radial deviation and resisted extension of the middle digit, which preferentially stresses extensor carpi radialis brevis as it contracts synergistically, anchoring the third metacarpal to allow the digit to extend (Brukner & Khan 2007). A clinical observation of the authors suggests that apparent weakness on resisted wrist extension may be due to pain inhibition and this sign is a useful reassessment tool. Smidt et al (2002a) recommend the use of pain-free grip strength using a hand-held dynamometer as a relatively easy test of functional disability in tennis elbow, showing it to have excellent reliability.
Mills’ sign is sometimes used to confirm diagnosis. The forearm is fully pronated and the wrist joint flexed. While maintaining this position, passive elbow extension is performed and a positive sign is elicited if pain is reproduced at the lateral side of the elbow (Noteboom et al 1994, Sölveborn et al 1995).
Cervical spine examination and radial nerve tension testing were the most popular differential diagnostic tests in the study by Greenfield & Webster (2002). Since the above positioning for the Mills’ test and the radial nerve tension test are similar, this may present a false positive result as symptoms would be provoked if neural tension and/or tendinopathy were present.
Palpation determines the site of the lesion. Of the cases of tennis elbow encountered, 90% involve the teno-osseous junction of the common extensor tendon (Cyriax 1982). Stratford et al (1989) demonstrated only a 22.5% occurrence at this site, hypothesizing that patients with tenderness over the lateral epicondyle and recurrent cases have a poorer short-term prognosis. They suggest that Cyriax would have seen more resistant cases in consultant practice whereas their research was conducted in primary care. If remaining with Cyriax’s clinical estimate, however, the remaining 10% involve the body of the tendon, the extensor carpi radialis longus attachment on the supracondylar ridge or the muscle bellies (Fig. 6.24) (Cyriax 1982).
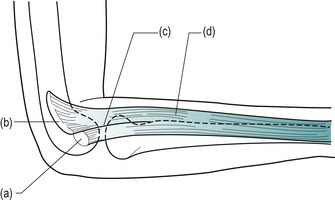 |
| Figure 6.24
Four possible sites of tennis elbow: (a) teno-osseous junction (enthesis); (b) supracondylar ridge; (c) body of the common extensor tendon; (d) the muscle bellies.
|
Mechanism of tennis elbow
The normal ageing process causes degenerative changes in collagen fibres and ground substance similar to the changes seen when tissues are immobilized (Akeson et al 1968). Degeneration and relative avascularity of the tendon make it susceptible to microtrauma through overuse activity.
The repeated gripping action may initially produce traction of the common extensor origin causing microtrauma and inflammation (Foley 1993). Microscopic and macros-copic tears occur at the common extensor origin, with the development of fibrous scar tissue and contracture. Eventually, degenerative foci and calcification can occur (Coonrad & Hooper 1973, Ernst 1992, Gellman 1992, Noteboom et al 1994).
Theoretically, initial inflammatory changes may produce a characteristic tendinopathy in an early acute lesion, but this is rarely seen clinically. Histologically, as the chronic condition develops, the degenerative features of tendinosis are thought to become paramount. This degenerative condition of the tendon is considered to be similar to the ongoing degenerative tendinosis seen in the Achilles tendon and rotator cuff tendons (Bennett 1994). With continued overuse, the degenerative changes lead to microscopic tearing and scar tissue development within the tendon. An area of vascular granulation tissue develops which contains many nociceptive nerve endings, possibly explaining why the lesion is so painful (Brukner & Khan 2007).
Chard et al (1994) conducted histological studies of normal and biopsy tendon specimens (rotator cuff tendinopathy and tennis elbow) to determine the mechanisms involved in tendon degeneration. The major mechanism of tennis elbow or rotator cuff was not inflammation, but a sequence of degenerative changes which increased with age, although chronic traction is believed to have an effect. The tendons studied were considered to have an area of relative avascularity which seemed to predispose them to degeneration.
The sequence of degeneration included changes in the blood vessel walls and fibroblasts and alteration in the gel to fibre ratio, with glycosaminoglycans replacing collagen fibres. This led to lack of maintenance of collagen turnover, loss of the wavy configuration of collagen fibres and transformation of the fibroblasts into chondrocyte-type cells, with subsequent cartilage formation, calcification and eventual bone formation. It would seem that as the degenerative process progresses the tendon fibroblasts undergo fibrocartilaginous change, ultimately to convert the tendon to bone. This theory is supported by Edelson et al (2001) who examined a large number of cadaver elbow specimens and found characteristic bone formation at the point of usual tenderness to palpation in the area that corresponded to the origin of extensor carpi radialis brevis. A C-shaped crescent of bone was identified along the posterior margin of the epicondyle, although it was also noted that the anatomical relationship of both the insertion of the tendon and the lateral collateral ligament complex at this point could not be distinguished.
Treatment of tennis elbow
Treatment of tennis elbow should always look to address the causative factors. A full explanation should be given so that the patient is responsible for modifying activities to give treatment, whatever the choice, the best possible opportunity. Lifting should be performed with a supination action rather than pronation (Gellman 1992), and various counterforce elbow or forearm supports are available to alter the stress on the common extensor origin or to rest the wrist to avoid strain. Patient and therapist can discuss the best choice for the individual patient.
With current knowledge that tendinopathy is more likely to be due to degenerative change than to inflammation, educating the patient in terms of prognosis becomes important. Many treatment options are available for the more common tendinopathies and several seem to have good pain relief in the short term. The patient needs to understand that a minimum of 3–6 months may be required to resolve their problem and that they have an important role to play in terms of activity modification (Gabel 1999).
Greenfield & Webster (2002) identified 24 different treatment modalities, demonstrating that physiotherapists use judgment largely based on past experience when choosing treatment for tennis elbow. Progressive stretch and strengthening were identified as popular treatments, with 67.5% of respondents using deep transverse frictions and 64.4% using Mills’ manipulation (see below). Although not specified in the study, it is assumed that the regime of deep transverse frictions to prepare the tendon, followed by Mills’ manipulation was used, as this is taught in the orthopaedic medicine approach.
Many studies have set out to confirm the most effective way of treating tennis elbow but definitive evidence remains elusive. Summaries of key studies follow to provide a chronological overview of the principal research conducted.
Stratford et al (1989) failed to demonstrate statistical power in a study comparing deep transverse frictions with phonophoresis, and Vasseljen (1992) demonstrated that ‘traditional physiotherapy’ consisting of transverse frictions and ultrasound performed better under subjective, but not objective, testing when compared with laser treatment.
Sölveborn et al (1995) conducted a study of 109 cases of tennis elbow treated with a single corticosteroid injection (10 mg triamcinolone) together with local anaesthetic. Bupivacaine (a long-acting local anaesthetic) was compared with lidocaine (lignocaine) (a short-acting local anaesthetic). An impressive improvement was reported 2 weeks after the injection, with the patients treated with bupivacaine showing a significantly better outcome. However, at 3 months the results in both groups showed deterioration and relapse, with patients seeking other treatments.
Verhaar et al (1996) conducted a prospective randomized trial of 106 patients with tennis elbow. They compared the effects of corticosteroid injections with Cyriax physiotherapy (i.e. deep transverse frictions followed by Mills’ manipulation – see below). Both groups showed significant improvement at 6 weeks, with the injection group demonstrating better results. However, at 1-year follow-up there was no significant difference between the groups, with 17 patients in the injection group and 14 patients in the physiotherapy group going on to eventual surgery. There were no adverse side-effects in either group. The authors reached the conclusion that, although corticosteroid injections alleviate pain in the short term, they do not address the cause of the condition. Since corticosteroid injection is more time-efficient than physiotherapy (three visits maximum for the injection group; 12 visits for the physiotherapy group), it was considered to be the more effective treatment in the short term. However, as mentioned above, the effect of corticosteroid injection on healing at different stages is uncertain.
Assendelft et al (1996), on reviewing the literature, determined that the existing evidence on effectiveness, optimal timing of injections, composition of injection fluid and adverse effects of injections is not conclusive, although they appear to be safe and effective in the short term (2–6 weeks). Three injections seem to be the recommended maximum in several reviews, with post-injection pain and subcutaneous atrophy being the adverse side-effects.
Drechsler et al (1997) compared two treatment regimes, a ‘standard’ treatment group exposed to several interventions including transverse frictions and a neural tension group exposed to mobilization of the radial nerve. The results showed no significant difference for any variable tested and the authors then attempted to validate the study through group analysis, incorporating further variables. While admitting that the study could have been confounded by these additions, they nevertheless concluded that neural and joint mobilizations together were superior to ‘standard’ treatment techniques.
Newcomer et al (2001) conducted a randomized controlled double-blind trial on 39 subjects with symptoms present for less than 4 weeks. The experimental group received corticosteroid injection and rehabilitation, the control group sham injection and rehabilitation. The authors recorded that there was no significant change in the experimental group and that subjects improved over time with the rehabilitation programme. They concluded that injections were not justified in patients who had symptoms for less than 4 weeks and that rehabilitation should be the first line of treatment.
Smidt et al (2002b) showed short-term relief for cortico-steroid injection, but physiotherapy consisting of ultrasound, deep transverse frictions and exercise was more effective in the long term, as was advice and pain medication from a family practitioner. However, there was no evidence of standardization of injection technique or of the way the physiotherapy programme was managed (Hart 2002).
Smidt et al (2003) evaluated current evidence of the effectiveness of physiotherapy for tennis elbow, identifying 23 randomized controlled trials. Little evidence was found to either support or refute the use of physiotherapy. Lack of evidence was judged to be due to low statistical power, inadequate validity and insufficient reported data. There is a need to standardize outcome measures, to increase sample sizes and to include short, medium and long-term follow-up. A few valid studies were identified which suggested the potential effectiveness of some commonly used treatments. Ultrasound may be better than placebo in alleviating pain; ultrasound with transverse frictions may be more effective than laser; and stretching, muscle conditioning and occupational exercises may be better than ultrasound with transverse frictions.
Nimgade et al (2005) provided an updated review, concluding that injections work best in the first 2–3 months of onset and that after 3 months active physio-therapy is better than injection but no better than rest. Physiotherapy was noted as better in the long term if patients are willing to wait for the improvement.
A later randomized study by Bisset et al (2006) compared mobilization with movement and exercise, corticosteroid injection, or wait and see for tennis elbow, noting outcomes at 6 and 52 weeks. Corticosteroid injection demonstrated better outcomes at 6 weeks but at 52 weeks the physiotherapy approach had superior benefit when compared to the other two groups. Tonks et al (2006) conducted a similar study, but also including steroid injection with physiotherapy, and on the basis of their results advocated that steroid injection alone should be given as the first line of treatment for patients demanding a quick return to daily activities.
In summary, relative rest and time will eventually improve function but the use of early active interventions, including steroid injection and physiotherapy modalities, may speed recovery (Nimgade et al 2005).
From this discussion the authors acknowledge that the evidence to support the use of transverse frictions and Mills’ manipulation is weak, but it should also be emphasized that these techniques have not been proven to be ineffective. It is interesting to note that the earlier studies tended to address inflammatory components rather than the degenerative features of tennis elbow. As studies continue to examine the degenerative nature of the lesion, more substantial support for treatment may emerge.
Davidson et al (1997) and Gehlsen et al (1998) show some interesting support for the use of augmented soft tissue mobilizations in animal studies. Pressures, similar to those delivered by deep transverse frictions, are applied to promote the healing process in tendinopathy, which provides a stimulus for further investigation into transverse frictions. The controlled application of microtrauma through pressure is thought to promote fibroblastic activity leading to repair in the absence of inflammation (see Ch. 4).
Greenfield & Webster (2002) demonstrate the lack of consensus on the best practice for the treatment of tennis elbow, but with well over half of the respondents choosing transverse frictions and Mills’ manipulation, positive clinical results can be assumed.
As mentioned above, Cyriax (1982) and Cyriax & Cyriax (1993) describe four possible sites of the lesion:
• Teno-osseous junction (enthesis) – mainly extensor carpi radialis brevis
• Supracondylar ridge – origin of extensor carpi radialis longus
• Body of the common extensor tendon
• The muscle bellies.
Tennis elbow at the teno-osseous junction
Cyriax (1982) and Cyriax & Cyriax (1993) describe the teno-osseous junction (enthesis) as the most common tennis elbow lesion, suggesting 90% occurrence at this site. As mentioned above, however, this may be an overestimation. Pain is localized to the common extensor tendon at the teno-osseous junction, mainly affecting the extensor carpi radialis brevis on the anterolateral aspect of the lateral epicondyle of the humerus. The facet for attachment of the common extensor tendon faces anteriorly and is approximately the size of the patient’s little finger nail. The choice of treatment may be corticosteroid injection or Mills’ manipulation.
The inflammatory model of chronic tendinopathy is under debate and the justification for corticosteroid injection is difficult in the absence of inflammation. Khan & Cook (2000) acknowledge that clinical experience and some studies show that corticosteroid injection produces short-term relief of pain in these lesions, although the mechanisms for this pain relief are currently not known. Corticosteroid injection for tennis elbow at the teno-osseous site is therefore still currently recommended as an appropriate treatment. Once rendered pain-free, the patient, through normal movement, will encourage alignment of fibres and mobility of the scar. However, injection should not be considered to be a panacea and an entire management programme, including activity modification and supports or braces, should be adhered to (Gabel 1999).
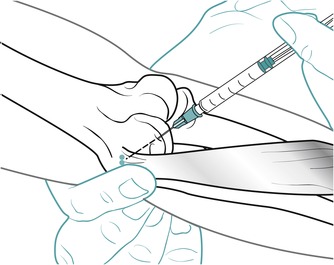
Support the patient with the forearm resting on a pillow, the elbow flexed to approximately 90° and fully supinated (Fig. 6.25). Identify the area of tenderness over the teno-osseous junction of the common extensor tendon with the anterolateral aspect of the lateral epicondyle. Insert the needle from an anterior direction, perpendicular to the facet, and deliver the injection by a peppering technique (Fig. 6.26). The patient is advised to maintain a period of relative rest for approximately 2 weeks following injection.
 |
| Figure 6.25
Injection of tennis elbow, teno-osseous site.
|
 |
| Figure 6.26
Injection of tennis elbow, teno-osseous site, showing direction of approach and needle position.
|
Corticosteroid injections do have the advantage in that they are relatively easy and quick to administer, are cheap, and specialist referral is not necessary.
An alternative treatment to corticosteroid injection is to aim to elongate the scar tissue by rupturing adhesions within the teno-osseous junction, thus making the area mobile and pain-free. This is achieved by a Mills’ manipulation, which must be followed by stretching exercises to maintain the lengthening achieved. Before the Mills’ manipulation can be performed, the teno-osseous junction is prepared by deep transverse frictions to produce an analgesic effect, in preparation for the manipulative technique.
G. Percival Mills described this technique for the treatment of tennis elbow in the British Medical Journal in (1928). On examining patients with tennis elbow, he found that on combined pronation and wrist and finger flexion the elbow joint could not achieve full extension. He suggested that forcing the restricted movement (now known as Mills’ manipulation) could be curative.
Mills’ manipulation (cited in Cyriax 1984, Cyriax & Cyriax 1993)
The area should first be prepared by transverse frictions to produce an analgesic effect before applying the technique. Position the patient comfortably with the elbow fully supinated and in 90° of flexion; this exposes the tendon by allowing it to run directly forward from the anterior aspect of the epicondyle. Locate the anterolateral aspect of the lateral epicondyle and identify the area of tenderness (Fig. 6.27). Apply deep transverse frictions with the side of the thumb tip, applying the pressure in a posterior direction onto the teno-osseous junction (Fig. 6.28). Maintain this pressure while imparting deep transverse frictions in a direction towards your fingers, which should be positioned around the posteromedial side of the elbow for counterpressure.
 |
| Figure 6.27
Transverse frictions for tennis elbow, teno-osseous site.
|
 |
| Figure 6.28
Transverse frictions for tennis elbow, teno-osseous site, showing site of anterolateral facet on the lateral epicondyle of the humerus, and the direction of application.
|
The Mills’ manipulation is performed immediately after the transverse frictions, providing the patient has a full range of passive elbow extension, demonstrated during the clinical examination process. If the patient does not have full passive elbow extension on examination, the manipulative thrust will affect the elbow joint, rather than the common extensor tendon, possibly causing a traumatic arthritis.
Position the patient on a chair with a back rest. Stand behind the patient:
• Support the patient’s arm under the crook of the elbow with the shoulder joint abducted to 90° and medially rotated. The forearm will automatically fall into pronation (Fig. 6.29).
 |
| Figure 6.29
Mills’ manipulation, starting position.
|
• Place the thumb of your other hand in the web space between the patient’s thumb and index finger and fully flex the patient’s wrist and pronate the forearm (Fig. 6.30 a–c).
 |
 |
 |
| Figure 6.30
(a–c) The thumb placed in the palm, forearm pronated and wrist maintained in full flexion.
|
• Move the hand supporting the crook of the elbow onto the posterior surface of the elbow joint and, while maintaining full wrist flexion and pronation, extend the patient’s elbow until you feel all the slack has been taken up in the tendon.
• Step sideways to stand behind the patient’s head, taking care to prevent the patient from leaning away either forwards or sideways, which would reduce the tension on the tendon (Fig. 6.31). Straighten your arm if possible but be careful not to lose the wrist flexion.
 |
| Figure 6.31
Positioning of hand on posterior aspect of extended elbow for application of the Grade C manipulation.
|
• Apply a minimal amplitude, high velocity thrust (Grade C manipulation) by simultaneously side-flexing your body away from your arms and pushing smartly downwards with the hand over the patient’s elbow.
There should be no reproduction of paraesthesiae during the technique.
This manoeuvre is usually conducted once only at each treatment session since it is not a comfortable procedure for the patient and the effects of treatment often become fully apparent over the following few days. Between sessions the patient is instructed to continue stretching the tendon to maintain length and mobility.
Although more research is required, a review by Stasinopoulos et al (2005) noted that a combination of eccentric strengthening and stretching exercises achieved better results overall. The stretching exercises included the components of elbow extension with wrist flexion and ulnar deviation. They also compared the outcomes from a home exercise or a supervised exercise programme and, although the results were inconclusive, they were able to suggest that overall a supervised exercise programme achieved better results, in combination with the eccentric strengthening and stretching exercises mentioned above.
The resistant tennis elbow
The short-term relief gained from either injection or physiotherapy is an indication that the causative factors and ideal treatment for tennis elbow still elude us. From clinical experience, and with some support from the discussion above, injection or physiotherapy seem to work well for uncomplicated tennis elbow of recent onset. The chronic nature of the condition, however, means that most of us do not see patients until the condition is well-established. The disappointing results and recurrence of symptoms indicate that there may be one or more components involved in tennis elbow.
The gradual onset of tennis elbow means that problems can coexist within the elbow joint and surrounding neural structures. Pain may restrict the range of active movement and the relative immobilization may produce an associated capsular pattern in the elbow joint. Similarly, dysfunction at one site can cause dysfunction at others and adverse neural tension can be a primary cause or associated cause of tennis elbow (Yaxley & Jull 1993). A cervical lesion can refer pain into the forearm and mimic tennis elbow, or cervical syndromes can coexist with a lesion at the elbow.
The degenerative component of tennis elbow is believed to respond to a combination of eccentric strengthening and stretching exercises. As with other tendinopathies, Stasinopoulos et al (2005) conducted their eccentric training programme for 12 weeks and perseverance with the programme should be expected and encouraged to resolve the condition. The exercises should only be stopped if the pain is very disabling and the guideline for the treatment of tendinopathy can be offered that patients should work up to a level of pain that can be measured on the visual analogue scale as 3–5 (Bahr et al 2006, Cook 4th International Evidence-Based Physical Therapy Conference note 2008).
Nerve entrapment at the elbow may be a complication (Noteboom et al 1994, Hartley 1995). The radial nerve divides into its terminal branches at the elbow and the posterior interosseous nerve passes between the deep and superficial head of supinator. The upper edge of the superficial head of supinator is a thickened fibrous band forming a firm arch known as the arcade of Frohse, which provides a possible site for nerve entrapment.
The musculotendinous, neural, neurological and articular components should be assessed in the resistant tennis elbow, although there is little evidence in the literature to confirm that addressing all possible components gives any better results. Some cases of tennis elbow come to surgery, involving tenotomy of the extensor tendons at the lateral epicondyle.
Transverse frictions to the origin of extensor carpi radialis longus from the supracondylar ridge (Cyriax 1984, Cyriax & Cyriax 1993)
Transverse frictions are the recommended treatment at this site. Position the patient with the elbow supported in 90° of flexion. Sit facing the patient and place the pad of your thumb against the lower third of the lateral supracondylar ridge (Fig. 6.32). Direct the pressure back against the ridge and impart the transverse frictions in a superior inferior direction. Relative rest is advised where functional movements may continue, but no overuse or stretching until pain-free on resisted testing.
 |
| Figure 6.32
Transverse frictions for tennis elbow, supracondylar ridge.
|
Transverse frictions to the body of the common extensor tendon (Cyriax 1984, Cyriax & Cyriax 1993)
This variety of tennis elbow is less common. The area of tenderness is located in the region of the radial head. Injection of the tendon is controversial and treatment is preferably by transverse frictions.
Position the patient with the elbow supported in 90° of flexion and the forearm supported in pronation (Fig. 6.33). Locate the body of the tendon over the radial head. Impart deep transverse frictions across the fibres for 10 min after some analgesia has taken effect. Relative rest is advised where functional movements may continue, but no overuse or stretching until pain-free on resisted testing.
 |
| Figure 6.33
Transverse frictions for tennis elbow, body of the tendon.
|
Transverse frictions to the muscle bellies (Cyriax 1984, Cyriax & Cyriax 1993)
The lesion is in the bellies of the common extensor muscles lying deep to the brachioradialis. This tends to present as an acute lesion following unaccustomed activity but pain may also refer into the area from an acute lesion at the common extensor origin. Treatment with transverse frictions is usually successful and the lesion settles quickly.
Position the patient with the forearm supported with the elbow flexed to 90° and the forearm in the mid-position (Fig. 6.34). Palpate for the site of the lesion deep to brachioradialis. Grasp the affected muscle fibres between a finger and thumb and impart the transverse frictions by a pinching pressure applied up and down in a superior inferior direction. Relative rest is advised where functional movements may continue, but no overuse or stretching until pain-free on resisted testing.
 |
| Figure 6.34
Transverse frictions for tennis elbow, muscle bellies.
|
Golfer’s elbow
Although not as common as tennis elbow, golfer’s elbow has a similar presentation, aetiology, disease process and management.
The patient presents with a gradual onset of pain on the medial aspect of the arm. This may radiate distally, but in general it does not project as far as the pain seen in tennis elbow. The pain is aggravated by use and the elbow is often stiff after rest. Onset of symptoms may be associated with occupational overuse, sporting activities (e.g. tennis, bowling, archery) or hobbies (e.g. knitting, needlework) (Rayan 1992, Kurvers & Verhaar 1995). The motion of throwing may cause golfer’s elbow as it produces a valgus stress at the elbow which has to be supported by the flexor muscles (Ho 1995). On examination, pain on resisted wrist flexion with the elbow extended reproduces the patient’s pain.
The tendons involved in golfer’s elbow control movement at two joints and are susceptible to overuse through overload. Stretching, valgus forces and intrinsic forces from muscle contraction all contribute to the condition (Safran 1995). In the degenerative process of golfer’s elbow tendinosis is evident rather than the acute inflammatory changes of tendinopathy (Bennett 1994, Patten 1995).
Golfer’s elbow, generally speaking, is a less complicated condition to treat than tennis elbow, but coexistent ulnar neuritis (cubital tunnel syndrome) may produce medial elbow pain with tenderness and paraesthesia in the distribution of the ulnar nerve (Kurvers & Verhaar 1995, O’Dwyer & Howie 1995). Some cases of golfer’s elbow come to surgery, involving incision of the flexor tendons around the medial epicondyle, denervation of the epicondyle and transposition of the ulnar nerve.
There are two sites for the lesion: teno-osseous site and musculotendinous site.
Treatment of golfer’s elbow
The common flexor tendon takes origin from the anterior aspect of the medial epicondyle. Palpation will identify the site of the lesion. Treatment may be by either cortico-steroid injection or transverse frictions.
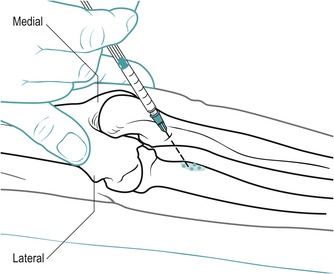
Teno-osseous site (enthesis)
Position the patient with the elbow supported in extension and fully supinated. Locate the anterior aspect of the medial epicondyle and identify the area of tenderness (Fig. 6.35). Insert the needle perpendicular to the facet and deliver the injection by a peppering technique (Fig. 6.36). Bear in mind the position of the ulnar nerve behind the medial epicondyle. The patient is advised to maintain a period of relative rest for approximately 2 weeks following injection.
 |
| Figure 6.35
Injection of golfer’s elbow, teno-osseous site.
|
 |
| Figure 6.36
Injection of golfer’s elbow, teno-osseous site, showing direction of approach and needle position.
|
Transverse frictions for golfer’s elbow, teno-osseous site (Cyriax 1984, Cyriax & Cyriax 1993)
Position the patient in supine lying with the elbow supported in extension and locate the area of tenderness on the anterior aspect of the medial epicondyle (Fig. 6.37). Using an index finger reinforced by the middle finger, and thumb for counterpressure, impart the transverse frictions by applying the pressure down onto the anterior aspect and sweeping transversely across the fibres (Fig. 6.38). Ten minutes’ deep transverse frictions are delivered after the analgesic effect has been achieved. Relative rest is advised where functional movements may continue, but no overuse or stretching until pain-free on resisted testing.
 |
| Figure 6.37
Transverse frictions for golfer’s elbow, teno-osseous site.
|
 |
| Figure 6.38
Transverse frictions for golfer’s elbow, teno-osseous site, to give an indication of the direction of application.
|
Musculotendinous site
Transverse frictions for golfer’s elbow, musculotendinous site
Transverse frictions are considered to be the most effective treatment here (Cyriax 1984, Cyriax & Cyriax 1993). Position yourself and the patient as above and, using the index finger, move 1 cm distally to palpate the musculotendinous junction at the inferior edge of the medial epicondyle (Fig. 6.39). Maintain the pressure against the bone and impart the frictions transversely across the fibres for 10 min after the analgesic effect has been achieved. Relative rest is advised where functional movements may continue, but no overuse or stretching until pain-free on resisted testing.
 |
| Figure 6.39
Transverse frictions for golfer’s elbow, musculotendinous junction.
|
An alternative position may be used for the application of transverse frictions to both sites. The patient is seated on the treatment couch with the shoulder in lateral rotation, the elbow extended and the forearm fully supinated. The clinician stands alongside and facing the patient to support the elbow in extension. Using the other hand, transverse frictions can then be applied transversely across the fibres at each site (Figure 6.40 and Figure 6.41).
 |
| Figure 6.40
Transverse frictions for golfer’s elbow, teno-osseous site (alternative position).
|
 |
| Figure 6.41
Transverse frictions for golfer’s elbow, musculotendinous junction. (Alternative position).
|
Biceps
At the elbow, the lesion lies either in the muscle belly or at the insertion onto the radial tuberosity. The patient complains of pain at the elbow on resisted elbow flexion and resisted supination of the flexed elbow. Passive stretching into elbow extension can also cause pain.
Excessive friction may cause inflammation of the subtendinous biceps bursa and differential diagnosis from bicipital tendinopathy may be difficult. A muddled presentation of signs is found, confirming the diagnosis of bursitis. Pain may be reproduced on resisted elbow flexion, passive elbow extension and passive elbow pronation, as the bursa is squeezed against its insertion.
An injection of corticosteroid is the treatment of choice for the insertion of biceps, since the tendon of insertion lies deeply.
Position the patient in prone lying in the anatomical position. Without changing the position of the glenohumeral joint, carefully pronate the extended forearm keeping your thumb in contact with the radial head to confirm your position. Insert the needle between the radius and ulna approximately 2 cm distal to the radiohumeral joint line until the resistance of the tendon insertion is felt (Fig. 6.42). Deliver the injection by a peppering technique to the tendon and adjacent area if the bursa is also involved (Fig. 6.43). The patient is advised to maintain a period of relative rest for approximately 2 weeks following injection.
 |
| Figure 6.42
Injection of biceps insertion at the radial tuberosity.
|
 |
| Figure 6.43
Injection of biceps insertion at the radial tuberosity, showing direction of approach and needle position.
|
Transverse frictions to the insertion of biceps at the radial tuberosity (Cyriax 1984, Cyriax & Cyriax 1993)
Position the patient with the elbow joint flexed to 90° and supinated. With your thumb, locate the insertion of biceps at the radial tuberosity and apply pressure against it, deeply and laterally (Fig. 6.44). Wrap your fingers around the forearm to provide counterpressure. Deliver the transverse frictions by alternately rotating the patient’s forearm between pronation and supination while maintaining the pressure against the radial tuberosity.
 |
| Figure 6.44
Transverse frictions to the insertion of biceps at the radial tuberosity.
|
If the lesion lies in the muscle belly, the general principles of treatment can be applied (see Ch. 4).
Triceps
Distal rupture of the triceps tendon due to forced overload into extension is uncommon. A triceps muscle lesion is also rare, but would present with posterior elbow pain, increased by resisted elbow extension. The general principles of treatment can be applied.
REFERENCES
Adeniran, A.; Merriam, W.F., Pulled elbow in an adult., J. Bone Joint Surg. 76B (1994) 848–849.
Akeson, W.H.; Amiel, D.; La Violette, D.; et al., The connective tissue response to immobility: an accelerated ageing response, Exp. Gerontol. 3 (1968) 289–301.
Assendelft, W.J.J.; Hay, E.M.; Adshead, R.; et al., Corticosteroid injections for lateral epicondylitis: a systematic overview, Br. J. Gen. Pract. 46 (1996) 209–216.
Bahr, R.; Fossan, B.; Loken, S.; et al., Surgical treatment compared with eccentric training for patellar tendinopathy (jumper’s knee)., J. Bone Joint Surg. 88-A (2006) 1689–1698.
Bennett, J.B., Lateral and medial epicondylitis, Hand Clin. 10 (1994) 157–163.
Bianchi, S.; Martinoli, C., Detection of loose bodies in joints., Radiol. Clin. N. Am. 37 (4) ( 1999) 679–690.
Bisset, L.; Beller, E.; Jull, G.; et al., Mobilisation with movement and exercise, corticosteroid injection or wait and see for tennis elbow: randomised trial, Br. Med. J. ( 2006); 333, 939.
Brukner, P.; Khan, K., Clinical Sports Medicine. 3rd edn. ( 2007)McGraw-Hill, Sydney.
Chard, M.D.; Cawston, T.E.; Riley, G.P.; et al., Rotator cuff degeneration and lateral epicondylitis: a comparative histological study, Ann. Rheum. Dis. 53 (1994) 30–34.
Coonrad, R.W.; Hooper, W.R., Tennis elbow: its course, natural history, conservative and surgical management., J. Bone Joint Surg. 55A (1973) 1177–1182.
Cyriax, J., th ednTextbook of Orthopaedic Medicine. vol.1 ( 1982)Baillière Tindall, London.
Cyriax, J., 11th ednTextbook of Orthopaedic Medicine. vol. 2 ( 1984)Baillière Tindall, London.
Cyriax, J.; Cyriax, P., Cyriax’s Illustrated Manual of Orthopaedic Medicine.. ( 1993)Butterworth Heinemann, Oxford.
Davidson, C.; Ganion, L.; Gehlsen, G.; et al., Rat tendon morphologic and functional changes resulting from soft tissue mobilisation, Med. Sci. Sports Exerc. 29 (3) ( 1997) 313–319.
Drechsler, W.; Knarr, J.; Snyder-Mackler, L., A comparison of two treatment regimes for lateral epicondylitis: a randomised trial of clinical interventions, J. Sport Rehabil. 6 (1997) 226–234.
Edelson, G.; Kunos, C.A.; Vigder, F.; et al., Bony changes at the lateral epicondyle of possible significance in tennis elbow syndrome, J. Shoulder Elbow Surg. 10 (2001) 158–164.
Ernst, E., Conservative therapy for tennis elbow, Br. J. Clin. Pract. 46 (1992) 55–57.
Foley, A.E., Tennis elbow, Am. Fam. Physician 48 (1993) 281–288.
Gabel, G.T., Acute and chronic tendinopathies at the elbow, Curr. Opin. Rheumatol. 11 (2) ( 1999) 138–143.
Gehlsen, G.; Ganion, L.; Helfst, R., Fibroblast responses to variation in soft tissue mobilisation pressure, Med. Sci. Sports Exerc. 31 (4) ( 1998) 531–535.
Gellman, H., Tennis elbow lateral epicondylitis, Orthop. Clin. N. Am. 23 (1992) 75–82.
Greenfield, C.; Webster, V., Chronic lateral epicondylitis: survey of current practice in the outpatient departments in Scotland., Physiotherapy 88 (10) ( 2002) 578–594.
Hardy, R.H., Pulled elbow., J. R. Coll. Gen. Pract. 28 (1978) 224–226.
Hart, L.E., Commentary on corticosteroid injections, physiotherapy or a wait-and-see policy for lateral epicondylitis, Clin. J. Sport Med. 12 (6) ( 2002) 403–404.
Hartley, A., Practical Joint Assessment, Upper Quadrant. 2nd edn. ( 1995)Mosby, London.
Ho, C.P., Sports and occupational injuries of the elbow: MR imaging findings., Am. J. Roentgenol. 164 (1995) 1465–1471.
Hoppmann, R.A., Diagnosis and management of common tendinopathy and bursitis syndromes., J. S. C. Med. Assoc. 89 (1993) 531–535.
Joji, S.; Murakami, T.; Murao, T., Osteochondritis dissecans developing in the trochlea humeri: a case report, J. Shoulder Elbow Surg. 10 (3) ( 2001) 295–297.
Katarincic, J.A.; Weiss, A.-P.C.; Akelman, E., Lateral epicondylitis tennis elbow: a review., R. I. Med. 75 (1992) 541–544.
Kesson, M.; Atkins, E.; Davies, I., Musculoskeletal Injection Skills. ( 2003)Butterworth Heinemann, Oxford.
Khan, K.M.; Cook, J.L., Overuse tendon injuries: where does the pain come from?Sports Med. Arthroscopic Rev. 8 (2000) 17–31.
Kohlhaas, A.R.; Roeder, J., Tee shirt management of nursemaid’s elbow., Am. J. Orthop. 24 (1995) 74.
Kurvers, H.; Verhaar, J., The results of operative treatment of medial epicondylitis., J. Bone Joint Surg. 77A (1995) 1374–1379.
Mills, G.P., Treatment of tennis elbow, Br. Med. J. 1 (1928) 12–13.
Miyasaka, K.C., Anatomy of the elbow., Orthop. Clin. N. Am. 30 (1) ( 1999) 1–13.
Newcomer, K.L.; Laskowski, E.R.; Idank, D.M.; et al., Corticosteroid injection in early treatment of lateral epicondylitis., Clin. J. Sports Med. 11 (4) ( 2001) 214–222.
Nicola, T.L., Elbow injuries in athletes, Prim. Care 19 (1992) 283–302.
Nimgade, A.; Sullivan, M.; Goldman, R., Physiotherapy, steroid injections, or rest for lateral epicondylosis?What the evidence suggests. Pain Pract. 5 (3) ( 2005) 203–215.
Noteboom, T.; Cruver, R.; Keller, J.; et al., Tennis elbow: a review, J. Orthop. Sports Phys. Ther. 19 (1994) 357–366.
O’Dwyer, K.J.; Howie, C.R., Medial epicondylitis of the elbow, Int. Orthop. 19 (1995) 69–71.
Palastanga, N.; Field, D.; Soames, R., Anatomy and Human Movement. 5th edn. ( 2006)Butterworth-Heinemann, Edinburgh.
Patten, R.M., Overuse syndromes and injuries involving the elbow: MR imaging findings., Am. J. Roentgenol. 164 (1995) 1205–1211.
Pienimäki, T.T.; Siira, P.T.; Vanharanta, H., Chronic medial and lateral epicondylitis: a comparison of pain, disability and function, Arch. Phys. Med. Rehabil. 83 (2002) 317–321.
Rayan, G.M., Archery-related injuries of the hand, forearm and elbow, South. Med. J. 85 (1992) 961–964.
Safran, M.R., Elbow injuries in the athlete, Clin. Orthop. Relat. Res. 310 (1995) 257–277.
Saotome K, Tamai K, Osada D et al., 2006 Histologic classification of loose bodies in osteoarthrosis. J. Orthop. Sci. 11(6), 607–613.
Saunders, S., Orthopaedic Medicine Course Manual. ( 2000)Saunders, London.
Schnatz, P.; Steiner, C., Tennis elbow: a biomechanical and therapeutic approach, J. Am. Osteopath. Assoc. 93 (1993) 778–788.
Smidt, N.; van der Windt, D.A.; Assendelft, W.J.; et al., Interobserver reproducibility of the assessment of severity of complaints, grip strength and pressure pain threshold in patients with lateral epicondylitis, Arch. Phys. Med. Rehabil. 83 (2002) 1145–1150.
Smidt, N.; van der Windt, D.A.; Assendelft, W.J., Corticosteroid injections, physiotherapy or wait-and-see policy for lateral epicondylitis, Clin. J. Sport Med. 12 (6) ( 2002) 403–404.
Smidt, N.; Assendelft, W.J.; Arola, H.; et al., Effectiveness of physiotherapy for lateral epicondylitis: a systematic review, Ann. Med. 35 (1) ( 2003) 51–62.
Sölveborn, S.A.; Buch, F.; Mallmin, H.; et al., Cortisone injection with anaesthetic additives for radial epicondylalgia tennis elbow, Clin. Orthop. Relat. Res. 316 (1995) 99–105.
Standring, S., Gray’s Anatomy: the Anatomical Basis of Clinical Practice. 14th edn. ( 2009)Churchill Livingstone, Edinburgh.
Stasinopoulos, D.; Stasinopoulos, K.; Johnson, M., An exercise programme for the management of lateral elbow tendinopathy, Br. J. Sports Med. 39 (2005) 944–947.
Stratford, P.W.; Levy, D.R.; Gauldie, S.; et al., The evaluation of phonophoresis and friction massage as treatments for extensor carpi radialis tendinopathy: a randomised controlled trial., Physiother. Can. 41 (2) ( 1989) 93–99.
Tonks, J.H.; Pai, S.K.; Murali, S.R., Steroid injection therapy is the best conservative treatment for lateral epicondylitis: a prospective randomised controlled trial, Int. J. Clin. Pract. 61 (2) ( 2006) 240–246.
Vasseljen, O., Low level laser versus traditional physiotherapy in the treatment of tennis elbow., Physiotherapy 78 (1992) 329–334.
Verhaar, J.; Walenkamp, G.; Kester, A.; et al., Lateral extensor release for tennis elbow., J. Bone Joint Surg. 75A (1993) 1034–1043.
Verhaar, J.A.N.; Walenkamp, G.H.I.M.; van Mameren, H.; et al., Local corticosteroid injection versus Cyriax-type physiotherapy for tennis elbow., J. Bone Joint Surg. 78B (1996) 128–132.
Yaxley, G.A.; Jull, G.A., Adverse neural tension in the neural system: a preliminary study of tennis elbow., Aust J. Physiother. 39 (1993) 15–22.