7
The ECG in Patients with Palpitations or Syncope
‘Palpitations’ means different things to different people, but essentially it means an awareness of the heartbeat. ‘Syncope’ means sudden loss of consciousness. The only way of being certain that a cardiac problem is the cause of either phenomenon is to record an ECG when the patient is having a typical attack, but this is seldom possible. Nevertheless, the ECG can be helpful, even when the patient is well.
THE ECG WHEN THE PATIENT HAS NO SYMPTOMS
If a patient is well at the time of recording, four possible ECG patterns can point to a diagnosis:
NORMAL ECGs
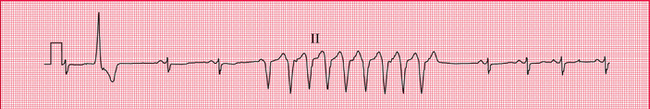
Symptoms may not be due to heart disease – the patient may have epilepsy or some other condition. However, a normal ECG does not rule out a paroxysmal arrhythmia, and the patient′s description of his or her symptoms may be crucial. For example, if the patient′s attacks are associated with exercise (think of anaemia) or anxiety, and the palpitations build up and slow down, sinus tachycardia is likely to be the cause of the symptoms. In paroxysmal tachycardia, the attack begins suddenly, often for no obvious reason, and may stop suddenly. Ambulatory recording over 24 h, using, for example, the Holter technique, may be necessary to obtain a record of an attack ( Fig. 7.1).
PATTERNS SUGGESTING CARDIAC DISEASE
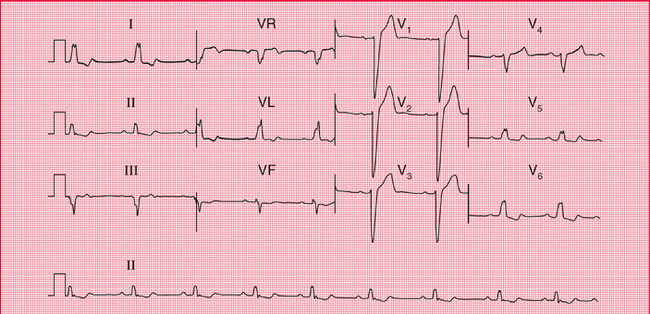
Marked T wave inversion may suggest either left ventricular hypertrophy or left bundle branch block, which may be due to aortic stenosis; or right ventricular hypertrophy, which may be due to pulmonary hypertension. In a young person, who is unlikely to have coronary disease, this pattern pattern suggests hypertrophic cardiomyopathy ( Fig. 7.2), which is associated with arrhythmias, syncope and sudden death.
PATTERNS SUGGESTING PAROXYSMAL TACHYCARDIA
Pre-excitation syndromes
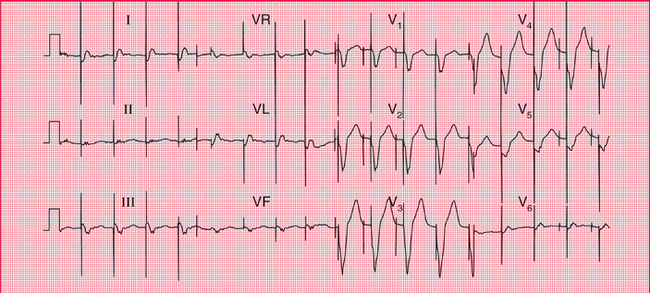
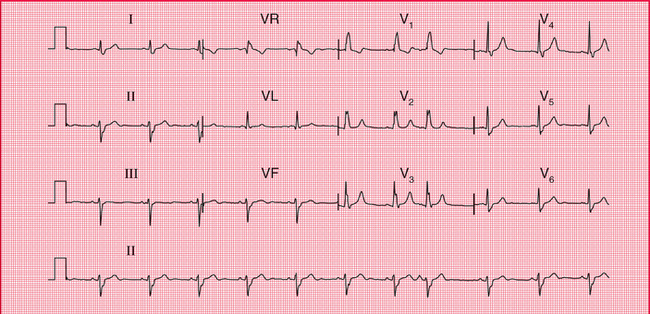
In the WPW syndrome, the abnormal pathway connects the atrium and the ventricle, and the QRS complex is wide, with a slurred upstroke. In the WPW syndrome type A, the pathway is left-sided, connecting the left atrium and left ventricle, and causes a dominant R wave in lead V1 ( Fig. 7.3; for another example see Fig. 3.28). This may be confused with right ventricular hypertrophy. Less commonly, the abnormal pathway can be right-sided, connecting the right atrium and right ventricle, and this is called the WPW syndrome type B ( Fig. 7.4). Here, lead V1 has no dominant R wave but has a deep S wave, and there is anterior T wave inversion, which may lead to a mistaken diagnosis of anterior ischaemia. The wide QRS complex seen in both types of the WPW syndrome may also lead to a mistaken diagnosis of bundle branch block, although the characteristic ‘M’ pattern of the QRS complexes in left bundle branch block is not seen in the WPW syndrome.
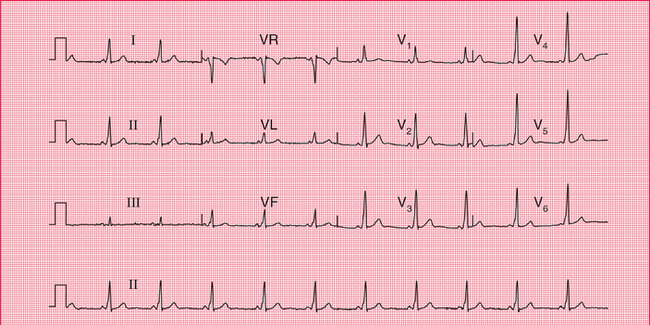
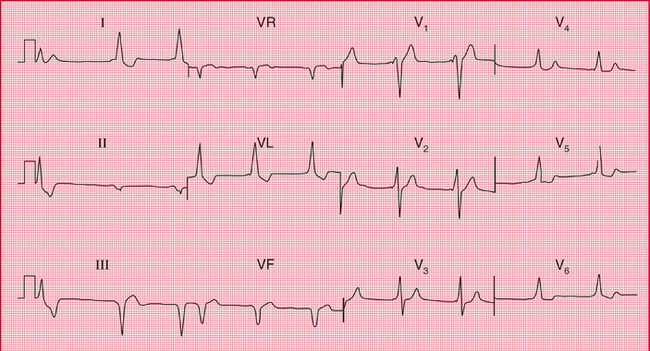
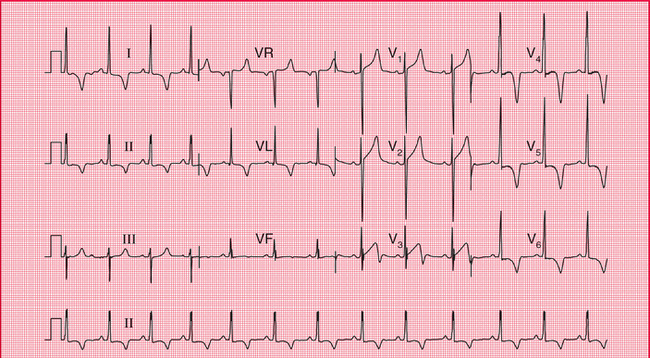
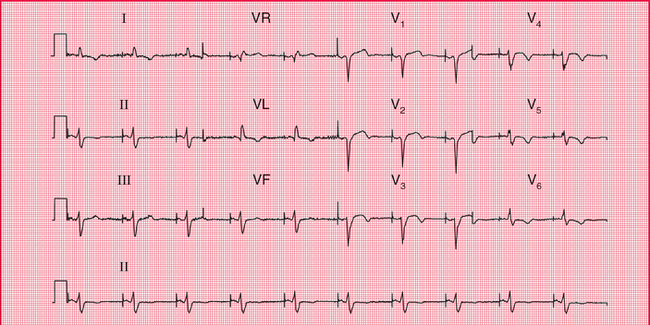
Fig. 7.4 The Wolff–Parkinson–White syndrome type B
Note
• Sinus rhythm, rate 55/min – P waves best seen in lead V1
• The first complex is probably a ventricular extrasystole
• Broad QRS complexes (160 ms) with a slurred upstroke (delta wave), seen best in leads V2–V4
• Inverted T waves in leads I, II and VL, and biphasic T waves in leads V5–V6
• The small second and third complexes in lead II appear to be due to a technical error
In the LGL syndrome the abnormal pathway connects the atria to the His bundle, so there is a short PR interval but a normal QRS complex ( Fig. 7.5).
Long QT interval
The QT interval varies with the heart rate (and also with gender and the time of day). The corrected interval (QTc) can be calculated using Bazett′s formula:
A QTc interval longer than 450 ms is likely to be abnormal. QT interval prolongation can be congenital, but is most often due to drugs, particularly to antiarrhythmic drugs ( Box 7.1 and Fig. 7.6).
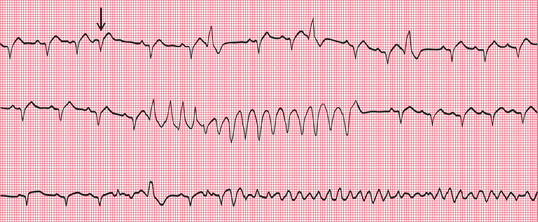
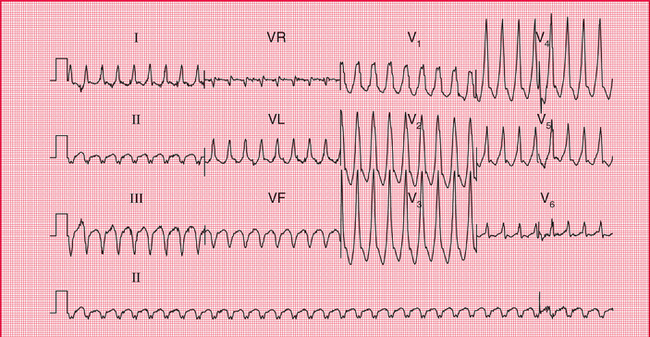
Whatever its cause, a corrected QT interval of 500 ms or longer can predispose to paroxysmal ventricular tachycardia of a particular type called ‘torsade de pointes’, which can cause either symptoms typical of paroxysmal tachycardia or sudden death. Figure 7.7 shows a continuous ECG from a patient who was being treated with an antiarrhythmic drug and who developed ventricular fibrillation while being monitored. A few seconds before the cardiac arrest, he developed a transient broad complex tachycardia in which the QRS complexes were initially upright but then changed, to become downward-pointing. This is typical of ‘torsade de pointes’ ventricular tachycardia.
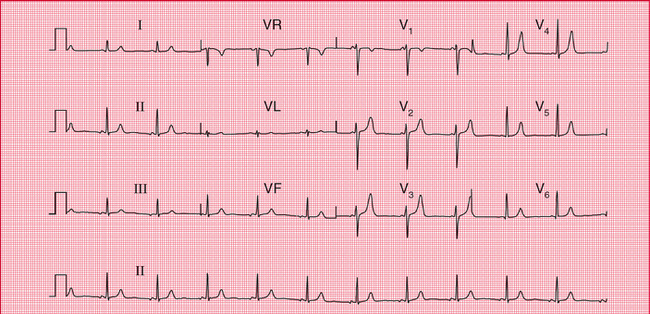
Sinoatrial disease
Sinoatrial disease, known as the ‘sick sinus’ syndrome, typically causes an inappropriate sinus bradycardia but is often asymptomatic ( Fig. 7.8). It can also be associated with a variety of conduction problems, escape rhythms or paroxysmal tachycardia ( Box 7.2). Patients may therefore complain of either dizziness, syncope or symptoms suggesting paroxysmal tachycardia.
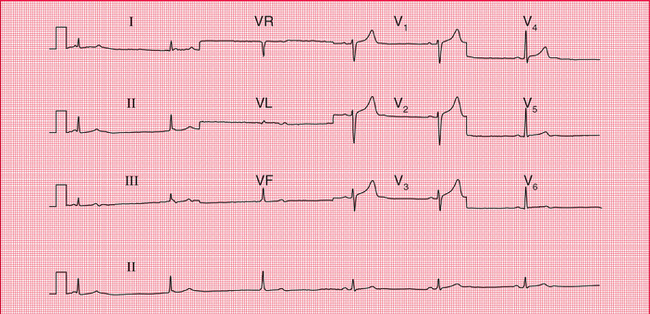
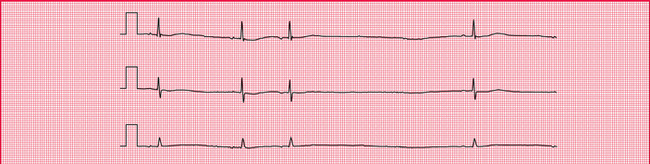
Fig. 7.8 Sick sinus syndrome
Note
• Look at the rhythm strip first
• The first three beats are due to AV nodal escape, with a rate of 35/min
• P waves can be seen immediately before or immediately after the QRS complex
• The next three beats are in sinus rhythm, rate 38/min
• The QRS complexes and T waves are normal
• A combination of sinus bradycardia and AV nodal escape is typical of the sick sinus syndrome
PATTERNS SUGGESTING SYNCOPE DUE TO BRADYCARDIA
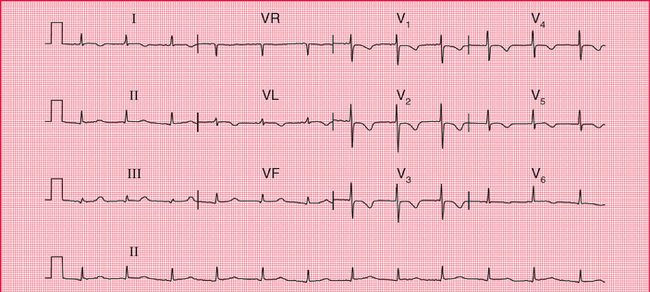
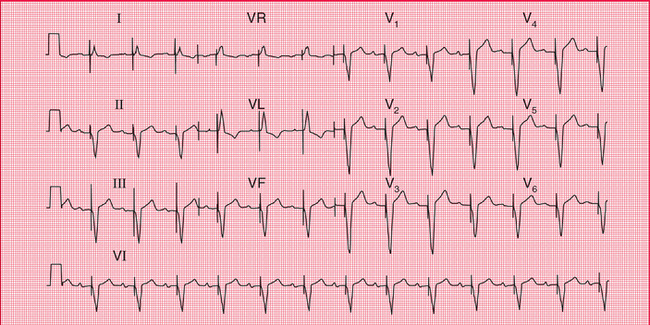
In apparently healthy subjects who complain of attacks of dizziness, the resting ECG when asymptomatic may show axis deviation, sick sinus syndrome or any variety of heart block. First degree block, second degree block of the Wenckebach (Mobitz type 1) variety, and bundle branch block do not in themselves indicate treatment, and neither do combinations of these blocks, such as first degree block and bundle branch block ( Fig. 7.9), or bifascicular block (left anterior hemiblock and right bundle branch block, Fig. 7.10). However, such combinations may also be associated with higher degrees of block, and ambulatory recording may be considered to see if second or third degree block is occurring intermittently.
It is important to consider the possible underlying causes of heart block, and these are summarized in Box 7.3.
THE ECG WHEN THE PATIENT HAS SYMPTOMS
PAROXYSMAL TACHYCARDIA
It is not possible to tell from a patient′s symptoms whether extrasystoles or a paroxysmal tachycardia are supraventricular or ventricular in origin – although paroxysmal ventricular tachycardia is perhaps more likely to cause dizziness or syncope than paroxysmal supraventricular tachycardia.
Narrow complex tachycardias may indicate:
The ECG characteristics of the supraventricular rhythms are summarized in the Reminders on page 165.
Broad complex tachycardias indicate:
REMINDERS
THE VENTRICULAR RHYTHMS
It can be very difficult to differentiate between the broad complexes of a supraventricular tachycardia with bundle branch block and ventricular tachycardia, but the following Reminders should help.
REMINDERS
THE SUPRAVENTRICULAR RHYTHMS
• In general, supraventricular rhythms have narrow (less than 120 ms) QRS complexes, the exceptions being bundle branch block and the WPW syndrome, in which wide QRS complexes are seen.
• Supraventricular extrasystoles:
− QRS complex rate greater than 150/min
− abnormal P waves, usually with short PR intervals
− usually one P wave per QRS complex, but sometimes P wave rate 200–240/min, with 2:1 block.
− the most irregular rhythm of all
− QRS complex rate characteristically over 160/min without treatment, but can be slower
− no P waves identifiable, but there is a varying, completely irregular baseline.
Figure 7.11 shows an ECG with all the usual features of ventricular tachycardia – left axis deviation, QRS complexes with duration 180 ms, and all the complexes in the chest leads pointing upwards.
REMINDERS
BROAD COMPLEX TACHYCARDIAS
• When seen in the context of acute myocardial infarction, a broad complex tachycardia is likely to be ventricular in origin.
• Comparison with a record made during sinus rhythm (if available) will show if bundle branch block is normally present.
• Left axis deviation with right bundle branch block is usually indicates a ventricular problem.
• Very wide (greater than 160 ms) QRS complexes usually indicate ventricular tachycardia.
• Concordance – ventricular tachycardia is likely if the QRS complexes all point predominantly upwards or downwards in the chest leads.
• An irregular broad complex rhythm is likely to be atrial fibrillation with bundle branch block, or atrial fibrillation in the WPW syndrome (a dangerous combination).
INTERMITTENT BRADYCARDIA
A low rate can be due to second or third degree heart block (see pp. 37–42) or to ‘pauses’, when the sinoatrial node fails to depolarize. This is seen in the sick sinus syndrome. Figure 7.12 shows an ambulatory record from a patient with sick sinus syndrome, who complained of attacks of dizziness which were due to sinus pauses of 3.3 s.
PACEMAKERS
Pacemakers produce a small electrical discharge that either replaces the function of the sinoatrial node or bypasses a blocked His bundle. The sophisticated design of pacemakers enables them to mimic many of the functions of the normal heart.
1. The first letter describes the chamber(s) paced (A for right atrium, V for right ventricle or D for dual, i.e. both chambers).
2. The second letter describes the chambers sensed (A, V or D).
3. The third letter describes the response to a sensed event (A, V or D for pacing; I for pacemaker inhibition).
4. The fourth letter (R) is used when the rate modulation is programmable.
Thus, ‘VVI’ means that the pacemaker paces and senses the right ventricle. When no spontaneous activity is sensed, the pacemaker stimulates the right ventricle; and when spontaneous activity is sensed, the pacemaker is inhibited. The ECG looks like that in Figure 7.13.
‘AAI’ means that the pacemaker has a single lead in the atrium, to both sense and pace it ( Fig. 7.14). If the pacemaker does not sense spontaneous atrial depolarization, it stimulates the atrium; and when there is spontaneous depolarization, the pacemaker is inhibited.
‘DDD’ means that there are pacemaker leads in both the right atrium and the right ventricle, and both chambers are sensed and paced. If no atrial activity is sensed within a predetermined period, the atrial pacing lead will pace. A maximum PR interval is also predetermined, and if no ventricular beat is sensed, the ventricle will be paced. Figure 7.13 could be the result of simple WI pacing, or could be the result of atrial sensing and ventricular pacing, the ventricular rate ‘following’ the atrial rate. A chest X-ray would show whether there were one or two pacing leads. Figure 7.15 shows both atrial and ventricular pacing.
CARDIAC ARREST
Cardiac arrest can be classified according to whether the rhythm is ‘shockable’ (i.e. correctable by DC cardioversion) or nonshockable. In either case, the first part of the treatment is a precordial thump and cardiopulmonary resuscitation at 30 compressions for each two ventilations.
3. Resume chest compressions at 30:2 for 2 min, then check the rhythm.
4. If unsuccessful, defibrillate at 360 J.
5. If unsuccessful, give adrenaline 1 mg i.v.
7. 2 min of cardiopulmonary rescuscitation (CPR).
8. If VF or pulseless VT persists, give amiodarone 300 mg i.v.
9. Give further shocks after 2-min periods of CPR, with adrenaline 1 mg i.v. before alternate shocks.
10. For refractory VF, give magnesium sulfate 2 g i.v. bolus (8 mmol).
Particularly in cases of PEA, consider possible reversible causes of cardiac arrest, all of which begin with H or T and are listed in Box 7.4.