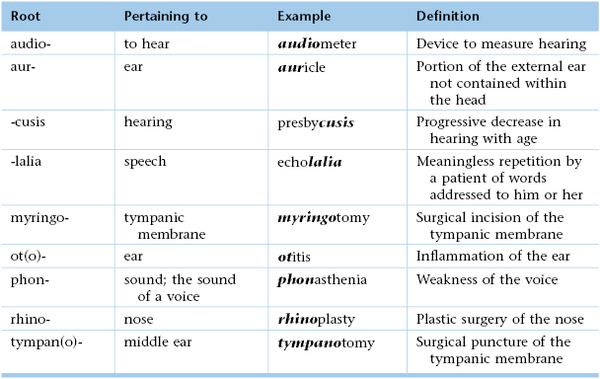
Chapter 8
The Ear and Nose
Yet it was not possible for me to say to people, “Speak louder, shout, for I am deaf. … Alas! how could I declare the weakness of a sense which in me ought to be more acute than in others—a sense which formerly I possessed in highest perfection, a perfection such as few in my profession enjoy, or ever have enjoyed.
Ludwig van Beethoven (1770–1827)
General Considerations
Most people are fortunate to hear the sounds of music, noise, and, above all, speech. Sometimes “silence is golden,” but silence can be golden only when a person can choose not to hear.
Although normal children are born with the apparatus necessary to produce speech, they are not born with speech. The ear and brain integrate and process sound, enabling the child to learn to imitate it. If sound cannot be heard, it cannot be imitated. Sounds will not become words; words will not become sentences; sentences will not become speech; speech will not become language.
Hearing is a perceptual process. To illustrate this concept, consider tinnitus as an example. Tinnitus, the name given to a sensation of sound in one or both ears, commonly accompanies deafness. When tinnitus is present, there is nearly always some degree of hearing loss. Conversely, when there is no appreciable hearing loss, there is rarely tinnitus. However, children who are born deaf do not complain of tinnitus.
Structure and Physiology
The Ear
The ear can be divided into the following four parts:
A cross section through the ear is illustrated in Figure 8-1.
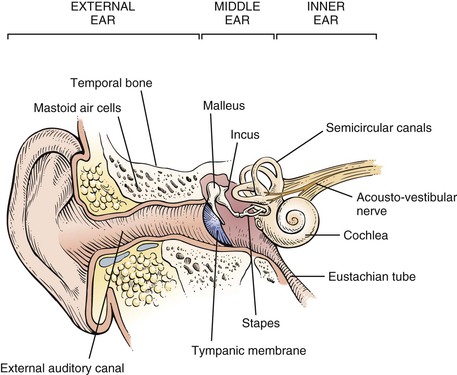
Figure 8–1 Cross-sectional view through the ear.
The external ear consists of the pinna and the external auditory canal. The pinna is composed of elastic cartilage and skin. Figure 8-2 illustrates the parts of the pinna.
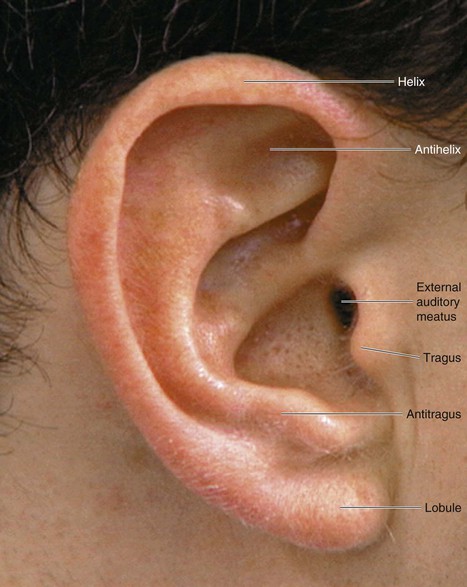
Figure 8–2 Landmarks of the pinna.
The external auditory canal is approximately 1 inch in length. Its outer third is cartilaginous, and its inner two thirds are composed of bone. Within the cartilaginous portion, there are hair follicles; pilosebaceous glands; and ceruminous, or wax-producing, glands. Secretions of these ceruminous glands, debris, and desquamated keratin are “earwax.” The glands secrete their product around the base of the hairs, as depicted in Figure 8-3. Figure 8-4 shows earwax in the external ear canal. Earwax color and consistency depend on the type of cerumen secreted, the amount of keratin present, and the presence of debris. The soft, brown form shown here is the most common type. The cartilaginous portion of the ear is continuous with the pinna. The canal curves slightly, being directed forward and downward. The innervation to most of the external canal is through the trigeminal, or fifth cranial, nerve. The innermost portion of the canal is innervated by the vagus, or tenth cranial, nerve.1
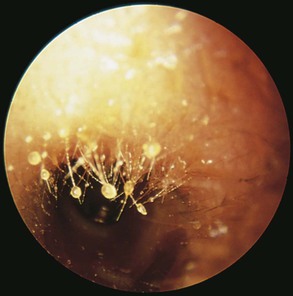
Figure 8–3 Earwax on the base of hairs.
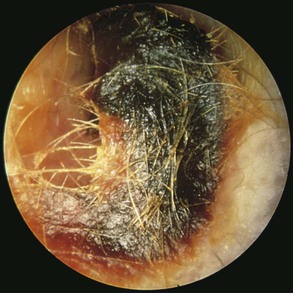
Figure 8–4 Earwax in the external ear canal.
The middle ear, or tympanic cavity, consists of connections to the mastoid antrum and to its connecting air cells and, through the eustachian tube, to the nasopharynx. The function of the eustachian tube is to provide an air passage from the nasopharynx to the ear to equalize pressure on both sides of the tympanic membrane. The eustachian tube is normally closed but opens during swallowing and yawning.
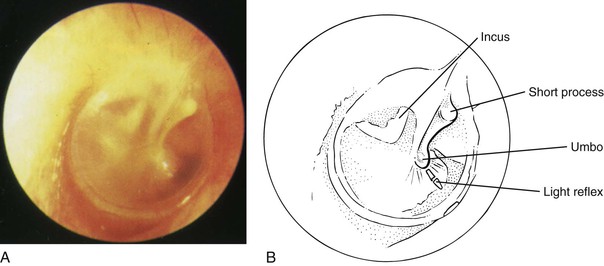
The tympanic membrane forms the lateral boundary of the middle ear. The medial boundary is formed by the cochlea. The tympanic membrane is gray, with blood vessels at its periphery. It is composed of two parts: the pars flaccida and the pars tensa. The pars flaccida is the upper, smaller portion of the tympanic membrane. The pars tensa comprises the remainder of the membrane. The handle of the malleus is a prominent landmark and divides the pars tensa into the anterior and posterior folds. The tympanic membrane is set slightly at an angle to the external canal. The inferior portion is more medial than is the superior portion. Figure 8-5 illustrates the left tympanic membrane.
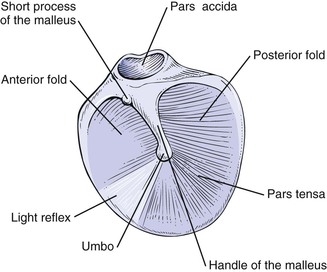
Figure 8–5 Landmarks of the left tympanic membrane.
Sound is conducted from the tympanic membrane to the inner ear by three auditory ossicles: the malleus, the incus, and the stapes. The malleus is the largest ossicle. At its upper end is the short process, which appears as a tiny knob. The handle (long process) of the malleus, or manubrium, extends downward to its tip, called the umbo. The short process and the handle of the malleus attach directly to the tympanic membrane. At the other end of the malleus is its head, which articulates with the incus. The incus then articulates with the head of the stapes, the footplate of which attaches to the oval window of the inner ear.
The middle ear also contains two muscles: the tensor tympani and the stapedius. The tensor tympani muscle attaches to the malleus, and the stapedius muscle attaches to the neck of the stapes. The tensor tympani muscle is innervated by the trigeminal nerve, and the stapedius muscle is innervated by the facial, or seventh cranial, nerve. Both muscles contract in response to high-intensity sound.
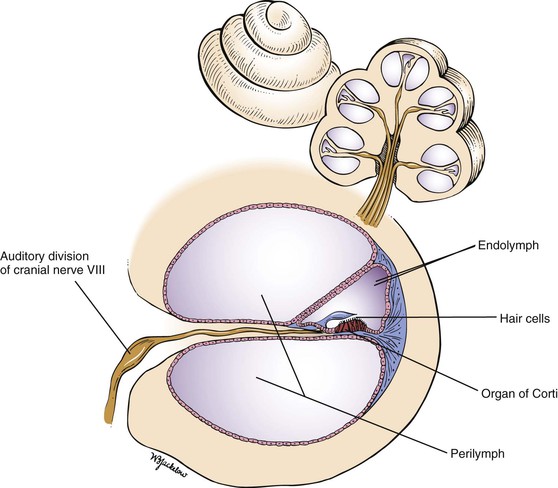
The inner ear is the end-organ for hearing and equilibrium. It is situated in the petrous portion of the temporal bone and consists of the three semicircular canals, the vestibule, and the cochlea. Each of these structures is made up of three parts: the osseous labyrinth, the membranous labyrinth, and the space between. The osseous labyrinth is the outer bone casing. The inner membranous labyrinth is within the osseous labyrinth and contains a fluid called endolymph and the sensory structures. The space between these two labyrinths is filled with another fluid, called perilymph. A cross section through this area is illustrated in Figure 8-6.
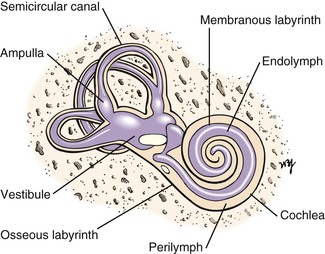
Figure 8–6 Cross sectional view through the cochlea.
The three semicircular canals are directed posteriorly, superiorly, and horizontally. Each canal has a dilated end, the ampulla, which is the sensory end-organ for balance.
The cochlea is a snail shell–shaped structure composed of  turns. Within its membranous labyrinth is the end-organ for hearing. The acoustic, or eighth cranial, nerve consists of two parts: the vestibular and cochlear divisions. These connect to the semicircular canals and cochlea, respectively. They join and pass through the internal auditory meatus to the brain stem.
turns. Within its membranous labyrinth is the end-organ for hearing. The acoustic, or eighth cranial, nerve consists of two parts: the vestibular and cochlear divisions. These connect to the semicircular canals and cochlea, respectively. They join and pass through the internal auditory meatus to the brain stem.
Sound waves stimulate the afferent fibers either by bone conduction (BC) or by air conduction (AC). BC is directly through the bones of the skull. AC is through the external auditory canal, tympanic membrane, and ossicles to the oval window. Most hearing is mediated by AC.
Sound waves set up vibrations that enter the external canal and are transmitted to the ossicles, which vibrate. This vibration causes an inward motion of the footplate of the stapes and deforms the oval window. Waves are created in the perilymphatic fluid of the labyrinth. These fluid motion changes are transmitted in a wavelike manner to the endolymphatic fluid, which causes distortion of the hair cells of the organ of Corti. These hair cells convert the mechanical force into an electrochemical signal that is propagated down the acoustic nerve and is ultimately interpreted as sound. It has been estimated that there are more than 30,000 of these afferent hair fibers, which constitute the auditory division. After many synapses, the impulse reaches the temporal cortex, where the appreciation of the sound occurs. A cross section through the cochlear duct is shown in Figure 8-7.
The sense of balance is achieved by visual, vestibular, and proprioceptive2 senses. The loss of one of these senses frequently goes unnoticed. The vestibular apparatus appears to be the most important. Motion within the endolymphatic fluid stimulates the hair cells in the ampulla of the semicircular canals. Electrical impulses are transmitted to the vestibular portion of the eighth cranial nerve. Synapses occur in the vestibular and oculomotor nuclei, which send efferent fibers to the extraocular and skeletal muscles. This produces a deviation of the eyes with rapid compensatory motions to maintain gaze and increased tone in the skeletal muscles.
Any alteration in the endolymphatic mechanism may affect the control of the eyes. Nystagmus is an involuntary, rapid back-and-forth eye motion, which can be horizontal, vertical, rotatory, or mixed. The direction of the nystagmus is determined by the direction of the quick component. Abnormalities of the labyrinth tend to produce horizontal nystagmus; brain-stem disorders often produce vertical nystagmus; and retinal lesions may produce ocular nystagmus, which is slow and produces an irregular, searching quality to the eyes.
The Nose
The external nasal skeleton consists of the nasal bones, part of the maxilla, and the cartilage. The upper third of the skeleton is composed of nasal bones, which articulate with the maxilla and frontal bones. The lower two thirds is made of cartilage.
The internal portion of the nose consists of two cavities divided by the nasal septum, which forms the medial wall of the nasal cavity. Projecting from the lateral wall are three turbinates, or conchae. The inferior turbinate is the largest and contains semierectile tissue. Inferior to each turbinate are openings to the paranasal sinuses; each opening is known as a meatus. Each meatus is named for the turbinate above it. The nasolacrimal duct empties into the inferior meatus. The middle meatus, below the middle turbinate, contains the openings of the frontal, maxillary, and anterior ethmoid sinuses. The posterior ethmoid sinus drains into the superior meatus. The olfactory region is located high in the nose between the nasal septum and the superior turbinate. Figure 8-8 illustrates the lateral wall of the nose.
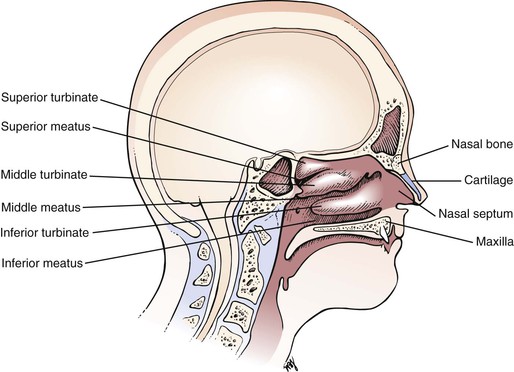
Figure 8–8 Lateral wall of the nose.
The blood supply to the nose is derived from the internal and external carotid arteries. The turbinates are vascular and contain large vascular spaces. The blood vessels of the anterior nasal septum meet at an area approximately 1 inch (2.54 cm) from the mucocutaneous junction, known as Little‘s area. This is the area usually responsible for epistaxis, or nosebleed. The blood vessels are under autonomic nervous system control. If there is an excess of sympathetic stimulation, the blood vessels constrict, and the vascular spaces in the turbinates shrink. If there is an increase in parasympathetic tone, the blood pools in the turbinates, resulting in their swelling, obstruction to airflow, and elaboration of a watery discharge.
The nerve supply to the internal area of the nose is from branches of the trigeminal nerve. The olfactory epithelium is supplied by the olfactory, or first cranial, nerve. Moist air with the dissolved odorous particles acts as a stimulus. The nerve fibers from this area pierce the cribriform plate to the olfactory bulb in the brain. In humans, the olfactory receptors’ ability to discern a stimulus diminishes rapidly with exposure to the stimulus.
The main functions of the nose are to provide the following:
The inspired air flows above and below the middle turbinate. This produces eddy currents that serve to protect the olfactory epithelium in the superior portion of the nose. The nasal mucosa produces mucus, which increases the relative humidity to nearly 100%. This prevents the epithelium from drying out and helps prevent possible infection. The air, by its circulation around the conchae, is warmed to nearly body temperature by the time it enters the nasopharynx. The mucus and the nasal hairs, or vibrissae, prevent particulate matter from entering the distal respiratory tract. The mucous blanket is swept posteriorly by the cilia and is swallowed. The mucus also contains immunoglobulins and enzymes, which serve as a line of defense.
The four paranasal sinuses of the head—the maxillary, the ethmoid, the frontal, and the sphenoid—are air-filled cavities lined with mucous membranes. The maxillary sinus is the largest and is bounded by the eye, the cheek, the nasal cavity, and the hard palate. The ethmoid sinuses are multiple and are present in the ethmoid bone, which lies medial to the orbit and extends to the pituitary fossa. The frontal sinus is located above the ethmoid sinuses and is bounded by the forehead, the orbit, and the anterior cranial fossa. Behind the ethmoid sinuses is the sphenoid sinus. The paranasal sinuses have no known functions. The maxillary, frontal, and ethmoid sinuses and their connections to the nose are illustrated in Figure 8-9.
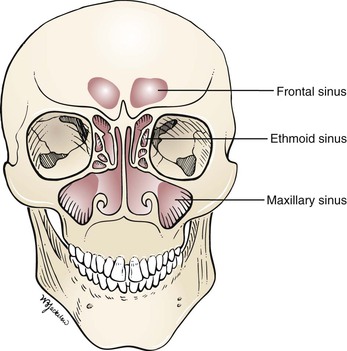
Figure 8–9 Nasal sinuses.
Review of Specific Symptoms
The Ear
The major symptoms of ear disease are the following:
Hearing Loss
Hearing loss may be unilateral or bilateral and may develop slowly or occur suddenly. For any patient with a hearing loss, ask the following questions:
“Is the hearing loss in one ear?”
“For how long have you been aware of a loss of hearing?”
“Is there a family history of hearing loss?”
“What type of work do you do?” “What other work have you done?”
“What types of hobbies do you have?”
“Have you noticed that you can hear better when it is noisy?”
“What kind of medications are you currently taking?”
“Do you know if you have ever been given an antibiotic called streptomycin or gentamicin?”
Occupational history is extremely important to ascertain. Patients with otosclerosis3 can often hear better in a noisy environment. Drugs are well known to cause sudden bilateral hearing loss. Salicylates and diuretics such as furosemide and ethacrynic acid may produce transient loss of hearing when ingested in high doses. The aminoglycoside antibiotics such as streptomycin and gentamicin can destroy the hair cells of the organ of Corti and cause permanent hearing loss. An anticancer medication, cisplatin, is also linked to severe ototoxicity.
There are two main types of hearing loss: conductive and sensorineural. Any condition that interferes with or blocks the transmission of sound waves from the external ear to the inner ear may result in a conductive hearing loss. Blockage may occur as a result of cerumen (earwax), foreign bodies, infection, or congenital abnormalities. Often the position of the cerumen is more important than the amount present. Not infrequently, a small amount of cerumen lying against the tympanic membrane can produce significant hearing loss. Blockage by foreign bodies occurs primarily in 2- to 5-year-old children. Once children discover the external canal, they may experiment and place beads or other objects inside. Figure 8-10 shows a clear plastic bead in the external canal of a young child. Effusions from infections in the middle ear represent one of the most common causes of conductive deafness among children 4 to 15 years of age. The fluid impedes the transmission of sound impulses by the tympanic membrane and the ossicles. Otosclerosis is the main cause of conductive hearing loss in individuals 15 to 50 years of age. With the exception of otosclerosis, conditions causing a conductive hearing loss produce alterations in the appearance of the tympanic membrane.

Figure 8–10 Clear plastic bead in the external ear canal.
Sensorineural hearing loss is caused by a disease process in the inner ear structures or auditory nerve. These conditions may be congenital or acquired, with delayed onset. Congenital deafness accounts for 50% of all deafness in children. In many cases of congenital sensorineural hearing loss, no other congenital abnormality is noted. At other times, deafness may accompany other defects, especially in the kidney. Infection with rubella during gestation accounts for most cases of sensorineural deafness that are caused by anomalous development of the fetus’s cochlea. The acquired, delayed-onset types of sensorineural hearing loss may or may not be genetic in origin. There are many syndromes, too numerous to mention, as well as viral infections and ototoxic drugs that may cause acquired, delayed-onset sensorineural deafness. Systemic diseases, tumors, and noise are also associated with this type of hearing loss.
A patient’s voice may provide a clue to the nature of his or her deafness. The speaking voice is regulated by the way one hears oneself. Patients with a conductive hearing loss hear their own voices better by BC than by AC. They therefore think that their voices are loud and tend to speak softly. In contrast, patients with a sensorineural hearing defect hear less by both air and BC; therefore, they tend to speak louder.
Vertigo
Vertigo is a sense of spinning or turning while in a resting position. It is frequently associated with a loss of vestibular function, such as unsteadiness of gait. For any patient with vertigo, ask the following questions:
“How long have you had this sensation?”
“Have you had repeated attacks?”
“How long does an attack last? Seconds? Minutes? Hours? Days?”
“Is the onset of an attack abrupt?”
“Was the sensation brought on by, or worsened by, changes in position?”
“Does the spinning sensation get worse during an attack?”
“Are there any positions that make you feel better?”
“What kind of medications are you currently taking?”
“Do you know if you have ever been given an antibiotic called streptomycin or gentamicin?”
Vertigo may result from otologic, neurologic, psychologic, or iatrogenic causes. Ménière‘s disease causes severe paroxysmal vertigo as a result of labyrinthine lesions. The vertigo has an abrupt onset and may last several hours. It is often associated with nausea, vomiting, headache, a ringing sensation in the ear, and decreased hearing. The auditory abnormalities frequently antedate the vertigo. Vertigo associated with an acoustic neuroma is usually mild. Some antibiotics, such as gentamicin, streptomycin, and kanamycin, are vestibulotoxic and cause vertigo. The neurologic causes of vertigo are discussed further in Chapter 18, The Nervous System.
Tinnitus
Tinnitus is the sensation of hearing sound, such as buzzing or ringing, in the absence of environmental input. It is often associated with a conductive or sensorineural hearing loss. Usually the description of the type of tinnitus (e.g. “ringing” or “buzzing”) is of little help in determining its cause. The most common causes are inner ear disease such as Ménière’s disease, noise trauma, ototoxic drugs, and otosclerosis. On occasion, patients describe pulsatile tinnitus. This type of tinnitus beats at the same rate as the heart and may be a symptom of a vascular tumor of the head or neck. See Table 8-1 for a list of common causes of tinnitus.
Table 8–1
Common Causes of Tinnitus
| Location | Pulsatile/Clicking Sensation | Nonpulsatile |
| External ear | Otitis externa Bullous myringitis Foreign body |
Cerumen Tympanic membrane perforation Foreign body |
| Middle ear | Otitis media Vascular anomalies Neoplasm Eustachian tube dysfunction |
Otosclerosis Serous otitis media |
| Inner ear | Vascular anomalies | Cochlear otosclerosis Ménière’s disease Labyrinthitis Noise trauma Drug toxicity Presbycusis |
| Central nervous system | Vascular anomalies Hypertension |
Syphilis Degenerative disease Cerebral atherosclerosis |
Otorrhea
Otorrhea, or discharge from the ear, usually indicates acute or chronic infection. For any patient complaining of an ear discharge, ask the following:
“Can you describe the discharge?”
“Have you had similar episodes?”
“Do you experience dizziness?”
“Have you had a recent ear or throat infection?”
“Have you had any change in your hearing?”
A bloody discharge may be associated with carcinoma or trauma. A clear, watery discharge may indicate a leakage of cerebrospinal fluid. Determine how long the discharge has been present, as well as its color, its smell, and its relationship to itching, pain, or trauma.
Otalgia
Otalgia, or ear pain, may be related to inflammatory conditions in or around the ear, or it may be referred4 from distant anatomic sites in the head and neck. External otitis and otitis media are infections of the external and middle ear, respectively, and are common causes of locally produced pain. Pain from the teeth, pharynx, and cervical spine is commonly referred to the ear. Inflammation, trauma, and neoplasms anywhere along the course of the trigeminal, facial, glossopharyngeal, and vagus cranial nerves or cervical nerves C2 or C3 may be responsible for referred pain in the ipsilateral ear.
Itching
Pruritus (itching) of the ear may result from a primary disorder of the external ear or from a discharge from the middle ear. A systemic disease, such as diabetes, hepatitis, or lymphoma, may also be the cause.
The Nose
The specific symptoms related to the nose are the following:
Obstruction
The most common symptom of nasal disease is obstruction. If the symptom of nasal obstruction is present, ask the following questions:
“Is the obstruction on one side?”
“Have you ever had an injury to your nose?”
“How long has the obstruction been present?”
“Does the obstruction worsen with stress?”
“Is there a history of nasal polyps?”
“Is the obstruction associated with other symptoms?”
“Is there a seasonal change in your symptoms?” If so, “Which season is the worst?”
Rhinitis, which is inflammation of the nasal mucosa, can have allergic or nonallergic causes. Allergic rhinitis is congestion of the nasal mucosa triggered by an allergen such as pollen. The main symptoms include nasal obstruction, sneezing, and a clear, watery nasal discharge. It is helpful to try to determine the allergen. Weeds pollinate in the spring and fall, trees in the spring, and grasses in the summer. Nonseasonal allergic rhinitis may result from animal dander, mold, or dust. Nonallergic rhinitis produces the same symptoms but is nonseasonal and is not triggered by allergens. An example of nonallergic rhinitis is vasomotor rhinitis. Vasomotor rhinitis occurs at stressful times and results in venous engorgement of the conchae, causing obstruction. There are many other causes of vasomotor rhinitis, such as nasal spray abuse (also known as rhinitis medicamentosa), pregnancy, and hypothyroidism.
Nasal polyps, usually bilateral, also cause obstruction and are the most common cause of anosmia, or loss of smell.
Discharge
Nasal discharge can be unilateral or bilateral. It usually accompanies nasal obstruction. The discharge may be characterized as follows:
A thin and watery discharge is usually caused by excess mucous production resulting from a viral infection or allergic condition. A thick and purulent nasal discharge results from bacterial infection. A bloody discharge can result from a neoplasm, trauma, or an opportunistic infection such as mucormycosis (fungal disease). A foul-smelling discharge is often associated with foreign bodies in the nose, chronic sinusitis, or malignant disease. A clear, watery discharge that is increased by bending the head forward or by coughing is suggestive of cerebrospinal fluid leakage.
Bleeding
Epistaxis, or bleeding, usually results from the traumatic or spontaneous rupture of the superficial mucosal vessels in Little’s area. To exclude other causes, the clinician should determine whether the epistaxis is related to trauma or to a bleeding disorder. It may also result from chronic sinusitis or malignancy within the sinuses. The most common cause of epistaxis is nose-picking. Another prevalent causative factor is cocaine abuse.
Sinus Disease Symptoms
The symptoms of sinus disease are similar to the symptoms of nasal disease. Fever, malaise, cough, nasal congestion, maxillary toothache, purulent nasal discharge, headache, and little improvement of symptoms with decongestants increase the likelihood of sinus disease. Pain, often made worse by bending forward, is an important symptom. Pain from localized sinus disease is usually present in the area overlying the involved sinus. The only exception is sphenoid sinus disease, which is felt diffusely. Maxillary sinus pain is felt behind the eye and near the second premolar and first and second molar teeth. Frontal sinus pain is localized to above the eye. Ethmoid sinus pain is usually periorbital. Sometimes sinus pain can be referred to another area. In addition to pain, ocular abnormalities may also be present with diseases of the sinuses.
The accuracy of the symptoms and signs of sinusitis has been evaluated. Colored nasal discharge, cough, and sneezing were the symptoms with the highest sensitivities (72%, 70%, and 70%, respectively); these symptoms, however, were not very specific. Maxillary toothache was the symptom most specific for sinusitis, with a specificity of 93%; however, only 11% of patients reported this symptom. This symptom had the highest positive likelihood ratio, of 2.5. The conclusion was that the combination of maxillary toothache, poor response to decongestants, colored nasal discharge, and abnormality on sinus transillumination (discussed later in this chapter) was the strongest predictor of sinusitis in primary care populations. If all these symptoms were present in one patient, the positive likelihood ratio was 6.4, and the patient probably had sinusitis; if none were present, sinusitis was ruled out.
Table 8-2 summarizes the location of pain associated with sinus disease. Table 8-3 lists other clinical signs and symptoms associated with sinus disease.
Table 8–2
Location of Pain Associated with Sinus Disease
| Sinus Involved | Local Pain | Referred Pain |
| Maxillary | Behind eye Cheek Nose Upper teeth Upper lip |
Teeth Retrobulbar |
| Ethmoid | Periorbital Retronasal Retrobulbar |
Occipital Upper cervical |
| Frontal | Supraorbital Frontal |
Bitemporal and occipital headache |
Table 8–3
Clinical Signs and Symptoms in Sinus Disease
| Sinus Involved | Signs and Symptoms |
| Maxillary | Ocular abnormalities |
| Diplopia | |
| Proptosis | |
| Epiphora (tearing) | |
| Nasal obstruction and rhinorrhea | |
| Epistaxis | |
| Loosening of teeth | |
| Ethmoid | Orbital swelling |
| Nasal obstruction and purulent rhinorrhea | |
| Ocular abnormalities | |
| Proptosis | |
| Diplopia | |
| Tenderness over inner canthus of eye | |
| Frontal | Nasal obstruction and rhinorrhea |
| Tenderness over frontal sinus | |
| Pus in middle meatus | |
| Signs of meningitis |
Effect of Deafness on the Patient
The ear is the sensory organ of hearing. Audition is one of the main avenues of communication. Any disturbance in the reception of sound waves by the external ear or the transmission of electrical impulses to the brain may result in an abnormal interpretation of language.
It is estimated that there are more than 15 million persons in the United States with some degree of hearing loss that interferes with their ability to understand speech. Approximately half of these individuals, 7.2 million, have bilateral hearing problems. Although persons older than 70 years of age account for 30% of all deaf individuals, there are more than 250,000 deaf children younger than 3 years of age. Since the late 1970s, the overall prevalence rate has increased substantially.
To understand the effect of deafness on an individual, it is necessary to consider the age at onset, the severity of the loss, the rapidity of the loss, and any residual hearing. Persons with insidious or sudden hearing loss experience grief and depression. Consider, for example, the grief expressed in the quotation by Beethoven at the beginning of this chapter.
The psychologic effects of deafness include paranoia, depression, withdrawal, irritability, and anxiety. Although it has not been proved, it appears that deaf persons have an increased tendency toward paranoia. Most deaf individuals tend to be suspicious of others’ conversations.
The most profound responses to a severe hearing deficit are depression and withdrawal. The following quotation from Beethoven dramatizes these responses:
Oh you men who think that I am malevolent, stubborn, or misanthropic, how greatly do you wrong me. You do not know the secret cause which makes me seem that way to you. … For me there can be no relaxation with my fellow men, no refined conversations, no mutual exchange of ideas. I must live alone, like one who has been banished. … What a humiliation for me when someone standing next to me heard a flute in the distance, and I heard nothing … a little more of that and I would have ended my life—it was only my art that held me back.
Hearing-impaired persons have social identity problems as well. They are frequently excluded from previous associations. If they use sign language, they cannot enjoy the company of individuals who do not know sign language. Work or career may have to be altered. The stigma associated with wearing a hearing aid can reinforce the feeling of alienation from others. A patient may avoid wearing a hearing aid for fear of being stigmatized.
Deaf children experience even more severe problems. Their lack of auditory input influences character, early childhood experiences, attitudes, and interpersonal relationships. They are deprived of many of the reassuring, loving, and comforting sounds that facilitate the development of personality. They are unable to obtain verbal cues of a parent’s affection. They are also unable to be alerted by auditory signs of danger.
Psychologic problems, social inadequacy, and educational retardation are common among deaf children. The worse the handicap is, the worse the psychologic and educational implications are.
A young hearing-impaired child who exhibits a delay in language development may be diagnosed as developmentally disabled. In general, children who are congenitally deaf or suffer from severe hearing impairment before 3 years of age suffer the most. As the type of lesion causing deafness progresses from the periphery inward, the deleterious effects increase.
Physical Examination
The equipment necessary for the examination of the ear and nose is as follows: otoscope, choice of specula, penlight, and 512-Hz tuning fork. A nasal illuminator attachment for the otoscope and a nasal speculum are optional.
The physical examination of the ear and the nose is performed with the examiner seated in front of the patient.
The Ear
If the patient has symptoms referable to one ear, examine the uninvolved ear first. The physical examination of the ear includes the following:
External Examination
Inspect the pinna and postauricular skin. Note the position, size, and shape of the pinna. The pinna should be positioned centrally and should be in proportion to the face and head. Note any obvious abnormalities or surgical scars.
Inspect the External Ear Structures
A small dimple in front of the tragus is usually a remnant of the first branchial arch.
Inspect the external ear for deformities, nodules, inflammation, or lesions. The presence of tophi is a highly specific but nonsensitive sign of gout. Tophi are deposits of uric acid crystals. They appear as hard nodules in the helix or antihelix. In rare cases, a white discharge may be seen in association with them. A “cauliflower ear” is a pinna that is gnarled as a result of repeated trauma. Figure 8-11 shows a squamous cell carcinoma and a malignant melanoma of one lobule.

Figure 8–11 Squamous cell carcinoma (on the right) and malignant melanoma (on the left) of the lobule.
Inspect for discharge. If discharge is present, note its characteristics, such as color, consistency, and clarity.
Palpate the External Ear Structures
Palpate the pinna for tenderness, swelling, or nodules. If pain is elicited by pulling up and down on the pinna or by pressing in on the tragus, an infection of the external canal is probably present.
Auditory Acuity Testing
Testing for auditory acuity is the next part of the physical examination. The easiest method of testing for a gross hearing loss is for the examiner to occlude one external canal by pressing inward on the tragus and to speak softly into the other ear. The examiner should hide his or her mouth to prevent lip reading by the patient. The examiner should whisper words such as “park,” “dark,” or “daydream” in the nonoccluded ear and determine whether the patient can hear them. This procedure is then repeated with the other ear. Alternately, the examiner can whisper a combination of three letters or numbers, such as “A, 7, F” while standing approximately 2 feet behind the patient and asking the patient to repeat the sequence. If the patient answers correctly, hearing should be considered within normal limits. Studies have shown that the normal test practically excludes significant hearing loss. An abnormal whispered hearing test has a sensitivity of 90% to 99%, and a specificity of 80% to 87%.
Another test, known as the finger rub test, has the highest specificity for hearing loss.5 The inability to hear a strong finger rub is pathognomonic for a hearing loss. In contrast, the ability to hear a faint finger rub indicates normal hearing on the side examined. To perform the finger rub test, the examiner stands with hands outstretched directly in front of the patient, whose eyes are closed. The examiner tests one ear at a time by rubbing fingers together. The patient is instructed to raise his or her hand on the side where the rubbing occurred.
The use of tuning fork testing for hearing loss is more accurate and should be performed regardless of the results of the whisper test. Although several tuning fork frequencies are available, the best for evaluating hearing is the 512-Hz fork.6
A tuning fork is held by its stem, and the tines are briskly struck against the palm of the hand. It should never be struck on a solid wooden or metal object. The two tuning fork tests to assess hearing are the Rinne test and the Weber test.
The Rinne Test
In the Rinne test, AC is compared with BC. Each ear is tested separately. Strike a 512-Hz tuning fork and place its handle on the mastoid tip near the external auditory meatus. Ask the patient whether he or she hears the sound and to indicate when he or she no longer hears it. When the patient can no longer hear the sound, place the tines of the vibrating tuning fork in front of the external auditory meatus of the same ear, and ask the patient whether he or she can still hear the sound. The tines of the vibrating tuning fork should not touch any hair because the patient may have a hearing impairment but still feel the vibration. The Rinne test is demonstrated in Figure 8-12.
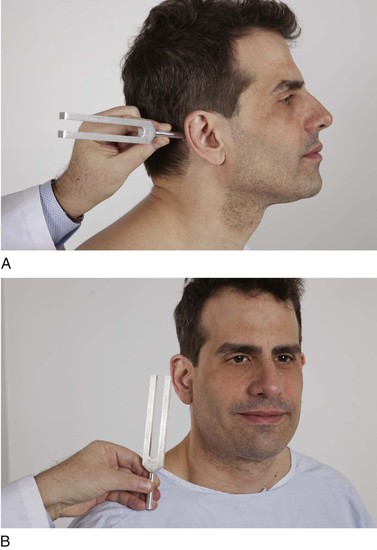
Figure 8–12 The Rinne test. A, The 512-Hz tuning fork is first placed on the mastoid process. B, When the sound can no longer be heard, the tuning fork is placed in front of the external auditory meatus. Normally, air conduction (AC) is better than bone conduction (BC); that is, AC > BC.
Normally, AC is better than BC, and patients are able to hear the tuning fork at the external auditory meatus after they can no longer hear it on the mastoid tip; this is a Rinne positive test result (AC > BC). In patients with a conductive hearing loss, however, BC is better than AC: a Rinne negative test result (BC > AC). Patients with sensorineural deafness have impaired AC and BC but maintain the normal response (AC > BC). The middle ear amplifies the sound in both positions.
If there is total deafness in one ear, the patient may hear the tuning fork even when it is placed on the mastoid process of the deaf ear. This results from the transmission of vibrations by bone across the skull to the opposite side, where they are sensed by the healthy ear. This is termed a false-negative Rinne test result.
Note that the words positive and negative are used in a manner different from other usage in medical tests. Positive or negative means that a certain parameter that was evaluated was present or not. In this case, that parameter refers to whether AC is better than BC. Thus a “positive” result indicates the healthy state, in contrast to many other medical tests. Therefore when presenting your findings, to avoid confusion, it is best to avoid using the term positive or negative, and simply state your findings.
The Weber Test
In the Weber test, BC is compared in both ears, and the examiner determines whether monaural impairment is neural or conductive in origin. Stand in front of the patient and place a vibrating 512-Hz tuning fork firmly against the center of the patient’s forehead. Ask the patient to indicate whether he or she hears or feels the sound in the right ear, in the left ear, or in the middle of the forehead. Hearing the sound, or feeling the vibration, in the middle is the normal response. If the sound is not heard in the middle, the sound is said to be lateralized, and thus a hearing loss is present. Sound is lateralized to the affected side in conductive deafness. Try it on yourself. Occlude your right ear and place a vibrating tuning fork in the center of your forehead. Where do you hear it? On the right. You have created a conductive hearing loss on the right by blocking the right canal; the sound is lateralized to the right side. The Weber test is illustrated in Figure 8-13.
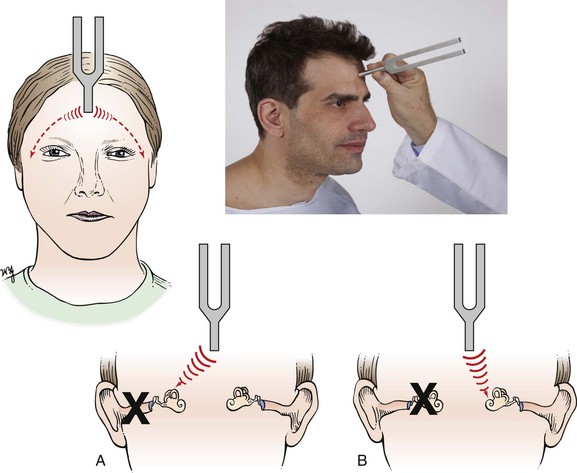
Figure 8–13 The Weber test. When a vibrating 512-Hz tuning fork is placed on the center of the forehead, the normal response is for the sound to be heard in the center, without lateralization to either side. A, In the presence of a conductive hearing loss, the sound is heard on the side of the conductive loss. B, In the presence of a sensorineural loss, the sound is heard better on the opposite (unaffected) side.
The explanation for the Weber test effect is based on the masking effect of background noise. In normal conditions, there is considerable background noise, which reaches the tympanic membrane by AC. This tends to mask the sound of the tuning fork heard by BC. In an ear with a conductive hearing loss, the AC is decreased, and the masking effect is therefore diminished. Thus the affected ear hears and feels the vibrating tuning fork better than does the normal ear.
In patients with unilateral sensorineural deafness, the sound is not heard on the affected side but is heard by, or localized to, the unaffected ear.
To test the reliability of the patient’s responses, it is occasionally useful to strike the tuning fork against the palm of the hand and hold it briefly to silence it. The Rinne and Weber tests are then carried out as indicated, using the silent tuning fork. This serves as a good control.
In summary, consider the following two examples:
Example 1
Example 2
Rinne: Right ear: AC > BC (Rinne positive—normal); left ear: BC > AC (Rinne negative—abnormal)
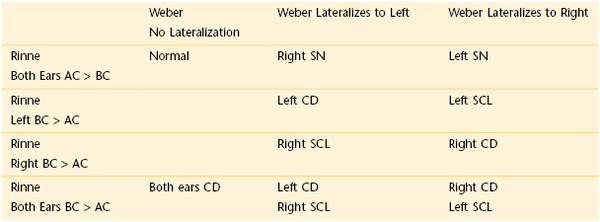
CD, Conductive deafness; SCL, combined loss (sensorineural and conductive); SN, sensorineural deafness.
It is important to remember that both the Rinne and Weber tests are screening tests and do not replace formal audiometry hearing tests.
Otoscopic Examination
The remainder of the examination of the ear is performed with the otoscope. The otoscope incorporates a halogen light source and fiberoptic circumferential distribution of the light. This provides a 360-degree ring of light-conducting fibers within the shell of the otoscope through which the observer views the inner structures of the ear. Most otoscopes are illuminated by a bright quartz halogen bulb requiring a 3.5-V power supply. Specially designed reusable or disposable polypropylene specula slip over the tip of the instrument. Most otoscopic heads can be used with a rubber squeeze bulb for pneumatic otoscopy (described later in this chapter). Take care in the use of the otoscope. The best visualization of the structure does not require the speculum to be wedged into the canal. Be gentle to achieve the best view of the anatomy.
Choose the correct speculum size: small enough to prevent discomfort to the patient and large enough to provide an adequate beam of light. Usually a tip 4 to 6 mm in diameter is used for adults, 3 to 4 mm in diameter for children, and 2 mm in diameter for infants.
The Techniques
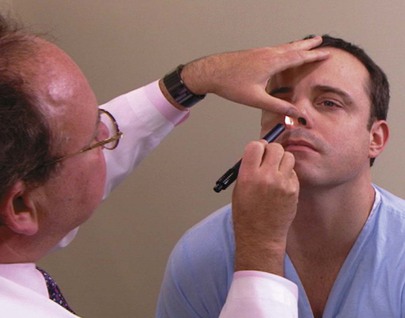
To examine the patient’s right ear, the examiner holds the otoscope in the right hand. The canal is straightened by the examiner’s left hand, pulling the pinna up, out, and back. The straighter the canal, the easier the visualization and the more comfortable the examination is for the patient.
In a child, the canal should be straightened by pulling the pinna down and back.
The patient is asked to turn his or her head to the side slightly so that the examiner can examine the ear more comfortably. The otoscope may be held in either of two positions. The first, and preferred, position involves holding the otoscope like a pencil, between the thumb and index finger, in a downward position with the ulnar aspect of the examiner’s hand braced against the side of the patient’s face. This position provides a buffer against sudden movement by the patient. By holding the end of the otoscope’s handle, the examiner then angles the speculum into the external canal. This technique at first feels more cumbersome than the alternative technique, but it is safer, especially for children. This technique is shown in Figure 8-14.
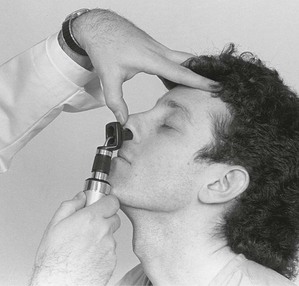
The second position involves holding the otoscope upward as the speculum is introduced into the canal. This technique feels more comfortable, but a sudden movement by the patient can cause pain and injury to the patient. This technique is shown in Figure 8-15.
Inspect the External Canal
Gently insert the speculum and inspect the external canal. The external auditory canal is 24 mm long in the adult and is the only skin-lined, blind-ended canal in the body. The canal follows a tortuous course from the external meatus to the tympanic membrane. The techniques previously described are used to straighten the canal. There should be no evidence of redness, swelling, or tenderness, which indicates inflammation. The walls of the canal should be free of foreign bodies, scaliness, and discharge. If a foreign body is seen, pay particular attention when inspecting the opposite ear canal, the nose, and other accessible body orifices.
Any cerumen should be left as is, unless it interferes with the visualization of the rest of the canal and tympanic membrane. Removal of cerumen is best left to an experienced examiner because any manipulation may result in trauma or abrasions. Figure 8-16 depicts an external ear canal with a large hematoma secondary to aggressive use of a cotton-tipped applicator stick. Notice the tympanic membrane in the background.

Figure 8–16 External ear canal with large hematoma.
If a discharge is present, look for the site of origin.
Inspect the Tympanic Membrane
As the speculum is introduced farther into the canal in a downward and forward direction, the tympanic membrane is visualized. The tympanic membrane should appear as an intact, ovoid, semitransparent, pearly gray membrane at the end of the canal. The lower four fifths of the tympanic membrane is called the pars tensa; the upper fifth, the pars flaccida. The handle of the malleus should be seen near the center of the pars tensa. From the lower end of the handle, there is frequently a bright triangular cone of light reflected from the pars tensa. This is called the light reflex, which is directed anteroinferiorly. The pars flaccida, the short process of the malleus, and the anterior and posterior folds should be identified. A normal tympanic membrane is pictured in Figure 8-17A, and the important landmarks are identified in Figure 8-17B.
The presence or absence of the light reflex should not be considered indicative of either normality or disease. The sensitivity of the light reflex for indicating disease is low. There are as many normal tympanic membranes without a light reflex as there are abnormal membranes with a light reflex.
Describe the color, integrity, transparency, position, and landmarks of the tympanic membrane.
Healthy tympanic membranes are usually pearly gray. Diseased tympanic membranes may be dull and become red or yellow. Is the eardrum injected? Injection refers to the dilatation of blood vessels, making them more apparent. The blood vessels should be visible only around the perimeter of the membrane. Dense, white plaques on the tympanic membrane may be caused by tympanosclerosis, which is caused by deposition of hyaline material and calcification within the layers of the tympanic membrane. This condition is commonly (in 50% to 60% of cases) secondary to the insertion of ventilation tubes. The classic horseshoe shape of tympanosclerosis is seen in the tympanic membrane shown in Figure 8-18. Despite the size of these lesions, they usually do not impair hearing and are rarely of clinical importance. If the lesion extends into the middle ear, however, conductive deafness may result.

Figure 8–18 Tympanosclerosis.
Is the tympanic membrane bulging or retracted? Bulging of the membrane may indicate fluid or pus in the middle ear. No bubbles or fluid should be seen behind the tympanic membrane in the middle ear. A tympanic membrane becomes retracted when intratympanic cavity pressures are reduced: for example, when the eustachian tube is obstructed. Figure 8-19 depicts a “retraction pocket” just above the lateral process of the malleus, a condition known as attic retraction. On occasion, the entire tympanic membrane may become retracted onto the ossicles of the middle ear. The ossicles may become eroded, with the development of a conductive hearing loss.

Figure 8–19 Retraction pocket.
If the tympanic membrane is perforated, describe the characteristics. Perforation of the tympanic membrane can occur after trauma or infection.
The normal position of the tympanic membrane is oblique to the external canal. The superior margin is closer to the examiner’s eye. This is frequently better seen in infants than in adults.
There are many differences in the color, shape, and contour of the tympanic membrane, which can be recognized only with experience.
After examining the right ear, examine the left ear by holding the otoscope in the left hand and straightening the canal with the right hand.
Determine the Mobility of the Tympanic Membrane
If there is a question of middle ear infection, pneumatic otoscopy should be performed. This technique requires the use of a speculum large enough to fit snugly into the external canal to establish a closed air chamber between the canal and the interior of the otoscopic head. A rubber squeeze bulb is attached to the otoscopic head. By squeezing the bulb, the examiner can increase the air pressure in the canal. Pneumatic otoscopy must be performed gently, and the patient should be informed that he or she may experience a blowing noise during the procedure. When the pressure in the otoscopic head is increased by squeezing the bulb, the normal tympanic membrane shows a prompt inward movement. In patients with an obstructed eustachian tube, the tympanic membrane moves sluggishly inward. If fluid is present in the middle ear, a marked decrease or absence of movement is detected. The reduction of movement of the tympanic membrane increases the probability of middle ear infection by as much as 40%. This simple technique can provide invaluable assistance in the early diagnosis of many middle ear problems.
The Nose
The examination of the nose consists of the following:
External Examination
Inspect the Nose
The external examination consists of inspection of the nose for any swelling, trauma, or congenital anomalies. Is the nose straight? Does a deviation involve the upper, bony portion or the lower, cartilaginous portion?
Inspect the external nares. Are they symmetric?
Test the patency of each nostril. Occlude one nostril by gently placing a finger across the opening. Ask the patient to sniff. Do not compress the contralateral nostril by aggressive pressure.
Any swelling or deformity should be palpated for pain and firmness.
Rhinophyma is a common condition in which there is prominent hypertrophy of the sebaceous glands of the nose with overgrowth of the soft tissue. This condition is more common in men than in women. The patient pictured in Figure 8-20 also has acne rosacea, which is a common associated condition consisting of papules, pustules, and erythema of the face. The cause is unknown. The rash is worsened by hot drinks, highly spiced food, and alcohol.

Figure 8–20 Rhinophyma.
Palpate the Sinuses
Palpation over the frontal and maxillary sinuses may reveal tenderness that is indicative of sinusitis.
Internal Examination
The key to the internal examination is proper positioning of the head. Ask the patient to hold his or her head back. Place your left hand firmly on top of the patient’s head, and use your left thumb to elevate the tip of the patient’s nose. In this manner, change the position of the patient’s head to visualize the intranasal structures. Use a light source to illuminate the internal structures. This technique is shown in Figure 8-21.
Inspect the position of the septum to the lateral cartilages on each side. Examine the vestibule for inflammation and the anterior septum for deviation or perforation. Evaluate the color of the nasal mucous membrane. Normal nasal mucous membranes are dull red and moist and have a smooth, clean surface. Nasal mucosa is usually darker in color than oral mucosa. Inspect for exudate, swelling, bleeding, and trauma. If epistaxis has occurred, examine Little’s area for vascular engorgement or crusting.
Is a discharge present? If so, describe it as purulent, watery, cloudy, or bloody. Is crusting present? Are any masses or polyps present?
Tip the patient’s head farther back, and check the posterior septum for deviation or perforation. Note the size and color of the inferior turbinates. The two inferior turbinates are rarely symmetric.
Use a Nasal Illuminator
If a nasal illuminator is used, the examiner’s left thumb is placed on the tip of the patient’s nose while the palm of the examiner’s hand steadies the patient’s head. The patient’s neck is slightly extended as the tip of the speculum of the illuminator is inserted into the nostril. After one nostril is evaluated, the illuminator is placed in the other nostril. The technique of using a nasal illuminator is shown in Figure 8-22.
Use a Nasal Speculum
If a nasal speculum is used, the instrument is held in the examiner’s left hand, and the speculum is introduced into the patient’s nostril in a vertical position (blades facing up and down). The speculum should not rest on the nasal septum. The blades are inserted approximately 1 cm into the vestibule, and the patient’s neck should be slightly extended. The examiner’s left index finger is placed on the ala of the patient’s nose to anchor the upper blade of the speculum while the examiner’s right hand steadies the patient’s head. The right hand is used to change the head position for better visibility of the internal structures. After one nostril has been examined, the speculum, still being held in the examiner’s left hand, is introduced into the patient’s other nostril. Figure 8-23 shows a patient with nasal polyps, visible by means of the nasal speculum.

Figure 8–23 Nasal polyps.
Transilluminate the Sinuses
If a patient has symptoms referable to sinus problems, transillumination of the sinuses is performed. This examination is performed in a darkened room, and a bright light source is placed in the patient’s mouth on one side of the hard palate. The light is transmitted through the maxillary sinus cavity and is seen as a crescent-shaped dull glow under the eye. The other side is then examined. Normally, the glow on each side is equal. If one sinus contains fluid, a mass, or mucosal thickening, there is a decrease in the glow, indicating loss of aeration on that side. An alternative method of examining the maxillary sinus is to direct a light downward from under the medial aspect of the eye. The patient is asked to open the mouth, and the glow is observed in the hard palate. This technique is illustrated in Figure 8-24. The frontal sinus can be examined in a similar manner by directing the light upward under the medial aspect of the eyebrow and observing the glow above the eye.
The ethmoid and sphenoid sinuses cannot be examined by transillumination.
The patient-to-patient variability of sinus transillumination is tremendous. In the absence of sinus symptoms, these differences in transillumination are nonspecific.
Clinicopathologic Correlations
Infectious, inflammatory, traumatic, and neoplastic diseases are common in the organs of the ear and nose. Some of the more common ear infections are discussed in this section.
Acute otitis externa is a common inflammatory condition of the external ear canal, most often caused by Pseudomonas aeruginosa. The prominent symptom is severe ear pain (otalgia) accentuated by manipulation of the pinna and especially by pressure on the tragus. Edema of the external ear canal, erythema, and a yellowish-green discharge are prominent signs of this disease. Commonly, the canal is so tender and swollen that adequate visualization of the entire canal and tympanic membrane is impossible. “Swimmer’s ear” is a form of otitis externa in which there is a loss of the protective cerumen, and chronic irritation and maceration by water and bacteria occur. Itching is a common precursor of otalgia. Figure 8-25 shows the external ear canal of a patient with acute otitis externa. Notice the follicular appearance of the canal, which resulted from epithelial swelling. As the condition progresses, the lumen may be occluded, producing conductive deafness.

Figure 8–25 Acute otitis externa.
Bullous myringitis is a localized form of external otitis, commonly associated with an acute viral upper respiratory infection. Severe otalgia is present, caused by bullous, often hemorrhagic, lesions on the skin in the deep external ear canal and on the tympanic membrane. A blood-tinged discharge may also occur. Fortunately, bullous myringitis is a self-limited condition. Figure 8-26 shows the tympanic membrane of a patient with bullous myringitis. Notice the blood-filled bullae on the membrane. Figure 8-27 shows the left ear of another patient with bullous myringitis. Notice the huge bulla filled with serosanguineous fluid arising from the floor of the bony external auditory canal. The bulla is so large that it obscures the tympanic membrane from view.

Figure 8–26 Bullous myringitis.

Figure 8–27 Bullous myringitis.
Acute otitis media is a bacterial infection of the middle ear, occurring most commonly in children. Up to 50% of all children experience an attack of acute otitis media before they reach 1 year of age, and 75% of children are affected before their second birthdays. After 5 years of age, the incidence declines rapidly. Affected patients suffer ear pain and have constitutional symptoms of fever and malaise, often associated with gastrointestinal problems and a conductive hearing loss. In contrast to external otitis, in which pulling on the auricle and tragus causes pain, no pain is elicited when these maneuvers are performed on a patient with acute otitis media. The tympanic membrane becomes injected, and the entire membrane is a fiery red. A mucopurulent exudate in the middle ear causes the membrane to bulge outward. In most cases, antibiotic therapy resolves the condition and restores normal hearing. Figure 8-28 shows the tympanic membrane of a young child with the classic features of acute otitis media. Notice the erythema, resulting from the acute inflammation, and the cloudiness and bulging of the tympanic membrane, resulting from the middle ear exudate.

Figure 8–28 Acute otitis media.
Spontaneous rupture of the tympanic membrane may result from the increased pressure, with discharge of the mucopurulent exudate into the external ear canal. If this occurs, advanced acute otitis media is said to be present. Figure 8-29 illustrates perforation of a tympanic membrane as a result of otitis media.
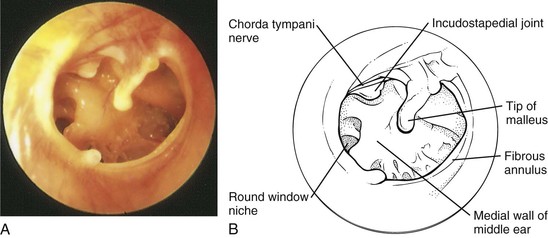
Figure 8–29 Photograph (A) and labeled schematic (B) illustrating a central perforation of the right tympanic membrane.
Perforations may be central or marginal and may result from either otitis media or trauma. A central perforation does not involve the margin or annulus of the tympanic membrane; a marginal perforation involves the margin. Marginal perforations are more serious because they predispose the patient to the development of a cholesteatoma, which is a chronic condition of the middle ear. A marginal perforation allows squamous epithelium from the external canal to grow into the middle ear. As these cells invade, they desquamate, and debris accumulates in the middle ear, forming a cholesteatoma. Slow enlargement of the cholesteatoma leads to erosion of the ossicles and expansion into the mastoid antrum. Figure 8-30 illustrates a cholesteatoma.
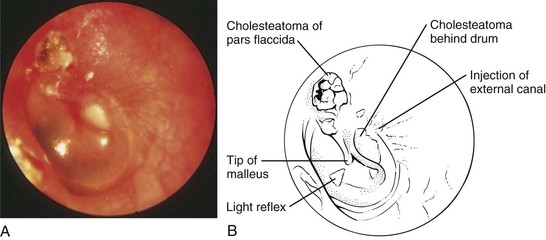
Figure 8–30 Photograph (A) and labeled schematic (B) illustrating a cholesteatoma of the left ear that resulted from a marginal perforation of the tympanic membrane. Note the injection of the distal external canal.
A congenital cholesteatoma of the right anterior middle ear is pictured in Figure 8-31. It is smooth and white, medial to a normal tympanic membrane.
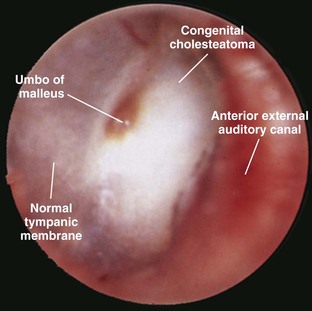
Figure 8–31 Congenital cholesteatoma.
Figure 8-32 depicts chronic tympanic membrane perforation of the right ear. Notice the smooth epithelium-covered margin of chronic perforation, as well as patches of tympanosclerosis.
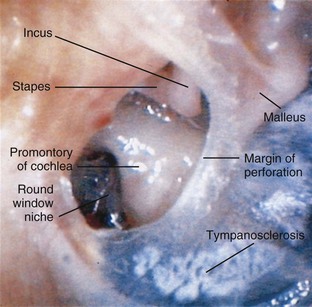
Figure 8–32 Chronic tympanic membrane perforation.
Serous otitis media occurs primarily in adults with viral upper respiratory infections or during sudden atmospheric pressure changes. In the presence of a blocked eustachian tube, air becomes trapped within. The tiny blood vessels in the middle ear absorb much of the air, producing a vacuum that draws in or retracts the tympanic membrane. The sensation of “plugged ears” occurs. If the pressure is not relieved, this vacuum draws serous, nonpurulent fluid from the blood vessels into the middle ear. The tympanic membrane appears yellowish-orange as a result of the amber-colored fluid, and the landmarks are clearly seen as the membrane is retracted against these structures. Partial obstruction of the eustachian tube produces air bubbles or an air-fluid level in the middle ear. Figure 8-33 shows the tympanic membrane of a patient with serous otitis media.
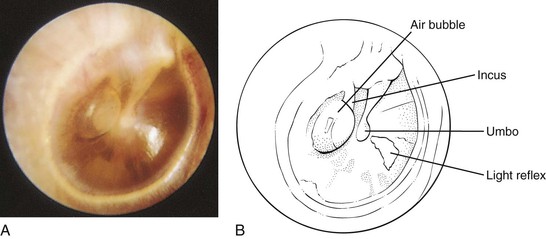
Figure 8–33 Photograph (A) and labeled schematic (B) illustrating serous otitis media of the right ear. Note the air bubble in the middle ear behind the tympanic membrane.
Recurrent middle ear infections and tympanic membrane rupture may lead to chronic otitis media. Chronic infections may produce a foul-smelling discharge, which is the main symptom of chronic otitis media; pain is usually not present. Erosion of the ossicles with formation of scar tissue may occur, causing a conductive hearing loss.
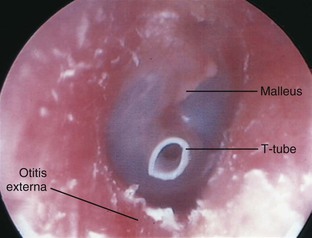
Figure 8-34 shows the right tympanic membrane in an adult patient with chronic eustachian tube dysfunction. An early pars flaccida retraction pocket is seen. These retraction pockets result from chronic negative pressure within the middle ear and may progress to form an acquired cholesteatoma. A pressure-equalizing tube, called a tympanostomy tube, or T-tube, has been placed to eliminate the negative middle ear pressure. Figure 8-35 shows the right tympanic membrane in another patient with long-standing eustachian tube dysfunction whose middle ear is ventilated with a long-term T-tube. Resolving mild otitis externa is seen, with canal skin erythema and desquamation of the epithelium.
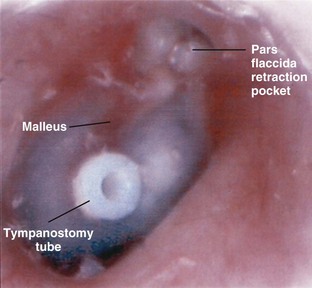
Figure 8–34 Chronic eustachian tube dysfunction.
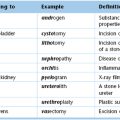
Table 8-4 summarizes the comparative features of conductive and sensorineural hearing loss. Table 8-5 enumerates the common causes of deafness. Table 8-6 differentiates acute otitis externa from acute otitis media.
Table 8–4
Comparative Features of Conductive and Sensorineural Hearing Loss
| Feature | Conductive Hearing Loss | Sensorineural Hearing Loss |
| Pathologic process | External canal Middle ear |
Cochlea Cochlear nerve Brain stem |
| Loudness of speech | Softer than normal | Louder than normal |
| External canal | May be abnormal | Normal |
| Tympanic membrane | Usually abnormal | Normal |
| Rinne test result | Negative | Positive |
| Weber test result | Heard on “deaf” side | Heard on better side (only in severe unilateral loss) |
Table 8–5
Common Causes of Deafness
| Patient | Conductive Deafness | Sensorineural Deafness |
| Child | Congenital Acute otitis media Chronic otitis media Cerumen Trauma |
Congenital Mumps labyrinthitis Maternal rubella during first trimester Birth trauma Congenital syphilis |
| Adult | Serous otitis media Chronic otitis media Otitis externa Cerumen Eustachian tube blockage Viral myringitis Cholesteatoma Otosclerosis |
Delayed-onset congenital Ménière’s disease Ototoxic drugs Viral labyrinthitis Acoustic neuroma Presbycusis (age-related deafness) |
Table 8–6
Differentiation of Acute Otitis Externa from Acute Otitis Media
| Signs and Symptoms | Acute Otitis Externa* | Acute Otitis Media† |
| Pressure on tragus | Painful | Painless |
| Lymphadenopathy | Frequent | Absent |
| External canal | Edematous | Normal |
| Season | Summer | Winter |
| Tympanic membrane | Normal | Fluid behind eardrum, possible perforation |
| Fever | Yes | Yes |
| Hearing | Slight loss or normal | Decreased |
* See Figure 8-25.
† See Figure 8-28.
The bibliography for this chapter is available at studentconsult.com.
Bibliography
Bagai A, Thavendiranathan P, Detsky AS. Does this patient have hearing impairment? JAMA. 2006;295:416.
Hawke M, Kwok P. A mini-atlas of ear-drum pathology. Can Fam Physician. 1987;33:1501.
Orlans H. Adjustment to adult hearing loss. College Hill Press: San Diego; 1985.
White J. Benign paroxysmal positional vertigo: how to diagnose and quickly treat it. Cleveland Clin J Med. 2004;71:722.
Williams JW, Simel DL. Does this patient have sinusitis? Diagnosing acute sinusitis by history and physical examination. JAMA. 1993;270:1242.
Williams JW, et al. Clinical evaluation for sinusitis: making the diagnosis by history and physical examination. Ann Intern Med. 1992;117:705.
Wilson JF. In the clinic: acute sinusitis. Ann Intern Med. 2010;163.
U.S. Preventative Services Task Force. Screening for hearing loss in older adults. [Available at] http://www.uspreventiveservicestaskforce.org/uspstf/uspshear.htm; March 2011 [Accessed January 29, 2013] .
1 On occasion, when the distal external canal is cleaned, coughing may result. This cough reflex is mediated through the vagus nerve.
2 Sensory stimulation from within the tissues of the body with regard to their movement or position.
3 Otosclerosis is the formation of new bone in the labyrinth, causing progressive fixation of the footplate of the stapes to the oval window.
4 Referred pain is felt in an area that is separate from the area that is actually the source of the pain. For example, pain from gallbladder disease is frequently felt in the right shoulder. Chapter 14, The Abdomen, discusses further aspects of referred pain.
5 Torres-Russotto D, Landau EM, Harding GW, et al: Calibrated finger rub auditory screening test (CALFRAST), Neurology 72:1595, 2009.
6 Different examiners prefer tuning forks of different frequencies for determining auditory acuity. A tuning fork of too high a frequency yields a tone that fades too quickly.