Chapter 5 The Ear
René Théophile Hyacinthe Laennec, 1821; letter to his cousin Menadec
St. John Baptiste de la Salle (1651–1719), The Rules of Christian Manners and Civility, I
A. External Ear
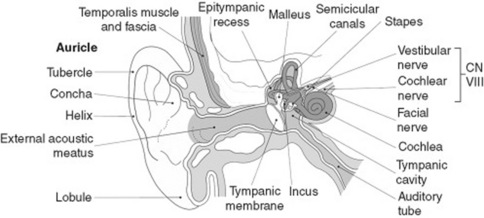
6 What is the auricle (or pinna)?
It is the part of the external ear that is outside the canal (Fig. 5-1). Made of cartilage and skin, it is highly flexible.
7 What are auricular bumps? What causes them?
 Darwin’s tubercle (Fig. 5-2): Benign and congenital nodule near the auricular apex (on the helix, at the junction of upper and middle thirds). Nontender and rarely bilateral, it was first described by the British sculptor Thomas Woolner, a founding member of the Pre-Raphaelite Brotherhood and a spare-time anatomist. Woolner depicted it in his statue of “Puck,” and Charles Darwin was so impressed that he named it the Woolnerian tip. It is an atavistic feature (i.e., a trait typical of our mammalian ancestors—more specifically, monkeys).
Darwin’s tubercle (Fig. 5-2): Benign and congenital nodule near the auricular apex (on the helix, at the junction of upper and middle thirds). Nontender and rarely bilateral, it was first described by the British sculptor Thomas Woolner, a founding member of the Pre-Raphaelite Brotherhood and a spare-time anatomist. Woolner depicted it in his statue of “Puck,” and Charles Darwin was so impressed that he named it the Woolnerian tip. It is an atavistic feature (i.e., a trait typical of our mammalian ancestors—more specifically, monkeys).
 Keloids (Fig. 5-3): Smooth and flesh-colored papule(s) on one or both sides of the earlobe. They indicate an exuberant and fibrotic response to injury.
Keloids (Fig. 5-3): Smooth and flesh-colored papule(s) on one or both sides of the earlobe. They indicate an exuberant and fibrotic response to injury.
 Tophi: One or more nontender nodules on the auricular edges. They are named after the Latin tufa (a calcareous and volcanic deposit) and may indeed be mildly hard. They can occur on both helix and antihelix, and usually indicate hyperuricemia and gout.
Tophi: One or more nontender nodules on the auricular edges. They are named after the Latin tufa (a calcareous and volcanic deposit) and may indeed be mildly hard. They can occur on both helix and antihelix, and usually indicate hyperuricemia and gout.
 Chondrodermatitis nodularis chronica helicis (CNH): This is a common, benign, and painful condition of the most prominent projection of the ear, usually the apex of the helix, but it also may affect the antihelix. It is typical of the right ear of middle-aged to older men, usually fair-skinned individuals with cutaneous sun-damage. In 10–35% of cases, it may also affect women. It is rather common (in a series, the most frequent external ear condition seen in an ear-nose-throat clinic) and is probably due to prolonged and excessive pressure, leading to inflammation, edema, and ischemic necrosis. This eventually degenerates into secondary perichondritis due to the vascular characteristics of the ear. Onset may be precipitated by pressure, trauma, or cold. Sleeping on the affected side is also common. The nodule appears spontaneously and painfully, rapidly enlarging to a maximum size of 4–8 mm, after which it remains stable. It is firm, tender, skin-colored, sharply demarcated, and round to oval in shape. The edge is usually raised, with a central ulcer or crust. It is not associated with systemic disorders.
Chondrodermatitis nodularis chronica helicis (CNH): This is a common, benign, and painful condition of the most prominent projection of the ear, usually the apex of the helix, but it also may affect the antihelix. It is typical of the right ear of middle-aged to older men, usually fair-skinned individuals with cutaneous sun-damage. In 10–35% of cases, it may also affect women. It is rather common (in a series, the most frequent external ear condition seen in an ear-nose-throat clinic) and is probably due to prolonged and excessive pressure, leading to inflammation, edema, and ischemic necrosis. This eventually degenerates into secondary perichondritis due to the vascular characteristics of the ear. Onset may be precipitated by pressure, trauma, or cold. Sleeping on the affected side is also common. The nodule appears spontaneously and painfully, rapidly enlarging to a maximum size of 4–8 mm, after which it remains stable. It is firm, tender, skin-colored, sharply demarcated, and round to oval in shape. The edge is usually raised, with a central ulcer or crust. It is not associated with systemic disorders.
16 What is the value of pushing over the mastoid process?
Tenderness suggests suppurative mastoiditis—an ominous complication of ear infections.
19 What may induce vesicles in the auricle?
Not too many causes: (1) severe contact dermatitis (such as poison ivy); (2) varicella/zoster; and (3) Ramsay Hunt syndrome (painful and vesicular rash of the inferior portion of the auricle, due to herpetic infection of the geniculate ganglion and treated with acyclovir. See questions 48 and 49).
20 What are the causes of auricular red spots?
 Trauma: This also may result in auricular ecchymoses and even hematomas (see question 22).
Trauma: This also may result in auricular ecchymoses and even hematomas (see question 22).
 Port wine stain: Usually congenital and of only cosmetic importance. One of the most famous port wine stains in history was on the forehead of Soviet President Michail Gorbachev.
Port wine stain: Usually congenital and of only cosmetic importance. One of the most famous port wine stains in history was on the forehead of Soviet President Michail Gorbachev.
 Sturge-Weber disease: Port wine nevus on the upper part of the scalp, associated with intracranial vascular abnormalities that may cause cerebellar calcifications and seizures.
Sturge-Weber disease: Port wine nevus on the upper part of the scalp, associated with intracranial vascular abnormalities that may cause cerebellar calcifications and seizures.
22 What is a tender and swollen auricle?
It is an uncommon but dramatic event. A diffusely swollen auricle is usually due to:
 Trauma: Easily identifiably by a history of recent altercation, especially if supported by other evidence of trauma, like a broken nose or a black eye. In fact, a “cauliflower” ear auricle is a time-honored occupational hazard of boxers, first portrayed in a beautiful Hellenistic statue of a resting fighter (Fig. 5-4). Unless evacuated, auricular hematomas heal with fibrosis and deformity and may even result in hearing loss. For instance, it has been suggested that Edison’s deafness was the result of having been picked up by the ears as a child. Still, there is no evidence that he had a cauliflower ear. President Johnson, on the other hand, contributed to our advance in veterinary medicine by demonstrating that cauliflower ears do not occur in dogs, especially beagles. In fact, he used to pick up his pooch by the ears and then toss him around in front of the press corps. LBJ, however, had no ear problems we know of, with the possible exception of selective deafness to war protesters in nearby Lafayette Park.
Trauma: Easily identifiably by a history of recent altercation, especially if supported by other evidence of trauma, like a broken nose or a black eye. In fact, a “cauliflower” ear auricle is a time-honored occupational hazard of boxers, first portrayed in a beautiful Hellenistic statue of a resting fighter (Fig. 5-4). Unless evacuated, auricular hematomas heal with fibrosis and deformity and may even result in hearing loss. For instance, it has been suggested that Edison’s deafness was the result of having been picked up by the ears as a child. Still, there is no evidence that he had a cauliflower ear. President Johnson, on the other hand, contributed to our advance in veterinary medicine by demonstrating that cauliflower ears do not occur in dogs, especially beagles. In fact, he used to pick up his pooch by the ears and then toss him around in front of the press corps. LBJ, however, had no ear problems we know of, with the possible exception of selective deafness to war protesters in nearby Lafayette Park.
 Relapsing polychondritis: May affect all facial cartilages, including the alar of the nose and the auricular of the ear(s).
Relapsing polychondritis: May affect all facial cartilages, including the alar of the nose and the auricular of the ear(s).
24 Why should one inspect (and palpate) the postauricular space?
To rule out mastoiditis in patients complaining of earache. In this case, there will be exquisite tenderness in the 1 -cm crescent-shaped depression immediately behind the external auditory canal (and also on the mastoid tip, see question 16). In addition, there may be (1) a palpable posterior auricular node (presenting as a nodule in the area of the mastoid process); and (2) a positive Battle’s sign (ecchymosis over the mastoid, most often due to trauma and indicative of basilar skull fracture).
25 When does Battle’s sign occur?
It usually occurs approximately 48 hours after the traumatic event.
B. Middle Ear (Tympanic Cavity)
C. Otoscopic Examination
36 Other than cerumen, what else may prevent visualization of the tympanic membrane?
 Otitis externa (also called swimmer’s ear): Swelling and erythema of the ear canal (see questions 13 and 14).
Otitis externa (also called swimmer’s ear): Swelling and erythema of the ear canal (see questions 13 and 14).
 Exostosis: Bony protuberance(s) covered by normal skin and projecting into the canal’s lumen making visualization difficult. Often bilateral.
Exostosis: Bony protuberance(s) covered by normal skin and projecting into the canal’s lumen making visualization difficult. Often bilateral.
 Furuncle(s): Exquisitely tender, erythematous, and inflammatory nodule(s) on the canal’s wall.
Furuncle(s): Exquisitely tender, erythematous, and inflammatory nodule(s) on the canal’s wall.
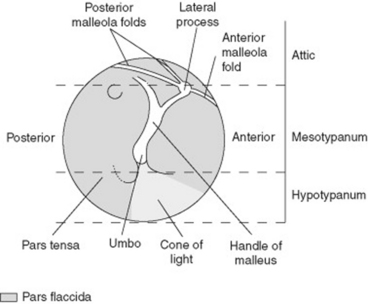
38 What does the normal tympanic membrane look like?
As pale, gray, translucent, and surrounded by a ring (anulus in Latin). Always inspect it carefully, since this may be the site of tiny perforations. The normal tympanic membrane also includes visible projections of the malleus (hammer in Latin), the largest of the three auditory ossicles, and actually more of a “club” than a hammer. It comprises a head (caput), a neck (collum), and a handle (manubrium) (Fig. 5-5). From the base of the manubrium arises the short lateral process. The manubrium and lateral process are attached firmly to the tympanic membrane, with the lateral process projecting anteriorly and superiorly. The head articulates instead with a saddle-shaped surface on the body of the incus. Otoscopically the only visualized structures are (1) the short lateral process and the manubrium; (2) the umbo of the malleus (from the Latin umbo, boss of a shield, knob), which coincides with the head of the hammer and presents as an inferior and posterior projection through the tympanic membrane; (3) a reflective triangular cone of light, located inferiorly and anteriorly to the umbo; (4) the flaccid portion of the tympanic membrane (pars flaccida), located anteriorly and superiorly to the manubrium; and (5) the pars tensa, which is located just posteriorly to the manubrium. “Flaccida” and “tensa” reflect, respectively, areas of greater or lesser mobility of the tympanic membrane.
39 What are the distinguishing otoscopic features in purulent otitis media?
Purulent otitis media (usually bacterial) is more common in children than adults, where it presents with a rim of redness, prominent vessel dilation (injection), and outward bulging of the eardrum. Other findings include loss of markings for the umbo, loss of the light reflex, and decreased mobility on pneumatic otoscopy (see questions 52–54). At times, spontaneous perforation of the eardrum may cause purulent discharge into the canal. Symptoms include earache, fever (often quite high), and hearing loss of the conductive type.
43 What is a hemotympanum? What are the other manifestations of basilar skull fracture?
Hemotympanum is the presence of blood behind the tympanic membrane, usually due to a basilar skull fracture. It was first described by the English surgeon William H. Battle (1855–1936), along with a plethora of other signs of similar significance, including (1) Battle’s sign (hematoma over the mastoid process; see questions 24 and 25); (2) periorbital ecchymoses; and (3) rhinorrhea and otorrhea (i.e., leakage of cerebrospinal fluid through the fractured planes).
D. Pneumatic Otoscopy
F. Bedside Hearing Tests
57 What is the whispered voice test?
It is a validated and standardized screening test. To carry it out:
1. Stand behind the patient at a distance of 2 feet (i.e., around an arm’s length). This is important since it prevents lip-reading.
2. Occlude one of the patient’s ears by rubbing in a circular fashion a finger over the external auditory canal.
3. After quietly exhaling, whisper three letters (or numbers or combination thereof), and ask the patient to repeat the entire sequence.
4. If the patient can do so, the hearing is normal. If the patient gets one of three items wrong, whisper an additional sequence by using the same technique. If the patient gets two or more items wrong, the test is abnormal, and the examined ear is then further tested with a tuning fork.
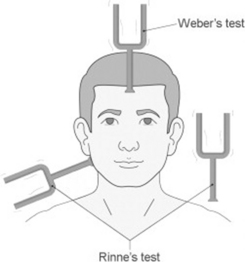
59 What are the tuning fork tests?
 Conductive loss involves the transmission of sound. This is usually due to problems of the external or middle ear (including the eardum, often perforated) and is found in patients whose speech is soften than normal.
Conductive loss involves the transmission of sound. This is usually due to problems of the external or middle ear (including the eardum, often perforated) and is found in patients whose speech is soften than normal.
 Sensorineural loss involves instead the perception of sound. This is usually due to problems of the inner ear (cochlea) or its neural connections/centers and is found in patients whose speech is louder than normal. In fact, most neurosensory loss is the result of presbycusis (i.e., the aging-related degenerative loss of the inner ear receptor/auditory nerve).
Sensorineural loss involves instead the perception of sound. This is usually due to problems of the inner ear (cochlea) or its neural connections/centers and is found in patients whose speech is louder than normal. In fact, most neurosensory loss is the result of presbycusis (i.e., the aging-related degenerative loss of the inner ear receptor/auditory nerve).
60 How do these tests work?
By the principle that in patients with hearing loss, sound conducts preferentially through the bone. The two tests most commonly used for this purpose are Weber and Rinne, whose combination can separate conductive from neurosensory deafness (Fig. 5-6).
1 Arbit E. A sensitive bedside hearing test. Ann Neurol. 1977;2:250-251.
2 Brady PM, Zive MA, Goldberg RJ, et al. A new wrinkle to the earlobe crease. Arch Intern Med. 1987;147:65-66.
3 British Society of Audiology. Recommended procedure for Rinne and Weber tuning-fork tests. Br J Audiol. 1987;21:229-230.
4 Browning GG, Swan IRC. Sensitivity and specificity of Rinne tuning fork test. Br Med J. 1988;1297:1381-1382.
5 Burkey JM, Lippy WH, Schuring AG, et al. Clinical utility of the 512-Hz Rinne tuning fork test. Am J Otol. 1998;19:59-62.
6 Chole RA, Cook GB. The Rinne test for conductive deafness: A critical reappraisal. Arch Otolaryngol Head Neck Surg. 1988;114:399-403.
7 Crowley H, Kaufman RS. The Rinne tuning fork test. Arch Otolaryngol. 1966;84:70-72.
8 Doyle PJ, Anderson DW, Pijl S. The tuning fork—An essential instrument in otologic practice. J Otolaryngol. 1984;13:83-86.
9 Eekhof JA, de Bock GH, de Laat JA, et al. The whispered voice: The best test for screening for hearing impairment in general practice? Br J Gen Pract. 1996;46:473-474.
10 Elliot WJ. Ear lobe crease and coronary artery disease. Am J Med. 1983;75:1024-1032.
11 Frank STM. Aural sign of coronary artery disease. N Engl J Med. 1973;289:327-328.
12 Gelfand SA. Clinical precision of the Rinne test. Acta Otorinolaryngol. 1977;83:480-487.
13 Golabek W, Stephens SDG. Some tuning fork tests revisited. Clin Otolaryngol. 1979;4:421-430.
14 Huizing E. The early description of the so-called tuning fork tests of Weber and Rinne: I. The “Weber test” and its first description by Schmalz. Otolaryngol Rel Spec. 1973;35:278-282.
15 Jacob V, Alexander P, Nalinesha KM, et al. Can Rinne’s test quantify hearing loss? ENT J. 1993;72:152-153.
16 Johnson EW. Tuning forks to audiometers and back again. Lanryngoscope. 1970;80:49-68.
17 Johnston DE. A new modification of the Rinne test. Clin Otolaryngol. 1992;17:322-326.
18 Lichtenstein M, Bess FN, Logan SA. Validation and screening tools for identifying hearing-impaired elderly in primary care. JAMA. 1988;259:2875-2878.
19 Macphee GJ, Crowther JA, McAlpine CH. A simple screening test for hearing impairment in elderly patients. Age Ageing. 1988;17:347-351.
20 Nadol JB. Hearing loss. N Engl J Med. 1993;329:1092-1102.
21 Ng M, Tackler RK. Early history of tuning fork tests. Am J Otolaryngol. 1993;14:100-105.
22 Samuel J, Eitelberg G, Habi JI. Tuning forks: The problem of striking. J Laryngol Otol. 1989;103:1-6.
23 Sheehy JL, Gardner C, Hambley WM. Tuning fork tests in modern otology. Arch Otolaryngol. 1971;94:132-138.
24 Stankiewicz JA, Mowry HJ. Clinical accuracy of tuning fork tests. Laryngoscope. 1979;89:1956-1973.
25 Swan IRC, Browning GB. The whispered voice as a screening test for hearing impairment. J R Coll Gen Pract. 1985;35:197.
26 Wilson WR, Woods LA. Accuracy of the Bing and Rinne tuning fork tests. Arch Otolaryngol. 1975;101:81-85.