3 The Conjunctiva: Diseases and Tumours
The conjunctiva is the transparent mucous membrane lining the inner surfaces of the eyelids; it is reflected over the anterior episclera and sclera before terminating at the limbus, where it is continuous with the corneal epithelium. In the embryo the conjunctiva develops from the ectoderm covering the lids and surface of the globe, and is formed during the third month of intrauterine life as the eyelids grow together. A healthy conjunctiva is essential for normal ocular function and together with the eyelids it is critical in maintaining a suitable environment for the cornea to function as the primary refractive element of the eye. Its mucous and accessory lacrimal secretions are important components of the precorneal tear film, and their deficiency gives rise to tear film instability and poor wetting of the corneal surface, which may lead eventually to pathological changes in the cornea. It follows, therefore, that examination of the whole conjunctival surface is necessary in order to interpret signs in the cornea, and an understanding of conjunctival pathology is a prerequisite to the effective management of many corneal disorders. As part of its function in maintaining the corneal environment, the conjunctiva also has an important role in defending the eye against a variety of agents.
THE NORMAL CONJUNCTIVA
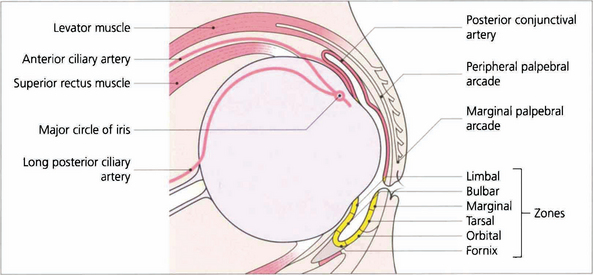
Fig. 3.1 The conjunctiva is comprised of a bulbar portion covering the anterior part of the globe (except for the cornea) and two palpebral portions that cover the posterior aspects of the upper and lower eyelids. The palpebral and bulbar conjunctiva are continuous through the upper and lower fornices. The blood supply of the conjunctiva is derived mainly from that of the eyelids, with some contribution from the anterior ciliary vessels in its bulbar portion through the limbal plexus. The nerve supply is mainly from the ophthalmic division of the trigeminal nerve but a variable proportion of the inferior conjunctiva is supplied by branches of the maxillary division.
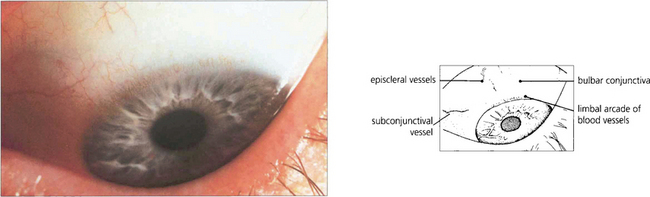
Fig. 3.2 The bulbar conjunctiva is normally transparent making the subconjunctival and episcleral blood vessels easily visible. Its anterior limit is the limbus where the epithelium becomes continuous with that of the cornea. The normal limbal arcade of blood vessels (formed by anastomosis of the terminal branches of the posterior conjunctival and anterior ciliary vessels) may extend a short distance on to the cornea but in so doing terminates in an even border on the clear cornea.
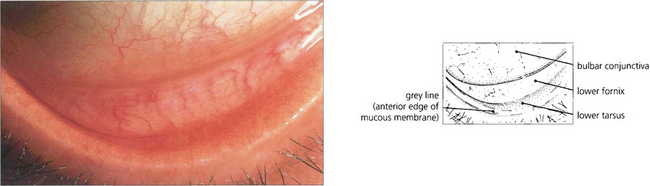
Fig. 3.3 The lower palpebral conjunctiva may be readily inspected by gentle downward traction on the lower eyelid. It is slightly thicker than the bulbar conjunctiva and is highly vascular, especially in its tarsal portion where it derives its blood supply from the tarsal arcades. The lower fornix itself has few blood vessels but a larger amount of lymphoid tissue and mucus-secreting glands.
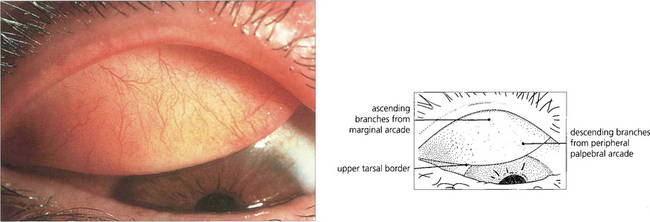
Fig. 3.4 The upper tarsal conjunctiva is inspected by everting the upper eyelid. As in the lower lid, it is firmly adherent to the underlying tarsal plate. The blood supply is derived from the palpebral arcades, of which the branches are readily visible. A small number of lymphoid follicles can often be seen at the medial and lateral aspects of its upper border.
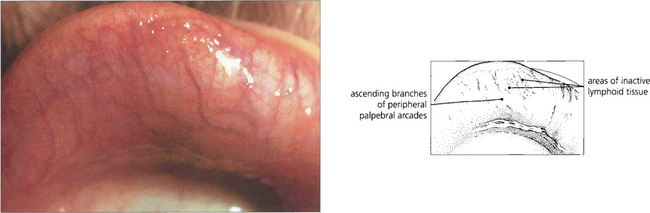
Fig. 3.5 The upper fornix is visible only on double eversion of the upper eyelids using Desmarres’ retractor. Here the posterior conjunctival vessels are visible and interspersed with yellowish patches of inactive lymphoid tissue. It is particularly important to examine the upper fornix when searching for foreign bodies or in cases of suspected chlamydial conjunctivitis when enlarged follicles are seen (see Ch. 4).
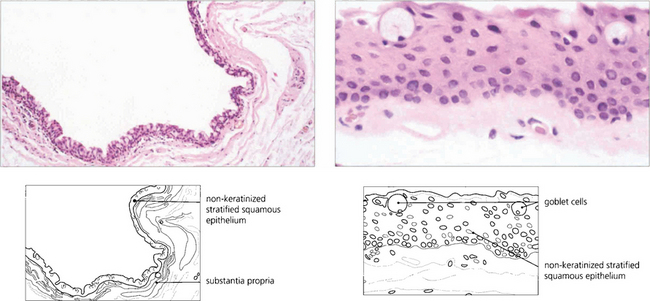
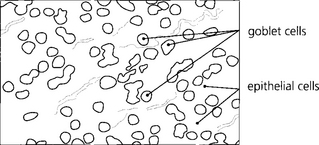
Fig. 3.6 The microscopic anatomy of the conjunctiva shows it to consist of non-keratinized squamous epithelium overlying a substantia propria. In its tarsal portion, the connective tissue elements of the latter form a fine network creating a papillary structure, but towards the fornices it is looser and contains elastic fibres, blood vessels and lymphoid tissue. In addition, the conjunctiva contains numerous goblet (mucus-secreting) cells, especially in the fornices, and the accessory (lacrimal) glands of Krause and Wolfring.
PATHOLOGICAL CHANGES OF THE CONJUNCTIVA
Causes of papillary and follicular conjunctivitis are listed in Table 3.1.
| Papillae | Follicles |
|---|---|
| Allergic conjunctivitis; atopic, vernal, seasonal or perennial | Virus infection: adenovirus, herpes simplex, molluscum contagiosum |
| Topical preparations: drops, preservatives, ointments | Cnlamydial infection: trachoma (subtypes A–D), paratrachoma (subtypes E–K) |
| Chronic 1irritation: giant papillary conjunctivitis, superior limbic conjunctivitis, dry eyes | Drug induced: glaucoma, antiviral drops |
| Lymphoid disease: reactive hyperplasia, conjunctival lymphoma |
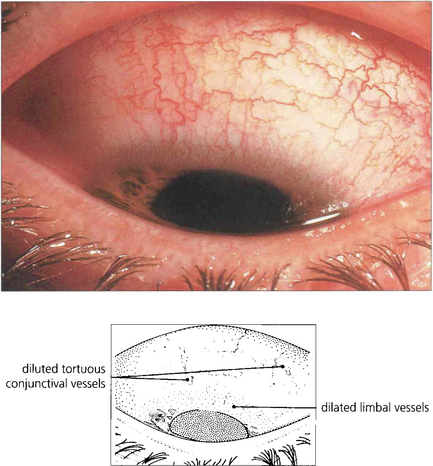
Fig. 3.9 Hyperaemia of the conjunctiva may occur as part of any acute inflammatory process or in response to chronic irritative factors. There is an increase in the number, calibre and tortuosity of the vessels, producing a characteristic bright red appearance. Hyperaemia is often associated with increased vascular permeability and oedema or cellular infiltration.
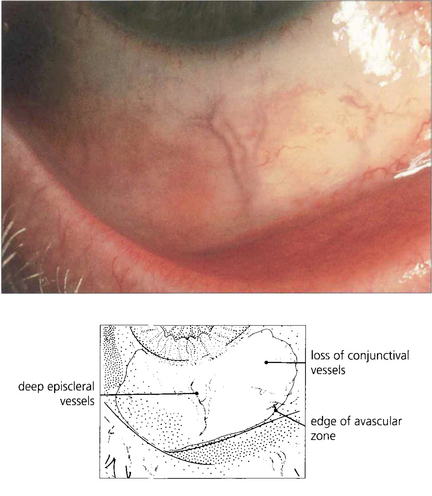
Fig. 3.10 Avascularity of the conjunctiva occurs as a result of vascular endothelial damage to the conjunctival vessels from toxic or chemical insult. The affected conjunctiva is blanched. Depending on the degree of penetration of the chemical agent, the episcleral and scleral vessels may be spared, as in this example. Such changes are most commonly seen acutely following alkali burns but may also follow subconjunctival antibiotic injections or prolonged use of topical antiviral preparations, as in this case, resulting from trifluorothymidine administration, an antiviral agent once used to treat herpes simplex keratitis.
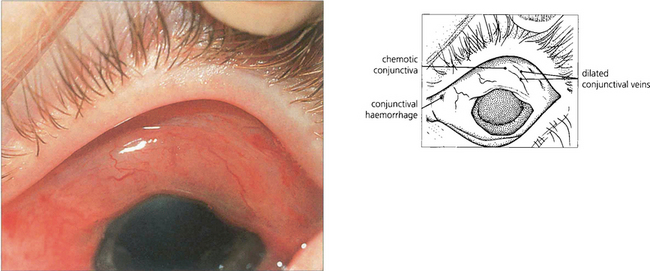
Fig. 3.11 Congestion of the conjunctival vessels arises as a result of impaired venous drainage or increased permeability which, if severe, may produce oedema of the conjunctiva (chemosis). The characteristic dusky red coloration results from increased vascular stasis within the conjunctiva. Chemosis without venous congestion occurs most commonly in association with acute allergic states when the pale swollen conjunctiva takes on a jelly-like appearance (see Fig. 5.2).
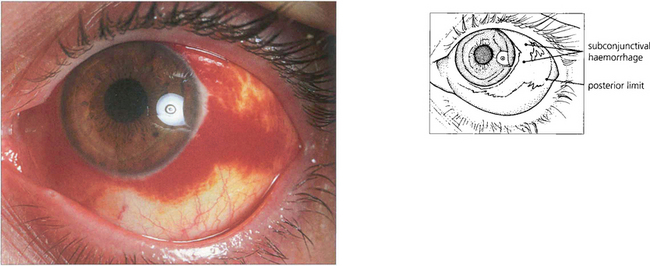
Fig. 3.12 Subconjunctival haemorrhages most frequently arise spontaneously and appear as red patches extending to the limbus. They may result from an episode of raised venous pressure (e.g. following coughing) or from trauma and very rarely from blood dyscrasias or vessel anomalies. With head trauma, if no posterior limit to the haemorrhage is defined, the blood may have resulted from a middle or anterior cranial fossa fracture and patients should be examined with this in mind.
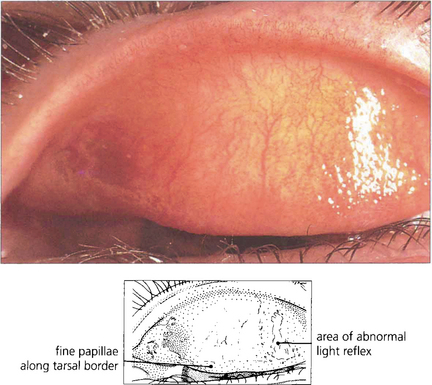
Fig. 3.13 Papillary hypertrophy is caused by the conjunctiva being thrown into folds and characterizes the subacute stage of many types of inflammation. Basically, the papillae represent a vascular response with an exaggeration of some aspects of the normal conjunctival anatomy. Clinically they can be recognized as small elevations of the conjunctiva that produce a slightly granular or velvety appearance. They break up the smooth glistening light reflex of normal conjunctiva. In this example, the minute surface irregularity produced by the individual papillae are highlighted in the light reflex laterally. Each papilla contains a central dilated arteriole with a surrounding clear or slightly infiltrated zone of swollen conjunctiva. Usually, papillae can be seen only on biomicroscopic examination, but in some chronic conditions giant papillae may form that can be seen with the naked eye.
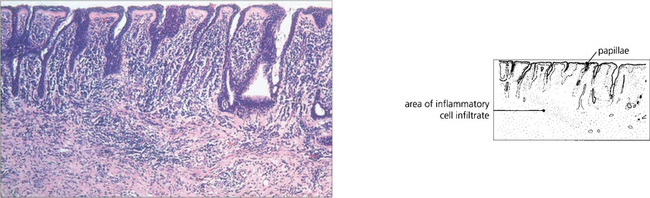
Fig. 3.14 Histologically, the conjunctiva between individual papillae is tethered to the underlying tarsal plate by the fibrous network normally present in the substantia propria, and the papillae are produced by oedema, cellular infiltration and vasodilatation within the spaces of this meshwork. Many chronic inflammatory cells are present.
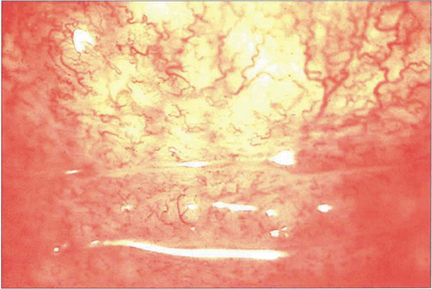
Fig. 3.15 The clinical appearance of follicles is of large pink or pale grey elevations lying beneath the conjunctival epithelium with small blood vessels frequently visible on their surface. In the early stages, they are present only in the fornices but may extend on to the tarsi if the disease becomes chronic. Follicles are associated particularly with conditions in which cell-mediated immune mechanisms are involved, such as viral infections and drug hypersensitivity. They can be seen in normal conjunctiva in childhood.
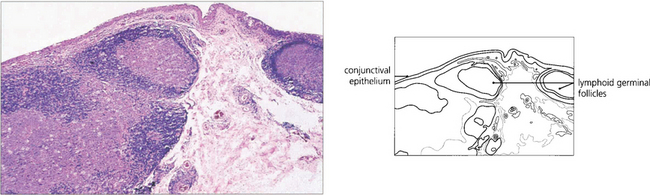
Fig. 3.16 Conjunctival follicles are collections of lymphoid germinal follicles in the subepithelial stroma with immature cells centrally and mature cells peripherally.
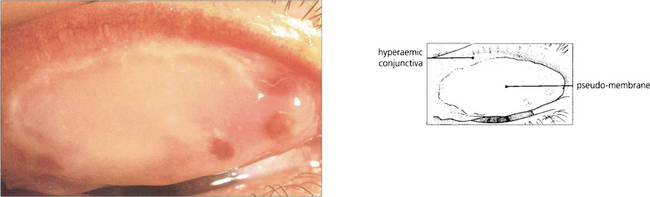
Fig. 3.17 Pseudomembrane formation on the surface of the conjunctiva is seen in patients with severe acute conjunctivitis. A coagulum of fibrin and proteinaceous exudate forms, and is initially loosely adherent to the underlying tissues from which the pseudomembrane may be separated without causing bleeding from the surface. A true membrane is firmly adherent to the conjunctival epithelium and attempted removal gives rise to a bleeding conjunctival surface. Subsequent organization of the membrane produces scar tissue.
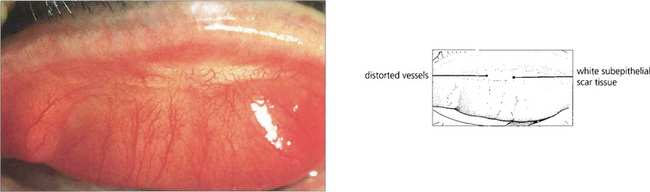
Fig. 3.18 Conjunctival scarring may be the end-result of a wide variety of inflammatory processes. Its effects on the eye vary from insignificant to devastating, depending on its effects on the tear film and lid architecture. Subepithelial fibrosis is seen as white tissue, usually with associated distortion of the overlying superficial blood vessels. Localized superficial linear scarring may have little clinical significance, as in this example, which followed a severe viral conjunctivitis.
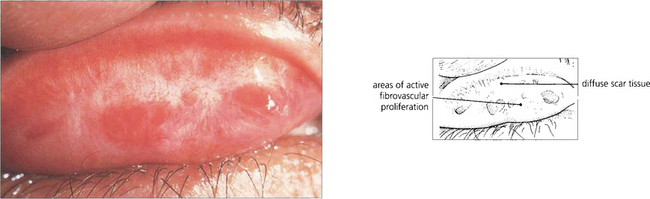
Fig. 3.19 Extensive diffuse scarring (resulting from trachoma in this case) may have serious effects on the eye by diminishing the protective functions of the lids and conjunctiva. Contraction of the scar may result in entropion, trichiasis and lid shortening. Obliteration of the normal mucus-secreting cells may affect the stability of the tear film. This example also shows some fibrovascular proliferation in the superficial scar tissue; subsequently this may add to the already extensive scar by further fibrosis (see also Ch. 4).
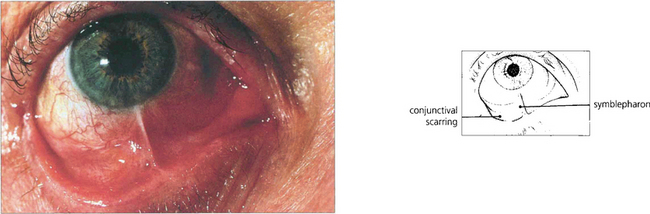
Fig. 3.20 Symblepharon is an adhesion between the conjunctiva covering the lids and the globe. In this example, severe conjunctival adhesions developed following an alkali burn. Disorders of ocular motility and poor lid closure with corneal exposure or instability of the tear film may result.
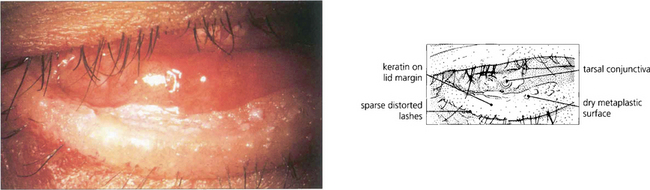
Fig. 3.21 Squamous metaplasia of the conjunctiva can be recognized clinically by altered wetting characteristics of the affected conjunctiva. Such changes usually arise as a result of prolonged chronic inflammation and eventually lead to keratinization which may cause further damage to an already compromised cornea.
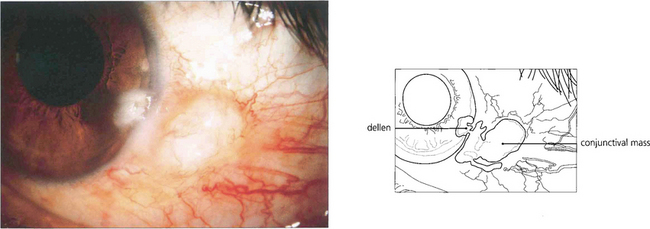
Fig. 3.22 A paralimbal mass alters the tear film and, in particular, causes a meniscus and thinning of the tear film over the adjacent limbus and cornea. This can lead to localized corneal drying, thinning and epithelial ulceration, known as a dellen. The condition resolves on treatment or removal of the lump.
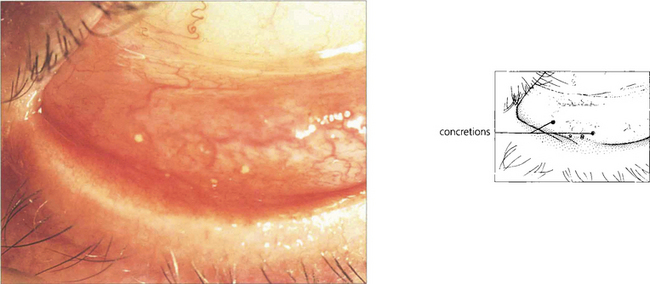
Fig. 3.23 Concretions are minute, hard, yellow spots seen in the palpebral conjunctiva of elderly people, although they may also be the result of chronic inflammatory disease. They rarely cause symptoms but, if large, they occasionally project through the surface of the conjunctiva to produce a foreign body sensation and will stain with Bengal Rose or fluorescein. If necessary, they may be removed using a needle point under topical anaesthesia. Concretions are formed by cellular degeneration when the debris remains trapped in small recesses of the conjunctiva and becomes calcified.
DRUG-INDUCED CHANGES
Contact hypersensitivity reactions may arise in the conjunctiva or eyelids from a wide variety of agents but are commonly related to the use of cosmetic preparations, contact lens solutions or topical medications (eye drops or ointments). Substances may also be transferred to the periocular tissues from the hand by means of eye-rubbing or contact with bedlinen. The skin changes on the eyelids resemble those of a contact dermatitis, whereas in the conjunctiva there is primarily a follicular response. Symptoms include redness, irritation, discharge and, especially, itching of the eye. Patients may also complain that symptoms are most marked immediately after application of the drop or ointment. The pathogenesis involves delayed (cell mediated) hypersensitivity; the condition evolves gradually over several days or weeks unless previous sensitization has occurred, in which case its onset may be much more acute.
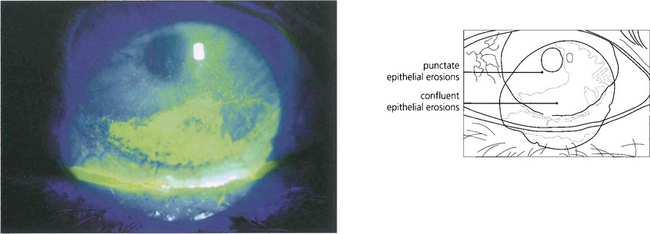
Fig. 3.25 Superficial punctate erosions on the cornea are a common feature of drug toxicity. The patient usually has a mildly red, inflamed eye with some discomfort. The erosions are usually more pronounced over the inferior cornea where the exposure to the topical drug is greatest. They stain with Bengal Rose or fluorescein.
By courtesy of Mr M G Falcon.
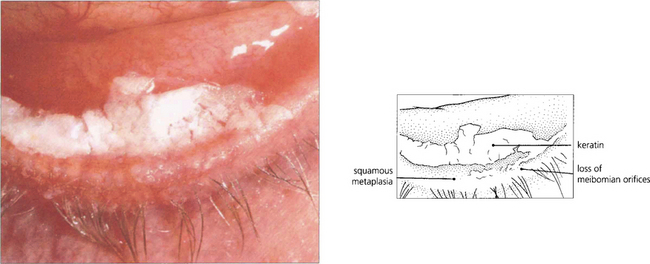
Fig. 3.26 This patient has developed squamous metaplasia of the conjunctival surface near the lid margin, following prolonged idoxuridine therapy, once used to treat herpes simplex keratitis. A thick, white, keratin plaque is present, with the normal conjunctival mucous membrane replaced by stratified squamous epithelium which has obliterated the meibomian orifices along the lower lid margin.
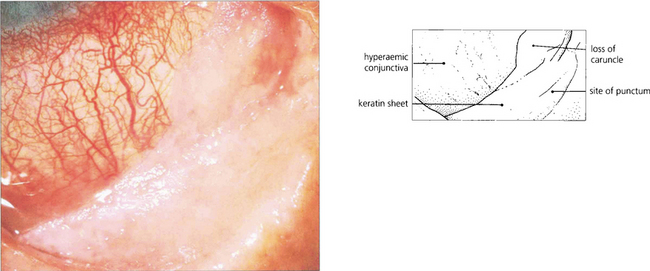
Fig. 3.27 Dyskeratotic changes are seen over the whole of the lower fornix and tarsus with extension on to the bulbar conjunctiva on the medial side in this unusual example in which pilocarpine and neutral adrenaline (epinephrine) drops had been used over many years. Keratin sheet formation is seen as a whitish, nonwetting surface in the areas of conjunctiva that might be expected to have had most contact with the drug. The lower punctum appears to have been completely obliterated and the remaining visible conjunctiva is hyperaemic.
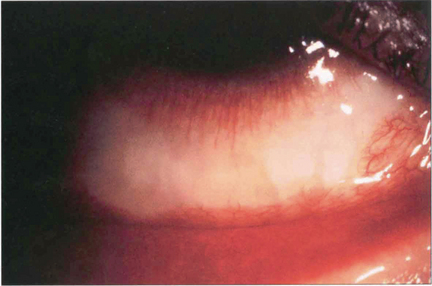
Fig. 3.28 Topical aminoglycoside antibiotics can cause bulbar conjunctival ischaemia, as in this case following several weeks’ administration of tobramycin. This change reverses after cessation of the drug.
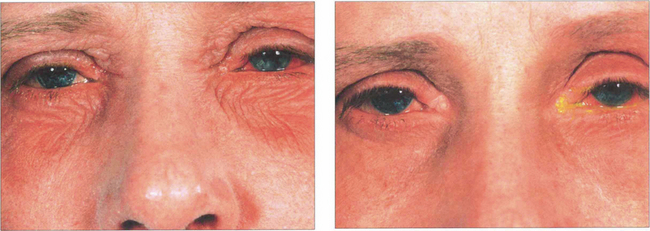
Fig. 3.29 This patient with atopic keratoconjunctivitis has inferior periocular dermatitis following treatment of both eyes with ointment (left). As is characteristic, the skin became less erythematous and tender within days after the ointment was discontinued (right).

Fig. 3.30 In a more severe reaction, such as in this case where the patient was given antibiotic ointment to the right eye, the swelling and erythema are more marked, the area of involvement is more extensive and the skin has a weeping eczematous appearance.
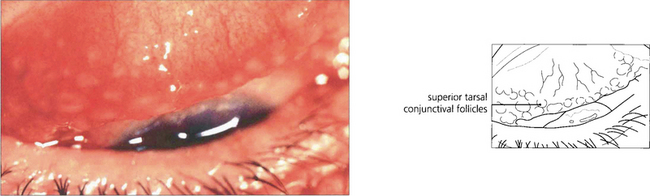
Fig. 3.31 A wide range of topical medications such as antibiotics and antiglaucoma preparations, such as brimonidine and preservative agents can produce a follicular response, most commonly seen in the inferior fornix. Reversal of the changes occurs over a period of several weeks when the patient is changed to treatment with a preservative-free solution or an alternative drug.
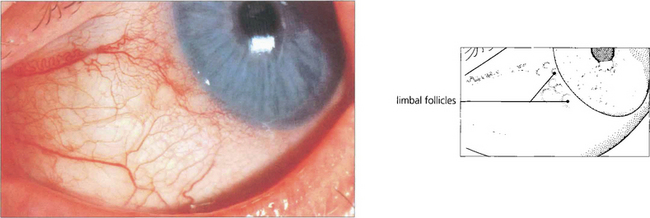
Fig. 3.32 Bulbar follicles are frequently seen in drug hypersensitivity reactions. This figure shows a typical grouping of bulbar follicles at the limbus of a sensitized patient who has recommenced treatment with trifluorothymidine drops (once used to treat herpes simplex keratitis).
By courtesy of Dr A H S Rahi.
CHEMICAL BURNS
Acid burns coagulate and precipitate the superficial proteins of the conjunctiva and cornea; they do not penetrate the eye and so tend to cause only superficial scarring. In contrast, alkalis saponify the lipid in cell membranes and rapidly penetrate the eye producing devastating damage to both blood vessels and intraocular structures within minutes of contact. First-aid measures, especially prompt immersion of the eye in cold water or irrigation of the conjunctiva with bicarbonate solution to dilute and remove the alkali are vital in reducing damage. Alkali burns are followed by collagenase secretion from the limbal conjunctiva in the recovery phases; this may produce corneal melting and is compounded by destruction of the accessory lacrimal glands and goblet cells in the conjunctiva, producing tear film abnormalities. Corneal ulceration is the most serious complication of chemical injury and can lead to perforation. Decreased collagen synthesis is associated with local ascorbate deficiency and keratocyte loss. Damage to the limbus results in delayed epithelialization with conjunctiva-derived epithelium resulting in a vascularized opaque corneal surface and very poor prognosis with corneal transplantation. Surgical management of these eyes involves either autologous or donor limbal stem cell transplantation (see Ch. 6).
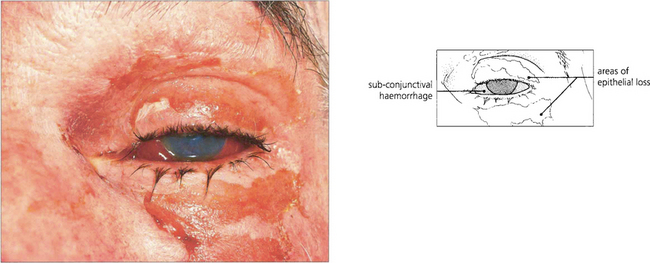
Fig. 3.33 This patient shows acute changes in the skin and outer eye immediately after an ammonia burn. There are large sloughing areas with erythema of the skin of the upper and lower eyelids. The conjunctiva is chemotic and haemorrhagic and there is loss of corneal epithelium over the lower half of the cornea.
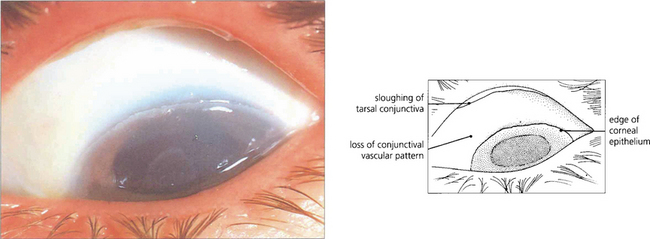
Fig. 3.34 This is the appearance of the bulbar conjunctiva immediately after a severe alkali burn, showing the typical appearance with complete absence of the normal conjunctival vascular markings in a dense, white, slightly chemotic conjunctiva. There is complete loss of the whole corneal epithelium and early sloughing of necrotic conjunctiva beneath the upper tarsus.
By courtesy of Professor R J Buckley.
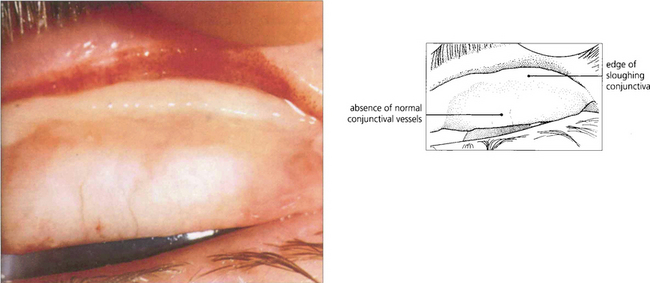
Fig. 3.35 In the same patient as Fig. 3.34, there is extensive conjunctival necrosis 3 weeks after the ammonia burn. The whole upper tarsal conjunctiva is pale, yellowish and swollen, with poorly defined vessels. The upper edge is starting to slough away from the underlying tissues. Healing will occur with fibrosis of the lid leading to cicatricial entropion, tear film deficiency and further corneal damage.
By courtesy of Professor R J Buckley.
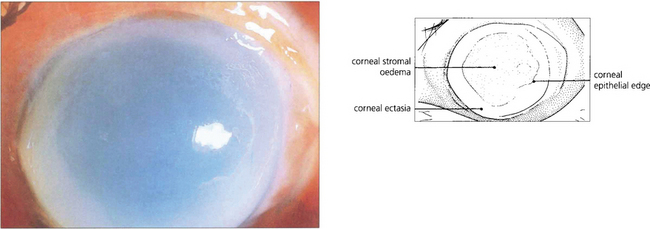
Fig. 3.36 The corneal changes of the same patient are shown 6 weeks later. The corneal stroma has become oedematous and is undergoing melting, as evidenced by the ectatic shape and peripheral guttering. There is failure of epithelialization over the central part of the cornea.
By courtesy of Professor R J Buckley.
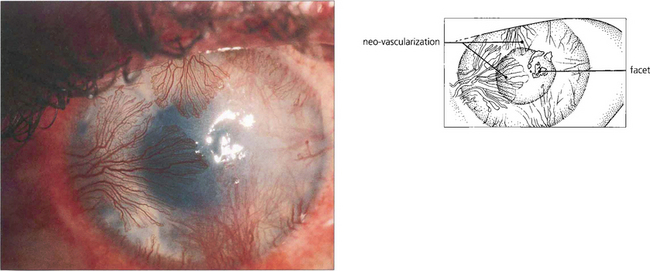
Fig. 3.37 Loss of the limbal stem cells leads to healing with dysplastic epithelium derived from the conjunctiva. In this eye there is massive neovascularization of the cornea with diffuse stromal scarring associated with thinning and faceting of the cornea. The corneal problems are usually compounded by abnormalities in the tear film from the conjunctival damage; this, together with the neovascularization, produces an extremely poor prognosis for corneal grafting.
By courtesy of Dr A H S Rahi.
NONPIGMENTED TUMOURS OF THE CONJUNCTIVA
Tumours may be classified, according to their tissue of origin, into those arising from the surface epithelium (or its associated glandular elements), connective tissue, vascular tissue, lymphoid tissue or peripheral nerves. Some common conjunctival tumours are listed in Table 3.2. Pigmented lesions of the conjunctiva are an important group of conditions that are considered in detail separately.
| Cell/tissue of origin | Benign | Malignant |
|---|---|---|
| Epithelium | Hyperplasia, papilloma, CIN* | Squamous cell carcinoma |
| Vascular | Haemangioma | Kaposi’s sarcoma |
| Lymphoid system | Reactive lymphoid hyperplasia | Lymphoma |
| Nerve | Neurofibroma | |
| Melanocytic | Naevus, melanocytosis | Melanoma |
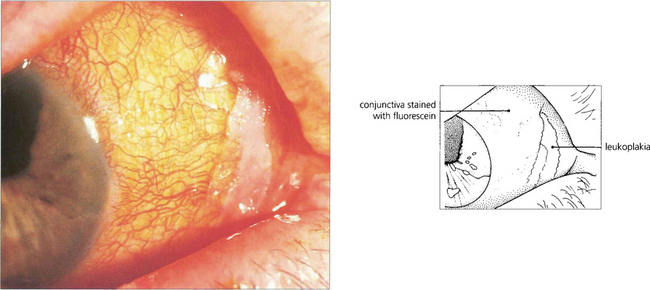
Fig. 3.38 Dyskeratosis is a feature of dysplasia, now known as conjunctival intraepithelial neoplasia (CIN); this encompasses a variety of pathological changes seen in the conjunctival and corneal epithelium which may present clinically as a dry white plaque on the surface of the globe (leukoplakia). The disorder may arise as a result of chronic irritative factors such as solar radiation and topical drug therapy; it may also be due to human papilloma virus infection. This dry, keratinized, white plaque shows clearly against the chronically inflamed conjunctiva which has taken up fluorescein stain.
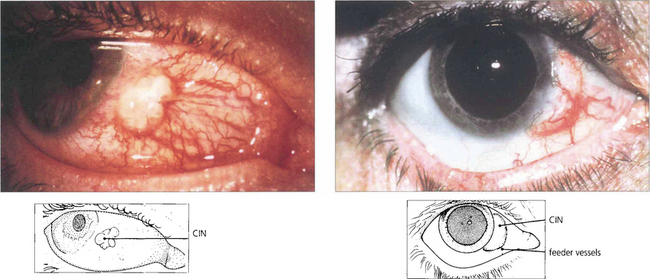
Fig. 3.39 The limbus and interpalpebral aperture are the commonest sites for CIN which may develop over a pinguecula or pterygium. Such lesions should be excised if there is any suspicion of malignancy.
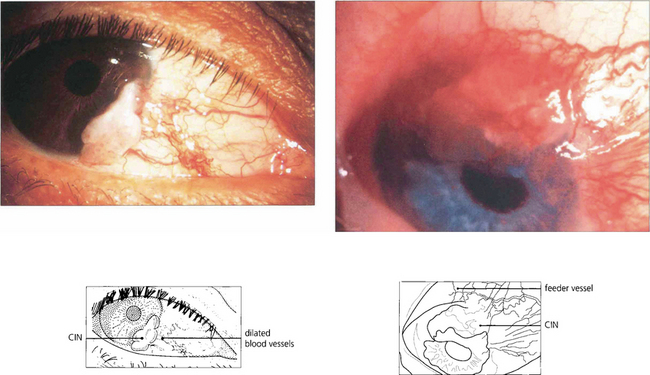
Fig. 3.40 Risk factors for malignancy are solar exposure and human immunodeficiency virus (HIV) infection. Malignant change is suggested by the development of feeding vessels and increased bulk. Tumours can invade the orbit, but invasion of the eye is uncommon.
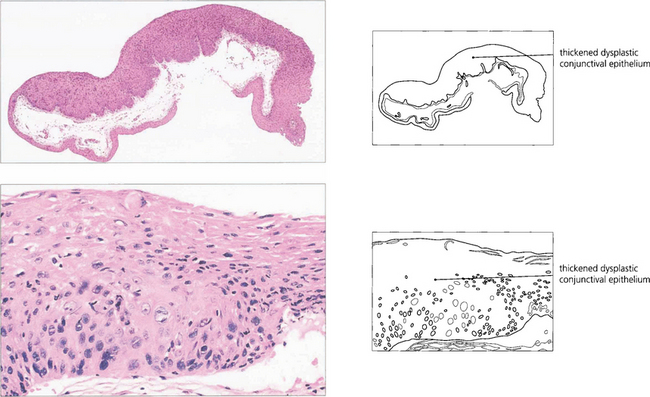
Fig. 3.41 CIN – low and high magnification. The lesions show dysplastic changes throughout the full thickness and are thus CIN stage 3 (carcinoma in situ).
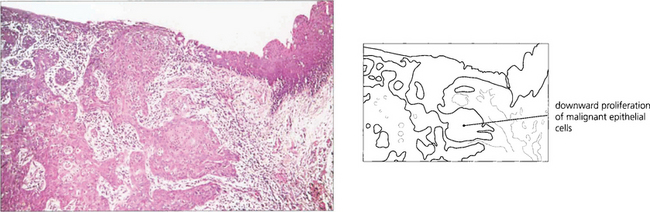
Fig. 3.42 Histological appearance of a moderately well-differentiated squamous cell carcinoma with downward proliferation of malignant cells.
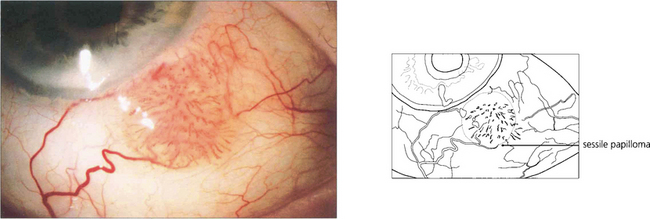
Fig. 3.43 Papillomas arising in the conjunctiva may be either sessile or pedunculated lesions with a slightly irregular surface. They occur most commonly in patients over 40 years of age either at the caruncle or in the fornices, and are occasionally found in the lacrimal canaliculi or lacrimal sac. They may occasionally be multiple. This is an example of a sessile papilloma on the bulbar conjunctiva. Treatment is by excision and should, where possible, include an area of healthy conjunctiva around the base.

Fig. 3.44 Histological examination shows fingers of non-keratinized stratified squamous epithelium around a central fibrovascular stalk. Goblet cells are present within the proliferating epithelium. Human papilloma viruses are implicated in the pathogenesis.
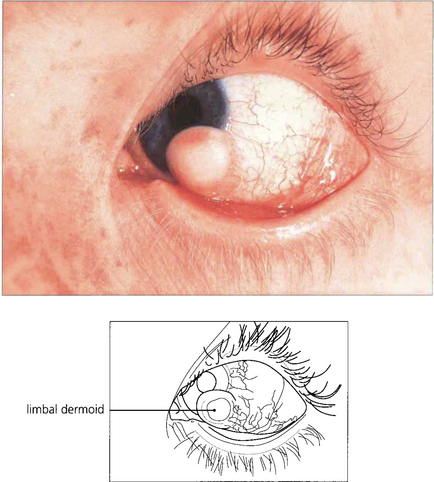
Fig. 3.45 Limbal dermoids are congenital tumours of mesodermal and ectodermal origin. They appear as raised, circumscribed, pale yellowish lesions and are generally situated at the lower temporal limbus where they involve the cornea, conjunctiva and sclera. They are normally present at birth and, although enlargement is unusual, removal may be justified on cosmetic grounds when the child is nearing school age. If the deeper layers of the cornea are involved, a lamellar keratoplasty may be required to restore corneal thickness and reduce astigmatism.
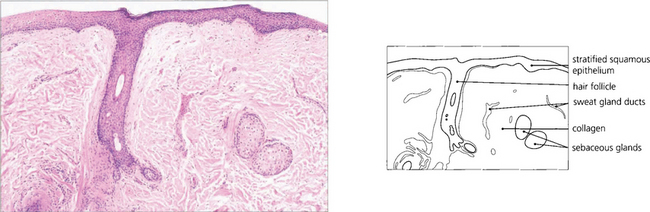
Fig. 3.46 Limbal dermoids are solid rather than cystic. Histological examination shows dense collagenous tissue with dermal elements covered by stratified squamous epithelium. A variety of tissues may be present within the collagen matrix, as in this example, where islands of sebaceous glands, sweat gland ducts and a hair follicle are visible.
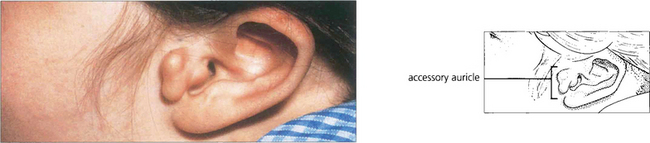
Fig. 3.47 Children with limbal dermoids should be examined for other signs of Goldenhar’s syndrome (first branchial arch syndrome—accessory auricles, limbal and orbital dermoids, sometimes with maldevelopment of the jaw).

Fig. 3.49 This small haemangioma of the conjunctiva had been present for many years with no alteration in size. The dilated blood vessels reflect the vascular nature of the lesion and should be distinguished from the enlarged feeding vessels associated with malignant tumours.
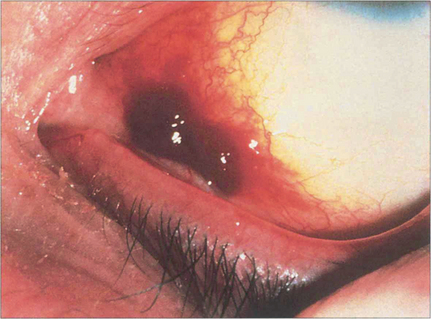
Fig. 3.50 Kaposi’s sarcoma is a multicentric tumour thought to be of vascular endothelial cell origin. It was rare until the advent of HIV infection in which it is related to infection with herpes virus type 8. Mucous membrane involvement, as in this example, in the conjunctiva, is usually a later manifestation of the condition, although about 20 per cent of patients with Kaposi’s sarcoma show conjunctival involvement. The lesions appear as bright red or purplish fleshy masses and haemorrhages are frequently present within the tumour reflecting the highly vascular nature of the condition. They are radiosensitive and can therefore be treated by radiotherapy if they become large and bulky.
By courtesy of Mr Bruce Mathalone.
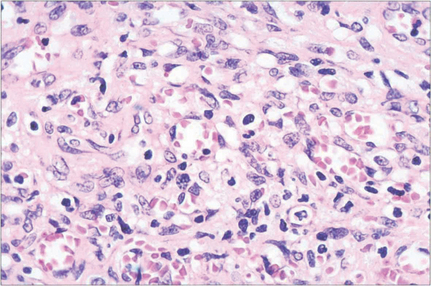
Fig. 3.51 Histological examination shows proliferating spindle-shaped endothelial cells with vascular spaces and a chronic inflammatory cell infiltrate.
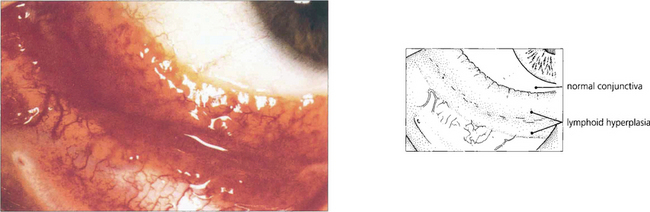
Fig. 3.52 Reactive lymphoid hyperplasia and lymphoma cannot be distinguished from each other on clinical findings. Reactive lymphoid hyperplasia presents as a slowly growing, diffuse mass involving the bulbar conjunctiva and fornices. There are no inflammatory changes in the unaffected normal-appearing conjunctiva and therefore the condition should not be confused with lymphoid follicles seen in cases of conjunctivitis.
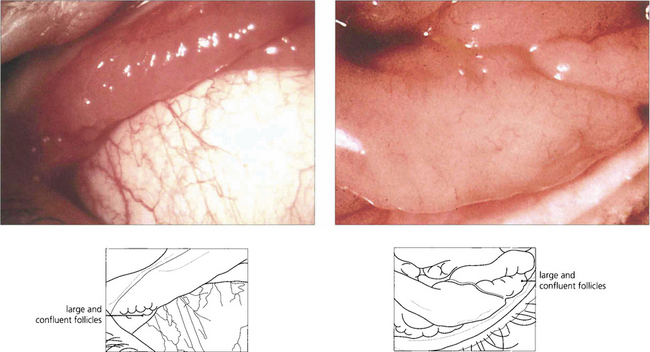
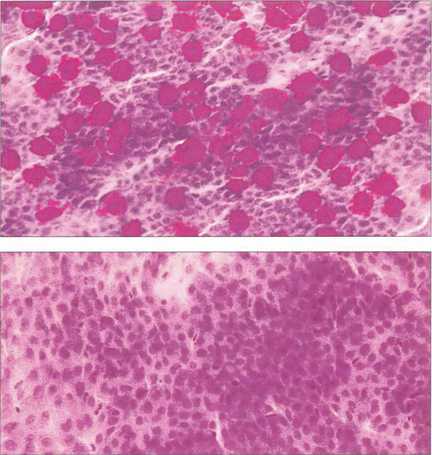
Fig. 3.53 Conjunctival lymphoma involving upper (left) and lower (right) fornices. Large follicular masses usually involve the fornices in both eyes. The histological appearance of conjunctival lymphomas is complex and monoclonal antibodies and molecular genetics are necessary to distinguish reactive lymphoproliferation from lymphoma. Conjunctival lymphomas are usually B-cell tumours arising from the mucosa-associated lymphoid tissue (MALT) system, and are known as ‘maltomas’. Assessment for orbital and extraocular systemic lymphoma is required. Lymphomas restricted to the conjunctiva respond well to radiotherapy and have a good prognosis.
PIGMENTED LESIONS OF THE CONJUNCTIVA
CLASSIFICATION OF PIGMENTED LESIONS OF THE CONJUNCTIVA
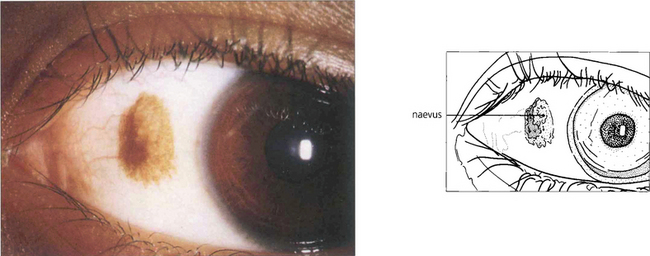
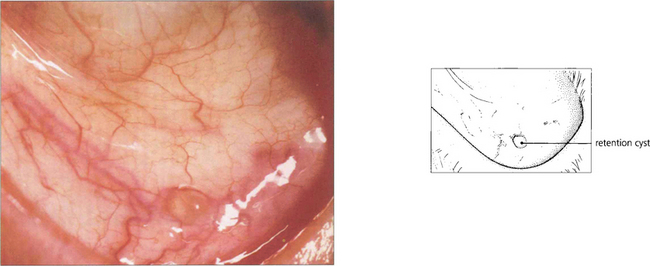
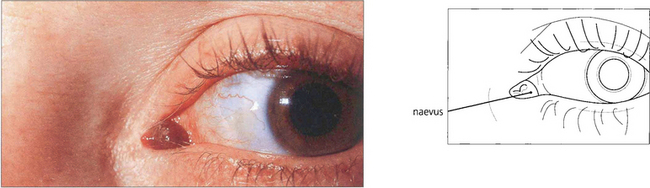
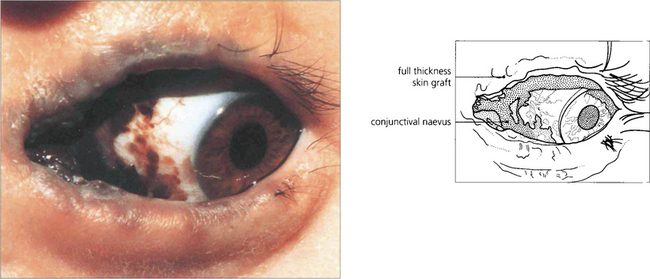
Fig. 3.54 Conjunctival naevi, although congenital, are not always present at birth and in many cases may not become apparent until they become pigmented in adulthood. They are common benign lesions, often seen at the limbus. In this example the pigmented area in the bulbar conjunctiva contrasts markedly with the white sclera. They tend to grow slowly but, provided they do not undergo rapid change, develop feeder vessels or become raised, no treatment is required.
MELANOSIS
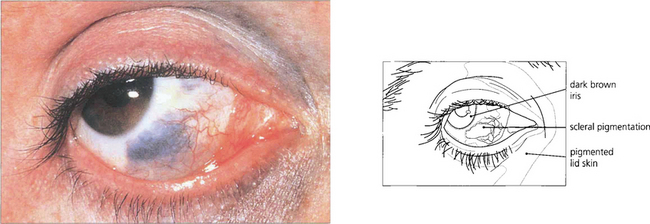
Fig. 3.58 A naevus of Ota is a blue naevus of the sclera and periorbital skin together with a diffuse naevus of the uvea. This example shows a large bluish-grey area of scleral pigmentation extending up to the limbus with an edge that is slightly mottled. Unlike conjunctival naevi this lesion does not move with the conjunctiva. The iris was darker than that in the fellow eye, indicating an associated or diffuse naevus of the uvea.
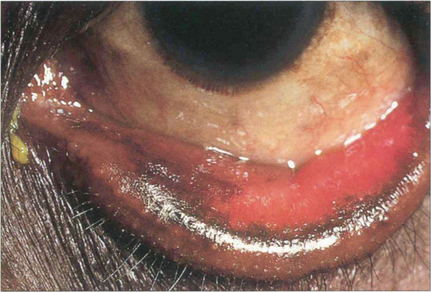
Fig. 3.59 Secondary acquired melanosis associated with long-standing conjunctival disease is shown in this case of ectropion in a black patient. Similar pronounced pigmentary changes may be seen in the conjunctiva of patients with radiation, trachoma or allergic conjunctivitis and probably reflect the high rate of conjunctival epithelial turnover associated with chronic disease. The condition is not premalignant.
MALIGNANT MELANOMA OF THE CONJUNCTIVA
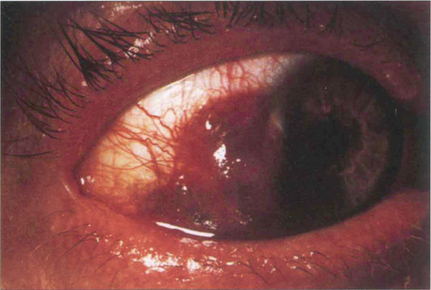
Fig. 3.60 Malignant melanomas of the conjunctiva may arise spontaneously from a pre-existing junctional or compound naevus, or from an area of primary acquired melanosis. They occur with equal frequency in males and females, most commonly between the ages of 40 and 60 years. This is an example of a malignant melanoma arising at the limbus and spreading into the cornea. Many feeding blood vessels are visible. Localized lesions may be treated by excision of the affected conjunctiva with a wide margin of tissue. The prognosis is most dependent on the location, fornix involvement being associated with the worst outcome.

Fig. 3.61 This eye shows multiple malignant melanomas of the conjunctiva arising in areas of primary acquired melanosis. This rare unilateral condition is seen in Caucasian eyes with onset in middle age and a protracted course of lesions slowly enlarging in area over many years with increasing atypical melanocytic hyperplasia. About 20 per cent of lesions become malignant. The condition is analogous to lentigo maligna of the skin. All patients should be followed at regular intervals with serial photography. Pigmented areas that increase in size or thickness or develop feeding vessels should be excised and examined histologically for evidence of malignancy. Small lesions can be treated by cryotherapy.
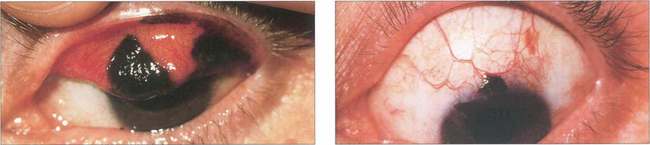
Fig. 3.62 Malignant melanomas may spread by direct invasion or by seeding to other parts of the conjunctival sac. In this example a melanoma on the upper tarsus has given rise to lesions at the lid margin and the upper limbus. In this instance exenteration of the orbit, with the eyelids, offers the only sure way of surgically removing all tumour-bearing tissue.
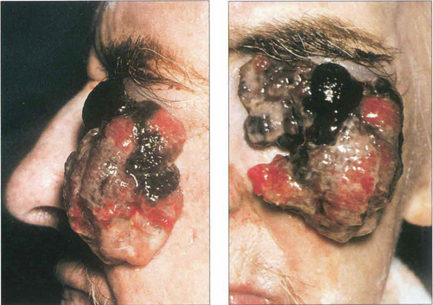
Fig. 3.63 This gross example of a neglected malignant melanoma shows a fungating tumour that has arisen from the anterior part of the globe and spread on to the cheek. In spite of its size, there was no direct invasion of neighbouring orbital or facial structures and no evidence of distant metastases.
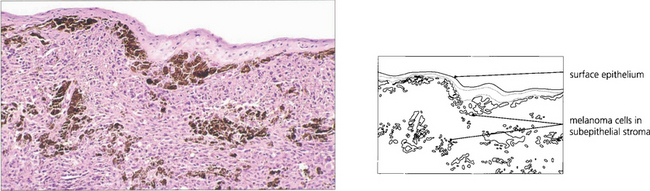
Fig. 3.64 Histological examination shows sheets of melanoma cells in the subepithelial stroma. Conjunctival melanomas have features similar to those of cutaneous melanoma. Tumours less than 1.5 mm in thickness and those on the bulbar conjunctiva carry a better prognosis than tumours on the tarsal conjunctiva.