The circulatory system consists of the heart and the vessels (tubes) which carry blood or lymph. The heart provides a force that moves blood in the vessels of the cardiovascular system. This part of the circulatory system, the cardiovascular system, ensures blood, carrying oxygen, carbon dioxide, various nutrients, metabolites, hormones and blood cells, is conveyed to, through and from the tissues and organs of the body.
Part of the circulatory system comprises lymphatic vessels which drain some of the extracellular fluid from all regions of the body except the central nervous system. The fluid in lymphatic vessels is known as lymph. It is similar to plasma but does not transport red cells. Lymph is an important means of transporting immune cells, particularly lymphocytes, and lymph vessels carry lymph into and out of lymph nodes (Chapter 8). Lymphatic vessels in the gastrointestinal system also transport lipids absorbed from the gut (Chapter 12). Lymph eventually drains into larger lymph vessels which in turn drain into the blood vessels of the cardiovascular system returning blood to the heart.
Cardiovascular system
The heart is an organ which consists of two muscular pumps that work in synchrony. The two pumps are attached side by side but blood, in adults, does not pass directly between the two sides. The heart develops (in utero) from a single tube which duplicates and twists and only takes on the adult structure and the physical separation of the two sides shortly after birth (see Mitchell B, Sharma R. Embryology: An Illustrated Colour Text. Elsevier: 2004).
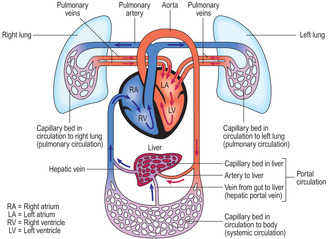
Arteries are vessels which carry blood away from the heart whilst vessels carrying blood to the heart are veins (Fig. 10.1). Blood is carried between arteries and veins in small vessels, arterioles, capillaries and venules. Veins deliver deoxygenated blood to the right side of the heart, which pumps it into pulmonary arteries and on to the lungs. In the lungs, the deoxygenated blood passes into capillaries and there it becomes oxygenated. The oxygenated blood returns to the left side of the heart via pulmonary veins. This flow of blood between heart and lungs is known as the pulmonary circulation. Simultaneously, the left side of the heart pumps oxygenated blood into the aorta (the largest artery) from where it is distributed around the whole body. Arterial blood passes through progressively branching and narrowing arterial vessels and eventually through the narrowest vessels, the capillaries. It is from capillaries that oxygen diffuses into surrounding tissues and blood becomes deoxygenated. Capillaries drain into venules and these in turn drain into veins which return the deoxygenated blood to the right side of the heart. This flow of blood around the body is described as the systemic circulation.
In some regions of the body, e.g. the liver (Fig. 10.1), in addition to arterial blood delivering oxygenated blood to capillaries, other blood enters the capillaries from a vein. In the case of the liver, capillaries draining blood from the gut join together and drain into the hepatic portal vein. This portal vein, carrying nutrients absorbed from the gut, supplies blood to capillaries in the liver. This arrangement of vessels involving two sets of capillaries joined by a vein is described as a portal circulation.
Heart
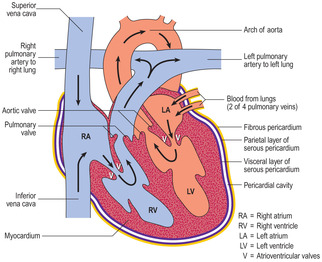
Each side of the heart has two compartments: an atrium and a ventricle (Fig. 10.2). The left atrium receives blood from the lungs in four pulmonary veins and the right atrium receives blood from the rest of the body via the superior and inferior vena cavea. The atria simultaneously contract and pump blood into the paired ventricles. The ventricles then pump the blood into either the systemic circulation (left ventricle) or the pulmonary circulation (right ventricle). Valves between each atrium and its ventricle ensure that blood does not flow back into the atria when the ventricles contract. Other valves prevent back flow of blood from the arteries to the ventricles when the ventricles relax. The contraction of heart muscle is regulated by the autonomic nervous system, though heart muscle cells have an intrinsic ability to contract.
■ Myocardium. The myocardium forms the majority of the wall of the heart: it consists mainly of cardiac muscle cells supported by sparse, fibrous connective tissue. If these muscle cells are sectioned along their length, transverse striations are apparent (Fig. 10.3), reflecting the arrangement of myofilaments in the sarcoplasm of the cells (Chapter 5). Specialised junctions (intercalated discs) attach cells together in series and may be apparent as transverse lines (Fig. 10.3). Although heart muscle cells have an intrinsic ability to contract, sympathetic and parasympathetic nerves are able, respectively, to increase and decrease the rate at which the heart beats. The contraction of cardiac muscle cells is coordinated by specialised cells in several regions of the heart and by communication, via intercalated discs, between individual muscle cells. One specialised cell type, the Purkinje cell, conducts electrical impulses to specific parts of the myocardium so that atria and ventricles contract at appropriate times and blood flows smoothly from atria to ventricles then into the arteries. Purkinje cells are distinguished by their rounded shape (Fig. 10.3) and they have a high content of glycogen.
■ Endocardium. This lines the myocardium. It is made up of a surface layer of squamous epithelial cells, their basement membrane and a sparse layer of connective tissue attaching the endocardium to the myocardium. The epithelial cells of the endocardium are similar to, and continuous with, the endothelial cells lining the blood vessels carrying blood to and from the heart.
■ Epicardium. The epicardium covers the heart and comprises a single layer of squamous epithelial cells, their basement membrane and loose connective tissue which attaches it to the underlying myocardium. Coronary blood vessels supply blood to the heart and lie in the epicardium, in which fat cells may be present in large numbers (Fig. 10.4).
The epicardium is part of a closed sac, the pericardium, which enfolds the heart (Fig. 10.2). It is the inner, visceral layer of the pericardium and is continuous with the outer parietal layer. Each of these two layers is composed of a squamous epithelium, basement membrane and supporting connective tissue and they enclose a potential space, the pericardial cavity. The secretion of minute amounts of fluid into the pericardial cavity by the lining of squamous epithelial cells ensures a relatively friction-free zone against which the heart can move and beat without damaging adjacent cells.
Connective tissue of the heart
Some connective tissue of the heart is condensed and described as a fibrous skeleton. It is a complex arrangement of dense collagen between the atria and ventricles, and around the orifices of the arteries taking blood from the heart (Fig. 10.4). The connective tissue ensures electrical discontinuity between the myocardium of the atria and ventricles except via the specialised conducting tissue; this is essential for the normal rhythm of heart contraction. In addition, the connective tissue anchors the cardiac muscle cells and is the major component of, and anchor for, the valves (Figs 10.3 and 10.4).
Angina This is caused by a slow, but progressive, reduction in the luminal diameter of the coronary arteries that supply blood to the heart and is usually due to the accumulation of fatty material in the walls of these arteries. This process, atheroma formation, may begin as early as 21years of age as a result of Western-style diets. Angina is manifested by characteristic pain which spreads across the chest wall after exercise. The pain is perceived when insufficient oxygen reaches the cardiac muscle cells and they are unable to sustain the increased rate of contraction needed for the exercise.
Myocardial infarction This is the term used to describe the pathological process of complete or incomplete obstruction of the coronary arteries supplying the heart. The blockage may be due to the deposition of fatty material in the wall of a coronary artery or the presence of a blood clot blocking a coronary artery. Once the blood supply, and therefore oxygen supply, to the cardiac muscle cells is reduced or cut off, the cells die and the patient suffers what is often referred to as a heart attack. If the attack is not fatal the heart may be weakened. The dead muscle cells are not replaced by new muscle cells and connective tissue forms a scar. The normal pattern of heart muscle contraction may be compromised as a result.
Blood vessels
Blood is pumped away from the heart into arteries which branch and distribute blood, under relatively high pressure, to all regions of the body. Arterial blood passes into smaller arteries (arterioles) and then into very small vessels (capillaries) which have very thin walls (one cell thick). Capillaries are described as exchange vessels because molecules, including carbon dioxide and oxygen, move into and out of capillaries across concentration gradients. In addition, some of the components of plasma leave capillaries and form extracellular (tissue) fluid. Some excess tissue fluid returns to small veins (venules) whereas other fluid drains to lymph capillaries (see below). The rate at which extracellular fluid is formed from plasma normally equals the rate at which fluid drains back into blood and lymph vessels. Blood in capillaries, under relatively low pressure, passes into venules which join and form veins. In turn, veins join together and return blood to the heart. In several regions of the body, some arterial blood bypasses capillaries and passes into venules in what are described as arteriovenous shunts. In the skin, such a route reduces heat loss and thus aids thermoregulation.
The walls of arteries and veins are similar in that they are made up of three layers but the layers vary in structure according to the function of the vessels. In some veins the boundary between the layers is not clearly defined. The layers are:
■ Tunica intima. This is the very thin inner layer which lines all arteries and veins and which is composed of endothelium (i.e. a simple squamous epithelium) and its basement membrane and a small amount of underlying loose connective tissue. In many vessels the endothelial cells are attached firmly to each other by tight junctions (Chapter 2).
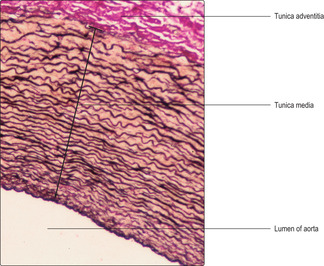
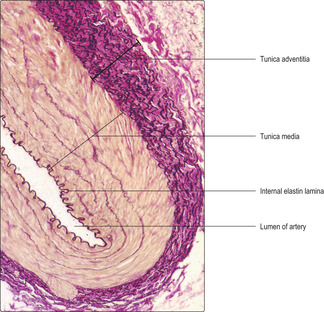
■ Tunica media. This is the middle layer and it forms the largest proportion of the wall of many arteries and veins. Smooth muscle cells and the connective tissue fibre elastin may be predominant in this layer. In general, arteries closest to the heart have most elastin in this layer and some vessels have numerous sheets (laminae) of elastin (Figs 10.4 and 10.5). Arteries further from the heart have more smooth muscle than elastin in this layer (Fig. 10.6). Some veins have smooth muscle in the tunica media, but generally they have fewer smooth muscle cells in their walls than arteries.
■ Tunica adventitia. This is the outer layer, surrounding the tunica media, and it is usually composed of collagenous connective tissue (Fig. 10.5). It is an indistinct layer and it merges with adjacent connective tissue fascia (the packing tissue of the body) and thus holds vessels in place. In some vessels elastin fibres are present in this layer (Fig. 10.6). Blood vessels (and nerves supplying smooth muscle cells in the tunica media) pass though the tunica adventitia.
In addition to the three tunicae, an internal elastin lamina may be present between the tunica intima and tunica media (Fig. 10.6) and an external elastin lamina between the tunica media and the tunica adventitia.
Arteries
Arteries may be classed as conducting or distributing arteries or as arterioles.
■ Conducting arteries are the largest arteries, closest to the heart and they contain a high proportion of elastin in their walls with few smooth muscle cells. They include the aorta (Fig. 10.5), which receives blood from the left ventricle of the heart. The elastin is arranged as multiple sheets around the vessels which allow conducting arteries to distend each time the heart contracts and propels blood into them. Importantly, between each heart beat the elastin recoils and this returns the vessels to normal dimensions and helps propel the blood along the arteries and thus maintain blood flow and pressure.
■ Distributing arteries have a high proportion of smooth muscle cells in their walls and this is related to their ability to maintain muscle tone (a state of prolonged, partial contraction) and thus arterial blood pressure, particularly in the periphery of the body. The internal elastin lamina in distributing arteries (Fig. 10.6) is pronounced in contrast to that in conducting arteries. Distributing arteries include the arteries of the limbs.
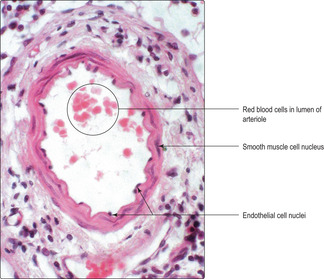
■ Arterioles are much smaller in diameter than arteries though they share a pattern of layers in their walls similar to that of distributing arteries. However, they have only one to three layers of smooth muscle in their tunica media. The smooth muscle cells are arranged concentrically in the walls of arterioles (Figs 10.7 and 10.8) and so their contraction and relaxation alters the diameter of their lumina. (This contraction does not pump blood along the vessels; instead, it varies the amount of muscle tone and thus provides varying resistance to the flow of blood.) In general, the sympathetic part of the autonomic nervous system controls the amount of tone (contraction) of the smooth muscle in the walls of arterioles and thus the rate of blood flow to capillaries.
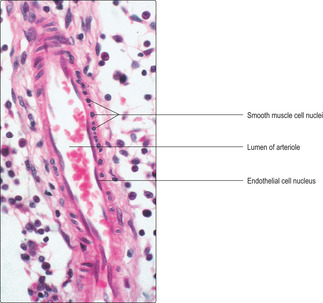 |
| Fig. 10.8
Arteriole sectioned (partly) along its length. Some nuclei of the smooth muscle cells in the wall of this arteriole appear circular. These smooth muscle cells are fusiform in shape and encircle the arteriole but have been sectioned across their length and through the region of the nucleus. Contrast this appearance with the nuclei of smooth muscle cells in Fig. 10.7. Similarly, contrast the fusiform shape of the endothelial cell nuclei lining this arteriole with those in Fig. 10.7. High magnification.
|
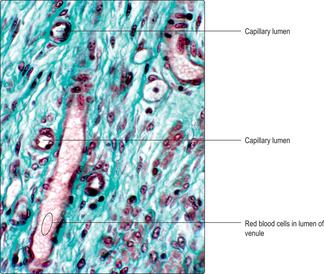
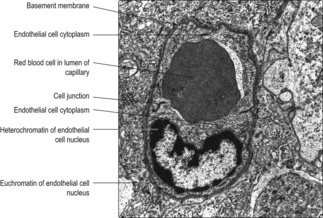
Capillaries
Most capillaries are 4–10μm in diameter and most are also short in length. They are perfused by blood from arterioles. Networks of branching and connecting (anastomosing) capillaries are present in many regions of the body and are referred to as capillary beds. Capillary walls (Figs 10.9 and 10.10) are formed by a single layer of squamous epithelial cells known as endothelial cells, and their basement membrane (Fig. 10.10). The endothelial cells form the narrow tubes of the capillaries through which blood cells and plasma flow. Around the periphery of some capillaries are pericytes, which have long cytoplasmic processes that wrap around the walls of capillaries. Pericytes contain contractile proteins and thus are able to contract and modify the flow of blood through capillaries. After injury, pericytes are able to differentiate and form new blood vessels and supporting connective tissue.
Although capillaries are very small, they are vital in the functioning of the cardiovascular system as they are the site where exchange of gases, nutrients and waste molecules takes place. They are also important sites where some of the components of blood plasma and white blood cells pass between capillaries and surrounding tissues. Capillaries may be categorised into three groups: continuous, fenestrated or sinusoidal. These groups have significant morphological and functional differences and are present in different locations.
■ Continuous capillaries. These are located in brain, spinal cord, peripheral nervous tissue, muscle and connective tissues (Fig. 10.9). The endothelial cells lining these capillaries are tightly joined together. Gases diffuse through the endothelial cells and pinocytosis and exocytosis occur in many regions, passing fluid and molecules through the cells.
■ Fenestrated capillaries. The endothelial cells in these capillaries are tightly joined together but they exhibit tiny pores. These pores are closed by diaphragms formed of cell membranes. This type of capillary is present in endocrine glands and the gastrointestinal tract and allows some large molecules, e.g. hormones, to pass readily across the capillary walls.
■ Sinusoidal capillaries. Sinusoidal capillaries differ from other capillaries in that the endothelial cells do not form a continuous layer of tightly attached cells; their basement membrane is also discontinuous. They have fenestrae (openings) in the cytoplasm of endothelial cells and these do not have diaphragms across them. Sinusoids are generally wider in diameter than capillaries and their shape contours around adjacent parenchymal cells. In the walls of some sinusoids, e.g. in the spleen and liver, fixed macrophages are present. The structure of the walls of sinusoids, in comparison with the walls of other capillaries, facilitates greater opportunities for exchange activities, particularly those involving cells of the immune system.
Veins
Veins are low-pressure blood vessels compared with arteries, and they return blood to the heart. In general, compared with arteries, there is much less smooth muscle and elastin and more collagen in the walls of veins, which accords with the lower pressure within them. Furthermore, the ratio of luminal diameter to wall thickness is greater in veins than in arteries if the comparison is made between vessels adjacent to each other in the body (Fig. 10.11).
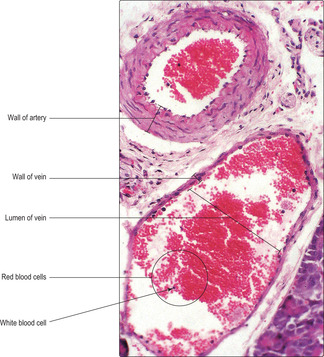 |
| Fig. 10.11
Artery and vein. The wall of this artery contains numerous smooth muscle cells which have been fixed in the contracted state (Chapter 5) and the nuclei of the endothelial cells appear as dark dots projecting into the lumen. Low magnification.
|
Veins may be grouped into three categories according to their size: small, medium and large. The smallest veins, venules, drain capillaries. In medium-sized veins valves are present that prevent the back flow of blood. Valves are flap-like structures which have an endothelial covering and a fibrous core of connective tissue. The flaps project towards the heart; thus, if blood flow to the heart stops, the blood cannot pass backwards because the valve flaps are forced together and close the lumen. Valves are particularly important where there is a need to counteract the force of gravity such as in the limbs. Interestingly, the superficial veins in the lower limbs in humans have a well-developed component of smooth muscle in their walls which, by maintaining muscle tone, is thought to assist in preventing excess distension of the veins due to gravitational forces. The largest veins, close to the heart, do not have valves aiding unidirectional flow. Venous return from large veins below the heart is aided by pressure changes that occur in the thorax during inspiration and gravity aids venous return from the vessels above the heart.
Lymphatic vessels
The lymphatic vessels are an important component of the circulatory system returning some excess extracellular fluid and white blood cells to veins. The smallest lymphatic vessels are lymphatic capillaries. These begin as very small blind-ended tubes formed by endothelial cells. The extracellular (tissue) fluid which drains into lymphatic capillaries is known as lymph. Lymph capillaries resemble blood capillaries but they are characterised by the presence of non-return valves. The pressure in lymphatic vessels is very low and the valves help prevent back flow of lymph. Lymph is carried in lymph vessels to and from lymph nodes (Chapter 8). As lymph passes through lymph nodes immune responses to foreign molecules occur and immune cells such as lymphocytes may be added to the draining lymph (Chapter 8). Lymph draining particular organs and regions of the body passes through specific lymph nodes before draining into wider lymph vessels (lymph ducts). Eventually, the lymph ducts join veins in the neck region and thus lymph is returned to the cardiovascular system.
Deep vein thrombosis Deep veins accompany the deeply placed arteries in the limbs. These veins are of relatively small calibre and normally venous return is aided by valves. Maintaining tone in the smooth muscle in the walls of these veins helps prevent the veins from distending. In addition, contraction of skeletal muscles in the limb compresses these veins and helps propel the blood towards the heart (as long as the valves are effective). During lengthy periods of inactivity, sufficient venous blood may not be propelled away from the lower limb veins. The blood may become stagnant and clot (i.e. form a thrombus), blocking the deep veins. This causes the limb to swell and become red and painful. The particular danger is that the clot or part of it may detach and pass, via the heart, to the lung, where it may lodge in small blood vessels. This is termed a pulmonary embolism and it can be fatal.
Oedema This is the accumulation of tissue fluid in body tissues which would normally have re-entered venules and lymphatic vessels. It causes swelling of the affected region. It may be part of a local inflammatory reaction or if, for example, it is present in both lower limbs it may be due to increased venous pressure as a result of weak contractions of the right chambers of the heart (right heart failure).
The circulatory system
■ Consists of the heart and the vessels which carry blood or lymph.
The heart
■ The heart has paired atria and paired ventricles separated by valves which prevent back flow of blood.
■ It has a connective tissue skeleton.
■ It is supplied by autonomic nerves which modify the rate at which it eats.
■ The myocardium, the middle (thickest) layer, is formed mostly by cardiac muscle cells. Specialised cells (e.g. Purkinje cells) are involved in organising muscle contraction.
■ The endocardium, the inner layer, is lined by endothelial cells.
■ The epicardium, the outer layer, supports blood vessels supplying the heart, may accumulate fat and is part of the pericardium.
Blood vessels
■ These vary in structure and function.
■ Arteries (and arterioles) carry blood at relatively high pressure from the eart to capillaries.
■ Veins (and venules) carry blood at low pressure from capillaries to the heart. Some veins and venules have valves which aid return of blood to the heart.
■ Capillaries have only endothelial cells in their walls and gases, molecules, white blood cells and fluid move across their walls.
■ Larger blood vessels have three layers in their walls:
■ tunica intima, the inner layer comprising endothelium and connective tissue
■ tunica media, the middle layer comprising varying amounts of elastin, smooth muscle and collagen
■ tunica adventitia, the outer layer of connective tissue binding vessels to adjacent structures.
■ Contraction of smooth muscle in vessel walls is controlled (largely) by sympathetic nerves.
Extracellular (tissue) fluid
■ This is formed from plasma.
■ Some returns to venules and some to lymphatic capillaries which eventually drain into veins.