CHAPTER 14 The Central Septum in Breast Reduction and Mastopexy
Key Points
Introduction
For a long time we have been used to seeing the breast as a homogeneous organ with unpredictable location of the neurovascular structures. In the course of numerous clinical breast reductions, nourished by the inferior pedicle1 I always came across a distinct layer of vascular networks. It emerged from the thoracic wall along the level of the fourth intercostal space and passed through the whole breast within the inferior pedicle to supply the nipple. The vascular layer was caudally attached to a horizontal septum of dense connective tissue.
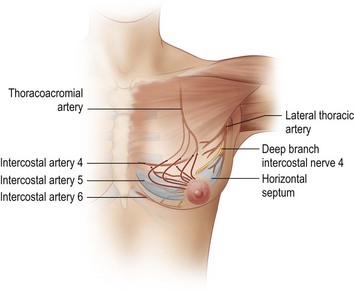
Anatomical investigations showed that this septum is part of a suspension apparatus, which is attached to the thoracic wall, mainly following the borders of pectoralis major.2–4 This ligamentous suspension carries the whole weight of the breast like a sling. The horizontal septum takes its origin from the periosteum of the fifth rib and merges medially into a vertical medial ligament, which attaches to the sternum. Laterally, the septum merges into a lateral vertical ligament, which originates from the pectoral fascia at the lateral edge of pectoralis minor (Fig. 14.1). These vertical ligaments continue into the capsule of the breast in an anterior direction (Fig. 14.1). A ligamentous structure also arises from the origin of this deep part of the ligamentous suspension, which inserts into the overlying skin, thereby determining the shape of the breast. This structure can be seen as a densification of Cooper’s ligaments and builds the intermammary sulcus and the cleavage medially as well as the inframammary fold inferiorly. Laterally, it forms a strong ligament heading into the skin of the axilla, the suspensory ligament of the axilla, which shapes the axillary hollow.
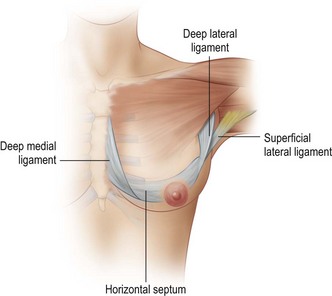
Fig. 14.1 Diagram of left breast, anteromedial view.
Redrawn from Würinger E, Mader N, Posch E, Holle J. Nerve and vessel supplying ligamentous suspension of the mammary gland. Plast Reconstr Surg 1998;101:1486–500.
Most importantly, the deep branch of the lateral cutaneous branch of the fourth or fifth intercostal nerve (also the main nerve to the nipple), attaches to the caudal vascular layer (Fig. 14.2).
The second main path comprises perforating branches from anastomoses of the internal thoracic artery and the anterior cutaneous branches of the second to fourth intercostal nerves along the medial ligament as well as branches of the lateral thoracic artery and the corresponding lateral cutaneous nerve branches along the lateral ligament (Fig. 14.3).
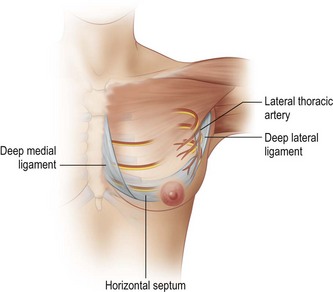
Fig. 14.3 Diagram of left breast, anteromedial view, neurovascular supply guided by vertical ligaments.
Redrawn from Würinger E, Mader N, Posch E, Holle J. Nerve and vessel supplying ligamentous suspension of the mammary gland. Plast Reconstr Surg 1998;101:1486–500.
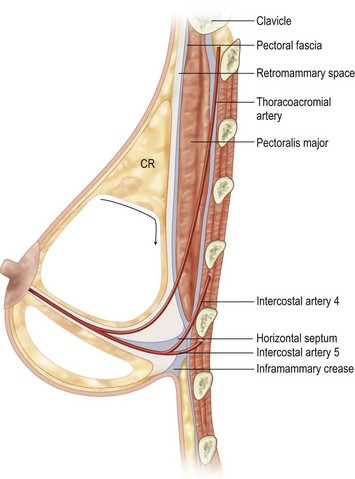
The ligamentous suspension can be developed easily by blunt dissection along the retromammary space in a caudal direction. At the level of the fourth intercostal space the retromammary space changes its direction to continue as a horizontal plane of loose areolar tissue heading toward the nipple. This areolar tissue provides a pre-existing bipartition of the breast, as it divides the breast and its system of milk ducts into a cranial and a caudal glandular layer. Below this areolar tissue is the horizontal septum (Fig. 14.4).
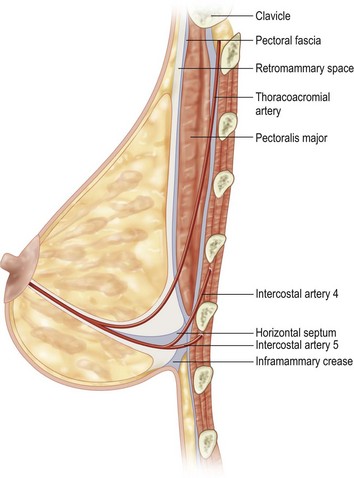
Fig. 14.4 Vertical sectional view.
The horizontal septum can be found by opening up the retromammary space in a caudal direction.
Redrawn from Würinger E, Mader N, Posch E, Holle J. Nerve and vessel supplying ligamentous suspension of the mammary gland. Plast Reconstr Surg 1998;101:1486–500.
The ability to localize the course of the neurovascular supply of the breast is important for any surgical treatment of this organ; it has allowed maintenance of the neurovascular supply in breast reduction procedures to be more precise.5–7
The nipple can be supplied by the vessels running along either of the vertical ligaments, merging into the subdermal plexus along the capsule of the breast, which affords a dermal pedicle to elevate the nipple. These pedicles can be cranial, medial, or lateral pedicles.8–10
The second big group of pedicles derives its neurovascular supply via the horizontal septum by a central parenchymal pedicle. These are the central and inferior pedicle techniques such as the techniques of Georgiade,1 Levet,11 Hester,12 or McKissock.13 Combining those two main neurovascular sources is possible.
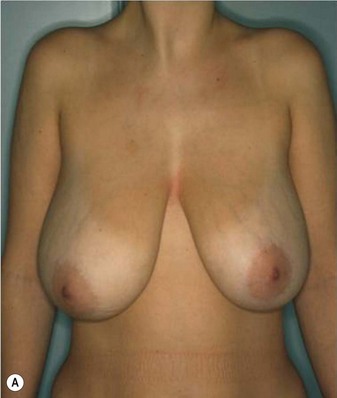
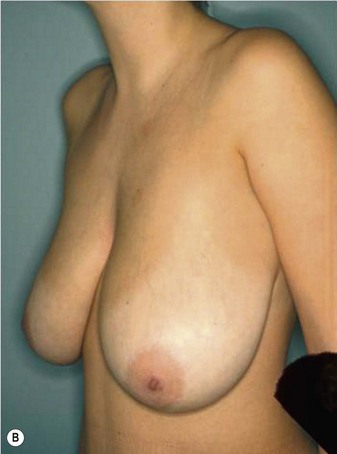
Patient Selection
The technique could be offered to patients with large and ptotic breasts, to elderly patients, to smokers and obese patients, to pre-irradiated breasts, and to patients with weak connective tissue. Because of its safe neurovascular supply it can be applied to all these difficult cases. In secondary reduction the technique can be applied, when the horizontal septum was maintained previously.6
Operative Technique (Box 14.1)
Markings
After sterile draping in a semi-upright position the preoperative marking is drawn freehand (Fig. 14.5). As the resection of the gland is handled independent of the resection of the skin envelope, most patterns of scar reducing resections can be applied. The midsternal line, the inframammary fold, the suprasternal notch and the xiphoid are marked as fixed reference points.
Box 14.1 Summary of operative technique
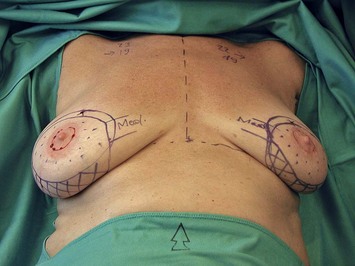
Fig. 14.5 Marking of the medial pedicle (stippled) with narrow dermal bridge.
The residual skin excess (hatched) will be excised.
From Würinger E, Vertical scar mammaplasty with the inferocentral pedicle. In: Hamdi M, Hammond DC, Nahai F, editors. Vertical scar mammaplasty, Springer; 2005. With kind permission from Springer Science + Business Media.
These vertical lines are joined cranially just below the marking of the new nipple position. Caudally they are joined about 4–5 cm (in bigger breasts 6–8 cm) above the submammary fold. The bigger the breast, the more the submammary fold will be elevated. The lines finally build a periareolar circle or oval shape (Fig. 14.5).
Resection
Whereas the determination of skin excess and the marking is performed similar to most vertical scar patterns, the resection differs distinctly and I think that this is the main point in my technique. Knowing the location of the main neurovascular supply within a clearly defined, regular structure makes it easier to predict which areas can be safely resected. The easy clinical accessibility of the horizontal septum allows for maintenance of optimal supply for the nipple.2,3
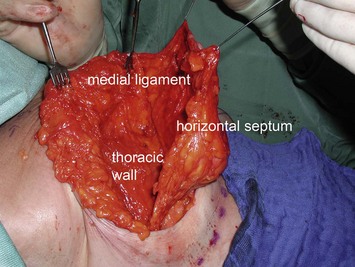
The level of resection is found bluntly taking advantage of the pre-existing bipartition of the gland (Fig. 14.6). The retromammary space is reached by a horizontal incision through the gland at the cranial border of the pedicle, approximately at the level of the third rib. The part of the breast cranial of this horizontal incision is left intact, thereby maintaining superior fullness (Fig. 14.7). The part of the breast caudal to the incision is peeled off bluntly following the retromammary space down to the level of the fourth intercostal space. Here the retromammary space merges into areolar tissue, which can be progressively opened up with the fingers in an anterior direction to the nipple (Fig. 14.8). The horizontal septum is situated caudal to this areolar tissue. With blunt dissection the medial and lateral vertical ligaments are encountered. This tissue between the horizontal incision through the breast and the horizontal septum corresponds to the cranial glandular layer; it is resected and builds the main part of the resection. The amount of resected tissue varies as the thickness of the cranial layer varies with different breast sizes. In small breasts the cranial glandular layer amounts to less than 2 cm, in large breasts it can be more than 6 cm thick, whereas the caudal glandular layer usually has a thickness of about 2 cm in all breast sizes.
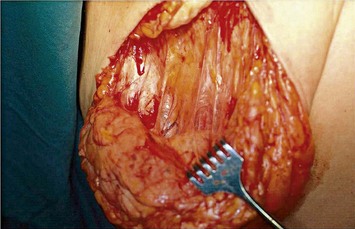
Fig. 14.7 The retromammary space is reached via a horizontal cut through the gland.
Redrawn from Würinger E. Refinement of the central pedicle breast reduction by application of the ligamentous suspension. Plast Reconstr Surg 1999;103:1400–10.
The horizontal septum can thus be used as a guide to achieve symmetry and this can also be done in preoperatively asymmetric breasts. The cranial glandular layer, which comprises the difference in volume, is mostly removed in this technique. This allows removing the very region where the actual hypertrophy and the accumulation of fat seems to take place. The thickness of the pedicle, comprising the caudal glandular layer, will be more or less equal on both sides.5
According to the desired size of the breast, at least the medial two-thirds of the horizontal septum and the medial ligament are maintained. Resection usually affects the lateral ligament including the tail of Spence and the lateral third of the horizontal septum, which allows for resection of lateral fullness. The deep branch of the lateral cutaneous branch of the fourth intercostal nerve can thereby be preserved, which runs within the retromammary space from lateral to medial and changes its direction after 3 to 5 cm to rise toward the nipple along the level of the fibrous septum.2 The pedicle consists finally of the horizontal fibrous septum and its attached neurovascular layers, of both the caudal glandular layer and of the medial ligament (Fig. 14.9).
Shaping
After resection of the cranial glandular layer, the pedicle mainly consists of parts of the ligamentous suspension. Its fibrous elements provide sturdy structures, which are more suitable for shaping than the residual breast tissue, where sutures cut through easily. The new breast shape is mainly gained by upward rotation of the pedicle similar to the technique described by Hall-Findlay.14 This allows combining the advantage of a technique that keeps the upper parts of the breast intact, and that acts against the force of gravity, with the advantage of keeping the horizontal septum intact, which means an optimized neurovascular supply. Upward rotation of the pedicle reduces the diameter of the base of the breast and increases projection of the nipple. The pedicle can be held in an elevated position with some fixation sutures. Also the periareolar dermis can be used for shaping to accentuate projection of the nipple. Usually no fixation sutures are necessary.
Postoperative Care
The patient stays at the hospital overnight. The drains and the bandage are removed the next day. Then a sports bra is worn day and night, and then after 2 weeks only during the day. The patient is allowed to move her arms freely. Non-resorbable stitches are removed after 2 weeks; the scars are then treated with ointment, with massage of the scar starting 2 weeks later. Examples of two patients are shown preoperatively and with their postoperative result in Figs 14.10 and 14.11.
1 Georgiade NG, Serafin D, Riefkohl R, Georgiade GS. Is there a reduction mammaplasty for ‘all seasons’? Plast Reconstr Surg. 1979;63:765-773.
2 Würinger E, Mader N, Posch E, Holle J. Nerve and vessel supplying ligamentous suspension of the mammary gland. Plast Reconstr Surg. 1998;101:1486-1500.
3 Würinger E, Tschabitscher M. New aspects of the topography of the mammary gland regarding its neurovascular supply along a regular ligamentous suspension. Eur J Morphol. 2003;40(3):181-189.
4 Würinger E. Vertical scar mammaplasty with the inferocentral pedicle. In: Hamdi M, Hammond DC, Nahai F, editors. Vertical scar mammaplasty. Berlin: Springer, 2005.
5 Würinger E. Refinement of the central pedicle breast reduction by application of the ligamentous suspension. Plast Reconstr Surg. 1999;103:1400-1410.
6 Würinger E. Secondary reduction mammaplasty. Plast Reconstr Surg. 2002;109:812-814.
7 van Deventer PV, Page BJ, Graewe FR. The safety of pedicles in breast reduction and mastopexy procedures. Aesth Plast Surg. 2008;32:307-312.
8 Strömbeck JO. Mammaplasty: Reports on a new technique based on the two pedicle procedure. Br J Plast Surg. 1961;13:79.
9 Pitanguy I. Surgical treatment of breast hypertrophy. Br J Plast Surg. 1967;20:78.
10 Lejour M. Vertical mammaplasty and liposuction of the breast. Plast Reconstr Surg. 1994;94:100-114.
11 Levet Y. The pure posterior pedicle procedure for breast reduction. Plast Reconstr Surg. 1990;86:67.
12 Hester TR, Bostwick J, Miller L, Cunningham SJ. Breast reduction utilizing the maximally vascularized central breast pedicle. Plast Reconstr Surg. 1985;76:890.
13 McKissock PK. Reduction mammaplasty with a vertical dermal flap. Plast Reconstr Surg. 1972;49:245-252.
14 Hall-Findlay EJ. A simplified vertical reduction mammaplasty: shortening the learning curve. Plast Reconstr Surg. 1999;104:748-759.