Chapter 14 The breasts
History
The breast cancer genes BRCA1 and BRCA2 are associated with a strong risk of breast (and ovarian) cancer, as well as breast cancer in men. For all women from the age of 50 years, screening mammography1 is generally recommended.
Examination
When it is done properly, the examination takes some time to perform (about 3 minutes per breast).2 This must obviously be explained to the patient at the start. The patient should be offered a chaperone for the examination.
The examination is only just over 50% sensitive for carcinoma but specificity is as high as 90%. The likelihood ratio of a positive examination is 14.1 and the LR of a negative examination is 0.47.3
Inspection
Ask the patient to raise her arms above her head and then lower them slowly. Look for tethering of the nipples or skin, a shift in the relative position of the nipples or a fixed mass distorting the breast (Figure 14.1).
Note whether there are any obvious visible masses in the axillae.
Next ask her to rest her hands on her hips and then press her hands against her hips (the pectoral contraction manoeuvre). This accentuates areas of dimpling or fixation.
Palpation
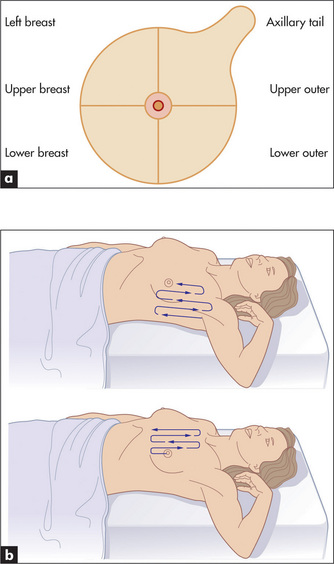
Palpation is performed gently with the pulps of the middle three fingers parallel to the contour of the breast. Feel the four quadrants of each breast systematically (Figure 14.2a). Don’t pinch the breast as you may think you then feel a mass. The total examination should involve a rectangular area bordered by the clavicle, sternum, mid-axillary line and the bra line. Start in the axilla and palpate in a line down to the bra line inferiorly. The pattern of palpation is like that of mowing a lawn, a series of vertical strips that cover the whole of the rectangle (Figure 14.2b).
Don’t mistake normal breast structures for a mass!4 You may feel a rib or costochondral junction normally on deep palpation. The inferior ridge of breast tissue (inframammary fold) may be felt and is symmetrical. You may feel normal rubbery-type plaques (fibroglandular tissue), especially in the upper outer quadrant. It is normal to feel firm breast tissue at the areola border.
Evaluation of a breast lump
The following five points need to be carefully elucidated if a lump is detected.
A palpable breast mass is likely to be significant (called a dominant mass) if it is:4
A palpable breast mass is more likely to be malignant if it has the following characteristics:4
Remember that many normal breasts have palpable lumps and that although benign lumps tend to be soft, moveable and regular, they can also have the characteristics of malignant lumps (Good signs guide 14.1). Causes of a lump in the breast are listed in Table 14.1.
| Non-tender | Tender |
| Cyst | Cyst |
| Carcinoma | Breast abscess |
| Fibroadenosis (chronic mastitis) | Fibroadenosis |
| Fibroadenoma (benign highly mobile ‘breast mouse’) | Costal cartilage chondritis |
| Uncommon causes | Inflammatory breast cancer |
| • Trauma, fat necrosis | |
| • Other cysts—e.g. galactocele | |
| • Other neoplasms—e.g. duct papilloma | |
| • Chest wall—e.g. lipoma, costal cartilage chondritis (causes tenderness but not a lump) (Tietze’s* disease) |
* Alexander Tietze (1864–1927), Chief Surgeon, Allerheiligen Hospital, Breslau, Poland. He described the condition in 1921.
In men with true gynaecomastia, a disc of breast tissue can be palpated under the areola. This is not present in men who are merely obese. Causes of breast enlargement in men are presented on page 316.
GOOD SIGNS GUIDE 14.1 Breast lump characteristics and likelihood of cancer in a woman of average risk3
| Sign | Positive LR |
| Mass | 2.1 |
| Fixed | 2.4 |
| Hard | 1.6 |
| Irregular | 1.8 |
| >2 cm diameter | 1.9 |
From McGee S, Evidence-based physical diagnosis, 2nd edn. St Louis: Saunders, 2007.
1. Kerlikowske K, Smith-Bindman R, Ljung BM, et al. Evaluation of abnormal mammography results and palpable breast abnormalities. Ann Intern Med. 2003;139:274-284.
2. Fenton JJ, Rolnick SJ, Harris EL, Barton MB, Barlow WE, Reisch LM, Herrinton LJ, Geiger AM, Fletcher SW, Elmore JG. Specificity of clinical breast examination in community practice. J Gen Intern Med. 22(3), 2007. Mar 332–327
3. Barton MB, Harris R, Fletcher SW. Does this patient have breast cancer? JAMA. 1999;282:1270-1280. The clinical breast examination may have an overall specificity which is high (94%) but the sensitivity is poor (54%). Unfortunately interobserver variation seems to be high
4. Pruthi S. Detection and evaluation of a palpable breast mass. Mayo Clin Proc. 2001;76:641-647.