The Body
What is anatomy?
How can gross anatomy be studied?
Anatomy can be studied following either a regional or a systemic approach.
 With a regional approach, each region of the body is studied separately and all aspects of that region are studied at the same time. For example, if the thorax is to be studied, all of its structures are examined. This includes the vasculature, the nerves, the bones, the muscles, and all other structures and organs located in the region of the body defined as the thorax. After studying this region, the other regions of the body (i.e., the abdomen, pelvis, lower limb, upper limb, back, head, and neck) are studied in a similar fashion.
With a regional approach, each region of the body is studied separately and all aspects of that region are studied at the same time. For example, if the thorax is to be studied, all of its structures are examined. This includes the vasculature, the nerves, the bones, the muscles, and all other structures and organs located in the region of the body defined as the thorax. After studying this region, the other regions of the body (i.e., the abdomen, pelvis, lower limb, upper limb, back, head, and neck) are studied in a similar fashion.
 In contrast, in a systemic approach, each system of the body is studied and followed throughout the entire body. For example, a study of the cardiovascular system looks at the heart and all of the blood vessels in the body. When this is completed, the nervous system (brain, spinal cord, and all the nerves) might be examined in detail. This approach continues for the whole body until every system, including the nervous, skeletal, muscular, gastrointestinal, respiratory, lymphatic, and reproductive systems, has been studied.
In contrast, in a systemic approach, each system of the body is studied and followed throughout the entire body. For example, a study of the cardiovascular system looks at the heart and all of the blood vessels in the body. When this is completed, the nervous system (brain, spinal cord, and all the nerves) might be examined in detail. This approach continues for the whole body until every system, including the nervous, skeletal, muscular, gastrointestinal, respiratory, lymphatic, and reproductive systems, has been studied.
Important anatomical terms
The anatomical position
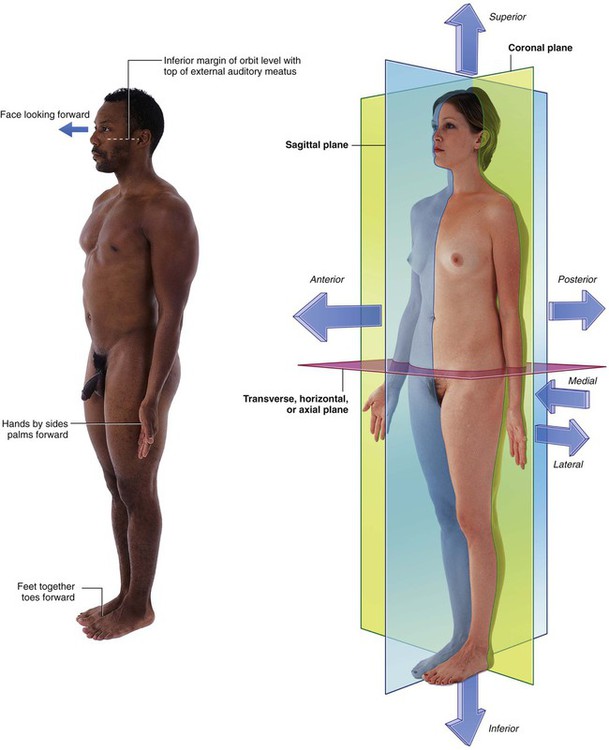
The anatomical position is the standard reference position of the body used to describe the location of structures (Fig. 1.1). The body is in the anatomical position when standing upright with feet together, hands by the side and face looking forward. The mouth is closed and the facial expression is neutral. The rim of bone under the eyes is in the same horizontal plane as the top of the opening to the ear, and the eyes are open and focused on something in the distance. The palms of the hands face forward with the fingers straight and together and with the pad of the thumb turned 90° to the pads of the fingers. The toes point forward.
Anatomical planes
Three major groups of planes pass through the body in the anatomical position (Fig. 1.1).
 Coronal planes are oriented vertically and divide the body into anterior and posterior parts.
Coronal planes are oriented vertically and divide the body into anterior and posterior parts.
 Sagittal planes also are oriented vertically but are at right angles to the coronal planes and divide the body into right and left parts. The plane that passes through the center of the body dividing it into equal right and left halves is termed the median sagittal plane.
Sagittal planes also are oriented vertically but are at right angles to the coronal planes and divide the body into right and left parts. The plane that passes through the center of the body dividing it into equal right and left halves is termed the median sagittal plane.
 Transverse, horizontal, or axial planes divide the body into superior and inferior parts.
Transverse, horizontal, or axial planes divide the body into superior and inferior parts.
Terms to describe location
Anterior (ventral) and posterior (dorsal), medial and lateral, superior and inferior
Three major pairs of terms are used to describe the location of structures relative to the body as a whole or to other structures (Fig. 1.1).
 Anterior (or ventral) and posterior (or dorsal) describe the position of structures relative to the “front” and “back” of the body. For example, the nose is an anterior (ventral) structure, whereas the vertebral column is a posterior (dorsal) structure. Also, the nose is anterior to the ears and the vertebral column is posterior to the sternum.
Anterior (or ventral) and posterior (or dorsal) describe the position of structures relative to the “front” and “back” of the body. For example, the nose is an anterior (ventral) structure, whereas the vertebral column is a posterior (dorsal) structure. Also, the nose is anterior to the ears and the vertebral column is posterior to the sternum.
 Medial and lateral describe the position of structures relative to the median sagittal plane and the sides of the body. For example, the thumb is lateral to the little finger. The nose is in the median sagittal plane and is medial to the eyes, which are in turn medial to the external ears.
Medial and lateral describe the position of structures relative to the median sagittal plane and the sides of the body. For example, the thumb is lateral to the little finger. The nose is in the median sagittal plane and is medial to the eyes, which are in turn medial to the external ears.
 Superior and inferior describe structures in reference to the vertical axis of the body. For example, the head is superior to the shoulders and the knee joint is inferior to the hip joint.
Superior and inferior describe structures in reference to the vertical axis of the body. For example, the head is superior to the shoulders and the knee joint is inferior to the hip joint.
Proximal and distal, cranial and caudal, and rostral
Other terms used to describe positions include proximal and distal, cranial and caudal, and rostral.
 Proximal and distal are used with reference to being closer to or farther from a structure’s origin, particularly in the limbs. For example, the hand is distal to the elbow joint. The glenohumeral joint is proximal to the elbow joint. These terms are also used to describe the relative positions of branches along the course of linear structures, such as airways, vessels, and nerves. For example, distal branches occur farther away toward the ends of the system, whereas proximal branches occur closer to and toward the origin of the system.
Proximal and distal are used with reference to being closer to or farther from a structure’s origin, particularly in the limbs. For example, the hand is distal to the elbow joint. The glenohumeral joint is proximal to the elbow joint. These terms are also used to describe the relative positions of branches along the course of linear structures, such as airways, vessels, and nerves. For example, distal branches occur farther away toward the ends of the system, whereas proximal branches occur closer to and toward the origin of the system.
 Cranial (toward the head) and caudal (toward the tail) are sometimes used instead of superior and inferior, respectively.
Cranial (toward the head) and caudal (toward the tail) are sometimes used instead of superior and inferior, respectively.
 Rostral is used, particularly in the head, to describe the position of a structure with reference to the nose. For example, the forebrain is rostral to the hindbrain.
Rostral is used, particularly in the head, to describe the position of a structure with reference to the nose. For example, the forebrain is rostral to the hindbrain.
Imaging
Diagnostic imaging techniques
Plain radiography
The basic physics of X-ray generation has not changed.
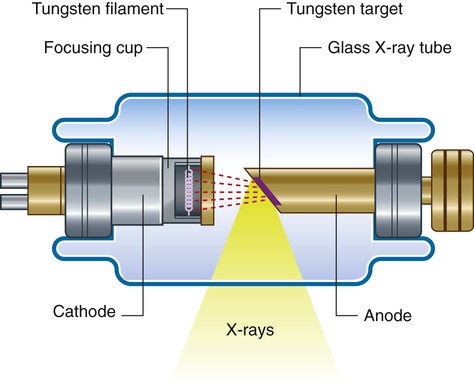
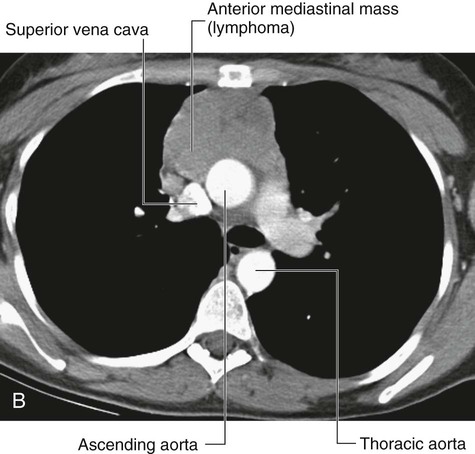
X-rays are photons (a type of electromagnetic radiation) and are generated from a complex X-ray tube, which is a type of cathode ray tube (Fig. 1.2). The X-rays are then collimated (i.e., directed through lead-lined shutters to stop them from fanning out) to the appropriate area, as determined by the radiographic technician. As the X-rays pass through the body they are attenuated (reduced in energy) by the tissues. Those X-rays that pass through the tissues interact with the photographic film.
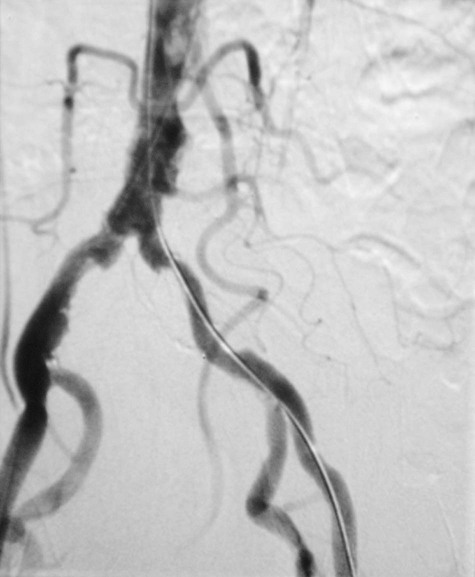
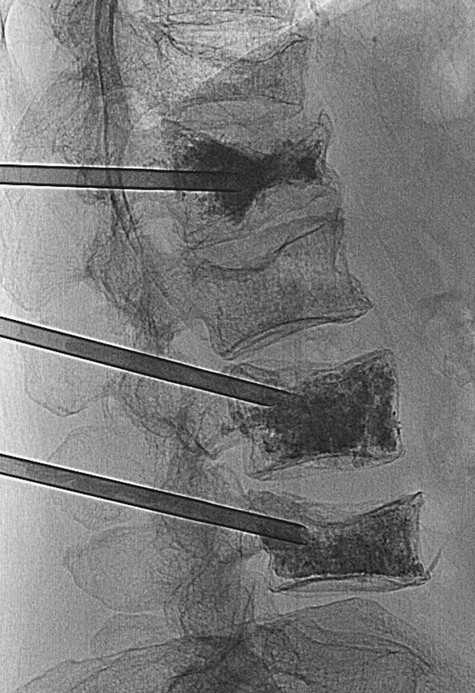
Modifications to this X-ray technique allow a continuous stream of X-rays to be produced from the X-ray tube and collected on an input screen to allow real-time visualization of moving anatomical structures, barium studies, angiography, and fluoroscopy (Fig. 1.3).
Contrast agents
To demonstrate specific structures, such as bowel loops or arteries, it may be necessary to fill these structures with a substance that attenuates X-rays more than bowel loops or arteries do normally. It is, however, extremely important that these substances are nontoxic. Barium sulfate, an insoluble salt, is a nontoxic, relatively high-density agent that is extremely useful in the examination of the gastrointestinal tract. When barium sulfate suspension is ingested it attenuates X-rays and can therefore be used to demonstrate the bowel lumen (Fig. 1.4). It is common to add air to the barium sulfate suspension, by either ingesting “fizzy” granules or directly instilling air into the body cavity, as in a barium enema. This is known as a double-contrast (air/barium) study.
Subtraction angiography
During angiography it is often difficult to appreciate the contrast agent in the vessels through the overlying bony structures. To circumvent this, the technique of subtraction angiography has been developed. Simply, one or two images are obtained before the injection of contrast media. These images are inverted (such that a negative is created from the positive image). After injection of the contrast media into the vessels, a further series of images are obtained, demonstrating the passage of the contrast through the arteries into the veins and around the circulation. By adding the “negative precontrast image” to the positive postcontrast images, the bones and soft tissues are subtracted to produce a solitary image of contrast only. Before the advent of digital imaging this was a challenge, but now the use of computers has made this technique relatively straightforward and instantaneous (Fig. 1.5).
Ultrasound
Ultrasonography of the body is widely used for all aspects of medicine.
Doppler ultrasound
Traditionally ultrasound is used for assessing the abdomen (Fig. 1.6) and the fetus in pregnant women. Ultrasound is also widely used to assess the eyes, neck, soft tissues, and peripheral musculoskeletal system. Probes have been placed on endoscopes, and endoluminal ultrasound of the esophagus, stomach, and duodenum is now routine. Endocavity ultrasound is carried out most commonly to assess the genital tract in women using a transvaginal or transrectal route. In men, transrectal ultrasound is the imaging method of choice to assess the prostate in those with suspected prostate hypertrophy or malignancy.
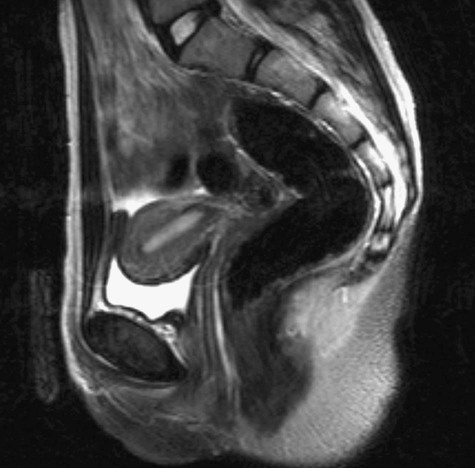
Magnetic resonance imaging
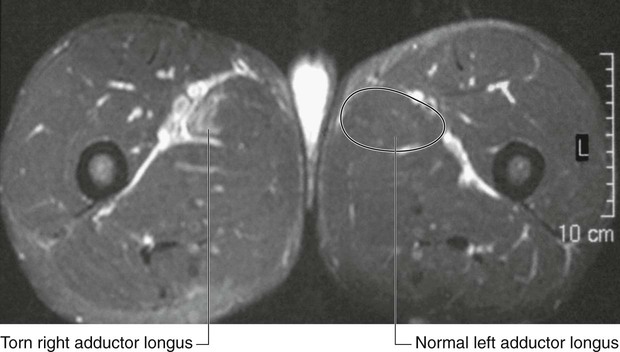
The process of magnetic resonance imaging (MRI) is dependent on the free protons in the hydrogen nuclei in molecules of water (H2O). Because water is present in almost all biological tissues, the hydrogen proton is ideal. The protons within a patient’s hydrogen nuclei can be regarded as small bar magnets, which are randomly oriented in space. The patient is placed in a strong magnetic field, which aligns the bar magnets. When a pulse of radio waves is passed through the patient the magnets are deflected, and as they return to their aligned position they emit small radio pulses. The strength and frequency of the emitted pulses and the time it takes for the protons to return to their pre-excited state produce a signal. These signals are analyzed by a powerful computer, and an image is created (Fig. 1.9).
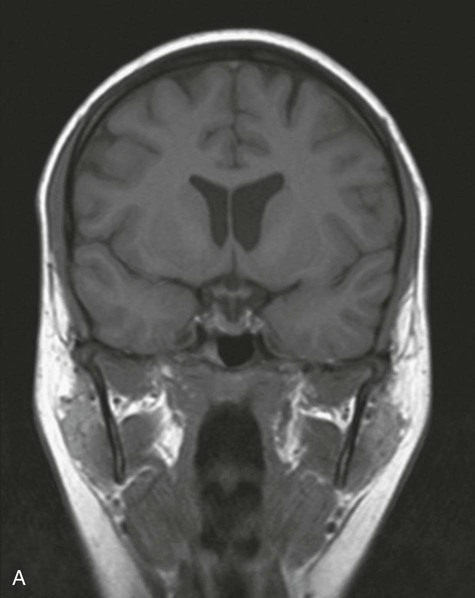
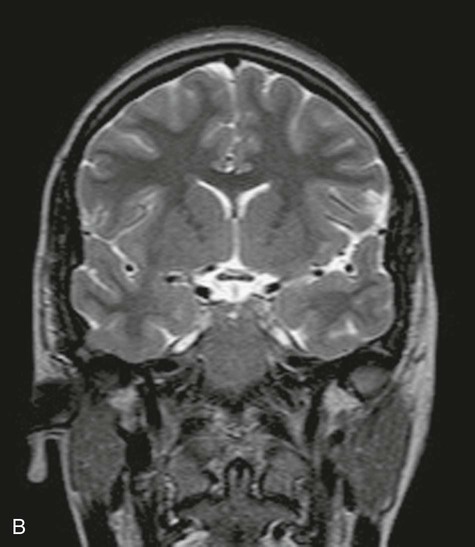
By altering the sequence of pulses to which the protons are subjected, different properties of the protons can be assessed. These properties are referred to as the “weighting” of the scan. By altering the pulse sequence and the scanning parameters, T1-weighted images (Fig. 1.10A) and T2-weighted images (Fig. 1.10B) can be obtained. These two types of imaging sequences provide differences in image contrast, which accentuate and optimize different tissue characteristics.
Nuclear medicine imaging
 a reasonable half-life (e.g., 6 to 24 hours),
a reasonable half-life (e.g., 6 to 24 hours),
 an easily measurable gamma ray, and
an easily measurable gamma ray, and
 energy deposition in as low a dose as possible in the patient’s tissues.
energy deposition in as low a dose as possible in the patient’s tissues.
Depending on how the radiopharmaceutical is absorbed, distributed, metabolized, and excreted by the body after injection, images are obtained using a gamma camera (Fig. 1.11).
Image interpretation
Plain radiography
Gastrointestinal contrast examinations
High-density contrast medium is ingested to opacify the esophagus, stomach, small bowel, and large bowel. As described previously (p. 6), the bowel is insufflated with air (or carbon dioxide) to provide a double-contrast study. In many countries, endoscopy has superseded upper gastrointestinal imaging, but the mainstay of imaging the large bowel is the double-contrast barium enema. Typically the patient needs to undergo bowel preparation, in which powerful cathartics are used to empty the bowel. At the time of the examination a small tube is placed into the rectum and a barium suspension is run into the large bowel. The patient undergoes a series of twists and turns so that the contrast passes through the entire large bowel. The contrast is emptied and air is passed through the same tube to insufflate the large bowel. A thin layer of barium coats the normal mucosa, allowing mucosal detail to be visualized (see Fig. 1.4).
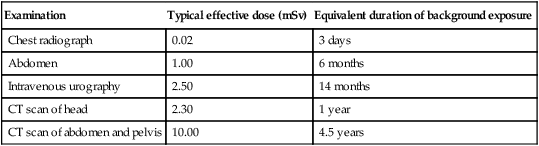
Safety in imaging
Whenever a patient undergoes an X-ray or nuclear medicine investigation, a dose of radiation is given (Table 1.1). As a general principle it is expected that the dose given is as low as reasonably possible for a diagnostic image to be obtained. Numerous laws govern the amount of radiation exposure that a patient can undergo for a variety of procedures, and these are monitored to prevent any excess or additional dosage. Whenever a radiograph is booked, the clinician ordering the procedure must appreciate its necessity and understand the dose given to the patient to ensure that the benefits significantly outweigh the risks.
Table 1.1
The approximate dosage of radiation exposure as an order of magnitude
| Examination | Typical effective dose (mSv) | Equivalent duration of background exposure |
| Chest radiograph | 0.02 | 3 days |
| Abdomen | 1.00 | 6 months |
| Intravenous urography | 2.50 | 14 months |
| CT scan of head | 2.30 | 1 year |
| CT scan of abdomen and pelvis | 10.00 | 4.5 years |
Body systems
Skeletal system
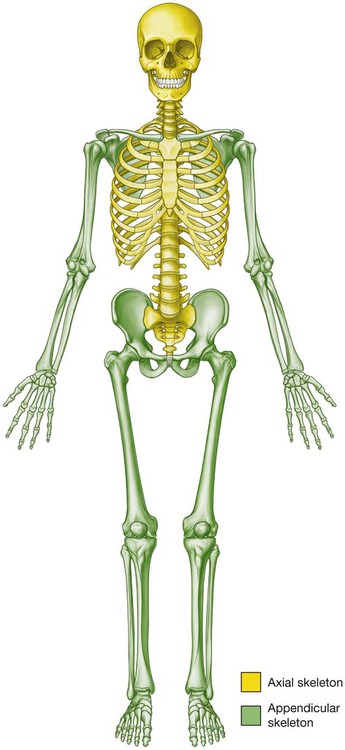
The skeleton can be divided into two subgroups, the axial skeleton and the appendicular skeleton. The axial skeleton consists of the bones of the skull (cranium), vertebral column, ribs, and sternum, whereas the appendicular skeleton consists of the bones of the upper and lower limbs (Fig. 1.12).
The skeletal system consists of cartilage and bone.
Cartilage
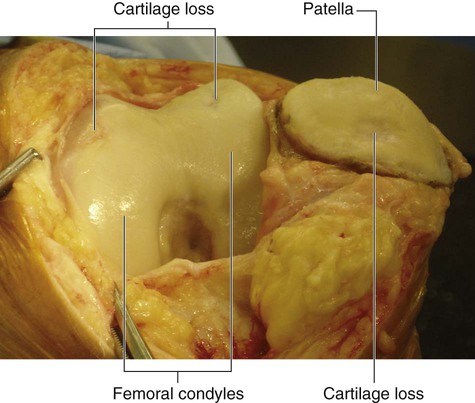
There are three types of cartilage:
 hyaline—most common; matrix contains a moderate amount of collagen fibers (e.g., articular surfaces of bones);
hyaline—most common; matrix contains a moderate amount of collagen fibers (e.g., articular surfaces of bones);
 elastic—matrix contains collagen fibers along with a large number of elastic fibers (e.g., external ear);
elastic—matrix contains collagen fibers along with a large number of elastic fibers (e.g., external ear);
 fibrocartilage—matrix contains a limited number of cells and ground substance amidst a substantial amount of collagen fibers (e.g., intervertebral discs).
fibrocartilage—matrix contains a limited number of cells and ground substance amidst a substantial amount of collagen fibers (e.g., intervertebral discs).
Cartilage is nourished by diffusion and has no blood vessels, lymphatics, or nerves.
Bone
 supportive structures for the body,
supportive structures for the body,
 reservoirs of calcium and phosphorus,
reservoirs of calcium and phosphorus,
 Long bones are tubular (e.g., humerus in upper limb; femur in lower limb).
Long bones are tubular (e.g., humerus in upper limb; femur in lower limb).
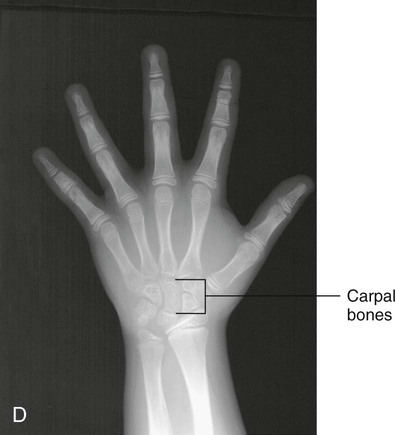
 Short bones are cuboidal (e.g., bones of the wrist and ankle).
Short bones are cuboidal (e.g., bones of the wrist and ankle).
 Flat bones consist of two compact bone plates separated by spongy bone (e.g., skull).
Flat bones consist of two compact bone plates separated by spongy bone (e.g., skull).
 Irregular bones are bones with various shapes (e.g., bones of the face).
Irregular bones are bones with various shapes (e.g., bones of the face).
 Sesamoid bones are round or oval bones that develop in tendons.
Sesamoid bones are round or oval bones that develop in tendons.
Joints
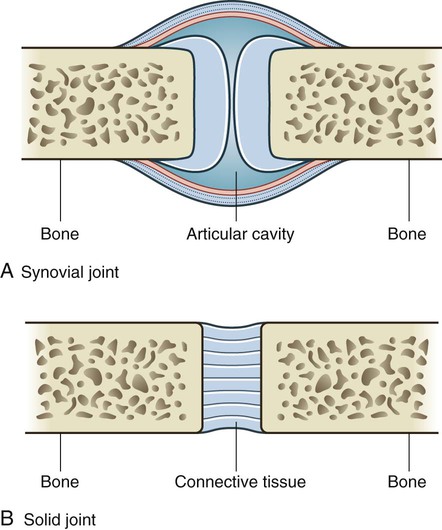
The sites where two skeletal elements come together are termed joints. The two general categories of joints (Fig. 1.19) are those in which:
 the skeletal elements are separated by a cavity (i.e., synovial joints), and
the skeletal elements are separated by a cavity (i.e., synovial joints), and
 there is no cavity and the components are held together by connective tissue (i.e., solid joints).
there is no cavity and the components are held together by connective tissue (i.e., solid joints).
Synovial joints
Synovial joints are connections between skeletal components where the elements involved are separated by a narrow articular cavity (Fig. 1.20). In addition to containing an articular cavity, these joints have a number of characteristic features.
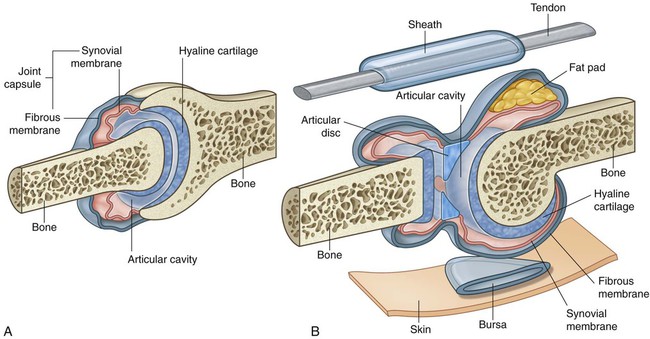
 The synovial membrane attaches to the margins of the joint surfaces at the interface between the cartilage and bone and encloses the articular cavity. The synovial membrane is highly vascular and produces synovial fluid, which percolates into the articular cavity and lubricates the articulating surfaces. Closed sacs of synovial membrane also occur outside joints, where they form synovial bursae or tendon sheaths. Bursae often intervene between structures, such as tendons and bone, tendons and joints, or skin and bone, and reduce the friction of one structure moving over the other. Tendon sheaths surround tendons and also reduce friction.
The synovial membrane attaches to the margins of the joint surfaces at the interface between the cartilage and bone and encloses the articular cavity. The synovial membrane is highly vascular and produces synovial fluid, which percolates into the articular cavity and lubricates the articulating surfaces. Closed sacs of synovial membrane also occur outside joints, where they form synovial bursae or tendon sheaths. Bursae often intervene between structures, such as tendons and bone, tendons and joints, or skin and bone, and reduce the friction of one structure moving over the other. Tendon sheaths surround tendons and also reduce friction.
 The fibrous membrane is formed by dense connective tissue and surrounds and stabilizes the joint. Parts of the fibrous membrane may thicken to form ligaments, which further stabilize the joint. Ligaments outside the capsule usually provide additional reinforcement.
The fibrous membrane is formed by dense connective tissue and surrounds and stabilizes the joint. Parts of the fibrous membrane may thicken to form ligaments, which further stabilize the joint. Ligaments outside the capsule usually provide additional reinforcement.
Descriptions of synovial joints based on shape and movement
Synovial joints are described based on shape and movement:
 based on the shape of their articular surfaces, synovial joints are described as plane (flat), hinge, pivot, bicondylar (two sets of contact points), condylar (ellipsoid), saddle, and ball and socket;
based on the shape of their articular surfaces, synovial joints are described as plane (flat), hinge, pivot, bicondylar (two sets of contact points), condylar (ellipsoid), saddle, and ball and socket;
 based on movement, synovial joints are described as uniaxial (movement in one plane), biaxial (movement in two planes), and multiaxial (movement in three planes).
based on movement, synovial joints are described as uniaxial (movement in one plane), biaxial (movement in two planes), and multiaxial (movement in three planes).
Hinge joints are uniaxial, whereas ball and socket joints are multiaxial.
Specific types of synovial joints (Fig. 1.21)
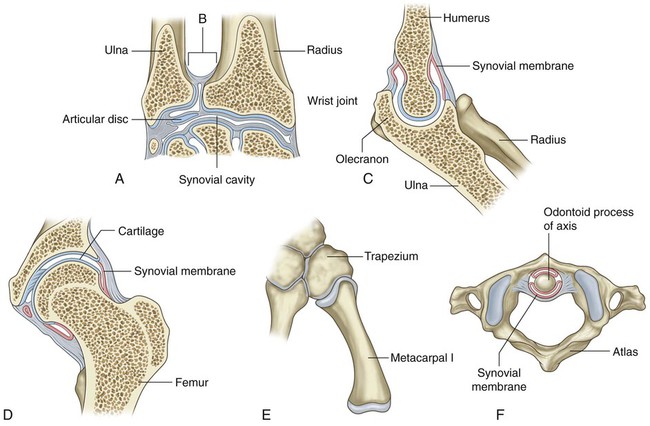
 Plane joints—allow sliding or gliding movements when one bone moves across the surface of another (e.g., acromioclavicular joint)
Plane joints—allow sliding or gliding movements when one bone moves across the surface of another (e.g., acromioclavicular joint)
 Hinge joints—allow movement around one axis that passes transversely through the joint; permit flexion and extension (e.g., elbow [humero-ulnar] joint)
Hinge joints—allow movement around one axis that passes transversely through the joint; permit flexion and extension (e.g., elbow [humero-ulnar] joint)
 Pivot joints—allow movement around one axis that passes longitudinally along the shaft of the bone; permit rotation (e.g., atlanto-axial joint)
Pivot joints—allow movement around one axis that passes longitudinally along the shaft of the bone; permit rotation (e.g., atlanto-axial joint)
 Bicondylar joints—allow movement mostly in one axis with limited rotation around a second axis; formed by two convex condyles that articulate with concave or flat surfaces (e.g., knee joint)
Bicondylar joints—allow movement mostly in one axis with limited rotation around a second axis; formed by two convex condyles that articulate with concave or flat surfaces (e.g., knee joint)
 Condylar (ellipsoid) joints—allow movement around two axes that are at right angles to each other; permit flexion, extension, abduction, adduction, and circumduction (limited) (e.g., wrist joint)
Condylar (ellipsoid) joints—allow movement around two axes that are at right angles to each other; permit flexion, extension, abduction, adduction, and circumduction (limited) (e.g., wrist joint)
 Saddle joints—allow movement around two axes that are at right angles to each other; the articular surfaces are saddle shaped; permit flexion, extension, abduction, adduction, and circumduction (e.g., carpometacarpal joint of the thumb)
Saddle joints—allow movement around two axes that are at right angles to each other; the articular surfaces are saddle shaped; permit flexion, extension, abduction, adduction, and circumduction (e.g., carpometacarpal joint of the thumb)
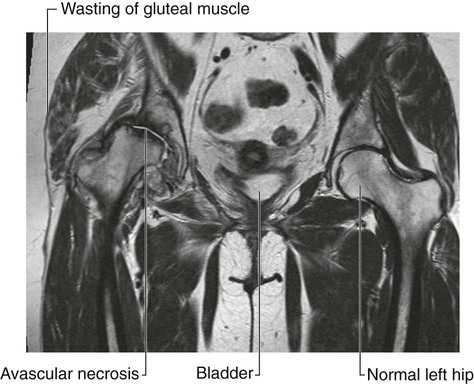
 Ball and socket joints—allow movement around multiple axes; permit flexion, extension, abduction, adduction, circumduction, and rotation (e.g., hip joint)
Ball and socket joints—allow movement around multiple axes; permit flexion, extension, abduction, adduction, circumduction, and rotation (e.g., hip joint)
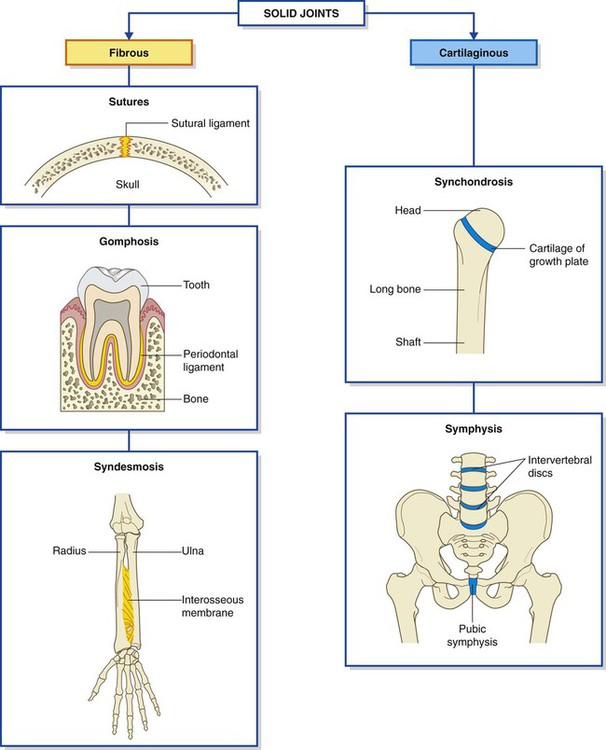
Solid joints
Solid joints are connections between skeletal elements where the adjacent surfaces are linked together either by fibrous connective tissue or by cartilage, usually fibrocartilage (Fig. 1.22). Movements at these joints are more restricted than at synovial joints.
Fibrous joints include sutures, gomphoses, and syndesmoses.
 Sutures occur only in the skull where adjacent bones are linked by a thin layer of connective tissue termed a sutural ligament.
Sutures occur only in the skull where adjacent bones are linked by a thin layer of connective tissue termed a sutural ligament.
 Gomphoses occur only between the teeth and adjacent bone. In these joints, short collagen tissue fibers in the periodontal ligament run between the root of the tooth and the bony socket.
Gomphoses occur only between the teeth and adjacent bone. In these joints, short collagen tissue fibers in the periodontal ligament run between the root of the tooth and the bony socket.
 Syndesmoses are joints in which two adjacent bones are linked by a ligament. Examples are the ligamentum flavum, which connects adjacent vertebral laminae, and an interosseous membrane, which links, for example, the radius and ulna in the forearm.
Syndesmoses are joints in which two adjacent bones are linked by a ligament. Examples are the ligamentum flavum, which connects adjacent vertebral laminae, and an interosseous membrane, which links, for example, the radius and ulna in the forearm.
Cartilaginous joints include synchondroses and symphyses.
 Synchondroses occur where two ossification centers in a developing bone remain separated by a layer of cartilage, for example, the growth plate that occurs between the head and shaft of developing long bones. These joints allow bone growth and eventually become completely ossified.
Synchondroses occur where two ossification centers in a developing bone remain separated by a layer of cartilage, for example, the growth plate that occurs between the head and shaft of developing long bones. These joints allow bone growth and eventually become completely ossified.
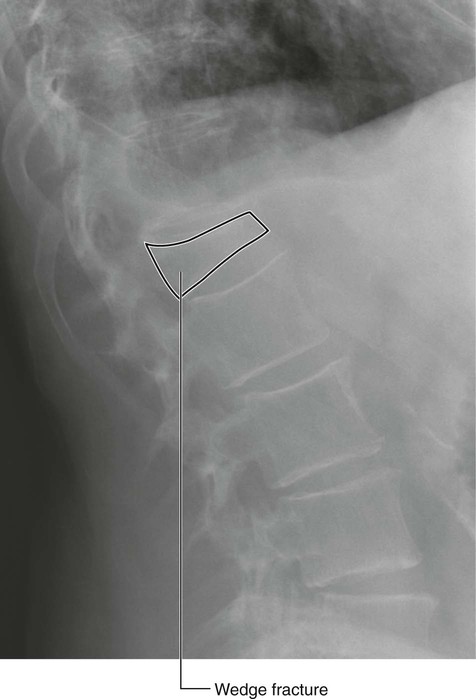
 Symphyses occur where two separate bones are interconnected by cartilage. Most of these types of joints occur in the midline and include the pubic symphysis between the two pelvic bones, and intervertebral discs between adjacent vertebrae.
Symphyses occur where two separate bones are interconnected by cartilage. Most of these types of joints occur in the midline and include the pubic symphysis between the two pelvic bones, and intervertebral discs between adjacent vertebrae.
Skin and fascias
Skin
Fascia
 Superficial (subcutaneous) fascia lies just deep to and is attached to the dermis of the skin. It is made up of loose connective tissue usually containing a large amount of fat. The thickness of the superficial fascia (subcutaneous tissue) varies considerably, both from one area of the body to another and from one individual to another. The superficial fascia allows movement of the skin over deeper areas of the body, acts as a conduit for vessels and nerves coursing to and from the skin, and serves as an energy (fat) reservoir.
Superficial (subcutaneous) fascia lies just deep to and is attached to the dermis of the skin. It is made up of loose connective tissue usually containing a large amount of fat. The thickness of the superficial fascia (subcutaneous tissue) varies considerably, both from one area of the body to another and from one individual to another. The superficial fascia allows movement of the skin over deeper areas of the body, acts as a conduit for vessels and nerves coursing to and from the skin, and serves as an energy (fat) reservoir.
 Deep fascia usually consists of dense, organized connective tissue. The outer layer of deep fascia is attached to the deep surface of the superficial fascia and forms a thin fibrous covering over most of the deeper region of the body. Inward extensions of this fascial layer form intermuscular septa that compartmentalize groups of muscles with similar functions and innervations. Other extensions surround individual muscles and groups of vessels and nerves, forming an investing fascia. Near some joints the deep fascia thickens, forming retinacula. These fascial retinacula hold tendons in place and prevent them from bowing during movements at the joints. Finally, there is a layer of deep fascia separating the membrane lining the abdominal cavity (the parietal peritoneum) from the fascia covering the deep surface of the muscles of the abdominal wall (the transversalis fascia). This layer is referred to as extraperitoneal fascia. A similar layer of fascia in the thorax is termed the endothoracic fascia.
Deep fascia usually consists of dense, organized connective tissue. The outer layer of deep fascia is attached to the deep surface of the superficial fascia and forms a thin fibrous covering over most of the deeper region of the body. Inward extensions of this fascial layer form intermuscular septa that compartmentalize groups of muscles with similar functions and innervations. Other extensions surround individual muscles and groups of vessels and nerves, forming an investing fascia. Near some joints the deep fascia thickens, forming retinacula. These fascial retinacula hold tendons in place and prevent them from bowing during movements at the joints. Finally, there is a layer of deep fascia separating the membrane lining the abdominal cavity (the parietal peritoneum) from the fascia covering the deep surface of the muscles of the abdominal wall (the transversalis fascia). This layer is referred to as extraperitoneal fascia. A similar layer of fascia in the thorax is termed the endothoracic fascia.
Muscular system
 Skeletal muscle forms the majority of the muscle tissue in the body. It consists of parallel bundles of long, multinucleated fibers with transverse stripes, is capable of powerful contractions, and is innervated by somatic and branchial motor nerves. This muscle is used to move bones and other structures, and provides support and gives form to the body. Individual skeletal muscles are often named on the basis of shape (e.g., rhomboid major muscle), attachments (e.g., sternohyoid muscle), function (e.g., flexor pollicis longus muscle), position (e.g., palmar interosseous muscle), or fiber orientation (e.g., external oblique muscle).
Skeletal muscle forms the majority of the muscle tissue in the body. It consists of parallel bundles of long, multinucleated fibers with transverse stripes, is capable of powerful contractions, and is innervated by somatic and branchial motor nerves. This muscle is used to move bones and other structures, and provides support and gives form to the body. Individual skeletal muscles are often named on the basis of shape (e.g., rhomboid major muscle), attachments (e.g., sternohyoid muscle), function (e.g., flexor pollicis longus muscle), position (e.g., palmar interosseous muscle), or fiber orientation (e.g., external oblique muscle).
 Cardiac muscle is striated muscle found only in the walls of the heart (myocardium) and in some of the large vessels close to where they join the heart. It consists of a branching network of individual cells linked electrically and mechanically to work as a unit. Its contractions are less powerful than those of skeletal muscle and it is resistant to fatigue. Cardiac muscle is innervated by visceral motor nerves.
Cardiac muscle is striated muscle found only in the walls of the heart (myocardium) and in some of the large vessels close to where they join the heart. It consists of a branching network of individual cells linked electrically and mechanically to work as a unit. Its contractions are less powerful than those of skeletal muscle and it is resistant to fatigue. Cardiac muscle is innervated by visceral motor nerves.
 Smooth muscle (absence of stripes) consists of elongated or spindle-shaped fibers capable of slow and sustained contractions. It is found in the walls of blood vessels (tunica media), associated with hair follicles in the skin, located in the eyeball, and found in the walls of various structures associated with the gastrointestinal, respiratory, genitourinary, and urogenital systems. Smooth muscle is innervated by visceral motor nerves.
Smooth muscle (absence of stripes) consists of elongated or spindle-shaped fibers capable of slow and sustained contractions. It is found in the walls of blood vessels (tunica media), associated with hair follicles in the skin, located in the eyeball, and found in the walls of various structures associated with the gastrointestinal, respiratory, genitourinary, and urogenital systems. Smooth muscle is innervated by visceral motor nerves.
Cardiovascular system
 arteries, which transport blood away from the heart;
arteries, which transport blood away from the heart;
 veins, which transport blood toward the heart;
veins, which transport blood toward the heart;
 capillaries, which connect the arteries and veins, are the smallest of the blood vessels and are where oxygen, nutrients, and wastes are exchanged within the tissues.
capillaries, which connect the arteries and veins, are the smallest of the blood vessels and are where oxygen, nutrients, and wastes are exchanged within the tissues.
 tunica externa (adventitia)—the outer connective tissue layer,
tunica externa (adventitia)—the outer connective tissue layer,
 tunica media—the middle smooth muscle layer (may also contain varying amounts of elastic fibers in medium and large arteries), and
tunica media—the middle smooth muscle layer (may also contain varying amounts of elastic fibers in medium and large arteries), and
 tunica intima—the inner endothelial lining of the blood vessels.
tunica intima—the inner endothelial lining of the blood vessels.
 Large elastic arteries contain substantial amounts of elastic fibers in the tunica media, allowing expansion and recoil during the normal cardiac cycle. This helps maintain a constant flow of blood during diastole. Examples of large elastic arteries are the aorta, the brachiocephalic trunk, the left common carotid artery, the left subclavian artery, and the pulmonary trunk.
Large elastic arteries contain substantial amounts of elastic fibers in the tunica media, allowing expansion and recoil during the normal cardiac cycle. This helps maintain a constant flow of blood during diastole. Examples of large elastic arteries are the aorta, the brachiocephalic trunk, the left common carotid artery, the left subclavian artery, and the pulmonary trunk.
 Medium muscular arteries are composed of a tunica media that contains mostly smooth muscle fibers. This characteristic allows these vessels to regulate their diameter and control the flow of blood to different parts of the body. Examples of medium muscular arteries are most of the named arteries, including the femoral, axillary, and radial arteries.
Medium muscular arteries are composed of a tunica media that contains mostly smooth muscle fibers. This characteristic allows these vessels to regulate their diameter and control the flow of blood to different parts of the body. Examples of medium muscular arteries are most of the named arteries, including the femoral, axillary, and radial arteries.
 Small arteries and arterioles control the filling of the capillaries and directly contribute to the arterial pressure in the vascular system.
Small arteries and arterioles control the filling of the capillaries and directly contribute to the arterial pressure in the vascular system.
Veins also are subdivided into three classes.
 Large veins contain some smooth muscle in the tunica media, but the thickest layer is the tunica externa. Examples of large veins are the superior vena cava, the inferior vena cava, and the portal vein.
Large veins contain some smooth muscle in the tunica media, but the thickest layer is the tunica externa. Examples of large veins are the superior vena cava, the inferior vena cava, and the portal vein.
 Small and medium veins contain small amounts of smooth muscle, and the thickest layer is the tunica externa. Examples of small and medium veins are superficial veins in the upper and lower limbs and deeper veins of the leg and forearm.
Small and medium veins contain small amounts of smooth muscle, and the thickest layer is the tunica externa. Examples of small and medium veins are superficial veins in the upper and lower limbs and deeper veins of the leg and forearm.
 The walls of veins, specifically the tunica media, are thin.
The walls of veins, specifically the tunica media, are thin.
 The luminal diameters of veins are large.
The luminal diameters of veins are large.
 There often are multiple veins (venae comitantes) closely associated with arteries in peripheral regions.
There often are multiple veins (venae comitantes) closely associated with arteries in peripheral regions.
 Valves often are present in veins, particularly in peripheral vessels inferior to the level of the heart. These are usually paired cusps that facilitate blood flow toward the heart.
Valves often are present in veins, particularly in peripheral vessels inferior to the level of the heart. These are usually paired cusps that facilitate blood flow toward the heart.
Lymphatic system
Lymphatic vessels
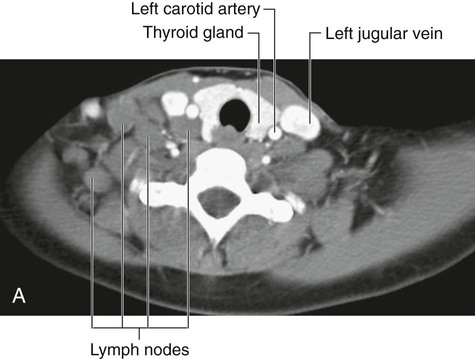
Lymphatic vessels mainly collect fluid lost from vascular capillary beds during nutrient exchange processes and deliver it back to the venous side of the vascular system (Fig. 1.29). Also included in this interstitial fluid that drains into the lymphatic capillaries are pathogens, cells of the lymphocytic system, cell products (such as hormones), and cell debris.
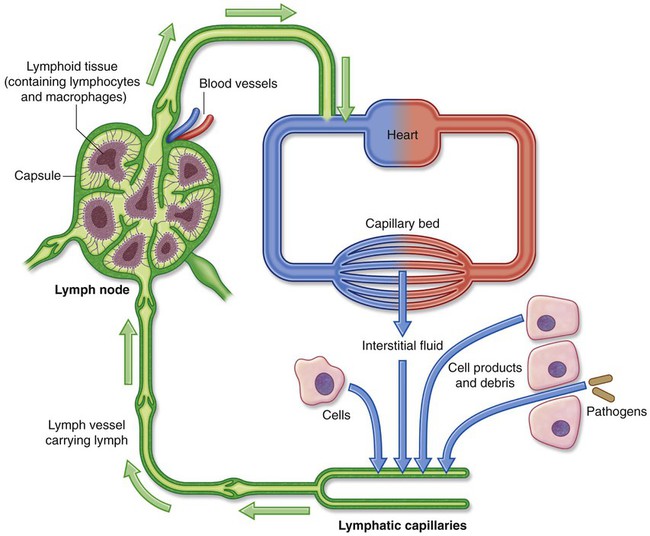
Lymph nodes
Lymph nodes are small (0.1–2.5 cm long) encapsulated structures that interrupt the course of lymphatic vessels and contain elements of the body’s defense system, such as clusters of lymphocytes and macrophages. They act as elaborate filters that trap and phagocytose particulate matter in the lymph that percolates through them. In addition, they detect and defend against foreign antigens that are also carried in the lymph (Fig. 1.29).
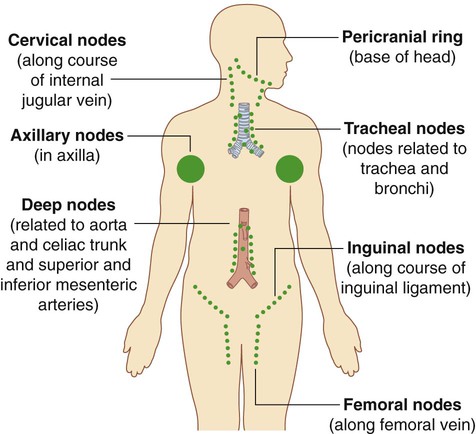
A number of regions in the body are associated with clusters or a particular abundance of lymph nodes (Fig. 1.30). Not surprisingly, nodes in many of these regions drain the body’s surface, the digestive system, or the respiratory system. All three of these areas are high-risk sites for the entry of foreign pathogens.
Lymphatic trunks and ducts
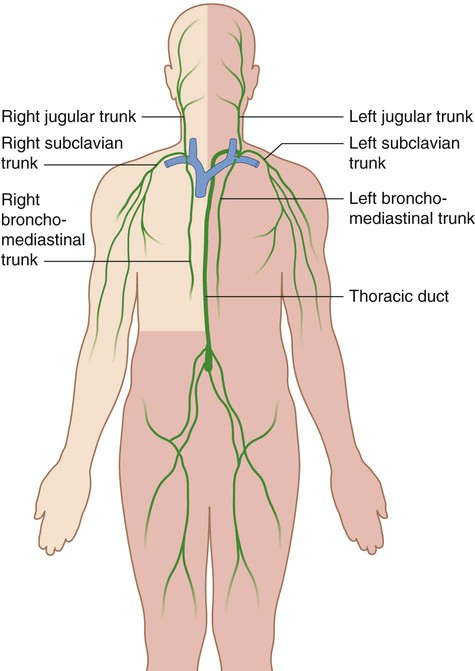
All lymphatic vessels coalesce to form larger trunks or ducts, which drain into the venous system at sites in the neck where the internal jugular veins join the subclavian veins to form the brachiocephalic veins (Fig. 1.31):
 Lymph from the right side of the head and neck, the right upper limb, right side of the thorax, and right side of the upper and more superficial region of the abdominal wall is carried by lymphatic vessels that connect with veins on the right side of the neck.
Lymph from the right side of the head and neck, the right upper limb, right side of the thorax, and right side of the upper and more superficial region of the abdominal wall is carried by lymphatic vessels that connect with veins on the right side of the neck.
 Lymph from all other regions of the body is carried by lymphatic vessels that drain into veins on the left side of the neck.
Lymph from all other regions of the body is carried by lymphatic vessels that drain into veins on the left side of the neck.
Nervous system
The nervous system can be separated into parts based on structure and on function:
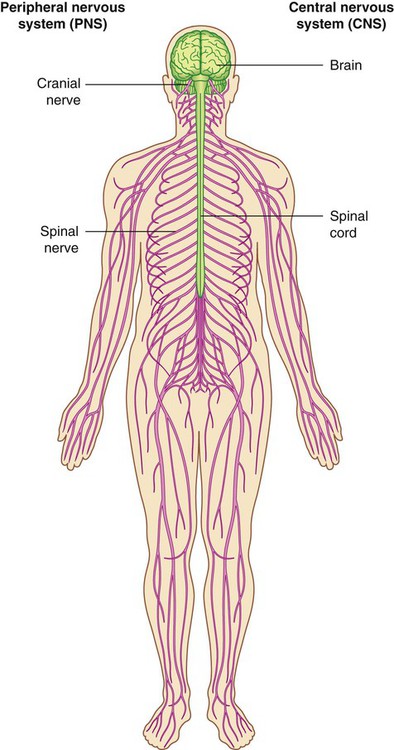
 structurally, it can be divided into the central nervous system (CNS) and the peripheral nervous system (PNS) (Fig. 1.33);
structurally, it can be divided into the central nervous system (CNS) and the peripheral nervous system (PNS) (Fig. 1.33);
 functionally, it can be divided into somatic and visceral parts.
functionally, it can be divided into somatic and visceral parts.
The PNS is composed of all nervous structures outside the CNS that connect the CNS to the body. Elements of this system develop from neural crest cells and as outgrowths of the CNS. The PNS consists of the spinal and cranial nerves, visceral nerves and plexuses, and the enteric system. The detailed anatomy of a typical spinal nerve is described in Chapter 2, as is the way spinal nerves are numbered. Cranial nerves are described in Chapter 8. The details of nerve plexuses are described in chapters dealing with the specific regions in which the plexuses are located.
Central nervous system
Meninges
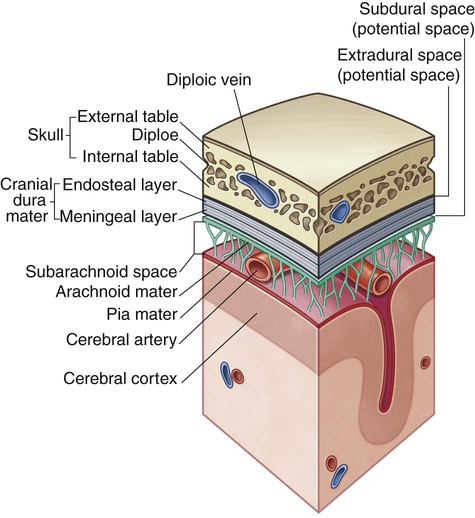
The meninges (Fig. 1.34) are three connective tissue coverings that surround, protect, and suspend the brain and spinal cord within the cranial cavity and vertebral canal, respectively:
 The dura mater is the thickest and most external of the coverings.
The dura mater is the thickest and most external of the coverings.
 The arachnoid mater is against the internal surface of the dura mater.
The arachnoid mater is against the internal surface of the dura mater.
Between the arachnoid and pia mater is the subarachnoid space, which contains CSF.
A further discussion of the cranial meninges can be found in Chapter 8 and of the spinal meninges in Chapter 2.
Functional subdivisions of the CNS
Functionally, the nervous system can be divided into somatic and visceral parts.
 The somatic part (soma, from the Greek for “body”) innervates structures (skin and most skeletal muscle) derived from somites in the embryo, and is mainly involved with receiving and responding to information from the external environment.
The somatic part (soma, from the Greek for “body”) innervates structures (skin and most skeletal muscle) derived from somites in the embryo, and is mainly involved with receiving and responding to information from the external environment.
 The visceral part (viscera, from the Greek for “guts”) innervates organ systems in the body and other visceral elements, such as smooth muscle and glands, in peripheral regions of the body. It is concerned mainly with detecting and responding to information from the internal environment.
The visceral part (viscera, from the Greek for “guts”) innervates organ systems in the body and other visceral elements, such as smooth muscle and glands, in peripheral regions of the body. It is concerned mainly with detecting and responding to information from the internal environment.
Somatic part of the nervous system
The somatic part of the nervous system consists of:
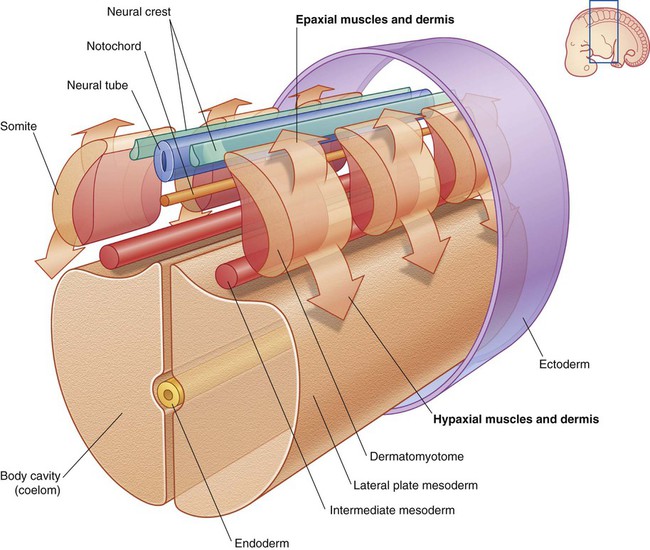
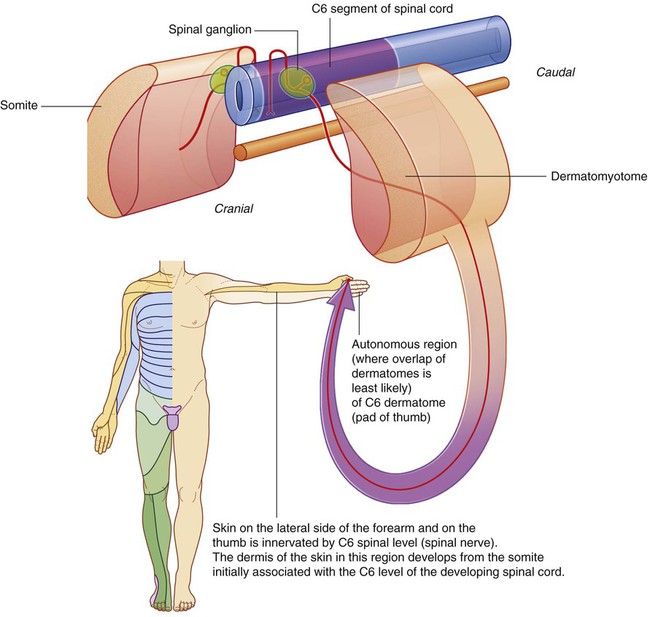
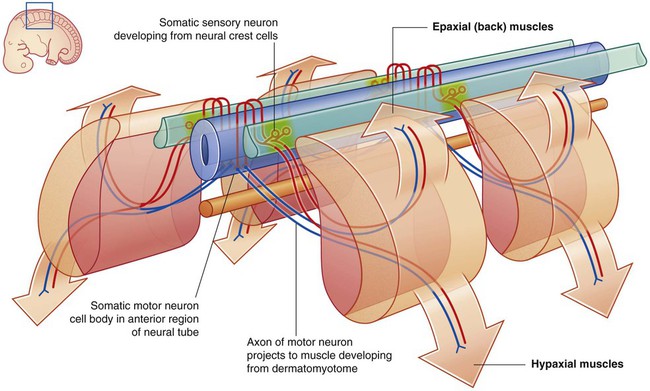
Somatic nerves arise segmentally along the developing CNS in association with somites, which are themselves arranged segmentally along each side of the neural tube (Fig. 1.35). Part of each somite (the dermatomyotome) gives rise to skeletal muscle and the dermis of the skin. As cells of the dermatomyotome differentiate, they migrate into posterior (dorsal) and anterior (ventral) areas of the developing body:
 Cells that migrate anteriorly give rise to muscles of the limbs and trunk (hypaxial muscles) and to the associated dermis.
Cells that migrate anteriorly give rise to muscles of the limbs and trunk (hypaxial muscles) and to the associated dermis.
 Cells that migrate posteriorly give rise to the intrinsic muscles of the back (epaxial muscles) and the associated dermis.
Cells that migrate posteriorly give rise to the intrinsic muscles of the back (epaxial muscles) and the associated dermis.
Simultaneously, derivatives of neural crest cells (cells derived from neural folds during formation of the neural tube) differentiate into neurons on each side of the neural tube and extend processes both medially and laterally (Fig. 1.36):
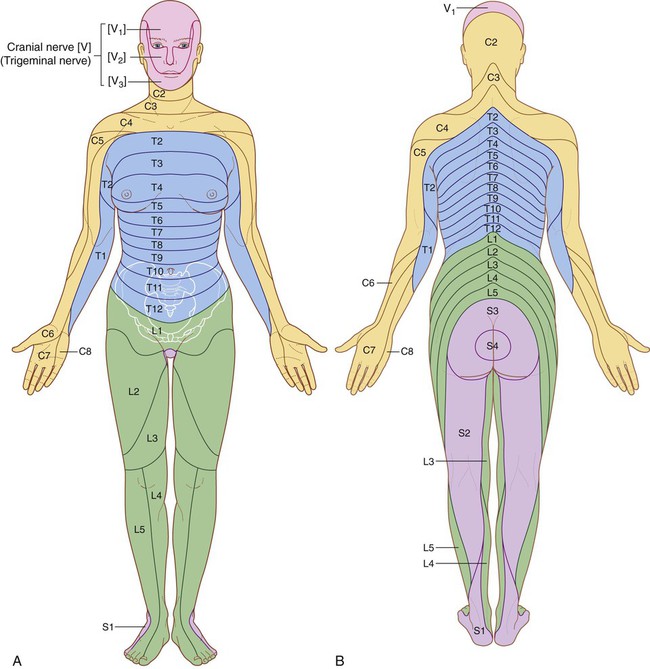
Dermatomes
Because cells from a specific somite develop into the dermis of the skin in a precise location, somatic sensory fibers originally associated with that somite enter the posterior region of the spinal cord at a specific level and become part of one specific spinal nerve (Fig. 1.37). Each spinal nerve therefore carries somatic sensory information from a specific area of skin on the surface of the body. A dermatome is that area of skin supplied by a single spinal cord level, or on one side, by a single spinal nerve.
Myotomes
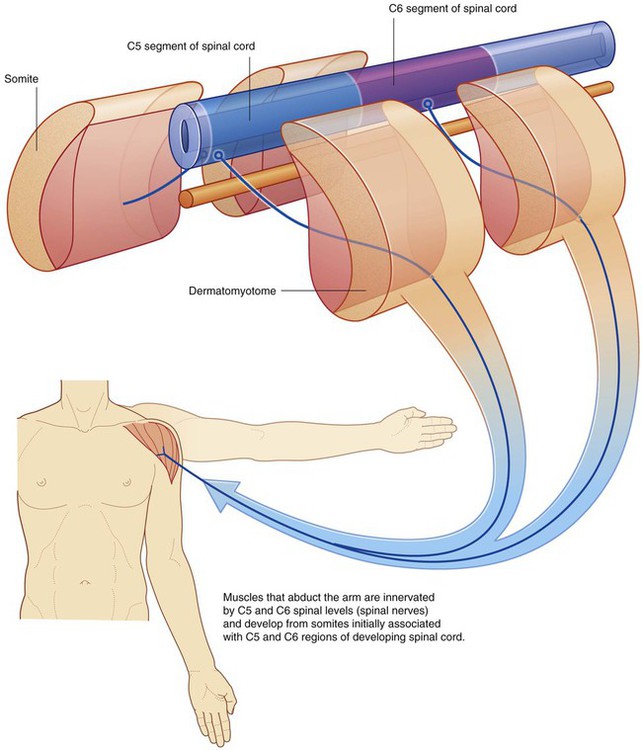
Myotomes are generally more difficult to test than dermatomes because each skeletal muscle in the body is usually innervated by nerves derived from more than one spinal cord level (Fig. 1.38).
 Muscles that move the shoulder joint are innervated mainly by spinal nerves from spinal cord levels C5 and C6.
Muscles that move the shoulder joint are innervated mainly by spinal nerves from spinal cord levels C5 and C6.
 Muscles that move the elbow are innervated mainly by spinal nerves from spinal cord levels C6 and C7.
Muscles that move the elbow are innervated mainly by spinal nerves from spinal cord levels C6 and C7.
 Muscles in the hand are innervated mainly by spinal nerves from spinal cord levels C8 and T1.
Muscles in the hand are innervated mainly by spinal nerves from spinal cord levels C8 and T1.
Visceral part of the nervous system
 Sensory nerves monitor changes in the viscera.
Sensory nerves monitor changes in the viscera.
 Motor nerves mainly innervate smooth muscle, cardiac muscle, and glands.
Motor nerves mainly innervate smooth muscle, cardiac muscle, and glands.
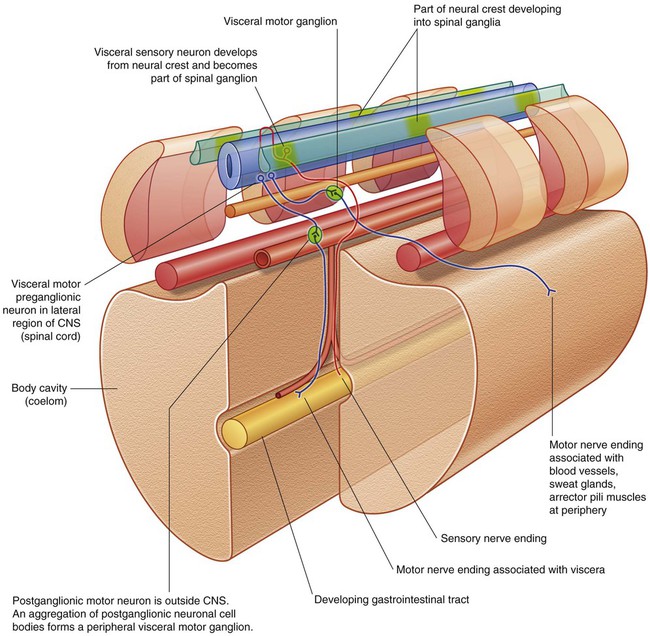
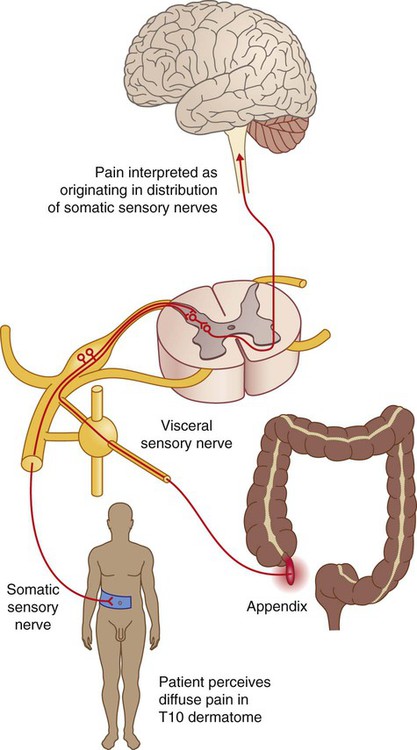
Like the somatic part of the nervous system, the visceral part is segmentally arranged and develops in a parallel fashion (Fig. 1.40).
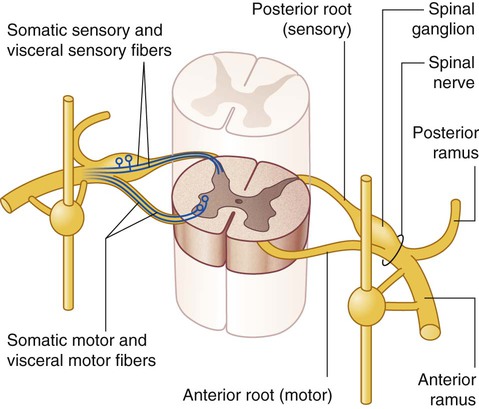
Visceral sensory and motor fibers enter and leave the CNS with their somatic equivalents (Fig. 1.41). Visceral sensory fibers enter the spinal cord together with somatic sensory fibers through posterior roots of spinal nerves. Preganglionic fibers of visceral motor neurons exit the spinal cord in the anterior roots of spinal nerves, along with fibers from somatic motor neurons.
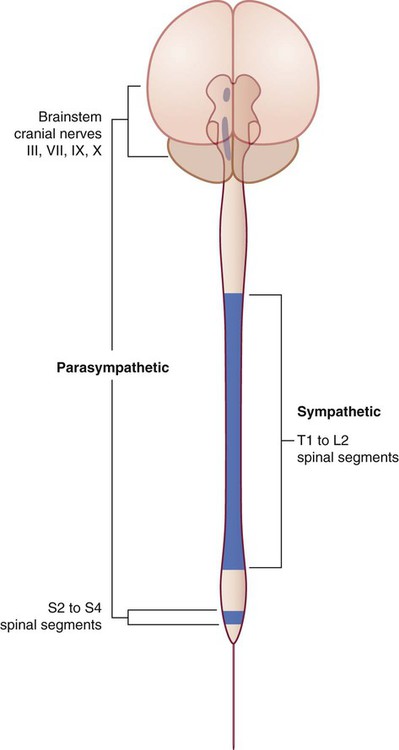
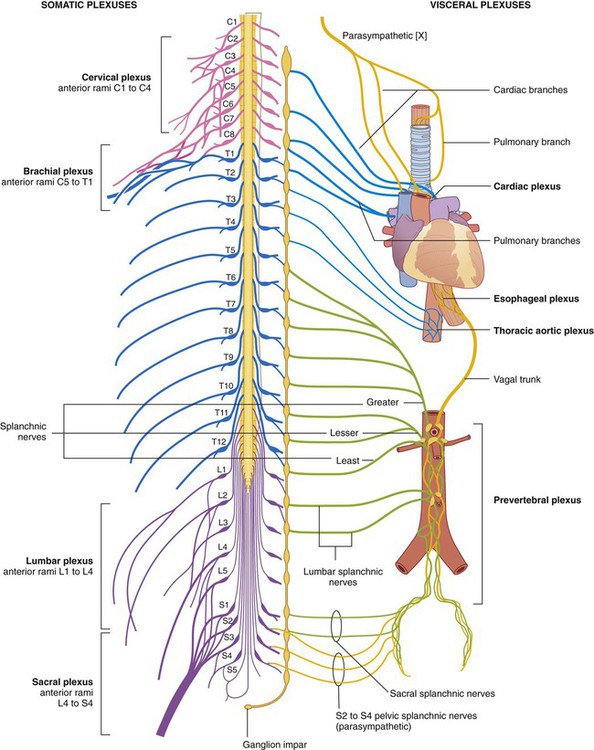
Visceral motor and sensory fibers do not enter and leave the CNS at all levels (Fig. 1.42):
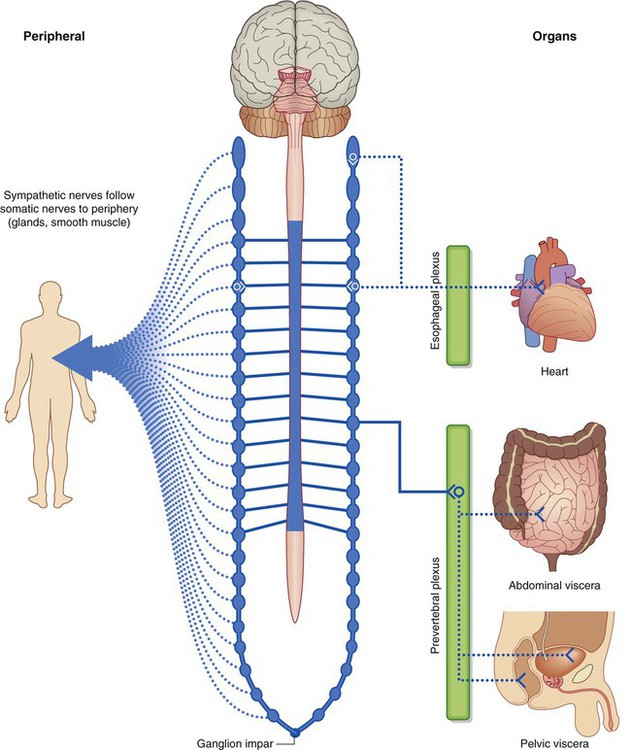
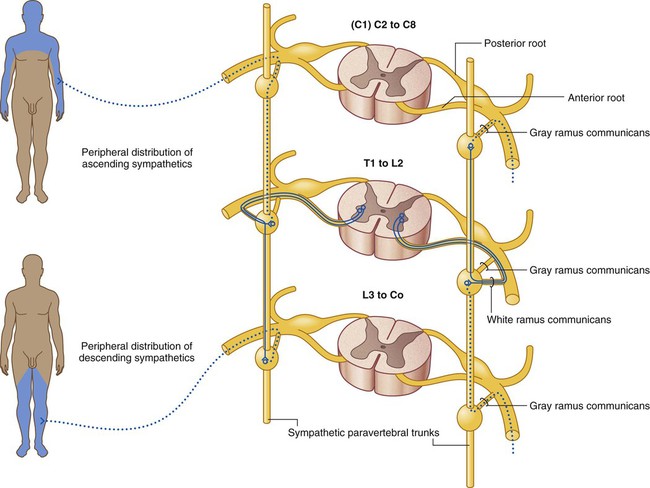
Sympathetic system
The sympathetic part of the autonomic division of the PNS leaves thoracolumbar regions of the spinal cord with the somatic components of spinal nerves T1 to L2 (Fig. 1.43). On each side, a paravertebral sympathetic trunk extends from the base of the skull to the inferior end of the vertebral column where the two trunks converge anteriorly to the coccyx at the ganglion impar. Each trunk is attached to the anterior rami of spinal nerves and becomes the route by which sympathetics are distributed to the periphery and all viscera.
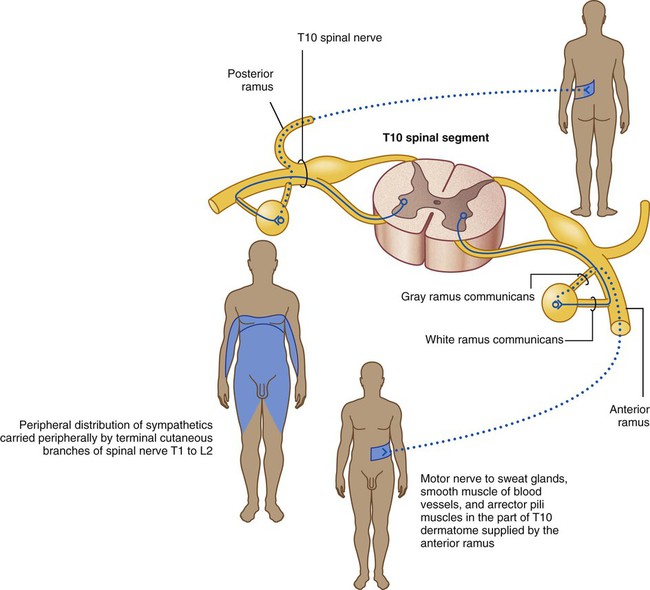
1 Peripheral sympathetic innervation at the level of origin of the preganglionic fiber
Preganglionic sympathetic fibers may synapse with postganglionic motor neurons in ganglia associated with the sympathetic trunk, after which postganglionic fibers enter the same anterior ramus and are distributed with peripheral branches of the posterior and anterior rami of that spinal nerve (Fig. 1.44). The fibers innervate structures at the periphery of the body in regions supplied by the spinal nerve. The gray ramus communicans connects the sympathetic trunk or a ganglion to the anterior ramus and contains the postganglionic sympathetic fibers. It appears gray because postganglionic fibers are nonmyelinated. The gray ramus communicans is positioned medial to the white ramus communicans.
2 Peripheral sympathetic innervation above or below the level of origin of the preganglionic fiber
Preganglionic sympathetic fibers may ascend or descend to other vertebral levels where they synapse in ganglia associated with spinal nerves that may or may not have visceral motor input directly from the spinal cord (i.e., those nerves other than T1 to L2) (Fig. 1.45).
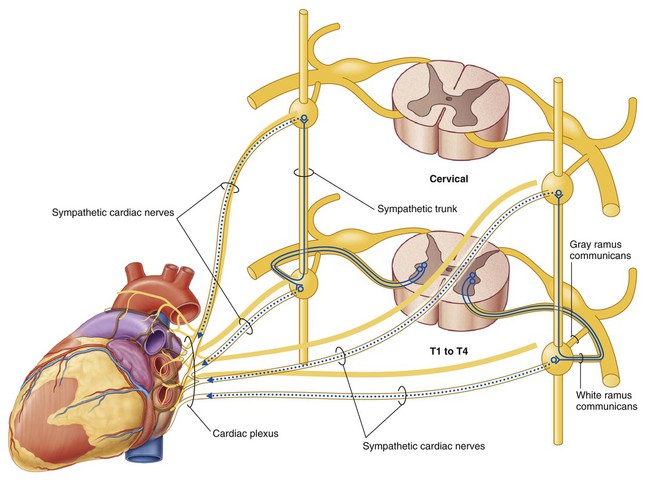
3 Sympathetic innervation of thoracic and cervical viscera
Preganglionic sympathetic fibers may synapse with postganglionic motor neurons in ganglia and then leave the ganglia medially to innervate thoracic or cervical viscera (Fig. 1.46). They may ascend in the trunk before synapsing, and after synapsing the postganglionic fibers may combine with those from other levels to form named visceral nerves, such as cardiac nerves. Often, these nerves join branches from the parasympathetic system to form plexuses on or near the surface of the target organ, for example, the cardiac and pulmonary plexuses. Branches of the plexus innervate the organ. Spinal cord levels T1 to T5 mainly innervate cranial, cervical, and thoracic viscera.
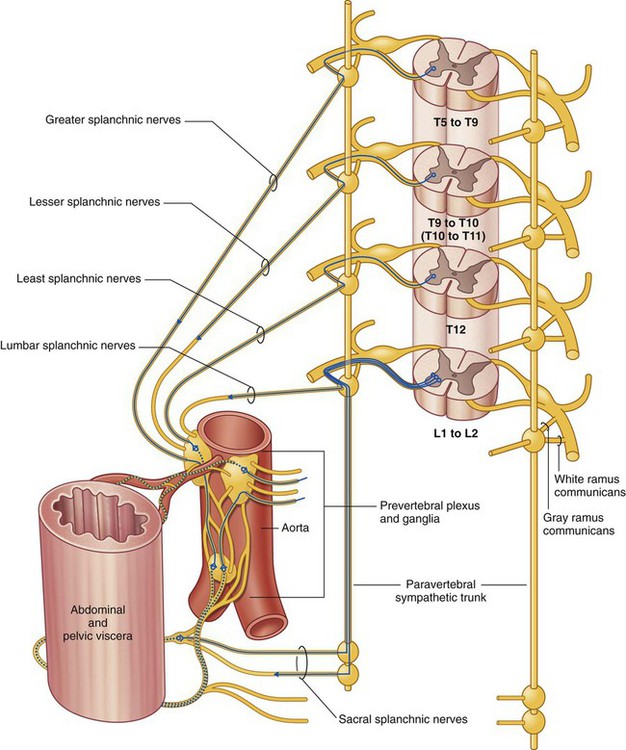
4 Sympathetic innervation of the abdomen and pelvic regions and the adrenals
Preganglionic sympathetic fibers may pass through the sympathetic trunk and paravertebral ganglia without synapsing and, together with similar fibers from other levels, form splanchnic nerves (greater, lesser, least, lumbar, and sacral), which pass into the abdomen and pelvic regions (Fig. 1.47). The preganglionic fibers in these nerves are derived from spinal cord levels T5 to L2.
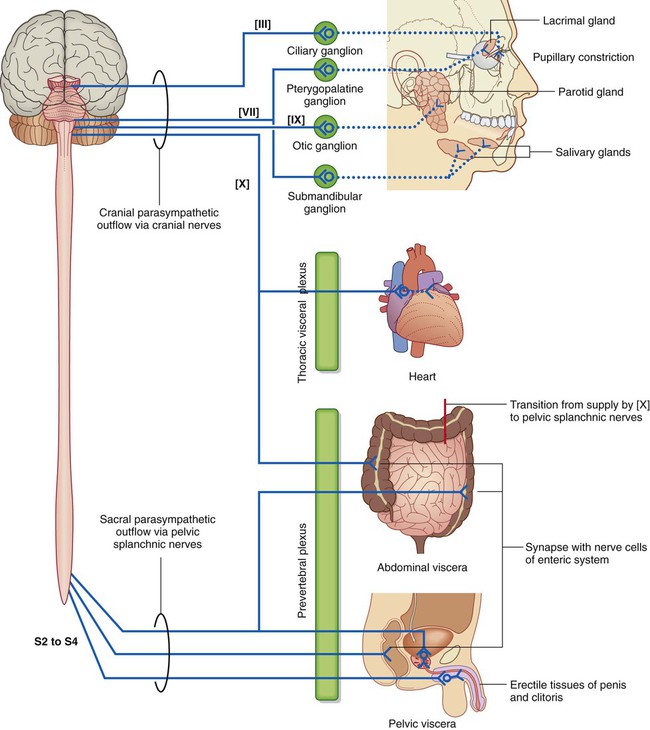
Parasympathetic system
The parasympathetic part of the autonomic division of the PNS (Fig. 1.48) leaves cranial and sacral regions of the CNS in association with:
 cranial nerves III, VII, IX, and X: III, VII, and IX carry parasympathetic fibers to structures within the head and neck only, whereas X (the vagus nerve) also innervates thoracic and most abdominal viscera; and
cranial nerves III, VII, IX, and X: III, VII, and IX carry parasympathetic fibers to structures within the head and neck only, whereas X (the vagus nerve) also innervates thoracic and most abdominal viscera; and
 spinal nerves S2 to S4: sacral parasympathetic fibers innervate inferior abdominal viscera, pelvic viscera, and the arteries associated with erectile tissues of the perineum.
spinal nerves S2 to S4: sacral parasympathetic fibers innervate inferior abdominal viscera, pelvic viscera, and the arteries associated with erectile tissues of the perineum.
The enteric system
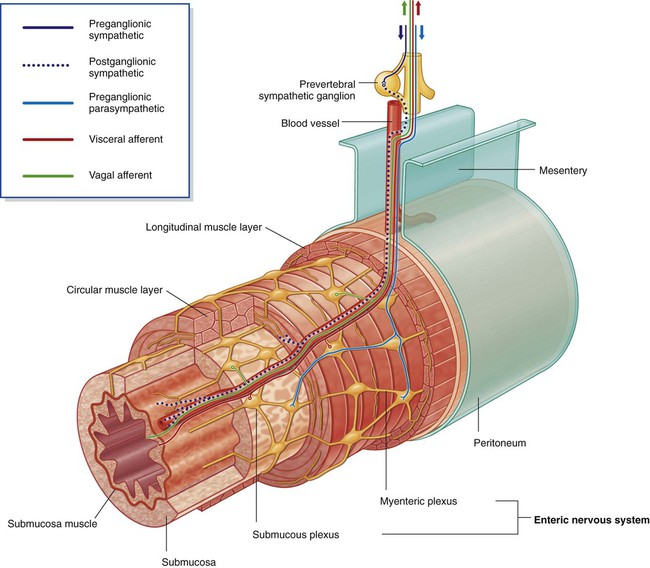
The enteric nervous system consists of motor and sensory neurons and their support cells, which form two interconnected plexuses, the myenteric and submucous nerve plexuses, within the walls of the gastrointestinal tract (Fig. 1.49). Each of these plexuses is formed by:
 ganglia, which house the nerve cell bodies and associated cells, and
ganglia, which house the nerve cell bodies and associated cells, and
 bundles of nerve fibers, which pass between ganglia and from the ganglia into surrounding tissues.
bundles of nerve fibers, which pass between ganglia and from the ganglia into surrounding tissues.
Sensory information from the enteric system is carried back to the CNS by visceral sensory fibers.
Visceral plexuses
Visceral nerve plexuses are formed in association with viscera and generally contain efferent (sympathetic and parasympathetic) and afferent components (Fig. 1.50). These plexuses include cardiac and pulmonary plexuses in the thorax and a large prevertebral plexus in the abdomen anterior to the aorta, which extends inferiorly onto the lateral walls of the pelvis. The massive prevertebral plexus supplies input to and receives output from all abdominal and pelvic viscera.