Blood and the immune system contain a wide variety of cells and carry out diverse functions. All the components of blood and the immune system may be considered as connective tissue and the vast majority of the cells is derived from mesoderm. Blood flows around the body in tubes known as blood vessels (Chapter 10) and is involved in moving cells and molecules. Tissue fluid (extracellular fluid), which bathes many of the cells in the body, is the aqueous component of extracellular matrix (Chapter 4) and is formed from blood. The immune system protects the body from invasion and damage by microorganisms and from many potentially harmful molecules. This system recognises cells and molecules ‘foreign’ to the body and generates immune cells and molecules in defensive immune responses. The immune system involves a wide variety of cells and molecules including non-specialised and specialised cells and molecules which carry out immune responses. The molecules vary in size and type but many are large protein molecules such as antibodies which react specifically with other molecules (antigens). Blood plays a major role in transporting immune cells and antibodies around the body.
The cellular components of the immune system, as well as circulating in blood, are widely distributed throughout organs of the body and are predominant in specialised organs (e.g. the thymus and spleen). Immune cells are also present in large numbers in lymph nodes, structures which are integral parts of the circulatory system that return excess tissue fluid to blood (see below and
Chapter 10). Localised clusters of immune cells are present in other regions of the body, particularly where mucosal surfaces are exposed to harmful molecules and organisms in the environment (e.g. substances ingested into the digestive tract or breathed into the respiratory tract).
Blood
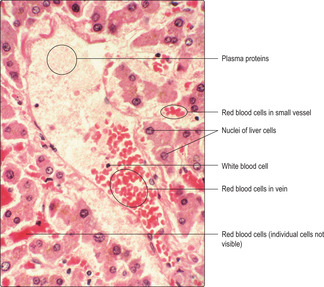
Blood consists of cells and parts of cells suspended in a fluid, the plasma. The cellular components of blood are red and white blood cells (respectively, erythrocytes and leucocytes) and parts of cells, platelets (thrombocytes). Plasma is a straw-coloured fluid that contains electrolytes, carbohydrates, lipids and proteins (including albumin and globulins); however, plasma is mainly water. Erythrocytes constitute just over 40% of blood volume with just 1% leucocytes; most of the rest is plasma.
Although blood is considered to be a form of connective tissue in which the extracellular matrix is the fluid plasma, the function of blood differs from the functions of other forms of connective tissue. Blood circulates via the cardiovascular system and delivers oxygen and various molecules, including nutrients and hormones, to cells of the body. Blood also facilitates the removal of waste molecules from body tissues, including carbon dioxide. Importantly, blood is able to coagulate and prevent excessive blood loss if blood vessels are damaged.
The ability of blood to deliver molecules to and remove other molecules from the body is facilitated by blood forming tissue fluid (extracellular fluid). Some of the plasma fluid (and the smaller molecules it contains) leaves blood vessels via the endothelial cells lining small blood vessels and bathes surrounding cells in tissue fluid. White blood cells also leave small blood vessels and these are particularly important in the defence mechanisms provided by the immune system. Some tissue fluid and white blood cells eventually return to blood via a series of lymphatic vessels and lymph nodes (see below).
Blood cells
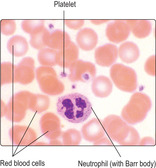
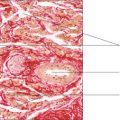
Blood cells in routine histological sections may be identified as individual cells. However, in many instances details of individual blood cells may not readily be distinguished (
Fig. 8.1). To study blood cells in detail it is usual to spread blood onto a glass microscope slide, a process which makes a ‘blood smear’. Smears display the whole of the cells as opposed to cells in histological sections which may have been sliced during preparation (and show only part of individual cells).
Erythrocytes (red blood cells)
An erythrocyte is a membrane-bound cytoplasmic structure which does not have a nucleus. Erythrocytes lose their nuclei during their formation in bone marrow, just before they are released into blood vessels. Mature erythrocytes are biconcave discs approximately 7
μm in diameter but are easily distorted and are able to pass along narrow blood vessels about 3.5μm in diameter. Identifying red blood cells and knowing their maximum diameter can be used as a scale for assessing the size of other features in histological specimens (Fig. 8.1). In blood smears, erythrocytes usually appear rounded and many have palely stained centres reflecting their central, thinner region of cytoplasm (Fig. 8.2, Fig. 8.3 and Fig. 8.4).Erythrocytes transport oxygen from the lungs to the other parts of the body. The majority of their cytoplasm is made up of the iron-containing protein haemoglobin and only a few organelles (mitochondria and ribosomes) are present. Erythrocytes are referred to as red blood cells because the iron of haemoglobin confers the red colour on blood. Oxygen has a high affinity for the iron in haemoglobin in locations where there is a high oxygen concentration, such as the lungs. In regions with relatively low oxygen concentrations, such as in most body regions other than the lungs, the oxygen is liberated and used in metabolic processes. The reverse is true of carbon dioxide, a waste product of glucose metabolism. It is the globin (the protein component of haemoglobin) that carries some of the carbon dioxide from body tissues to the lungs.
Erythrocytes have a life span of approximately 120
days and after this time they are destroyed by cells in the liver, spleen and bone marrow, probably because they become less able to change shape. The rate of production of new erythrocytes from the bone marrow normally equals the rate at which they are destroyed. Any loss of blood from the circulation, as a result of trauma for example, is followed by an increase in the production of erythrocytes and their release into circulation until normal numbers in blood are restored.
 Clinical note
Clinical note
Anaemia This common blood disorder occurs when there is not enough haemoglobin to supply oxygen to support the metabolic requirements of the body’s cells. An anaemic person may look pale, feel weak and easily become short of breath. The most common cause of anaemia is a shortage of iron, the element essential for the formation and function of haemoglobin. Excessively heavy blood loss, e.g. at menstruation, may be a cause of anaemia as enough iron may not be available to support red blood cell production at a rate which replaces the losses, particularly if the losses have occurred repeatedly over many months.
Other types of anaemia have a genetic basis. For example, in sickle cell anaemia the haemoglobin molecule is abnormal. In regions of the body in which oxygen levels are low the haemoglobin molecule becomes rigid and the red blood cells become less flexible and take on the shape of a sickle. As a result, many red blood cells die prematurely in the spleen or they may block small vessels around the body. Life expectancy is likely to be considerably reduced.
Leucocytes (white blood cells)
Granulocytes
■
Neutrophils. These constitute about 70% of the total leucocyte population in peripheral blood. Neutrophils are also known as polymorphonuclear leucocytes (PMNLs) because each has a multilobed nucleus (
Fig. 8.2). The nuclei of neutrophils in females are characterised by the possession of a Barr body (
Fig. 8.2), which is manifest as a small drumstick projection from one of the lobes of the nucleus. Barr bodies represent the inactive second X chromosome of females, but they are seen on only a small proportion of neutrophil nuclei. The granules of neutrophils do not stain with acidic or basic dyes. Some of the granules are very small and not readily seen by light microscopy. Some are lysosomes and the enzymes they contain are typical of lysosomes, e.g. acid phosphatase.
Neutrophils develop in bone marrow, enter blood vessels and thus circulate around the body. However, they migrate out of blood vessels within a few days and move rapidly through body tissues where normally they die after a few days. If neutrophils encounter bacteria they are able to engulf and kill them. They kill bacteria by a variety of mechanisms, one of which involves hydrogen peroxide. Neutrophils that have performed their killing function die and accumulate in pus at the site of the infection. If the infection persists, large numbers of neutrophils leave blood and are attracted to the site(s) of infection and large numbers are also released into circulation from the bone marrow.
■
Eosinophils. An eosinophil is characterised by its bi-lobed nucleus and by numerous granules which stain heavily pink with eosin and with the staining methods for examining blood smears (
Fig. 8.3). Lysosomes are also present in eosinophils. Eosinophils develop in bone marrow and normally constitute 2–4% of the leucocytes present in peripheral blood. Eosinophils function by their ability to respond to antigen–antibody complexes and to parasites. Their granules release their contents which bind to, and kill, parasites. They are able to phagocytose and digest antigen–antibody complexes and the remains of parasites. In addition, they release antihistamines that reduce the inflammatory processes that are initiated by such complexes and organisms. Eosinophils are present in increased numbers in blood and body tissues during allergic reactions, such as hay fever, and in response to infections by parasites.
■ Basophils. The granules of basophils are stained by basic dyes such as haematoxylin. The nuclei of basophils are bi-lobed but the granules are often so numerous that they obscure the rest of the cytoplasm and the nucleus in blood smears. Basophils develop in bone marrow and they constitute only 0.5–1% of the total leucocyte population in peripheral blood. They leave the blood and are involved in initiating inflammatory reactions.
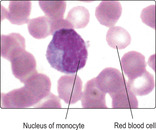
Agranulocytes
■ Lymphocytes. These make up 20–30% of the total number of leucocytes circulating in blood. Lymphocytes are also present in bone marrow, thymus, spleen and lymph nodes, and in lymphoid regions in other organs, e.g. in parts of the gastrointestinal, urinary, reproductive and respiratory tracts. Some lymphocytes develop in bone marrow but others are produced in the thymus and at other sites in the body in response to immune stimuli. In general, lymphocytes function at such sites, and not in peripheral blood.
Lymphocytes may be described as small, medium or large. Small lymphocytes make up about 95% of the lymphocytes in peripheral blood and they are distinguished by having a densely stained nucleus that occupies the bulk of the cell (
Fig. 8.3). Lymphocytes responding to an immune stimulus are larger than small lymphocytes and have relatively more cytoplasm – they are described as medium or large lymphocytes.
Lymphocytes are also categorised according to their function. Their morphology does not distinguish the functional types but categories can be identified by using labelled antibodies to identify specific molecules on their cell membrane. The categories are B lymphocytes, T lymphocytes and natural killer (NK) cells.
■ B lymphocytes constitute 5–15% of small lymphocytes in peripheral blood. They migrate out of blood vessels and through body tissues and respond to antigenic stimulation by increasing in size and differentiating into plasma cells (see below).
■ T lymphocytes constitute 65–75% of small lymphocytes in peripheral blood. They are small when they are inactive but differentiate into larger lymphocytes when responding to immune stimulation. T lymphocytes are responsible for cell-mediated immunity, which is the type of cellular immune response engaged in detecting foreign cells and destroying them. This involves T lymphocytes detecting certain molecules which may be on the surface of foreign cells, or on the body’s own cells that have become abnormal (e.g. malignant or infected by virus). This recognition stimulates the T lymphocytes to divide and increases the number of T lymphocytes able to attack specifically and destroy ‘foreign’ cells. T lymphocytes also produce a variety of molecular signals that regulate other cells involved in mounting immune responses.
■ Natural killer (NK) cells comprise 10–15% of the lymphocytes in peripheral blood. They are larger cells than small lymphocytes and they have a few granules in their cytoplasm. NK cells migrate through body tissues and have the ability to detect and kill foreign cells. Their activity is regulated by factors produced by subsets of T lymphocytes.
Platelets (thrombocytes)
Platelets (
Fig. 8.2) are cytoplasmic fragments of megakaryocytes, a large cell type present in bone marrow (see below). Platelets are released into blood vessels in bone marrow and they then circulate around the body. Platelets are essential for blood clotting and help control haemorrhage.
Other cells involved in immune responses
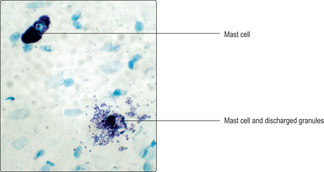
Mast cells
Mast cells are present in connective tissues of the body and they are densely packed with granules which may hide the nucleus (
Fig. 8.5). They resemble the basophils in blood. Mast cells have receptors for a type of antibody (immunoglobulin E) on their cell membranes and these antibodies are produced in response to allergen(s). A subsequent exposure to the same allergen(s) causes the mast cells to release histamine (a vasoactive molecule which affects the diameter of blood vessels) from their granules as well as other mediators of the inflammatory response. This type of reaction can be rapid and fatal and is known as an anaphylactic reaction.
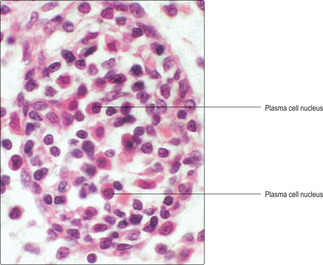
Plasma cells
Plasma cells are often evident at sites of infection associated with chronic inflammation and in lymph nodes (see below). They are the end stage of differentiation of B lymphocytes and they mount a humoral immune response by produc-ing specific antibodies (e.g. immunoglobulins A and G) to specific antigens. Plasma cells may appear ovoid in shape, are larger than the B lymphocytes and are identified by the eccentric position of their nucleus (
Fig. 8.6). The cytoplasm of each plasma cell has large amounts of rough endoplasmic reticulum synthesising a particular immunoglobulin which functions as a specific antibody. The antibody molecules are released from plasma cells and circulate in tissue fluids, lymph and peripheral blood where they are able to react with their specific antigen(s).

Clinical note
White blood cell disorders Increased numbers of normal neutrophils in peripheral blood or other areas of the body may be due to a bacterial infection whereas increased numbers of eosinophils may be due to a parasitic infection or to an allergic reaction.
Leukaemias result from the proliferation of malignant white blood cells in the bone marrow. Large numbers of white blood cells, which may appear normal or abnormal, enter peripheral blood. Leukaemias are classified according to the type of white cell produced in high numbers (granulocyte, lymphocyte or monocyte) and whether the progress of the disease can be described as chronic or acute. Chronic leukaemias progress slowly, but in acute leukaemias the disease process progresses rapidly and many of the cells released into the bloodstream appear immature or grossly abnormal.
Macrophages
Macrophages are able to phagocytose material such as dead cells and bacteria and inert particles, e.g. carbon. Some of the material they ingest (not carbon) is digested in lysosomes and some is presented as antigenic molecules to lymphocytes which then produce an immune response. Macrophages which have taken up inert material, such as carbon, remain in the body and account for the black colour seen in the lungs of many people at post mortem. Macrophage numbers can increase when exposure to antigens increases as monocytes leave peripheral blood and become macrophages.
Dendritic cells (antigen-presenting cells)
Dendritic cells are derived from cells in bone marrow and they are able to present antigens to lymphocytes and this initiates an immune response. Dendritic cells exhibit fine cytoplasmic processes which increase their surface area and hence the area available for antigen binding. They are present in the supporting connective tissue of many parenchymal organs and in lymph nodes. Dendritic cells in the skin are known as Langerhans cells and those in the brain as microglial cells.
The immune system
The immune system may be considered to have two types of response which help to protect the body from foreign molecules, cells and organisms, including viruses, bacteria and parasites.
■ Non-specific responses. These are carried out by cells such as neutrophils and macrophages which are able to engulf and destroy many microorganisms and molecules. The ability of neutrophils to migrate from blood vessels and find their way rapidly to sites of infection produces an acute inflammatory response which may quickly stop an infection.
■ Specific responses. The humoral (fluid) and cell-mediated responses carried out, respectively, by B and T lymphocytes are directed specifically at individual molecules (which may be free or attached to a cell’s membrane). Significantly these specific immune responses are associated with the ability of a lymphocyte to ‘remember’ a molecule it has encountered. At a subsequent meeting with a ‘remembered’ molecule such lymphocytes rapidly produce an immune response against the molecule and, importantly, also undergo rapid mitotic activity producing more lymphocytes which can also respond to the same molecule. This type of memory response is known as acquired immunity.
Immune cells are produced in the bone marrow, thymus, spleen and lymph nodes. In addition, there are numerous sites, particularly in the respiratory, digestive, urinary and reproductive systems, where lymphocytes are present in large numbers and are able to respond to foreign molecules or microorganisms.
Bone marrow
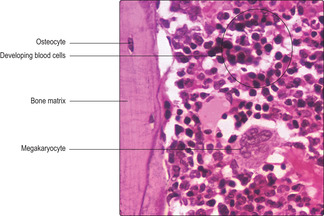
Bone marrow occupies spaces within bones (
Chapter 9). Red and white blood cells and platelets develop in bone marrow in a process known as haematopoiesis. In regions where haemato-poiesis occurs the marrow appears red to the unaided eye. With age, many of the haematopoietic regions are replaced by adipose cells which give marrow a yellow colour.
Within bone marrow blood flows in endothelium-lined blood vessels and a reticulin meshwork surrounding the vessels is packed with developing blood cells. Macrophages are associated with the meshwork and they are involved in destroying aged red blood cells. Megakaryocytes are also in the meshwork and they shed fragments of their cytoplasm, as platelets, into adjacent blood vessels. The appearance of bone marrow in sections reveals few details of the structure of the developing blood cells and smears of bone marrow are examined for detailed studies. Megakaryocytes, however, can be identified readily in sectioned material by their large size and multilobed nucleus (
Fig. 8.7).
Haematopoiesis
All blood cells arise from one type of stem cell in bone marrow which resembles a small lymphocyte and is described as being pluripotent. These stem cells undergo successive rounds of mitosis and replace themselves and produce cells which are able to differentiate into different types of cell with restricted stem cell ability. After several cycles of mitotic activity the potential to develop into several types of blood cell is restricted and unipotent stem cells develop. Unipotent stem cells are committed to produce one type of blood cell (and replace themselves). Unipotent stem cells are categorised by the type of blood cell they produce. For details of the stages in the formation of erythrocytes, eosinophils, basophils, neutrophils, monocytes, T lymphocytes and B lymphocytes, NK cells and megakaryocytes from stem cells, a more detailed textbook of histology or haematology should be consulted.
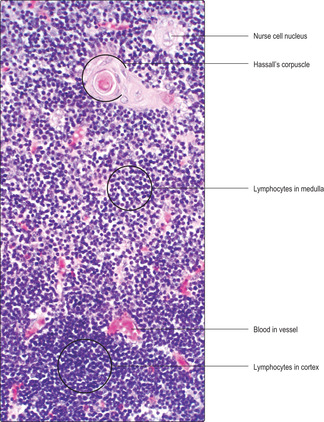
Thymus
The thymus is an organ in the mid-line of the upper anterior part of the thorax which is prominent in young children and gradually regresses after puberty. It is covered by a connective tissue capsule and has a fine meshwork which extends throughout the thymus. Unusually, the meshwork is formed by epithelial, not connective tissue, cells. The epithelial mesh supports lymphocytes and two regions, a peripheral cortex and inner medulla, are described. Virtually all of the lymphocytes in the thymus are in direct contact with the epithelial meshwork and the epithelial cells are sometimes referred to as ‘nurse’ cells.
Lymphocytes are densely packed in the meshwork in the cortex (
Fig. 8.8). In the medulla, fewer lymphocytes are present, and they appear in irregular clumps (
Fig. 8.8). The most recognisable components of the support meshwork are the epithelial cells which form whorl-like, lamellated structures in the medulla known as Hassall’s corpuscles (
Fig. 8.8). The function of these corpuscles is not known.
The thymus secretes factors that facilitate its functions. The functions are particularly important in the early stages of life and they are:
■ to provide an environment to receive immature T lymphocytes from bone marrow
■ to ensure that immature T lymphocytes become immunologically competent, i.e. able to produce immune responses to attack foreign molecules, cells and organisms
■ to ensure that immature T lymphocytes also become self-tolerant; this process enables T lymphocytes to distinguish ‘self’ from foreign cells and molecules and thus avoid attacking ‘self’ body cells and molecules
■ to release mature T lymphocytes into circulation.
The processes that produce mature T lymphocytes involve the generation of many new T lymphocytes by mitosis of the T lymphocytes in the cortex of the thymus. Many of these new lymphocytes die; these are thought to be T lymphocytes which are not self-tolerant. Other T lymphocytes move towards the medulla as they mature and become self-tolerant and immunologically competent. The mature T lymphocytes in the medulla are released into blood vessels. They live for many years and many leave the blood vessels and migrate through tissues where they may be triggered into producing immune responses.
Spleen
The spleen lies in the left, upper region of the abdomen. It is the largest lymphoid organ of the body and it has two main functions:
■ it monitors circulating blood for foreign material, particularly bacteria, and ensures immune responses develop to such material
■ it destroys aged red blood cells, probably when they have become relatively rigid.
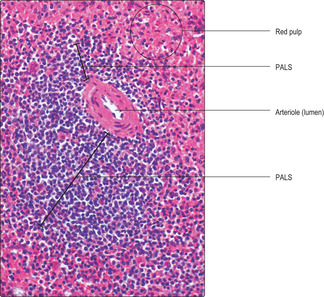
The spleen has a connective tissue capsule which is covered by a serosal membrane called the peritoneum (
Chapter 3). Connective tissue strands (trabeculae) extend from the capsule into the spleen and these support branches of arterial blood vessels distributing blood through the parenchyma. An intricate network of fine reticulin fibres connected to the trabeculae support the cells in the parenchyma. Two regions known as the red pulp and white pulp form the parenchyma. With the unaided eye the white pulp appears pale and the red pulp appears red: white cells are predominant in white pulp and red blood cells predominant in red pulp.
Some of the blood from central arterioles passes into endothelial-lined blood vessels (also known as sinuses or sinusoids) in the white pulp. These are relatively large spaces where blood moves slowly and blood cells, antigens and particulate matter intermingle. Macrophages attack any microorganisms present and macrophages and other antigen-presenting cells screen particulate matter for foreign antigens and ‘present’ them to lymphocytes which then mount immune responses.
■ Red pulp. Red pulp fills the spaces between white pulp. It receives blood that has passed through the central arterioles of the white pulp. The vascular arrangement of the spleen is unusual (in humans) in that some blood and blood cells leak from the sinuses and pass through the meshwork of the red pulp; this is described as an open circulation. Blood in red pulp passes among antigen-presenting cells, macrophages and lymphocytes and then returns into endothelium-lined sinuses. This passage through the red pulp enables immune responses to foreign molecules to develop and ageing red blood cells and platelets to be detected and destroyed. Macrophages ingest and digest the debris from dead cells and useful molecules circulate in blood and are reused. The blood in sinuses drains into venules (small veins) which join together and leave the spleen at the hilum. In addition, a closed circulation may also exist in humans whereby blood does not leave the vessels; instead, it remains in the endothelium-lined sinuses which connect arterioles with venules.
Lymphatic vessels
Lymphatic vessels are lined by endothelial cells and they begin as very small blind-ended tubes in most regions of the body. They serve to drain excess tissue fluid and transmit it through lymph nodes before it returns to peripheral blood in blood vessels (
Chapter 10). The fluid in lymph vessels is known as lymph. Valves in lymphatic vessels ensure drainage of lymph is unidirectional, away from an organ or region of the body.

Clinical note
Autoimmune disorders These are caused by inappropriate immune responses generated against the body’s own molecules (which may be free or on cell membranes). In myasthenia gravis, a condition in which muscle weakness and fatigue occurs, autoantibodies are detectable (in most patients) which interfere with synapses at neuromuscular junctions.
Lymph nodes
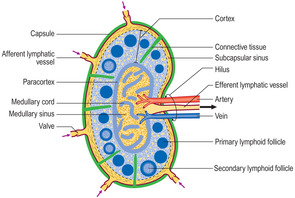
Lymph nodes are aggregations of lymphocytes where lymph is monitored for foreign molecules (e.g. in lymph or on bacteria, viruses or tumour cells) and where specific immune responses are generated as a result. Lymph nodes occur in defined anatomical sites where they receive lymph, which is draining tissue fluid from specific regions of the body. Lymph nodes, sometimes known as glands, are roughly bean shaped and their size depends on whether they are resting or are actively undergoing immune responses. In the case of an infection or tumour in a particular part of the body, the draining lymph node(s) can become swollen and painful.
Lymph nodes are encapsulated by connective tissue (Fig. 8.10). Projecting inwards from the capsule, at intervals, are connective tissue trabeculae (septa) and a fine meshwork of reticulin fibres extends throughout each node. Blood vessels enter and leave at the hilum of each node. Lymph is delivered to each node by several afferent lymphatic vessels which penetrate the capsule. Only one efferent vessel drains each node of lymph and this leaves at the hilum. Lying within the parenchyma of each node are aggregations of lymphocytes in two main regions, the cortex and medulla (
Fig. 8.10).
■
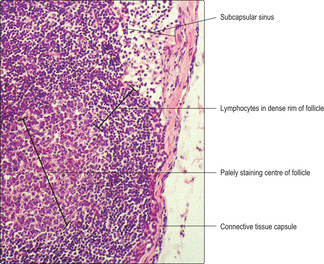
Cortex. Afferent lymph vessels deliver lymph into endothelium-lined sinuses which extend around each node immediately beneath the capsule (
Fig. 8.11). From these subcapsular sinuses some lymph continues in endothelium-lined sinuses through the cortex and medulla and some filters past lymphocytes in the cortex. Many of the lymphocytes in the cortex are in spherical aggregations forming lymphoid follicles which also contain antigen-presenting cells.
Lymphoid follicles which are inactive are composed mainly of small B lymphocytes which stain densely blue with haematoxylin. If B lymphocytes are responding to antigens the follicle has an outer rim of densely packed, small B lymphocytes and a central core of palely stained lymphocytes (
Fig. 8.11). Such follicles are described as secondary follicles (
Fig. 8.10) and the palely stained region is known as the germinal centre. New B lymphocytes are produced by mitosis in secondary follicles and become activated. Many activated B lymphocytes appear as medium- or large-sized lymphocytes and they have more cytoplasm than small lymphocytes. The cytoplasm of activated lymphocytes gives the palely stained appearance to the centre of secondary follicles. Activated B lymphocytes travel to the region between the cortex and the medulla (the paracortex) and interact with T lymphocytes. As a result, these B lymphocytes differentiate into plasma cells (
Fig. 8.6) and secrete specific antibodies. The antibodies leave the node in efferent lymph. ‘Memory’ B lymphocytes are also generated in germinal centres and these are involved in speedy specific responses to subsequent exposure to their ‘remembered’ antigen.
In the paracortex, lymphocytes are able to crawl out of blood in small veins and take part in the immune responses occurring in lymph nodes. This type of venule is characterised by being lined by cuboidal endothelial cells and is found only in lymph nodes.
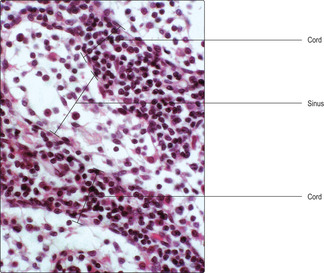
■
Medulla. The medulla of lymph nodes is composed of numerous endothelium-lined lymph vessels (sinuses) and medullary cords which are packed with immune cells (
Fig. 8.12), including plasma cells. Within the lymph in the sinuses are immune cells generated in the cortex and antibodies produced by plasma cells. Lymph, carrying many lymphocytes and antibodies, passes from the medullary sinuses to the efferent lymphatic vessel and is eventually returned to blood (
Chapter 10).

Clinical note
Metastasis This is the process by which tumour cells may become detached and spread from their original site to distant sites. One route by which they spread is via lymphatic vessels. Some tumour cells may enter lymphatic vessels and pass to lymph nodes draining the region where the tumour originated. They may remain in these lymph nodes and undergo further rounds of mitosis and initiate immune responses, and the nodes may swell. Some tumour cells may pass from the lymph nodes in efferent lymph and eventually pass around the body in blood and continue to proliferate and form metastases elsewhere. Screening lymph nodes for tumour cells helps to assess the spread of tumour cells, but once tumours have spread to lymph nodes such cancers are much more difficult to cure. (Tumours may also spread via veins (and/or directly) into adjacent tissues.)
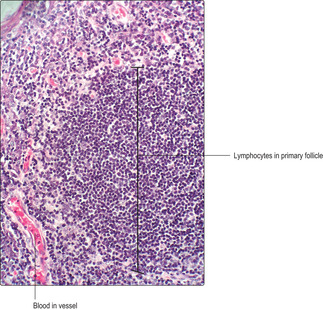
Non-encapsulated lymphoid tissue
Clusters of lymphocytes, not surrounded by a connective tissue capsule, are present in many regions of the body. They are particularly important features of the respiratory, digestive, urinary and reproductive tracts which are all lined by mucosae and vulnerable to foreign molecules and a variety of organisms. The clusters may resemble lymphoid follicles in lymph nodes and are known as mucosa-associated lymphoid tissue (MALT). If a cluster is not currently generating new lymphocytes, it is known as a primary follicle and is a mass of densely packed small B lymphocytes (Fig. 8.13). If lymphocytes in a cluster are responding to immune stimuli and generating new lymphocytes they have a palely stained centre typical of a secondary follicle (
Fig. 8.11).
Blood
■ Blood forms tissue fluid (extracellular fluid) and is able to clot and stop flow from damaged blood vessels.
Red blood cells (erythrocytes)
■ These are biconcave discs formed of cytoplasm and a cell membrane (but no nucleus) and are deformable:
■ the cytoplasm consists mainly of haemoglobin, which carries oxygen from the lungs to body tissues
■ red blood cells develop in bone marrow.
White blood cells (leucocytes)
Granulocytes:
■ have nuclei with two or more lobes and cytoplasmic granules
■ develop in bone marrow, circulate in blood and move into tissues
■ are categorised according to the staining characteristics of the granules:
■ neutrophils form 70% of the white cells in blood and phagocytose and kill bacteria
■ eosinophils form about 4% of the white cells in blood and ingest antigen–antibody complexes and kill and ingest parasites
■ basophils form about 1% of the white cells in blood and move into tissue and initiate inflammatory changes.
Agranulocytes:
■ have no (or very few) cytoplasmic granules and are categorised according to nuclear shape
■ lymphocytes have spherical nuclei and form about 25% of white blood cells:
■ B lymphocytes respond to antigens by secreting antibodies and T lymphocytes, respond to ‘foreign’ cells by killing them; NK cells kill ‘foreign’ cells
■ monocytes have indented nuclei and form about 5% of white blood cells
■ migrate from blood and become macrophages in tissues.
Platelets
■ These are small, membrane-bound fragments of cytoplasm that bud off from megakaryocytes in bone marrow. They aid blood clotting.
The immune system
■ The immune system defends the body from foreign molecules, cells and organisms.
■ It comprises a variety of cells (including white blood cells) in the thymus, spleen, lymph nodes and in mucosal surfaces exposed to the environment.
■ It mounts non-specific responses, e.g. phagocytosis by neutrophils, and specific responses, e.g. the humoral response of B lymphocytes and the cell-mediated response of T lymphocytes.
■ The immune system also involves mast cells, plasma cells, macrophages and dendritic cells.
Bone marrow
■ This comprises a meshwork of reticulin fibres supporting blood vessels and developing red and white blood cells and megakaryocytes which form platelets.
Thymus
■ This comprises a meshwork of epithelial cells supporting blood vessels and lymphocytes in an outer cortex densely packed with lymphocytes and an inner medulla where lymphocytes are less densely packed. Hassall’s corpuscles are present in the medulla.
■ It is particularly active in neonates and regresses with age.
■ Lymphocytes leave the thymus and enter the circulation as mature T lymphocytes which recognise self from non-self cells.
Spleen
■ This comprises a meshwork of reticulin fibres supporting blood vessels, red blood cells and lymphocytes and various antigen-presenting cells.
■ It has red and white pulp regions with sheaths of lymphocytes surrounding arterioles.
■ It monitors blood for foreign material and mounts immune responses and destroys aged red blood cells.
Lymphatic vessels and lymph nodes
■ Lymphatic vessels drain excess tissue fluid and return the fluid as lymph via lymph nodes to blood vessels.
■ Lymph nodes have an outer cortex and inner medulla region and receive lymph from numerous afferent lymph vessels.
■ In the cortex, spherical aggregations (follicles) of lymphocytes are numerous.
■ Lymph percolates through the cortex and lymphocytes may mount immune responses to foreign molecules or cells in lymph.
■ Lymph and cells then pass into the medulla where there are cords of immune cells, which may include plasma cells, and sinuses transporting the lymph.
■ A single efferent duct drains lymph from the medulla, and eventually all lymph drains into the cardiovascular circulation.
Histology An Illustrated Colour Text