CHAPTER 5 The black lung field
5.1 Chronic obstructive pulmonary disease (COPD)
When trying to decide the cause of bilateral black lungs you need to:
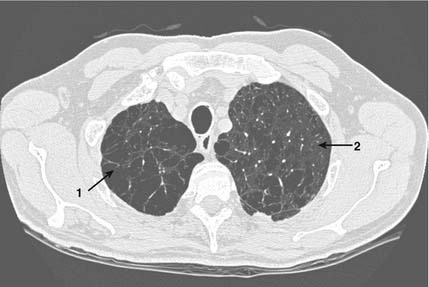
Cigarette smoking causes damage to the parenchyma of the lung. Cigarette smoke in a room tends to float upwards, and similarly smoking related lung damage tends to occur in the upper lungs. This image shows how the normal smooth lung texture has been destroyed with the formation of air cysts (bullae – 1) and small black holes in the lung (centrilobular emphysema – 2). The blood vessels through these areas can also become very narrowed, as the body will not perfuse areas of the lung where gas exchange is significantly impaired.
5.2 Pneumothorax
When you see a unilateral black lung you need to:
You must now decide the cause of the blackness. Lung markings are made up of bronchi and blood vessels and it is their absence that makes the lung look black. Vascular shadows will disappear if the lung is replaced by air, which will occur with a pneumothorax or bullous or cystic lung disease or if the vessels are deprived of blood as in a pulmonary embolus. Therefore think pneumothorax, bullae/cyst or pulmonary embolism and:
5.3 Tension pneumothorax
If you suspect a pneumothorax as a cause of a black lung field (see p. 110) you must consider carefully whether it may be under tension since this is a medical emergency.
5.4 Pulmonary embolus (PE)
 scanning
scanning
 scan, and may be better investigated by CTPA.
scan, and may be better investigated by CTPA.CT pulmonary angiogram
In order to interpret a spiral CT scan you need to:
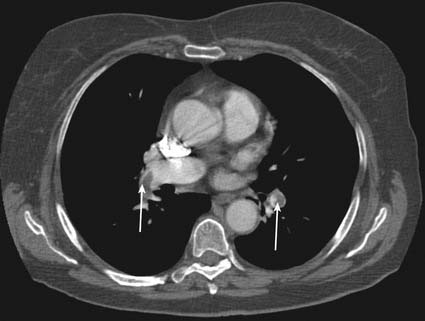
This patient became suddenly short of breath. CTPA showed a pulmonary embolism. Clots can be seen in both the right pulmonary artery and the left lower lobe pulmonary artery. (arrows)
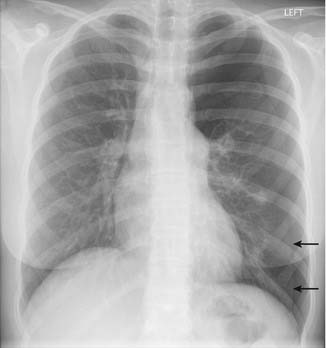
A plain film diagnosis of a pulmonary embolism is very rare.

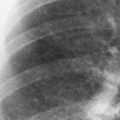
This X-ray is of a patient who has sustained an acute large pulmonary embolus. Look carefully at the right upper zone. Immediately above the horizontal fissure there is an area (1) which is blacker than the left side at the same level. This is Westermark’s sign of reduced perfusion to that area of lung which indicates that the artery to this area contains a large clot. Note also an area of consolidation below the horizontal fissure (2) – this is a small focus of infarction.
5.5 Mastectomy
A mastectomy will make the underlying lung look too black since there will be less soft tissue overlying the lungs on the affected side, compared to the normal side. Therefore, if one lung looks blacker than the other, look carefully for the breast shadows. There will be an absent breast shadow on the side of the mastectomy.





 ) scanning and CT pulmonary angiogram (CTPA).
) scanning and CT pulmonary angiogram (CTPA). scan is a nuclear medicine test. This uses small low-dose radioactive particles to compare the pattern of perfusion with that of ventilation. For the ventilation part of the test the particles are suspended in a gas, which is then inhaled, and stick to the walls of the airways to show airflow. For the perfusion part of the study the particles are injected intravenously and lodge in the very small blood vessels in the lungs. The distribution of radioactivity within the lung is then monitored using a gamma camera. Normally four views are taken (anterior, posterior, and right and left posterior oblique).
scan is a nuclear medicine test. This uses small low-dose radioactive particles to compare the pattern of perfusion with that of ventilation. For the ventilation part of the test the particles are suspended in a gas, which is then inhaled, and stick to the walls of the airways to show airflow. For the perfusion part of the study the particles are injected intravenously and lodge in the very small blood vessels in the lungs. The distribution of radioactivity within the lung is then monitored using a gamma camera. Normally four views are taken (anterior, posterior, and right and left posterior oblique). scan is therefore only of value in a patient with otherwise normal lungs.
scan is therefore only of value in a patient with otherwise normal lungs. scan does not give a definite diagnosis of pulmonary embolus (PE). Instead it gives you the probability of the patient having a PE. As such it must be interpreted alongside the clinical situation. A normal scan will virtually exclude a PE, certainly one of clinical significance.
scan does not give a definite diagnosis of pulmonary embolus (PE). Instead it gives you the probability of the patient having a PE. As such it must be interpreted alongside the clinical situation. A normal scan will virtually exclude a PE, certainly one of clinical significance. scan:
scan: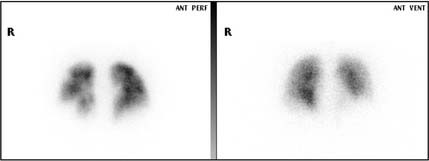
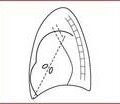
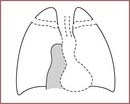
 scan in patient with pulmonary emboli. Note how the perfusion image is more patchy than the smoother texture of the ventilation scan.
scan in patient with pulmonary emboli. Note how the perfusion image is more patchy than the smoother texture of the ventilation scan. scan or ultrasound imaging of the peripheral veins to look for a deep vein thrombosis would be a reasonable alternative.
scan or ultrasound imaging of the peripheral veins to look for a deep vein thrombosis would be a reasonable alternative.