Chapter 27 The Assessment and Management of Posteromedial Instability
Introduction
The most common mechanism of elbow dislocation occurs from a fall on the outstretched arm resulting in a combination of compressive, external rotatory and valgus forces. This causes the forearm (radius and ulna) to supinate away from the humerus ultimately leading to joint dislocation. This is termed posterolateral rotatory instability (PLRI).1,2 A much less common, and more recently described, mechanism of elbow trauma results from applied internal rotation and varus force. In this case, the proximal forearm pronates relative to the humerus, termed posteromedial rotatory instability of the elbow (PMRI).2–4 The injury results in joint subluxation, not dislocation, and typically leads to a unique fracture of the anteromedial coronoid due to impaction from the humeral trochlea. The clinical presentation can be much more subtle than PLRI, and the coronoid fracture often appears small and innocuous on plain radiographs. Thus, the diagnosis of PMRI requires a high index of suspicion. It must be emphasized, however, that this is a true fracture–subluxation of the elbow which may lead to joint deterioration if not identified and properly managed.
Presentation, investigation and treatment options
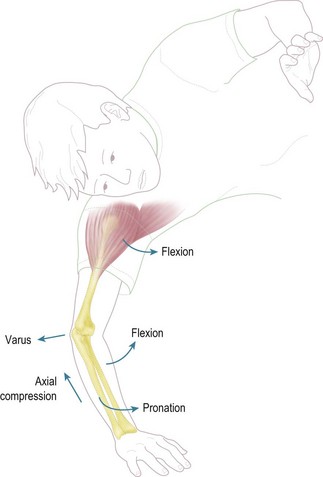
As noted, the mechanism of a posteromedial rotation injury to the elbow involves a fall in which the forearm pronates on the humerus. This is combined with axial compression and varus load (Fig. 27.1). Patients can present acutely after the trauma with a swollen and painful joint. When associated with larger coronoid fractures and greater force, radiographs can reveal obvious joint subluxation and incongruity. Three-dimensional computed tomography can allow a better appreciation of the bony injury as well as the rotatory mechanism (Fig. 27.2).
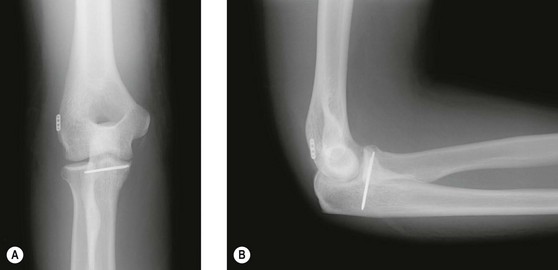
It is important to appreciate, however, that there is a spectrum of bony and soft tissue failure associated with these injuries. Patients can present acutely or in the subacute setting with a less significant history of injury, a less impressive examination (with limitation of only the end ranges of motion), and radiographs that appear quite innocuous only showing subtle evidence of a coronoid fracture (Fig. 27.3). This fracture is more vertically or obliquely oriented than the traditional transverse coronoid fracture.5 The extent of joint subluxation is hard to appreciate on frontal and lateral projections as the radiocapitellar relationship is preserved, i.e. there is no posterior translation of the radial head relative to the capitellum as seen in PLRI. In order to appreciate this injury pattern, the anteroposterior radiograph must be carefully evaluated for a double-density involving the coronoid along the medial joint line. This finding is characteristic of posteromedial rotatory injuries of the elbow. Again, three-dimensional computed tomography is very useful to identify the true extent of bony involvement and the joint subluxation (Fig. 27.3).
In addition to bony failure medially, the PMRI mechanism can also result in a soft tissue injury to the lateral ligamentous complex of the elbow. As the forearm pronates on the humerus and the medial ulnohumeral joint collapses and subluxates, the lateral joint is subjected to distraction forces. Thus, in almost all cases (an exception may be seen in the presence of an associated fracture of the coronoid at its base), there is an obligate failure of the lateral collateral ligament in tension (Fig. 27.3).2,3 This can be somewhat confusing, as this represents posterolateral joint instability (PLRI) in association with a posteromedial joint trauma (PMRI). However, recognition of lateral ligament disruption is important when addressing these injuries surgically.
Surgical techniques and rehabilitation
In order to surgically approach PMRI injuries, one must understand the anatomy of the coronoid. The proximal ulna has two main facets, the greater sigmoid notch, which articulates with the trochlea of the humerus, and the lesser sigmoid or radial notch, which forms the proximal radioulnar joint. The coronoid itself consists of an anterior projection and an anteromedial facet. The anteromedial facet is important for stability of the medial ulnohumeral joint. It also serves as an attachment for the anterior bundle of the medial collateral ligament, the primary stabilizer of the medial elbow (Fig. 27.4).6,7
The coronoid fracture that occurs with PMRI is commonly oblique and more vertical than that seen in PLRI and involves the anteromedial facet (Fig. 27.3). The fracture is best approached medially. This can be accomplished through a split in the flexor-pronator mass, which exposes the coronoid anteriorly. Alternatively, a more direct approach to the fracture line is through the floor of the cubital tunnel. With this method, dissection is carried out between the two heads of the flexor carpi ulnaris once the ulnar nerve is released and retracted posteriorly. Some motor branches to the anterior muscle will be sacrificed. Next, elevation of the humeral head of the flexor carpi ulnaris from distal to proximal off the ulna exposes the fracture from a medial perspective. This allows visualization of the joint surfaces and improves the ability to reduce the joint accurately (Fig. 27.5).
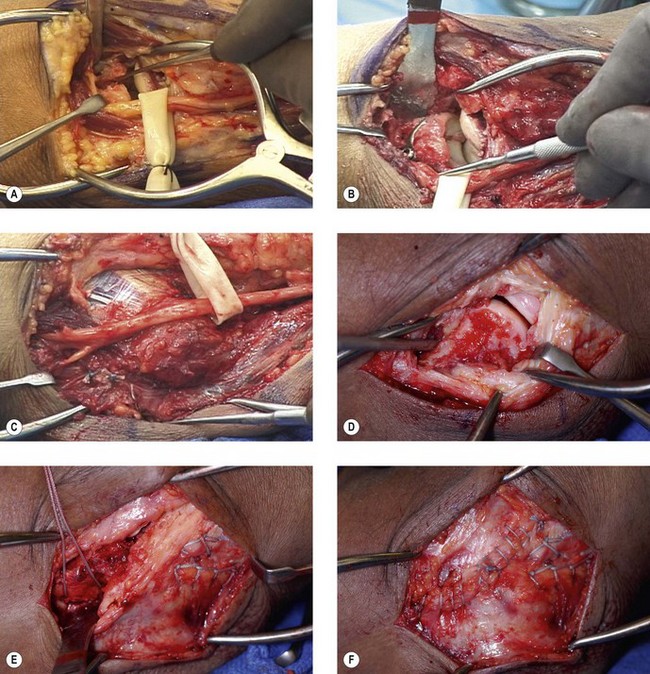
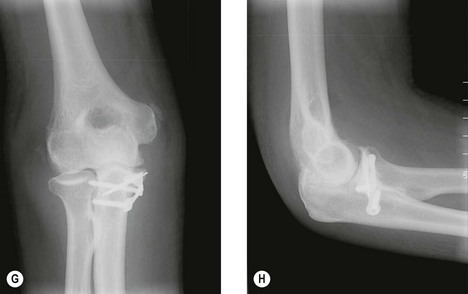
Figure 27.5 (A) Intraoperative view of the medial exposure of the fracture in Figure 3. The ulnar nerve has been dissected out and retracted posteriorly exposing the floor of the cubital tunnel. The flexor-pronator origin is not disturbed at the epicondyle. Note how this approach allows visualization of the medial joint line. The fracture fragment has been elevated anteriorly with an instrument. (B) Visualization of the coronoid and medial joint line following internal fixation. In this case, Kirschner wires were used followed by application of a precontoured buttress plate. Note the restoration of the articular surface of the ulna. (C) View following soft tissue repair and anterior transposition of the ulnar nerve into a subcutaneous position. (D) Lateral exposure revealing complete disruption of the soft tissues (lateral collateral ligament and extensor tendon origins) from the humeral epicondyle. (E) This lateral complex is being repaired by transosseus sutures placed through the isometric point and out the posterior column of the humerus. A running locking suture has been used for this purpose. (F) Final lateral repair. The longitudinal arthrotomy has been closed in addition to the transosseus sutures. This lateral repair protects the medial coronoid fixation as it does not allow the forearm to pronate on the humerus. (G) Postoperative anteroposterior and (H) lateral radiographs following surgical intervention. Note the restoration of the ulnohumeral joint on both the frontal and lateral projections. The double density of the coronoid is now absent.
(Figures copyright of Mark S. Cohen.)
Internal fixation of the coronoid fracture can be accomplished in several ways. One can use small screws if the fragment is large enough. Small plates can also be contoured and used in a buttress fashion. While there are small precontoured plates designed for this purpose (Fig. 27.5), they are no longer used in our practice as the dissection necessary to apply the screws distally can result in excessive retraction on the ulnar nerve. More recently, we have secured the coronoid fragment with simple threaded 0.062 inch Kirschner wires cut flush with the anteromedial cortex of the coronoid (Fig. 27.6). As will be discussed, the subsequent lateral soft tissue repair protects and neutralizes forces that would tend to displace this fragment, and thus a buttress plate is not essential.
Following medial osteosynthesis, the lateral soft tissue injury must be addressed. The lateral collateral ligament and part or all of the extensor tendon origin typically fail at the lateral epicondyle in distraction. Even if the superficial extensor fibres appear intact, there is a disruption of the tendon and ligament origins on the undersurface of this soft tissue sleeve (Fig. 27.5). This is appreciated once the overlying fascia is incised. Lateral joint stability is restored by repair of the lateral collateral ligament complex back to the humerus. This can be accomplished with bone anchors. However, we have found transosseus sutures to be more secure and effective in pulling the soft tissue back to bone. Care, however, must be taken to identify the isometric point of the humerus and the joint must be reduced when tying the sutures. It is not difficult to over-tighten the lateral side and gap the ulnohumeral joint medially during lateral repair.8 We have found placing the elbow across the body with the forearm in neutral rotation (using gravity assistance) with application of posteriorly applied pressure to the olecranon useful for this purpose. As noted previously, reconstitution of the lateral soft tissues protects the medial bony repair, as the forearm cannot pronate on the coronoid without concomitant gapping of the lateral joint.
Outcome including literature review
Stiffness of the elbow is much less common after a PMRI injury compared to the PLRI mechanism. This may be due to the more limited bony and soft-tissue injury associated with joint subluxation as opposed to the more severe fracture–dislocation which occurs with PLRI. There are few series that have reported solely on the outcome following PMRI. However, when the coronoid is properly reduced, normal motion and function are usually restored.9 This has also been our experience.
Complications of treatment
Due to the benign nature of the radiographs and the difficulty identifying the fracture on plain films, it is not uncommon for patients to be treated conservatively and present late after the injury with pain and loss of terminal elbow motion. Unfortunately, the prognosis for untreated injuries is less good due to joint incongruity and the development of posttraumatic arthrosis (Fig. 27.7).
In those injuries treated surgically, less satisfactory results occur if the coronoid fracture is not adequately addressed.9 Reduction of the medial fragment is required to ensure a concentric ulnohumeral joint. An additional postsurgical complication is ulnar neuropathy. This is most likely related to excessive handling of the ulnar nerve during exposure of the medial coronoid. We have found this complication to be more of a problem when precontoured plates are used as a buttress. These plates have medial to laterally directed screws distally that may require excessive traction on the ulnar nerve intraoperatively.
Finally, as with all significant injuries to the elbow, heterotopic ossification can occur.10,11 To avoid this, at our institution, heterotopic ossification prophylaxis is utilized in most cases with an oral non-steroidal antiinflammatory medication prescribed for approximately 2 weeks. In high-risk cases, such as those associated with a closed head injury, repeated surgical insult or with a delay in surgical treatment, consideration is given to low-dose external beam radiation. This can be administered as a single dose of 600–700 cGy with limited field technique to decrease soft tissue exposure.10 As with oral medication, radiation should be administered within 3–4 days to be effective.
1 Cohen MS, Hastings H. Acute elbow dislocation: evaluation and management. J Am Acad Orthop Surg. 1998;6:15-23.
2 O’Driscoll SW, Jupiter JB, Cohen MS, et al. Difficult elbow fractures: pearls and pitfalls. In: Ferlic DC, editor. Instructional Course Lectures. Rosement: American Academy of Orthopaedic Surgeons; 2003:113-136. 52
3 Cohen MS. Fractures of the coronoid process. Hand Clin. 2004;20:433-453.
4 Sanchez-Sotelo J, O’Driscoll W, Morrey BF. Medial oblique compression fracture of the coronoid process of the ulna. J Shoulder Elbow Surg. 2005;14:60-64.
5 Regan W, Morrey B. Fractures of the coronoid process of the ulna. J Bone Joint Surg (Am). 1989;71:1348-1354.
6 Cohen MS, Bruno RJ. The collateral ligaments of the elbow: anatomy and clinical correlation. Clin Orthop. 2001;383:123-130.
7 Cage DJ, Abrams RA, Callahan JJ, et al. Soft-tissue attachments of the ulnar coronoid process. Clin Orthop. 1995;320:154-158.
8 Fraser GS, Pichora JE, Ferreira LM, et al. Lateral collateral ligament repair restores the initial varus stability of the elbow: an in-vitro biomechanical study. J Orthop Trauma. 2008;22:615-623.
9 Doornberg JN, Ring DC. Fracture of the anteromedial facet of the coronoid process. J Bone Joint Surg (Am). 2006;88(10):2216-2224.
10 Cohen MS. Heterotopic ossification of the elbow. In: Jupiter JB, editor. The Stiff Elbow. Rosemont: American Academy of Orthopaedic Surgeons; 2006:31-40.
11 Jupiter JB, O’Driscoll SW, Cohen MS. The assessment and management of the stiff elbow. In: Ferlic DC, editor. Instructional Course Lectures. Rosemont: American Academy of Orthopaedic Surgeons; 2003:93-112. 52