CHAPTER 32 Testicular Torsion
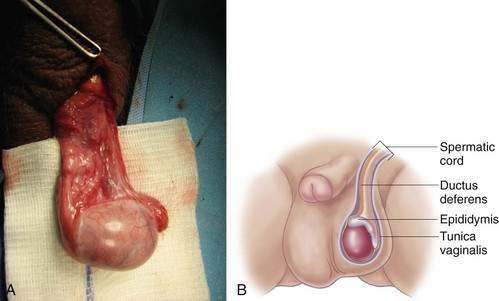
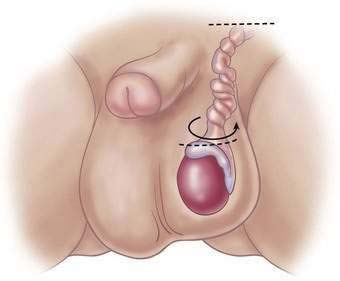
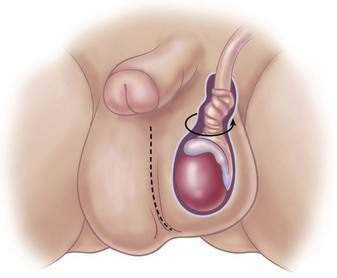
Step 1: Surgical Anatomy
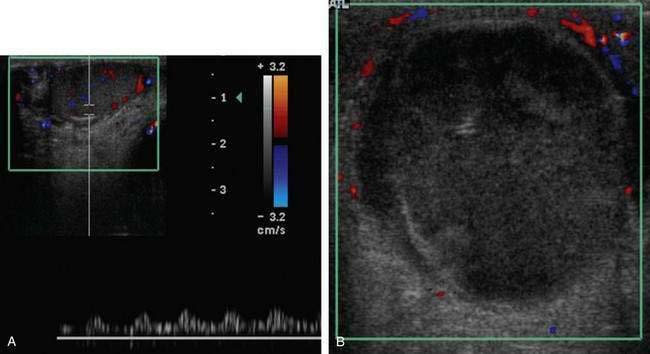
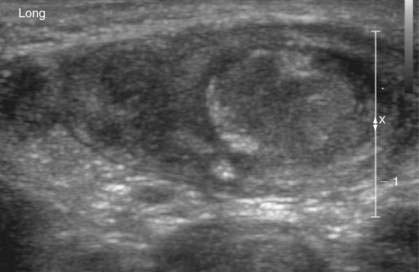
Step 2: Preoperative Considerations
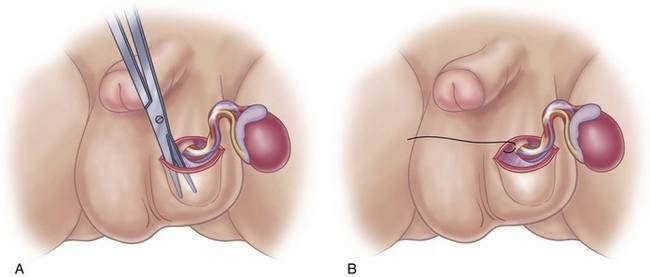
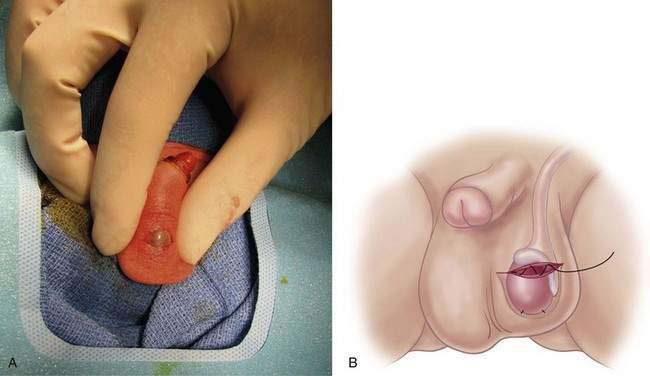
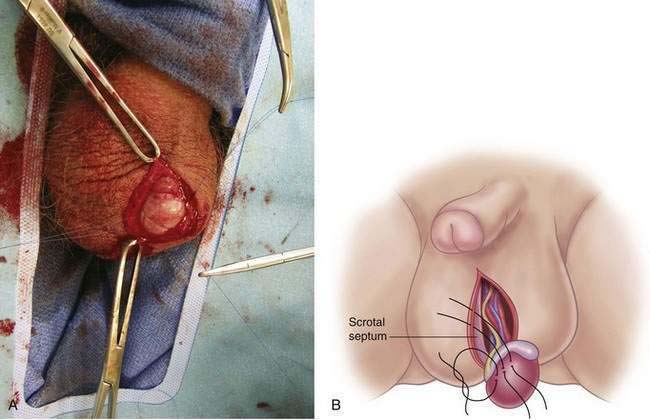
Step 3: Operative Steps
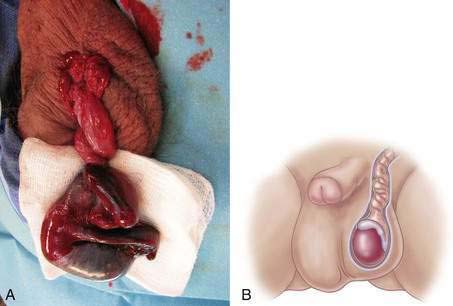
Neonatal Torsion
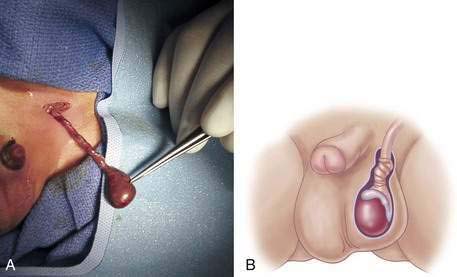
Non-neonatal Torsion
Step 4: Postoperative Care
Baker LA, Sigman D, Mathews RI, et al. An analysis of clinical outcomes using color Doppler testicular ultrasound for testicular torsion. Pediatrics. 2000;105(3 Pt 1):604-607.
Gatti JM, Murphy JP. Current management of the acute scrotum. Semin Pediatr Surg. 2007;16(1):58-63.
Hutson J. Undescended testis, torsion and varicocele. In: Grosfeld JL, Coran G, et al, editors. Pediatric surgery. Philadelphia: Mosby Elsevier; 2006:1193-1214.
Kiesling VJJr, Schroeder DE, Pauljev P, et al. Spermatic cord block and manual reduction: primary treatment for spermatic cord torsion. J Urol. 1984;132(5):921-923.
Mor Y, Pinthus JH, Nadu A, et al. Testicular fixation following torsion of the spermatic cord—does it guarantee prevention of recurrent torsion events? J Urol. 2006;175(1):171-173. discussion 173-174
Murphy J. The acute scrotum. In: Ziegler NM, Weber TR, et al, editors. Operative pediatric surgery. New York: McGraw-Hill; 2003:563-567.