CHAPTER 44 Tennis Elbow Tendinosis
INTRODUCTION
Tennis elbow is a common term used to describe what was originally introduced as lawn tennis arm in 1883.39 Over the years, it has been used to describe a variety of maladies that occur in and about the elbow.6,10,12,13,19,66 The accurate diagnosis of this entity requires a thorough understanding of the epidemiology and clinical presentation as well as the pathophysiology of this condition. The traditional terms tendinitis and epicondylitis do not accurately reflect the true pathology of this condition. On the basis of clinical and surgical experience,16,25,37,50,51 it can be stated with confidence that the pathology of classic tennis elbow resides primarily in tendon tissue. Associated intra-articular issues such as synovial plica or capsular defects or degeneration, may be noted in a small percentage of patients. Therefore, rather than being inflammatory the demonstrated changes are degenerative (E. R. Stay, personal communication).34,37,63 The absence of inflammatory cells and findings of dysfunctional vascular and fibrous elements with total distortion of collagen has prompted us to describe this pathology as angiofibroblastic tendinosis.34,35,37
INCIDENCE
Lateral tendinosis typically affects approximately 2% of the general population. The dominant arm is affected in more than half of the patients. The peak incidence of this condition is during the fourth and fifth decades of life. A random study of 200 tennis players in three tennis clubs revealed that half of the players older than 30 years of age had experienced symptoms of characteristic tennis elbow at one time or another.47,50 Of this group, half noted minor symptoms with a duration of less than 6 months, and the rest had had major symptoms with an average duration of 2½ years. A larger statistical analysis of 2500 patients performed by Priest at the Vic Braden Tennis Camps revealed similar data.61,62 A study performed by Gruchow and Pelletier29 correlated playing time with the incidence of tennis elbow in club players. Not restricted to tennis and racquet sports, the incidence of the malady varies among other sports and oc-cupations that require repetitive forearm and wrist movements, including baseball, fencing, and swimming. Stressful repetitive uses of the forearm, such as computer keyboard use, carpentry, plumbing, meat cutting, textile production, and constant handshaking (e.g., politicians) are occupations related to the occurrence of tennis elbow.
CLASSIFICATION
Elbow tendinosis may be simply classified on an anatomic basis.
Medial Elbow Tendinosis (Golfer’s Elbow)
An additional complicating factor associated with medial elbow tendinosis is ulnar nerve compression neuropraxia (cubital tunnel syndrome). This phenomenon is evident in approximately 30% of all cases51–53 (see Chapter 45).
ASSOCIATED ABNORMALITIES AND DIFFERENTIAL DIAGNOSIS
Ulnar Nerve Neuropraxia (Cubital Tunnel Syndrome)
Ulnar nerve neuropraxia is commonly as-sociated with medial elbow tendinosis and is of special note because it has an impact on the prognosis51–53 (see Chapter 45).
Carpal Tunnel Syndrome
Approximately 10% of elbow tendinosis patients may also have signs and symptoms of carpal tunnel syndrome.46,51–53
Mesenchymal Syndrome
The association of carpal tunnel syndrome and trigger finger, as well as the association of rotator cuff tendinosis, bilateral elbow tendinosis and cubital tunnel syndrome, has led me (R. N.) to the conclusion that a constitutional factor may play a significant role in certain patients with elbow tendinosis.46,51,53 This combination of pathology has been coined mesenchymal syndrome (R. P. Nirschl, unpublished data).
Radial Nerve Entrapment
Entrapment of the motor branch of the radial nerve in the radial tunnel at the canal of Froshe (posterior interosseus nerve) may coexist with and can cause symptoms similar to those seen with lateral elbow tendinosis. Diagnosis is confirmed by findings of electromyographic abnormality. Roles and Maudsley64 reported a surgical experience with 33 cases in 1972. In the Roles report, specific care was taken to decompress the radial tunnel by releasing the origin of the extensor carpi radialis brevis. Thus, the success of the reported operation may be due to an alteration of the origin of the extensor brevis rather than decompression of the nerve. Entrapment of the posterior interosseous nerve has also been implicated as the cause of lateral elbow pain by Werner,77 Dobyns (personal communication), and others (see Chapter 46). Entrapment of the radial nerve proximal to the sensory-motor bifurcation of the radial tunnel syndrome has also been described. A random sample of 20 electromyographic studies in patients with the classic signs of clinical lateral tennis elbow and suggested radial tunnel symptoms, however, failed to reveal any radial nerve abnormality (R. P. Nirschl, unpublished data). In most instances, if posterior interosseus nerve entrapment does occur, it is not associated in a major statistical way with classic lateral tennis elbow. In his classic study, Werner77 did report that the two coexist in about 5% of patients. When, on occasion, entrapment of the posterior interosseous nerve does occur, it may present as an entirely separate entity with vague aching symptoms that are more diffuse and felt more distally over the extensor muscle mass, tenderness in the same more distal forearm area, and a provocative handshake stress test that elicits symptoms in resisted supination. Most commonly, electromyographic studies tend to be normal in both radial tunnel syndrome and posterior interosseus nerve entrapment, thereby clouding the opportunity for objective laboratory diagnostic clarity.
Rotator Cuff Tendinosis
As noted earlier, multiple areas of tendinosis often occur in association with tennis elbow.46,51,53 As noted earlier, the term mesenchymal syndrome has been employed to identify this subset of patients.46 It is the author’s clinical hypothesis, that this entity is hereditarily based and probably represents a slight collagen distortion—perhaps cross-linkage—as it relates to tendons. The practical ramifications of this entity include the necessity of rehabilitative exercise dedicated to the shoulder as well as the elbow when one formulates a treatment plan.
Cervical Osteoarthritis and Nerve Root Compression
Gunn and Milbrandt30 have reported pain relief in 53 cases of tennis elbow by directing treatment to osteoarthritis of the cervical spine. Because the greatest incidence of tennis elbow occurs in individuals in the fourth and fifth decades of life, coincidental cervical osteoarthritis is common. Because the findings of lateral tennis elbow are usually specific, including response to local elbow tendon injections, it is unlikely that osteoarthritis in the cervical spine is anything but a coincidental finding. The report, however, reinforces the concept that shoulder and neck problems often occur in combination and must be addressed by rehabilitation.
Intra-articular Abnormalities and Joint Laxity
Individuals who use the arm with high torque and shearing forces, as in the aggressive activities of baseball or javelin throwing, are vulnerable to associated intra-articular problems. These generally take the form of synovitis, traumatic osteoarthritis,45 and osteocartilaginous loose bodies present in the lateral or, more rarely, medial elbow compartments, as well as in the posterior olecranon fossa when associated with ligamentous laxity of the medial ulnar collateral ligamentous structures. Ulnar nerve neuropathy (cubital tunnel syndrome) commonly complicates the medial tendinosis clinical picture. Appropriate history, physical, and imaging examinations identify this subset of patients, and treatment should be adjusted accordingly. In a review, Baker and Cummings1 demonstrated that in some, there is arthroscopic evidence of capsular degeneration and synovial plica coexists with degeneration of the extensor carpi radialis brevis.1 In a review of his arthroscopic findings, Cummins16 reported a low incidence of intra-articular pathology, and this report is consistent with my observation (e.g., less than 5%).16 Nonetheless, the intra-articular component does exist.
ETIOLOGY
Age and Sex
The characteristic age at onset of classic uncomplicated tennis elbow is between 35 and 50 years, with a median of 41 years.47,61 Although the condition is most common in the third, fourth, and fifth decades, tennis elbow occurs in patients as young as 12 and as old as 80 years. Depending on a given patient population, the overall male-to-female ratio is usually equal.
Overuse
Lateral tennis elbow is directly related to activities that increase tension loads, and hence the stress, of the wrist and finger extensors and, possibly, the supinator muscles. Funk and associates22 revealed that the extensor carpi radialis brevis is active with flexion, extension, varus, and valgus stress, hence, supporting the notion of overuse or overexertion of this anatomic structure.
Traumatic Etiology
Repetitive overuse is clearly associated with the development of tennis elbow.50,61,62 A typical sports patient is an active recreational tennis player who plays at least three or four times per week.6,61,62 Less commonly, acute onset may be associated with a direct blow to one of the epicondylar areas or a sudden extreme effort or activity.
PATHOLOGY
GROSS ABNORMALITIES
Before 1964, defined pathoanatomy was not known precisely. In 1922 Osgood,57 and in 1932 Carp,13 related the condition to radiohumeral bursitis. Goldie,25 in his classic 1964 report, was the first to describe pathology adjacent to the lateral elbow. Goldie used longitudinal incisions and binocular magnification for more thorough assessment of the tissues.25 Before Goldie’s report, previous release techniques described by Bosworth8 and Hohmann31 failed to observe specific pathologic tendon abnormalities.
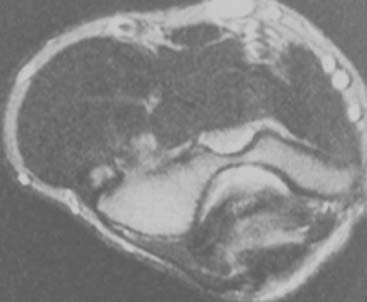
Careful gross surgical inspection of the abnormal tendinosis specimen reveals a characteristically grayish color and homogeneous and generally edematous tissue (Fig. 44-1). This typical gross pathologic appearance is present in lateral, medial, and posterior tendinosis. Indeed, similar visual characteristics are present in tendinosis involving the rotator cuff, and patellar and Achilles tendons, and even in plantar fasciosis (fasciitis). In my original surgical series of lateral tennis elbow, 97% of cases demonstrated varying degrees of this pathologic tissue at the origin of the extensor brevis tendon (which was ruptured in some degree in 35%).53 Observations in these and subsequent surgical cases also revealed that approximately 50% of cases also had associated tendinosis changes in the anteromedial edge of the extensor digitorum communis or extensor aponeurosis (usually 10% to 20% of the volume of the extensor digitorum communis tendon).51–53 Radiographic examination revealed that 22% of patients had some form of bony exostosis at the tip of the lateral epicondyle.51–53 Soft calcification in the substance of the tendon can also occur, but this finding is rare. Today, in some cases, the use of magnetic resonance imaging (MRI) may be helpful in demonstrating pathology at the lateral epicondyle. In the editor’s (B. F. M.) experience, this image is very rarely indicated to diagnose epicondylitis (Fig. 44-2).
MICROSCOPIC PATHOLOGY
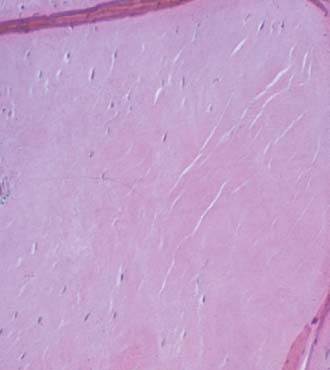
An understanding of the dense connective tissue that makes up the fibrous portion of the tendon is necessary for a better appreciation and definition of the pathologic process that is present in tennis elbow (E. R. Stay, personal communication). In tendons, collagen fibers and primary tendon bundles run parallel courses. In normal tendons, nerves and blood vessels extend through the major connective tissue septa but do not invade the fascicles (E. R. Stay, personal communication).67 On gross examination, the tendon appears firm, taut, and yellowish white or beige.51,53,54
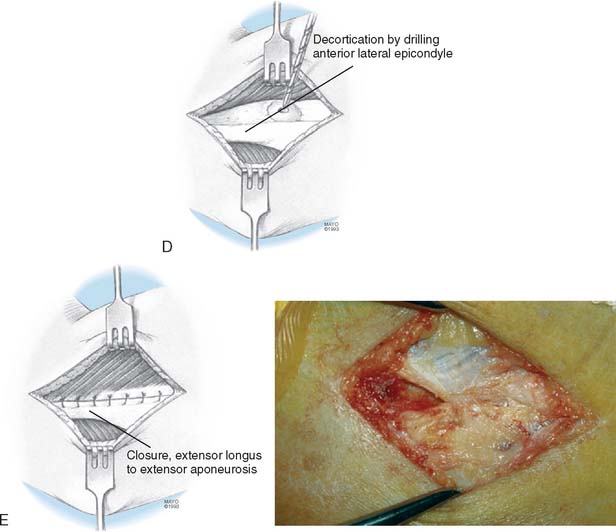
In tendinosis, the abnormal tissue ordinarily can be identified easily by its appearance and is distinct from the normal tendon. Visual examination usually reveals gray, dull, sometimes edematous and friable, immature-appearing tissue that grossly resembles firm granulation tissue.51,53,54 Microscopically, the normal orderly tendon fibers are disrupted by a characteristic invasion of fibroblasts and vascular granulation-like tissue, which may be described as an angiofibroblastic hyperplasia-tendinosis34,37,50,51,54,67 (Fig. 44-3). Adjacent to this early proliferating vascular reparative tissue, the tendon appears hypercellular, degenerative, and microfragmented. The degree of angiofibroblastic infiltration appears to correlate generally with the duration of symptoms.47,50,53 In advanced lesions, adipose, connective, and even musculoskeletal tissue can reveal infiltration by this pathologic proliferative tissue.37
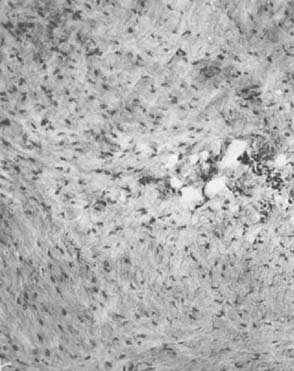
Others have noted the neovascular channels but emphasized that the mesenchymal cell proliferation indicated that the appearance was one of a healing process.67 On the other hand, Regan and colleagues63 compared 12 patients having surgery for lateral epicondylitis with 12 control patients. The unequivocal changes of hyaline degeneration were interpreted as demonstrating that the basic pathologic lesion was one of degeneration, although the increased vascularity noted by others also was reported. These investigators emphasized the fact that there is no microscopic evidence of inflammation associated with tennis elbow (Fig. 44-4).63 Evidence of acute or chronic inflammation is virtually absent in all cases.
In cases treated with corticosteroid injection, non-polarizable amorphous eosinophilic material can be identified, often without any foreign body response and usually without evidence of calcification (Fig. 44-5). Indeed, the proliferating vascular reparative tissue often insinuates itself between normal and abnormal tissues in regions close to the injection site.67
IMMUNOHISTOLOGY AND ELECTRON MICROSCOPY OF TENDINOSIS
In 1999, Kraushaar and Nirschl37 reported a study of the histology, immunohistochemistry, and electron microscopy of tennis elbow tendinosis in nine surgical resection specimens. The origin of the extensor carpi radialis brevis was compared with 10 cadaveric specimens of the same anatomic region. These studies revealed that myofibroblasts are present in tendinosis material, a cell type with contractive properties not usually found in healthy tendons. Tendinosis material, therefore, contains hyperplasia of nonfunctional vascular elements, active distorted fibroblasts, and a lack of lymphocyte or neutrophilic populations that is clearly distinct from inflammatory tendinitis and/or normal tendon.37 This study reinforces the prior original hematoxylin and eosin (H&E) stain microscopic observations that “tendinosis” or degeneration is the histopathologic lesion in tendon overuse.51,54,67
WHAT CAUSES THE PAIN?
We have pondered this question for a matter of years. The initial presumption of causation was that of regional anoxia with a production of noxious chemicals (e.g., soft tissue avascular necrosis). Khan and Cook34,35 have agreed that the histopathology is devoid of inflammatory cells and have suggested that noxious agents including chemical mediators, matrix substances and disrupted collagen may stimulate nociceptors. Voloshin and associates73 have advanced a similar suggestion concerning rotator cuff and bursal pain. Tasto and colleagues,71 in preliminary basic science investigations, report the possibility of free nerve endings, as noted by the identification of immunohistologic markers for nerve. However, the identification of free nerve endings themselves has not been supported by our electron microscopy evaluations.37 The work of Lian and associates38 on patellar tendinopathy identifies the ingrowth of substance P fibers with the presumption that this may play a nociceptive role.
CLINICAL CORRELATIONS OF PATHOLOGY
The area of maximal tenderness in lateral elbow tendinosis typically lies 5 mm distal and anterior to the midpoint of the lateral epicondyle (e.g., the pathoanatomy typically is not at the epicondyle). Provocative stress testing consists of resisted wrist and finger extension with the elbow in flexion with marked accentuation as the elbow is brought into extension (Fig. 44-6). Increased pain with extension is common even with mild tendinosis. When provocative tests are positive in flexion, the need for surgical intervention is more likely in our experience.
The following tendinosis pathologic categories, with corresponding clinical and therapeutic implications, are speculated.51
CATEGORY I
NONSURGICAL TREATMENT
The general concepts of elbow rehabilitation are covered in detail in Chapter 9. A brief overview, however, is appropriate at this time.48–5055 The patient with elbow tendinosis most commonly presents for evaluation and treatment because of pain, rather than impairment of mechanical function. Therefore, it is important to control pain, but this, in itself, does not necessarily imply enhancement of healing. The time-honored modalities of relative rest (not absence of activity but abstinence from abuse) and application of cold are appropriate. Activity that aggravates the condition should be eliminated. The use of aspirin as an anti-inflammatory agent is the first choice, but nonsteroidal anti-inflammatory medications, including ibuprofen, and naproxyn, seem to be helpful in some patients. The relief offered by the topical medication dimethyl sulfoxide (DMSO) was no greater than that of a placebo.59 The physical therapy modality of high-voltage electrical stimulation has been helpful in relieving pain, and the author’s anecdotal observations suggest the possibility of enhancing a biologic healing response.48,51,55 Paoloni and associates have suggested that nitric oxide patches aid in pain control.58
If the malady does not respond to an appropiate pain control program and the patient is incapable of performing the prescribed rehabilitative exercises, a cortisone injection may be indicated.14 The senior author uses 2.5 mL of 0.5% lidocaine (Xylocaine) mixed with 20 mg of triamcinolone, instilled under the extensor brevis just anterior and slightly distal to the lateral epicondyle into a triangular fatty recess that occupies this area. If the injection is too superficial (e.g., above the extensor carpi radialis brevis at the epicondyle) or is done on a repetitive basis, subdermal atrophy may occur.48,72 The repeated use of cortisone injections (more than a total of three) is inappropriate and harmful with the potential for tenocyte cellular death and weakening of the surrounding normal tissues.72 Indeed, some patients are extremely sensitive to local instillation of cortisone; subcutaneous atrophy (Fig. 44-7), occasionally after only one injection, may be noted, especially when the injection is placed superficial to the tendon. Therefore, we recommend that no more than three injections should be instilled in any one area. In addition to superficial or direct injections, intratendinous injections should be avoided.2,50–52,72
PROMOTION OF HEALING
A biologic healing response includes infiltration of healthy neovascular and fibroblastic elements, collagen production, and collagen maturation at the cellular level in addition to the restoration of strength, endurance, and flexibility to the entire extremity, including the upper back, neck, and shoulder. The healing process may be hastened by three general measures: relative rest, high-voltage electrical stimulation, and most importantly, rehabilitation exercises.48,49,55
Relative Rest
Alteration of Training Technique
Careful history taking and observation are fundamental to the identification of faulty activity technique. Evidence is accumulating that the correct technique of a sport or occupation not only enhances activity performance but also is less likely to cause injury.48–5055 The sports most likely to be causally related to either lateral or medial tennis elbow include tennis, golf, baseball throwing, squash, racquetball, weightlifting, fly and cast fishing, swimming, and track and field events. The commonly associated occupational activities include meat cutting and handling, carpentry, plumbing, repetitive assembly line activity, computer keyboard and mouse activity, typing, writing, and handshaking (e.g., politicians at campaign time).48,50,55
Alteration of Equipment
Equipment (especially in construction occupations and the racquet sports) may play an important role in imparting forces that can result in tendon overuse injury.6,29,47,48,50,51,55 Biomechanically, in tennis as well as other implement ball sports it is most appropriate to strike the ball at the center of percussion (“sweet spot”) because the increased torsion of off-center hits increases the stresses on musculotendon units, especially at or near the tendon epicondylar attachment areas.6,27,46,47,61,62
Activities that cause forearm impact or stress necessitate equipment of the proper size, weight, balance, and grip to avoid excessive forces.6,27,48 In general, the larger the handle of the device, the greater the leverage for torsion control, but the handle size should be matched to hand size.6,48,50,55 The distance from the midpalmar crease to the ring finger is a helpful aid in selecting the proper handle size48,50–52 (Fig. 44-8).
Finally, the weight, dimension, and flexibility of the equipment should match the available strength of the individual. It is better to use a device that is somewhat lighter to ensure proper positioning of the equipment at the time of impact.6,50 In racquet equipment, however, adequate mass is important to absorb the torsion of off-centered ball impacts.
Counterforce Bracing
The concepts of functional elbow bracing for tennis elbow were initially introduced by Ilfeld and Field in 1965,32 and by Froimson in 1971.20 The term counterforce, introduced by the senior author (R. P. N.) in 1973,47 describes a wide nonelastic support curved for better fit and support of the conical shape of the forearm.48,51,52,55 Simply stated, the counterforce concept supplements tendon origin and constrains full muscular expansion, thereby decreasing intrinsic muscular force to sensitive or vulnerable areas—namely, the forearm extensors for lateral tennis elbow and the forearm flexors for medial tennis elbow (Fig. 44-9). Studies have shown objective improvement in wrist extension and grip strength or positive biomechanical effects with elbow bracing.20,27,32,75 In medial tennis elbow, an additional support just distal to the medial epicondyle is sometimes helpful.48,50,51
As noted previously, rigid types of immobilization at the elbow or wrist relieve pain, but at the price of atrophy and immobility, and thus are not recommended.
High-Voltage Electrical Stimulation
High-voltage electrical stimulation in the treatment of both acute and chronic tendinosis is an accepted treatment modality.3,4 In the author’s experience, this modality diminishes pain (presumed chemical inflammation) and may promote healing. Our standard practice for tendinosis is to employ four to six sessions of high-voltage electrical stimulation during a 2- to 3-week period.48,53,55
Rehabilitative Exercise Program
This topic is discussed in detail in Chapter 9. It is important to emphasize, again, that rehabilitation should include not only the cardinal forearm exercises but also those for the upper back and shoulder.48,49,55 Once the probable initial adjacent inflammatory response and the pain have been controlled, an orderly progression of the graduated strength and endurance exercise is started.28,48,55 The patient is protected until about 60% of the rehabilitation exercise goals.44,48,51,53
Graduated Exercise and Full-Strength Training
Continuation of the strength and endurance exercise program beyond the preinjury level includes either isokinetic or isotonic, interspaced with isoflex exercises.28,48 Before a final return to a sport or an occupational activity, the patient should be capable of anaerobic sprint repetitions to fatigue without major activity pain.28,48,55
ALTERNATIVE NONOPERATIVE APPROACHES
Recent reports have suggested that pain control and possibly biologic alteration of tendinosis tissue may be achieved by other approaches. These include shock-wave, various forms of prolotherapy injections (autologous blood, platelets, and dilute sugar), cold laser, nitric oxide patches, magnetic and high intensity infrared heat,4 and acupuncture. Of this group, shock-wave, nitric oxide patches, and autologous injections have the most research support, but success has been inconsistent and further research is indicated.58,65,69,76
SURGICAL TREATMENT
HISTORICAL REVIEW
The popular literature concerning the surgical treatment of tennis elbow is considered to have begun in 1927 with Hohmann,31 who described release of the extensor aponeurosis at the level of the lateral epicondyle. The technique, now commonly referred to as a muscle slide or release procedure,5,8 does not identify the offending pathology.5,8–10,13,68
In 1936, Cyriax17 was the first to correctly identify by intuitive means the origin of the extensor carpi radialis brevis as the major site of pathology. For treatment, Cyriax theorized that the extensor brevis origin was often partially torn, and reported treatment by closed manipulation of passive forceful elbow extension and forearm supination, thereby converting a partial tear to a complete tear, and thus inciting an active biologic healing response while relieving tension overuse.
Wadsworth74 described a similar approach in 1972 with approximately a 50% success rate and with an audible or palpable snap or popping associated with the maneuver.
In 1955, Bosworth8 reported a series of 27 elbows, in which four different techniques were used. He suggested that his third technique, which included a release of the extensor aponeurosis as well as the orbicular ligament in and about the radial head in four patients, was seemingly curative. Curiously, Bosworth8 performed the Hohmann-type release operation in 17 instances, but “all” still had some complaints. In addition to the concepts of tendon release as advanced by Hohmann and Bosworth, a companion intervention of resection of a portion of the lateral epicondyle has been undertaken by some authors.23,41,57,60 This approach undoubtedly was based on the erroneous premise that the pathology was an inflammation of the lateral epicondyle.
In a fascinating application of the conviction that the origin of the extensor carpi radialis brevis was the source of pathology, Garden23 reported 50 instances in which the extensor brevis tendon was lengthened in the distal forearm. He concluded, as had others,15,70 that active muscular contraction with tendon tensioning of the extensor carpi radialis brevis, causes pain. In 44 cases treated with open Z-plasty lengthening at the extensor carpi radialis brevis musculotendinous junction, Garden noted that full pain relief at the elbow was obtained in all cases. However, in 20 cases (40%) strength had not returned to normal, and pain was noted at the distal surgical site in some cases.
SURGICAL OPTIONS
As noted earlier, historical open-surgical options have focused predominantly on the release of the extensor aponeurosis, as originally proposed by Hohmann. More recent versions of this approach have included percutaneous release.5,68,79 The reports to date are short-term follow-ups but do suggest that this approach can be effective in as many as 90% or more of patients and has a relatively low complication rate.5,68,79 As an adjunct to the surgical release of the common extensor tendon, Cabot11 also recommends the release of the anterior capsule for patients who have a flexion contracture. He indicates an 87% success rate among the 47 cases so treated. In my observation, elbow adhesive capsulitis is rare with the classic tennis elbow.
Several surgical options are available besides release of the extensor aponeurosis from the lateral epicondyle. In 1964, Goldie25 presented a comprehensive thesis of 49 patients that for the first time detailed pathologic changes in the subtendinous tissue in the lateral epicondyle. He described tendinous tissue invading fibroblastic cells, as well as vascular infiltrates.
Kaplan36 reported three cases of resection of the radial nerve branches to the lateral epicondyle and lateral articular areas, with no attempt to identify or remove pathologic tendon tissues. He noted excellent pain relief, but denervation of a motor branch to the extensor brevis probably occurred with this technique. Interestingly, his three patients were hospitalized postoperatively for an average of 7 days. Roles and Maudsley64 described 33 patients who responded to surgical decompression of the posterior interosseus nerve and release of the brevis tendon. The surgery was performed by 11 different surgeons over a 10-year period. Posterior interosseous nerve compression continues to be recognized as an entity, with recent reports emphasizing the association of compression of the nerve at the arcade of Frohse.12,33 In one study, 5% of patients were noted to have posterior interosseus nerve entrapment in association with tendinosis.77 In my observation, true posterior interosseous nerve compression syndrome is uncommon in association with lateral elbow tendinosis.
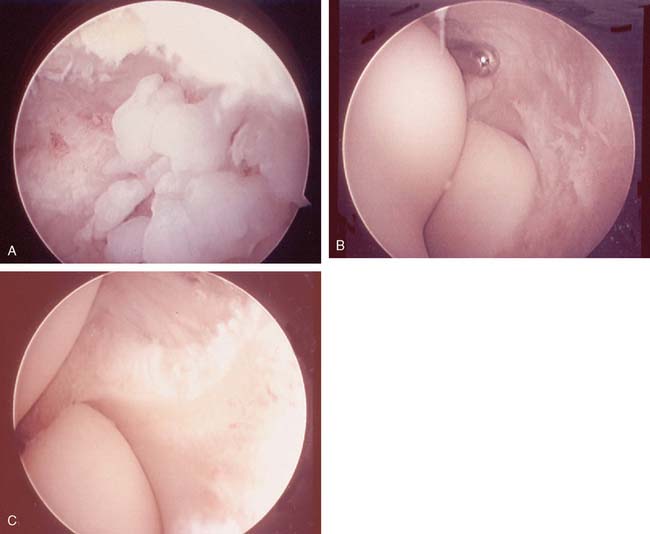
More recently, Tasto71 has introduced radiofrequency ablation of tendinosis pathologic tissue and Baker and Cummings1 introduced an arthroscopic release approach as a surgical option for lateral tennis elbow. The arthroscopic approach describes release of the extensor brevis as well as débridement of occasional intra-articular synovitis when present.21 Importantly, in a report of 18 cases in which Cummins did open surgical inspection after arthroscopy, he noted significant unresected tendinosis tissue in 14 of the cases.16 Further communication with Cummins reveals that he is no longer certain that arthroscopy adds value to lateral elbow tendinosis surgery.16 Arthroscopy also results in increased instrument costs, set-up time, and operative time. Arthroscopy also risks neurovascular harm and intra-articular scuffing, and results in some flexion contracture via intra-articular transgression for a problem that is extra-articular. For those few cases (5% in our experience) with associated intra-articular pathology45,55 (easily determined preoperatively by accurate history, and physical and imaging examinations), an expanded mini-open approach with a small incision arthrotomy expansion at the time of tendinosis surgery is more compelling than arthroscopy.53 Editors note: I do prefer arthroscopy to expanding the open procedure when concerned about intra-articular pathology (B. F. M.).
SURGICAL PATHOLOGY
A basic principle of any orthopedic surgery is that a clear definition of the pathology and its location is essential for a well-conceived surgical procedure. Because the extensor brevis origin is largely covered by the muscle of the extensor carpi radialis longus, extensor digitorum communis (EDC) aponeurosis release operations do not visualize the extensor carpi radialis brevis tendinosis pathology. Release of the common extensor origin, however, may alter the attachment of the brevis, because a significant segment of its origin is derived from the extensor aponeurosis.8,10,26,53 This anatomy helps to explain the instances of success of release techniques, including percutaneous procedures.5,24,68,78
Blazina and colleagues7 suggested that the major pathologic tendon changes in chronic patellar tendinosis occur by moderate but repetitive overload that results in microrupture of the normal tendinous tissue and secondary replacement by a healing process that is pathologic. Although this theory is attractive, I believe an additional more likely hypothesis is related to vascular supply and follows a sequence of events similar to that described by McNab,40 as well as Moseley and Goldie,43 in the rotator cuff region of the shoulder; namely, vascular compromise, an altered nutritional state, and intrinsic mechanical failure that results from force overload (e.g., tension and shear forces). In any event, actual gross disruption of the extensor carpi radialis brevis tendon, usually incomplete, occurs in approximately 35% of my surgical cases. Overall, the extensor carpi radialis brevis is involved by tendinosis in 100% of cases, with additional involvement of the anteromedial aspects of the extensor digitorum communis tendon (e.g., extensor aponeurosis) also in approximately 50%.
HISTORICAL SURGICAL RESULTS
The literature suggests that for lateral tennis elbow, approximately 85% to 90% of patients can expect some pain relief success with the varied surgical techniques discussed.8,9,15,19,41,60,68,78 Conversely, failure of release techniques is fairly common in this author’s experience. The most common cause for continuing pain after the index surgery is failure to identify and resect pain-producing tendinosis tissue (an integral conceptual deficiency in the release approach) (Chapter 46). Fortunately, when release techniques result in failure, revision salvage surgery can still offer an 85% opportunity of surgical success.42,56 Most articles citing release techniques also tend to be limited or silent regarding the logistics and speed of postoperative recovery. Using this author’s preferred technique, 97% of patients can expect pain improvement.51,53,54 In 85%, full return without pain to all prior activities including sport can be expected.54 In 12%, improvement has occurred, with some pain during aggressive activities, but often patients are able to participate in their usual sports, including the racquet and throwing sports. In about 3%, no improvement is obtained, and the surgery is considered a failure. The reasons for failure of the preferred technique are not always clear, but possibilities include misdiagnosis, such as entrapment of the posterior interosseous nerve and nonphysical or secondary gain factors.42,56 In 2006, we reported a 10- to 14-year follow-up of our pre-ferred technique. The results of 97% success were maintained.18
AUTHOR’S PREFERRED SURGICAL TREATMENT METHOD
SELECTION FACTORS FOR SURGERY
Failure of Rehabilitation and Duration of Symptoms
Patients who have undergone a high-quality resistance-exercise rehabilitation treatment program but have symptoms that linger for more than 1 year are more likely to have category III pathologic changes.53
Multiple Cortisone Injections
The success of cortisone injections or the delivery of corticosteroids by other mechanisms generally has been accepted clinically. Clarke and Woodland14 confirmed this clinical impression but emphasize that the improvement is short lived and recurrence is the rule. In my experience, patients who have received three or more cortisone injections in or about the same area are likely surgical candidates (R. P. Nirschl, unpublished data).52,53 There are two considerations in this group of candidates. First, the patient’s symptoms were of such severity that cortisone injection was warranted and may have indicated a higher initial pathologic category at the time the patient sought clinical help. Second, the studies of Unverferth and Olix72 and others2 suggest that large amounts of cortisone infiltration have a deleterious effect on the quality of the tendon, perhaps increasing the indication for surgery secondary to cortisone induced pathological change.
Pain (Constant) Without Activity
Pain at rest and that which alters routine daily function invariably reflects category III tendon pathology, suggesting the need for surgery.53
Tendon Calcification
Calcification in the body of the common extensor tendon (extensor aponeurosis) just distal to the lateral epicondyle has been noted on rare occasions. This form of presentation represents a pathologic tendon and is separate and distinct from lateral epicondylar exostosis (Fig. 44-10).
LATERAL TECHNIQUE (GENERAL CONCEPTS)
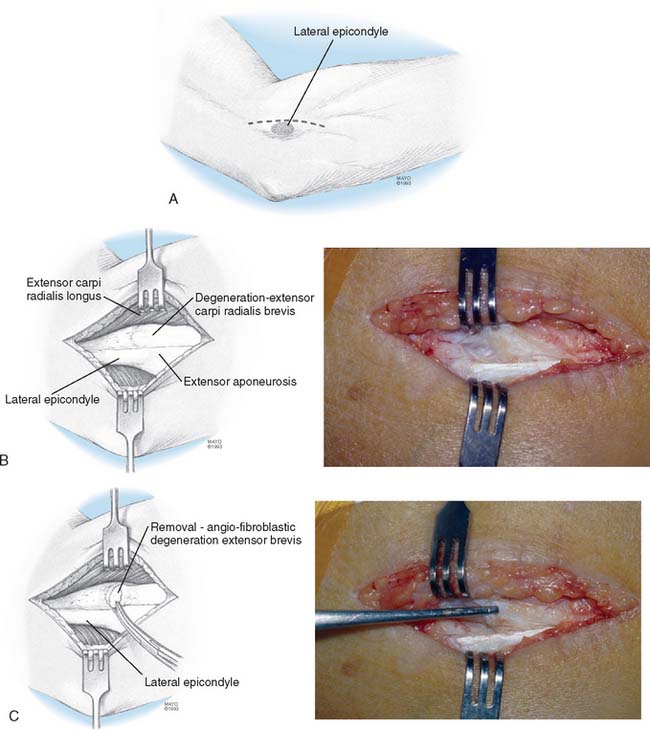
Identification of Pathology
Identification and excision of all pathologic tendinosis tissue generally includes most of, if not the entire, origin of the extensor carpi radialis brevis (Fig. 44-11). In addition (approximately 50%), excision of pathology also includes the anteromedial aspects of the extensor digitorum communis aponeurosis and, rarely, the removal of pathologic tissue from the underside of the extensor longus. When the extensor brevis origin is excised, the intimate and firm attachments between the fascia of the extensor brevis and the orbicular ligament and insertion into the distal aponeurosis eliminate any distal extensor brevis retraction beyond 1 to 2 mm (e.g., normal muscle-tendon unit length is maintained). Maintenance of normal muscle tendon length ensures normal leverage of the remainder of the musculotendinous unit of the extensor brevis; therefore, return to essentially normal forearm extensor strength can be anticipated.
Healing
Once the pathologic tissue has been removed, a tissue defect in the triangular recess is present in varying degrees. It is appropriate to attempt to enhance the blood supply to this area by drilling one or two small holes through the cortical bone to cancellous depth in the triangular recess just distal and anteromedial to the epicondyle. Do not however drill into the epicondyle itself because this will increase postoperative pain. Drilling in the appropriate area encourages hematoma formation with ingrowth of vascular and fibrotendinosis healthy replacement tissue52,53,56 (see Fig. 44-11).
Tissue Repair
Restoration of the normal extensor anatomic position, by sewing the posterolateral edge of the extensor longus to the anterior edge of the extensor aponeurosis, has been successful without causing loss of motion and is the repair technique of choice.51–53
Postoperative Rehabilitation
The postoperative rehabilitation of either lateral or medial tennis elbow for the author’s preferred techniques follows the treatment principles outlined for conservative care48,52 and detailed in Chapter 9. The elbow is maintained in 90 degrees of flexion, with wrist and hand free in an easily removable elbow immobilizer for approximately 6 days.48,52,53 Limbering activities are undertaken, however, on days 2 to 3, generally by working the arm actively in a warm shower, followed by a gradual return to strength training exercises (usually daily) without resistance for the first 3 weeks postoperatively. Starting at 3 weeks postoperatively, gradual strengthening isotonic and isoflex resistances are implemented, with protection by a medial or lateral counterforce brace. Postoperative counterforce bracing usually persists for 2 to 3 months for activities of daily living (ADLs) and thereafter for sports or occupational activity. Strength training and discretionary use of the arm for other activities are individualized to patient needs.48,52,53 For recreational tennis, it is usual to start easy strokes about 6 weeks from the time of surgery. For return to competitive athletics or occupational activities, the increase in intensity should be gradual and gentle, with counterforce brace protection until full strength has returned to the extremity. Some document this stage by Cybex or dynamometer tests and circumferential forearm girth.48,52,53 Satisfactory completion of the rehabilitative process includes transitional performance–type exercise programs for a return to sports or occupational activities. A return to full-strength use of the arm in competitive athletics, including the world class level, averages 5 to 6 months for lateral elbow tendinosis and 6 to 8 months for medial elbow tendinosis.
ASSOCIATED CONSIDERATIONS
When preoperative symptoms (e.g., history and physical examination) suggest an intra-articular component, preoperative bone scanning, computed tomography, or MRI may be ordered (Fig. 44-12). If positive or if intra-articular analgesia relieves the pain, arthroscopy might be considered to address intra-articular pathology. However, my experience with the miniarthrotomy, just anteromedial to the extensor digitorum communis aponeurosis closely reduplicates the postoperative morbidity of arthroscopy and is my preference in the combined surgical intervention of lateral elbow tendinosis and synovial plica (Fig. 44-13). (Editor prefers arthroscopy [B. F. M.].)
1 Baker C., Cummings P. Arthroscopic management of miscellaneous elbow disorders. Operative Techniques Sportsmed. 1998;6:16.
2 Balasubramaniam P., Prathap K. The effect of injection of hydrocortisone into rabbit calcaneal tendons. J. Bone Joint Surg. 1972;54B:729.
3 Bassett C.A.L. Pulsing electromagnetic fields: A new method to modify cell behavior in calcified and noncalcified tissues. Calcif. Tissue Int. 1982;34:1.
4 Bassett C.A.L., Choksh H.R., Hernandez E., Pawlik R.J., Strap M. The effect of pulsing electromagnetic fields on cellular calcium and calcification of nonunions. In: Brighton C.T., Black J., Pollack S.R., editors. Electrical Properties of Bone and Cartilage: Experimental Effects and Clinical Applications. New York: Grune & Stratton, 1979.
5 Baumgard S.H., Schwartz D.R. Percutaneous release of the epicondylar muscles for humeral epicondylitis. Am. J. Sports Med. 1982;10:233.
6 Bernhang A.M. The many causes of tennis elbow. N. Y. State J. Med. 1979;79:1363.
7 Blazina H.E., Kerlan R.K., Jobe F.W., Carter J.S., Carlson G.J. Jumper’s knee. Orthop. Clin. North Am. 1973;413:665.
8 Bosworth D.H. The role of the orbicular ligament in tennis elbow. J. Bone Joint Surg. 1955;37A:527.
9 Boyd H.B., McLeod A.C. Tennis elbow. J. Bone Joint Surg. 1973;55A:1183.
10 Briggs C.A., Elliott B.G. Lateral epicondylitis: A review of structures associated with tennis elbow. Anat. Clin. 1985;7:149.
11 Cabot A. Tennis elbow, a curable affliction. Orthop. Rev. 1987;16:69.
12 Capener N. The vulnerability of the posterior interosseous nerve of the forearm: A case report and an anatomical study. J. Bone Joint Surg. 1966;48B:770.
13 Carp L. Tennis elbow caused by radiohumeral bursitis. Arch. Surg. 1932;24:905.
14 Clarke A.K., Woodland J. Comparison of two steroid preparations used to treat tennis elbow, using the hypospray. Rheum. Rehabil. 1975;14:47.
15 Coonrad R.W., Hooper W.R. Tennis elbow: Its course, natural history, conservative and surgical management. J. Bone Joint Surg. 1973;55A:1177.
16 Cummins C.A. Lateral epicondylitis: in vivo assessment of arthroscopic debridement and correlation. Am. J. Sports Med. 2006;34:1486.
17 Cyriax J.H. The pathology and treatment of tennis elbow. J. Bone Joint Surg. 1936;18:921.
18 Dunn J., Kim J., Davis L., Nirschl R. Ten- to 14-year follow-up of the Nirschl surgical technique for lateral epicondylitis. Am. J. Sports Med. 2008;36:261.
19 Emery S.E., Gifford J.F. 100 years of tennis elbow. Contemp. Orthop. 1986;12:53.
20 Froimson A.I. Treatment of tennis elbow with forearm support band. J. Bone Joint Surg. 1971;53A:183.
21 Field L., Altchek D., Warren R., O’Brien S., Shyhar M., Wickiewicz T. Arthroscopic anatomy of the lateral elbow. Arthroscopy. 1994;10:602.
22 Funk D.A., An K.N., Morrey B.F., Daube J.R. Electromyographic analysis of muscles across the elbow joint. J. Orthop. Res. 1987;5:529.
23 Garden R.S. Tennis elbow. J. Bone Joint Surg. 1961;43B:100.
24 Gardner R.C. Tennis elbow: Diagnosis, pathology and treatment: Nine severe cases treated by a new reconstructive operation. Clin. Orthop. Rel. Res. 1970;72:248.
25 Goldie I.. Epicondylitis lateralis humeri (epicondylalgia or tennis elbow): A pathogenetical study. Acta Chir. Scand, 1964;Suppl.:339.
26 Greenbaum, B., and Vangsness, T.: Extensor carpi radialis brevis: An anatomic analysis of its origin. Presented to the Interim Meeting, American Orthopedic Society for Sportsmedicine. New Orleans, March 22, 1998.
27 Groppel J.L., Nirschl R.P., Pfantsch E., Greer N. A mechanical and electromyographical analysis of the effects of various joint counterforce braces on the tennis player. Am. J. Sports Med. 1986;14:195.
28 Groppel, J. L., Nirschl, R. P., Sholes, J., and Sobel, J.: A mechanical comparison of an isoflex exercise device to the use of free weights. Unpublished data, 1984.
29 Gruchow H.W., Pelletier D. An epidemiologic study of tennis elbow. Incidence, recurrence, and effectiveness of prevention strategies. Am. J. Sports Med. 1979;7:234.
30 Gunn C.C., Milbrandt W.E. Tennis elbow and the cervical spine. Can. Med. Assoc. J. 1976;114:803.
31 Hohmann G. Das Wesen und die Behandlung des Sogenannten tennissellenbogens. Munch. Med. Wochenschr. 1933;80:250.
32 Ilfeld F.W., Field S.M. Treatment of tennis elbow: Use of special brace. J. A. M. A. 1966;195:67.
33 Jalovaara P., Lindholm R.V. Decompression of the posterior interosseous nerve for tennis elbow. Arch. Orthop. Trauma Surg. 1989;108:243.
34 Kahn K., Cook B., Mafulli N., Kannus P. Where is the pain coming from in tendinopathy? Br. J. Sportsmed. 2000;34:81.
35 Kahn K., Cook B., Trunton J., Bonnar F. Overuse tendinosis, not tendinitis. Physician Sportsmed. 2000;28:38.
36 Kaplan E.B. Treatment of tennis elbow (epicondylitis) by denervation. J. Bone Joint Surg. 1959;41A:147.
37 Kraushaar B., Nirschl R. Tendinosis of the elbow (tennis elbow): Clinical features and findings of histological, immunohistochemical, and electron microscopy studies. J. Bone Joint Surg. 1999;81A:259.
38 Lian O., Dahl J., Ackerman P., Frihagen F., Engrebetsen L., Bahr R. Pronociceptive and antinociceptive neuromediators in patellar tendinopathy. Am. J. Sports Med. 2006;34:1801.
39 Major H.P. Lawntennis elbow. B. M. J. 1883;2:557.
40 McNab I. Rotator cuff tendinosis. Ann. R. Coll. Surg. Engl. 1973;53:271.
41 Michele A.A., Krueger F.J. Lateral epicondylitis of the elbow treated by fasciotomy. Surgery. 1956;39:277.
42 Morrey B.F. Reoperation for failed surgical treatment of refractory lateral epicondylitis. J. Shoulder Elbow Surg. 1992;1:47.
43 Moseley H.F., Goldie I. The arterial pattern of the rotator cuff of the shoulder. J. Bone Joint Surg. 1963;45B:780.
44 Neviaser T.J., Neviaser R.J., Neviaser J.S., Ain B.R. Lateral epicondylitis: Results of outpatient surgery and immediate motion. Contemp. Orthop. 1985;11:43.
45 Newman J.H., Goodfellow J.W. Fibrillation of the head of the radius: One cause of tennis elbow. J. Bone Joint Surg. 1975;57B:115.
46 Nirschl R.P. Mesenchymal syndrome. Virginia Med. M. 1969;96:659.
47 Nirschl R.P. Tennis elbow. Orthop. Clin. North Am. 1973;4:787.
48 Nirschl R.P. Arm Care. Arlington, VA: Medical Sports Publishing, 1996.
49 Nirschl R.P. Isoflex exercise system. Arlington, VA: Med. Sports Pub., 1983.
50 Nirschl R.P. Prevention and treatment of elbow and shoulder injuries in the tennis player. Clin. Sportsmed. 1998;7:289.
51 Nirschl R.P. Elbow tendinosis/tennis elbow. Clin. Sportsmed. 1992;2:851.
52 Nirschl R.P. Lateral and medial epicondyltis. In: Morrey B., editor. Master Techniques in Orthopedic Surgery: The Elbow. New York: Raven Press; 1994:129-148.
53 Nirschl R.P., Ashman E. Elbow tendinopathy: Tennis elbow. Clin Sports Med. 2003;22:813-836.
54 Nirschl R.P., Pettrone F. Tennis elbow: The surgical treatment of lateral epicondylitis. J. Bone Joint Surg. 1979;61A:832.
55 Nirschl R.P., Sobel J. Conservative treatment of tennis elbow. Phys. Sports Med. 1981;9:42.
56 Organ S., Nirschl R., Kraushaar B., Guidi E. Salvage surgery for lateral tennis elbow. Am. J. Sports Med. 1997;25:746.
57 Osgood R.B. Radiohumeral bursitis, epicondylitis, epicondylalgia (tennis elbow): A personal experience. Arch. Surg. 1922;4:420.
58 Paoloni J., Appleyard R., Nelson J., Murrell G. Topical nitric oxide application in the treatment of chronic extensor tendinosis at the elbow. Am. J. Sports Med. 2003;31:915.
59 Percy C., Carson J.D. Use of DMSO in tennis elbow and rotator cuff tendinosis: Double-blind study. Med. Sci. Sports Exer. 1981;13:215.
60 Posch J.N., Goldberg V.M., Larrey R. Extensor fasciotomy for tennis elbow: A long-term follow-up study. Clin. Orthop. 1978;135:179.
61 Priest J.D., Braden V., Gerberich J.G. The elbow and tennis (part I). Phys. Sports Med. 1980;8:80.
62 Priest J.D., Braden V., Gerberich J.G. The elbow and tennis (part II). Phys. Sports Med. 1980;8:77.
63 Regan W., Wold L.E., Coonrad R., Morrey B.F. Microscopic histopathology of lateral epicondylitis. Am. J. Sports Med. 1992;20:746.
64 Roles N.C., Maudsley R.H. Radial tunnel syndrome, resistant tennis elbow as a nerve entrapment. J. Bone Joint Surg. 1972;54B:499.
65 Rompe J., Decking J., Nafe B. Shock wave application for chronic plantar fasciitis in running athletes. a prospective randomized placebo controlled trial. Am. J. Sports Med. 2003;31:268.
66 Runge F. Zur Genese und Behandlung des Schreibekrampfes. Berl. Klin. Wochenschr. 1873;10:245.
67 Sarkar K., Uhthoff H.K. Ultrastructure of the common extensor tendon in tennis elbow. Virchows Arch. Pathol. Anat. Histol. 1980;386:317.
68 Savoie, F.: Percutaneous release in the release on the surgical treatment of lateral epicondylitis. Presented to the 3rd International Meeting of the Society for Tennis Medicine. New Haven, Conn., June 1997.
69 Sems A., Dimeff R., Iannotti J. Extracorporeal shock wave therapy in the treatment of chronic tendinopathies. J. Am. Acad. Orthop. Surg. 2006;14:195.
70 Stovall P.B., Beinfield M.S. Treatment of resistant lateral epicondylitis of the elbow by lengthening of the extensor carpi radialis brevis tendon. Surg. Gynecol. Obstet. 1979;149:526.
71 Tasto J., Cummings J., Medlock J., Harwood F., Hardesty R., Amiel D. The Tendon Treatment Center; New horizons in the treatment of tendinosis. Arthroscopy. 2003;19(suppl 1):213.
72 Unverferth L.J., Olix M.L. The effect of local steroid injection on tendon. J. Sports Med. 1973;1:31.
73 Voloshin I., Gelinas J., Maloney M.D., O’Keefe R.J., Bigliani L.U., Blaine T.A. Pro-inflammatory cytokines and metalloproteases as expressed in the subacromial bursa in patients with rotator cuff disease. Arthroscopy. 2005;21:1076.
74 Wadsworth T.G. Lateral epicondylitis. Lancet. 1972;1:959.
75 Wadsworth C.T., Nielsen D.H., Burns L.T., Krull J.D., Thompson C.G. The effect of the counterforce armband on wrist extension and grip strength and pain in subjects with tennis elbow. J. Orthop. Sports Phys. Ther. 1989;11:192.
76 Wang C., Chen H. Shock wave therapy for patients with lateral epicondylitis of the elbow: a one- to two-year follow-up study. Am. J. Sports Med. 2002;30:422.
77 Werner C.O. Lateral elbow pain and posterior interosseous nerve entrapment. Acta Orthop. Scand. Suppl. 1979;174:1.
78 Yerger B., Turner T. Percutaneous extensor tenotomy for chronic tennis elbow: An office procedure. Orthopaedics. 1985;8:1261.