11 Ten questions to ask when planning a curriculum
1. What are the needs to be met by the training programme?
2. What are the expected learning outcomes?
3. What content should be included?
4. How should the content be organised?
5. What educational strategies should be adopted?
6. What teaching methods should be used?
7. How should assessment be carried out?
8. How should details of the curriculum be communicated?
9. What educational environment or climate should be fostered?
What are the expected learning outcomes?
Key to a curriculum are the learning outcomes expected of the learner. We highlighted in Section 2 the importance of learning outcomes and the move away from an emphasis on the education process to an outcome-based education model where the emphasis is on the product. We looked at how learning outcomes can be expressed and communicated relating to technical competencies and clinical skills; approaches to practice embracing an understanding of the basic sciences, appropriate attitudes and decision-making strategies; and personal development and professionalism. Decisions about the learning outcomes should inform the answers to the questions that follow.
What content should be included?
There will be an agreed core content which has to be mastered by all students, with opportunities to study other subjects through electives or student-selected courses, as described in Chapter 17.
How should the content be organised?
With the learning outcomes and the content determined, the next step is to consider how the curriculum should be organised and the content sequenced. The traditional approach in medical education has been to introduce students first to the basic medical sciences and normal function, structure and behaviour of the human body. As students progressed through the curriculum to the later years, the focus was on abnormal function and the development of clinical skills. Later, students developed their clinical competence on the job as they managed patients. This sequence, while having much to commend it, has disadvantages. The relevance of the content is not obvious to the student and, as we discuss in Chapter 2, as a consequence the learning may be less effective. How content can be arranged and sequenced in a way that leads to more effective and efficient learning as students progress through their training is important and is covered in Chapter 12.
What educational strategies should be adopted?
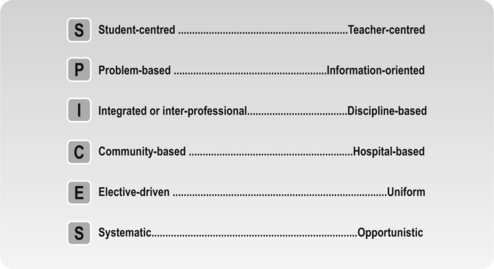
Educational strategies may be seen as the key element in a curriculum with the curriculum labelled in terms of the educational strategy, e.g. a ‘problem-based curriculum’ and ‘a community orientated curriculum’. The SPICES model for curriculum planning identifies six educational approaches and presents each on a continuum (Fig. 11.1).
Student-centred/teacher-centred
There has been a significant move towards a more student-centred approach in the curriculum, as described in Chapter 13, with students given more responsibility for their own learning. It is what students learn that matters and not what teachers teach. Teachers are being challenged and programmes scrutinised to establish whether they are meeting the needs of individual students in terms of content, approaches to learning and time taken to complete.
Problem-based/information-orientated
A problem-based approach to learning has been adopted in a number of schools over the past two decades. The starting-off point and the focus for the learning is a clinical problem. It is what the students need to know to understand the problem that drives their activities. This topic is discussed further in Chapter 14. Task-based learning is described as a variation of problem-based learning.
Integrated/discipline-based
There has been a significant move away from curricula based on courses that relate to individual subjects or disciplines such as anatomy, surgery and pathology, to courses integrated around body systems such as the cardiovascular system. There is also a move towards a greater integration between the basic medical sciences and clinical subjects. An inter-professional approach where different professions share, to a greater or lesser extent, their learning experiences is being explored and implemented in some education programmes. This makes sense given the need for students to develop teamwork skills. Integration and inter-professional education is explored further in Chapter 15.
Community based/hospital based
There has been a move away from a curriculum that provides only a hospital-based setting for students to gain their experience. More attractive is a curriculum that, in addition, offers experience in a community setting. This is covered in Chapter 16.
Elective/uniform
A curriculum should include both core elements common to all students, and electives or student-selected components. Such options provide students with a choice of topics for their study. The concept of a core curriculum with options is addressed in Chapter 17.
What teaching methods should be used?
A description of traditional approaches and the introduction of exciting newer methods is provided in Section 4.
How should assessment be carried out?
A key element in the curriculum and one that significantly influences students’ behaviour is assessment. It is essential that assessment matches closely the expected learning outcomes. Decisions have to be taken about the overall assessment strategy and the appropriate instruments to be adopted with this in mind. The objective structured clinical examination (OSCE) and assessment portfolios have been introduced to meet the need for more authentic and performance assessment instruments. Work-based assessment is growing in popularity particularly in postgraduate education. Section 5 describes established and newer approaches to assessment and the key issues that have to be addressed when an assessment programme is planned.
How should details of the curriculum be communicated?
• a clear statement and explanation of the expected learning outcomes
• a series of blueprints relating the learning outcomes to the available learning opportunities, the phases of the curriculum and the assessment
• a curriculum map, as described in Chapter 19, that shows the relationship between the different elements in the curriculum.
What educational environment or climate should be fostered?
Important, but often ignored in the consideration of the curriculum, is the educational climate or environment. This is the overall atmosphere of the school or wherever learning is taking place. It embraces, for example, the extent to which students feel they are studying in a supportive or threatening environment and whether the environment encourages teamwork and collaboration, appropriate professional behaviour, and creativity. A number of instruments are available that allow the educational environment to be measured. This topic is discussed in Chapter 18.
How should the process be managed?
• the coordination of each phase in the curriculum
• the organisation and delivery of each course
• the management of electives and options
• support for students including students with difficulties
• computer and information technology
• a clinical skills centre and the use of simulators and simulated patients.
Reflect and react
1. Think about the ten questions as they relate to your own teaching situation. You may not be a member of a curriculum committee or directly involved with curriculum planning, but as a stakeholder you have an important role to play and will be able to discharge your responsibilities more effectively if you have an understanding of the issues involved.
2. Think about the educational strategies for the educational programme with which you are involved. Where do you lie on the SPICES continuum and where would you like to be?
Harden R.M. Ten questions to ask when planning a course or curriculum. Med. Educ.. 1986;20:356-365.
A description of the ten questions to be asked when planning a curriculum.
Harden R.M., Sowden S., Dunn W.R. Some educational strategies in curriculum development: the SPICES model. ASME Medical Education Booklet No. 18. Med. Educ.. 1984;18:284-297.
A description of the SPICES model and how it can be used in curriculum planning and evaluation.
Fleiszer D.M., Posel N.H. Development of an undergraduate medical curriculum: the McGill experience. Acad. Med.. 2003;78:265-269.
Grant J. Principles of curriculum design. In: Swanwick T., editor. Understanding Medical Education: Evidence, Theory and Practice. Chichester: Wiley-Blackwell, 2010.
A description of the steps in curriculum design.
Kern D.E., Thomas P.A., Howard D.M., Bass E.B. Curriculum Development for Medical Education. A Six-Step Approach. Baltimore and London: The Johns Hopkins University Press; 2011.