T
tabes dorsalis A degenerative disease of the posterior columns of the spinal cord, the posterior spinal roots and the peripheral nerves accompanied by a number of ocular signs and symptoms such as atrophy of the optic nerve, visual field defects, ptosis, Argyll Robertson pupil and paralysis of one or more of the extraocular muscles. The disease is a result of neurosyphilis.
TABO notation See axis notation, standard.
tachistoscope An instrument that presents visual stimuli for a brief and variable period of time (usually less than 0.1 s).
tacrolimus See immunosuppressants.
Talbot-Plateau law See law, Talbot-Plateau.
tamponade agent A gas, pad or silicone oil used to plug a cavity, stop a haemorrhage or compress a part. In the eye it may be employed in vitreous surgery to fill the vitreous space with either gas or silicone, and in retinal detachment therapy.
tangent scale See Maddox cross.
tangent screen See screen, tangent.
tangential focus See astigmatism, oblique.
tapetoretinal degeneration See degeneration, tapetoretinal.
tapetum lucidum A reflecting pigment layer lying behind the visual receptors of the retina of certain mammals (e.g. cats, dogs), birds and fish, which gives a shining appearance to the eyes when illuminated in the dark. The tapetum is located either in the pigment epithelium or in the choroid and covers either the whole fundus or more often only the upper and back portion. The role of the tapetum lucidum is to increase the probability of visual stimulation of the photoreceptors by reflecting light back after having already traversed them once, thus aiding vision in dim illumination. In some species the tapetum consists of guanine crystals.
target A pattern or an object of fixation such as a red dot or an optotype.
See optotype.
tarsal Pertaining to the tarsus.
tarsal gland See glands, meibomian.
tarsal muscles See muscles, Müller’s palpebral.
tarsal plate See tarsus.
tarsorrhaphy A surgical procedure consisting of suturing the upper and lower eyelids together either partially or completely. It provides a temporary protection to the eye or forms part of the treatment of dry eyes.
See alacrima; keratoconjunctivitis sicca.
tarsus Thin flat plate of dense connective tissue, situated one in each eyelid, which gives it shape and firmness. Each tarsus extends from the orbital septum to the eyelid margin. The upper tarsal plate, shaped like the letter D placed on its side, is much larger than the lower. Its width is 11 mm in the centre whereas the corresponding measurement in the lower tarsus, which is somewhat oblong in form, is 5 mm. Each tarsus is about 29 mm long and 1 mm thick. Within each tarsus are the meibomian glands, approximately 25 in the upper and 20 in the lower. Syn. tarsal plate.
See ligament, palpebral; orbital septum.
Tay’s choroiditis See drusen, familial dominant.
Tay–Sachs disease See disease, Tay–Sachs.
tear duct One of about a dozen ducts of the lacrimal gland. It originates in the orbital part of the gland, traverses the palpebral part of the gland and opens into the lateral superior fornix of the conjunctival sac. Syn. lacrimal duct.
See lacrimal apparatus.
tear exchange See lens, fenestrated.
tear film See film, precorneal.
tear film break-up test See test, break-up time.
tear film, prelens Tear film found on the front surface of a contact lens on the eye. The oily layer of the film is slightly thinner with soft lenses than in the precorneal film and almost absent with rigid lenses. The aqueous layer is thinner with rigid lenses than in the precorneal film. The exact composition of the prelens tear film varies with the characteristics of the contact lens on the eye.
See film, precorneal.
tear layer See film, precorneal.
tear meniscus A thin strip of tear fluid with concave outer surfaces at the upper and lower lid margins. It contains most of the exposed tear volume. The absence of a tear meniscus is an indication of a dry eye. Syn. marginal tear strip; lacrimal prism; tear prism.
See film, precorneal; lacrimal lake.
tear prism See tear meniscus.
tear pumping The mechanism involving blinking, which acts to bring fresh tears with oxygen and nutrients to the cornea behind a contact lens, and pumping stale tears containing carbon dioxide, lactic acid and other waste products from beneath the lens. It occurs most readily with hard contact lenses (between 14% and 20% of the tear volume is exchanged with each blink) and to a much smaller extent with soft lenses (between 1% and 5% of the tear volume is exchanged with each blink).
See hypoxia; oxygen transmissibility.
tear, retinal See retinal break.
tear secretion There are two types of tear secretion: (1) Basal (basic) tear secretion, which occurs normally without any stimulation. It maintains the cornea and conjunctiva continuously moist, but is reduced in dry eyes (e.g. keratoconjunctivitis sicca) and in elderly individuals. (2) Reflex tear secretion, which is produced in response to a corneal or conjunctival irritant and also depends on psychological factors. Basal secretion and reflex secretion are produced by the lacrimal gland and the accessory glands of Krause and Wolfring. The amount of tears secreted amounts to 14–33 g per 24 hours or 0.5–2.2 μl/minute, being about 2 μl/minute at 15 years of age and less than 1 μl/minute at 65 years of age. Note: it was formally thought that basal secretion was produced solely by the accessory glands and reflex secretion by the lacrimal gland but it is now thought that they all contribute to both forms of tear secretion.
See reflex, lacrimal; test, basic secretion; test, Schirmer’s.
tear stasis The slowing down or stoppage of tear flow behind a contact lens. It can lead to lens adherence (lens binding) to the cornea with the possible consequences of acute red eye, arcuate corneal staining, and, if severe, corneal ulceration. Fitting or refitting in such a way that some lens movement is maintained usually prevents this condition.
See lens adherence; staining, fluorescein.
tear strip, marginal See tear meniscus.
tearing reflex See reflex, lacrimal.
tears The clear watery fluid secreted by the lacrimal gland which, together with the secretions from the meibomian glands, the goblet cells, the gland of Zeis, as well as the accessory lacrimal glands of Krause and Wolfring, helps to maintain the conjunctiva and cornea moist and healthy. Periodic involuntary blinking spreads the tears over the cornea and conjunctiva and causes a pumping action of the lacrimal drainage system, through the lacrimal puncta into the nasolacrimal duct. Approximately 25% of the tears is lost by evaporation, the remaining 75% is pumped into the nasal cavity and over 60% of the tear volume is drained through the lower canaliculus. Tears contain water (98.2%), salts, lipids (e.g. wax esters, sterol esters, hydrocarbons, polar lipids, triglycerides and free fatty acids), proteins (e.g. lysozyme, lactoferrin, albumin, IgA, IgE, IgG, complement proteins C3, C4, C5 and C9, and beta-lysin), magnesium, potassium, sodium, calcium, chloride, bicarbonate, urea, ammonia, nitrogen, citric acid, ascorbic acid, and mucin. Tears have a pH varying between 7.3 and 7.7 (shifting to a slightly less alkaline value when the eye is closed) and the quantity secreted per hour is between 30 and 120 ml. Syn. lacrimal fluid.
See alacrima; blink; epiphora; film, precorneal; hyperlacrimation; keratoconjunctivitis sicca; lacrimal apparatus; lacrimal lake; lysozyme; mucin; staining, fluorescein; test, break-up time; test, non-invasive break-up time; test, phenol red cotton thread; test, Schirmer’s.
artificial t. Any eye drop solution that can replace tears by approximating its consistency in terms of viscosity and tonicity and may contain many of the substances found in tears. The most common agents found in artificial tears are cellulose derivatives, such as methylcellulose, hydroxymethylcel-lulose, hydroxypropylcellulose, hypromellose (hydroxypropylmethylcellulose), hydroxyethylcellulose, and polyvinyl alcohol, povidone (polyvinyl pyrrolidine), sodium hyaluronate and sodium chloride, which have low viscosity. Carbomer (polyacrylic acid), carmellose (carbomethylcellulose), liquid paraffin and yellow soft paraffin have medium to high viscosity. Acetylcysteine, a mucolytic agent prepared with hypromellose is used when the tear deficiency is associated with threads and filaments of mucus to soften and make the mucus more fluid, as well as shrinking the mucous membranes (astringent). Syn. ocular lubricant.
See alacrima; corneal erosion, recurrent; ectropion; eye, dry; hypromellose; keratoconjunctivitis sicca; methylcellulose; palsy, Bell’s; wetting solution; xerophthalmia.
crocodile t. Copious secretion of tears occurring during eating in cases of abnormal regeneration of the seventh cranial nerve after recovery from Bell’s palsy. Syn. paradoxic lacrimation.
Tearscope plus Trade name of a handheld instrument designed to view the tear film non-invasively. It uses a cold light source to minimize any drying of the tear film during the examination. It can be used directly in front of the eye or in conjunction with a slit-lamp biomicroscope to gain more magnification. Evaluation of the interference patterns of the anterior surface of the tear film lipid layer facilitates the diagnosis of the cause of dry eye symptoms, as well as screening patients for contact lens wear. The instrument also allows the measurement of the non-invasive break-up time.
See film, precorneal; test, non-invasive break-up time.
technique See method or test.
tectal midbrain syndrome See syndrome, Parinaud’s.
tectum of the mesencephalon Structure comprising the plate of grey and white matter (called the tectal lamina) that forms the roof of the midbrain and from which project the inferior and superior colliculi. The area anterior to it is called the pretectal region. Syn. tectum of the midbrain; optic tectum. Note: The word tectum comes from the Latin and means roof. The word mesencephalon is made up of two parts that come from the Greek and means middle brain.
See colliculi, inferior; colliculi, superior; fibres, pupillary; nystagmus, convergence-retraction; pathway, retinotectal; pretectum.
tectum of the midbrain See tectum of the mesencephalon.
teichopsia A transient, shimmering visual sensation. Example: the fortification spectrum of a scintillating scotoma.
telangiectasia A dilatation of small blood vessels (arterioles, capillaries, venules), often multiple in character. Telangiectasias create small red lesions, sometimes spidery in appearance, usually in the skin or mucous membranes, which blanch on pressure. They can develop into naevus flammeus (‘port-wine stain’), a birthmark found usually on the head or neck.
See syndrome, Sturge–Weber.
retinal t. See disease, Coat’s.
Telebinocular A trade name for a stereoscope based on that of Brewster–Holmes and used to investigate distance and near visual functions such as acuity, stereopsis, etc.
See stereoscope, Brewster’s.
telecanthus Excessive separation between the medial canthi of the eyelids. It may occur in isolation or form part of the blepharophimosis syndrome. Treatment consists in shortening and re-fixating the medial canthal tendons to the lacrimal crest.
See syndrome, blepharophimosis.
telecentric Pertains to an optical system in which its aperture stop is positioned so that the entrance pupil falls in the first focal plane, the exit pupil is at infinity, and the rays through the centre of the entrance pupil from all points on the object are parallel to the axis in the image space. Similarly, if the exit pupil lies in the second focal plane the entrance pupil will be at infinity, and the rays through the centre of the exit pupil will be parallel to the axis in the object space.
teleopsia Anomaly of visual perception in which objects appear to be much further away than they actually are. It may be due to vision in a hazy atmosphere, intoxication, neurosis, etc.
See metamorphopsia.
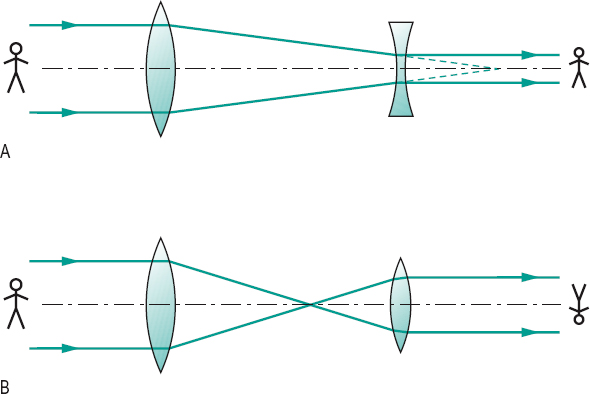
telescope An optical instrument for magnifying the apparent size of distant objects. It consists, in principle, of two lenses: (1) the objective, being a positive lens which forms a real inverted image of the distant object; (2) the eyepiece through which the observer views a magnified image of that formed by the objective. The eyepiece may be either positive (astronomical or Kepler telescope) or negative (galilean telescope). The magnification M of a telescope is given by the following formula
< ?xml:namespace prefix = "mml" />
where f’o is the second focal length of the objective, fe the first focal length of the eyepiece, and Do and De are the diameters of the entrance and exit pupils of the telescope (approximately equal to the diameters of the objective lens and the eyepiece).
There are also some telescopes that do not use a lens (or lens system) as objective, as these are difficult to produce if large apertures and minimum aberrations are required. These telescopes use a concave mirror (usually parabolic) as the objective. They are called reflecting telescopes. Light from a distant object is collected by the large concave mirror and reflected onto a small mirror (positive in the Cassegrain telescope and negative in the gregorian telescope). This mirror is located on the optical axis and light is then transmitted through a central hole in the concave mirror onto the eyepiece. In the newtonian telescope the light collected by the large concave mirror is reflected onto a small plane mirror at a 45° angle to the optical axis, and transmitted to the eyepiece, which is at right angles to the optical axis (Fig. T1).
See binoculars; eyepiece; magnification, telescopic; objective.
astronomical t. See telescope.
bioptic t . A system of lenses forming a galilean or Kepler telescope which is mounted high on a plastic spectacle or carrier lens with the distance correction, so as to allow the patient to look through either the telescope, or below, by moving his or her head. It is used to magnify distant objects for patients with low vision. Syn. bioptic position telescope.
Cassegrain t . See telescope.
Dutch t. See telescope, galilean.
galilean t. A simple optical system that allows observation of far objects with a low magnification and without image inversion. It consists of a convex lens, which acts as the objective, and a concave lens as the eyepiece. Magnification of such a telescope rarely exceeds x 5. This optical system is used in opera glasses and as a low vision aid (Fig. T1). Syn. Dutch telescope.
See binoculars; minification.
gregorian t.; Kepler t.; newtonian t.
See telescope.
reflecting t. A telescope that uses a concave mirror as the objective.
refracting t . A telescope that uses a positive lens system as the objective.
reverse t . See field, visual expander.
terrestrial t. A telescope that provides an erect image of a distant object. The image is usually erected by means of a lens system placed between the objective and the eyepiece. It does, however, make the terrestrial telescope relatively longer than an astronomical telescope.
See binoculars; erector.
telescopic spectacles See lens, telescopic.
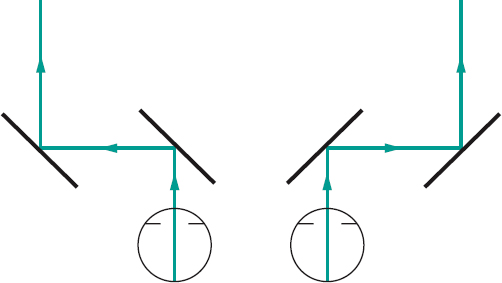
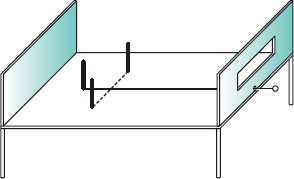
telestereoscope, Helmholtz Instrument designed to produce an exaggerated perception of depth by optically increasing the length of the base line of the viewer, using a system of mirrors or prisms (Fig. T2).
Teller acuity cards See acuity cards, Teller.
temple 1 . See side of a spectacle frame. 2. The lateral area of the human head between the outer canthi and the ears and above the zygomatic arch.
temple, library A straight side of a spectacle frame.
See spectacles, library.
temporal arteritis; induction; summation
See under the nouns.
tendon See muscles, extraocular.
tendon of Zinn See annulus of Zinn.
Tenon’s capsule The fibrous membrane that envelops the globe from the margin of the cornea to the optic nerve. Its inner surface is in close contact with the episclera to which it is connected by fine trabeculae. These trabeculae also attach it to the extraocular muscles. The posterior surface of the capsule is in contact with the orbital fat. Anteriorly, it becomes thinner and merges gradually into the subconjunctival connective tissue. Syn. Bonnet’s capsule; capsule of the eyeball; fascia bulbi.
See injection, sub-Tenon’s; ligament of Lockwood.
tension, ocular See pressure, intraocular.
Terrien’s disease See ectasia, corneal.
Terson’s syndrome See syndrome, Terson’s.
tertiary action; position See under the nouns.
test 1 . A method of examination to determine a disease or a performance. 2. To try; to prove. 3. The equipment used to carry out the test.
after-image t . A subjective test used to determine the presence or absence of abnormal retinal correspondence (ARC). The subject is instructed to fixate the centre of a vertical light filament for some 15 s with one eye and then the centre of a horizontal light filament for some 15 s with the other eye. Looking at the after-images of the two filaments on a uniform surface (e.g. a wall) the subject sees either a cross, which indicates normal retinal correspondence or two separated filaments, indicating ARC. Syn. Hering’s after-image test.
See after-image; retinal correspondence, abnormal.
after-image transfer t. Test aimed at detecting and measuring the angle of eccentric fixation in an amblyopic eye in a patient with normal retinal correspondence. The normal eye fixates an illuminated vertical line and is then occluded, while the amblyopic eye fixates a dot. If the after-image and the fixation point coincide the amblyopic eye has no eccentric fixation, otherwise the relative position of one to the other indicates the angle of eccentric fixation. Syn. Brock’s after-image test.
See fixation, eccentric; retinal corresponding points.
alternate cover t. See test, cover.
Ammann’s t. See test, neutral density filter.
Arden grating t. A clinical test for contrast sensitivity. It consists of photographic plates, each with a sinusoidal grating of constant spatial frequency but of increasing contrast from top to bottom. There are seven plates, one being for demonstration. The other six, each with a different spatial frequency, are used for testing. The spatial frequencies are: 0.2, 0.4, 0.8, 1.6, 3.2 and 6.4 cycles per degree when viewed at a distance of 50 cm. Contrast levels are numbered from 1 to 20 on a vertical scale on the side of the plate. The testing procedure consists of slowly removing each plate from its folder until the grating becomes visible to the patient, at which point the contrast level is noted. The testing is carried out monocularly with optical correction, if any. The procedure is repeated for each plate and all the contrast levels are added to arrive at a score, which is compared with normal values provided in the instructions. Syn. Arden gratings; Arden plates.
See chart, contrast sensitivity; function, contrast sensitivity; Vistech.
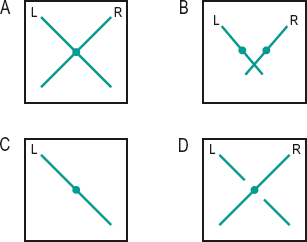
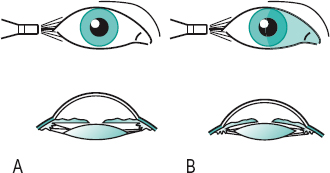
Bagolini’s lens t. A test to detect binocular sensory and motor anomalies such as abnormal retinal correspondence and suppression. Two Bagolini lenses, one in front of each eye with their striations oriented 90° apart (typically 135° for one eye, 45° for the other) are used. The patient fixates a punctate light source at distance and near. Each eye sees a diagonal line perpendicular to that seen by the fellow eye. For example, if one line, or part of one line, is missing there is suppression. If the two diagonal lines cross at the source the patient is orthophoric or if strabismic, as indicated by the cover test, the patient has harmonious abnormal retinal correspondence (Fig. T3). Syn. Bagolini’s striated lens test.
See glass, Bagolini’s.
balancing t. A test designed to obtain equal focusing or equal accommodative states in the two eyes. This is accomplished either objectively (by retinoscopy) or, more commonly, subjectively using either the duochrome test, or comparing the visual acuity in the two eyes simultaneously or successively, or using prisms to present two images of a chart and ask the patient to compare these images, or using a binocular refraction technique (e.g. Turville infinity balance test). Syn. equalization test.
See balance, binocular; method, Humphriss; vectogram.
bar reading t. A test for determining the presence of binocular vision and also used in the management of amblyopia in which a narrow bar (or a pencil) is held vertically between the reader’s eyes and a page of print. The bar occludes a vertical strip of print but the strip is different for the two eyes and if binocular vision is present the subject will experience no difficulty reading the text. Syn. Welland’s test.
basic secretion t. Measurement of the basal tear secretion independently of reflex tear secretion. A filter paper strip (e.g. Whatman No. 41) is placed in the anaesthetized lower fornix, and after five minutes the strip is removed and the amount of wetting measured from the folded end.
See tear secretion; test, Schirmer’s.
Bielschowsky’s head tilt t . A test to determine which of the inferior or superior extraocular muscles and of which eye is paretic. The test is based on the following fact: if the head is tilted to the right, the right intorters of the right eye (superior oblique and superior rectus muscles) contract as well as the extorters of the left eye (inferior oblique and inferior rectus muscles). If the head is tilted to the left, the inferior oblique and inferior rectus muscles of the right eye contract to cause extorsion while the superior oblique and superior rectus of the eye contract to cause intorsion. Thus, tilting the head towards one side will indicate the palsied muscle. For example, in the right superior rectus muscle palsy, when the head is tilted to the left there will be no change in the vertical deviation, since contraction of the right superior rectus muscle is not involved. However, when the head is tilted to the right there will be an increase in downward movement. This test is not reliable in an adult with congenital ocular palsy.
See test, forced duction; test, three-step.
Bielchowsky’s phenomenon t. A test used to differentiate between dissociated vertical deviation (DVD) and alternating hypertropia. After the occlusion of one eye (which elevates behind the cover) a wedge of increasing density is placed in front of the fixating eye; if the patient has DVD the eye behind the cover will perform a gradual downward movement with increasing filter density and a gradual upward movement if the wedge is moved in the opposite direction. Syn dark wedge test.
See deviation, dissociated vertical; phenomenon, Bielchowsky’s.
blind t. See study, single-blind; study, double-blind.
blue field entoptoscope t. See entoptoscope, blue field.
blur back t. See test, plus 1.00 D blur.
break-up time t. (BUT) A test for assessing the precorneal tear film. Fluorescein is applied to the bulbar conjunctiva and the patient is asked to blink once or twice and then to refrain from blinking. The tear film is scanned through the slit-lamp using a cobalt blue filter with a wide beam, while the examiner counts or records the time between the last blink and the appearance of the first dry black spot which indicates that the tear film is breaking up. In normal subjects, break-up times vary between 15 and 35 s (in Caucasians). A BUT of 10 s or less is abnormal and may be due to mucin deficiency, and is often considered to be a negative factor for success in contact lens wear, especially soft lenses. However, this test has been shown to be flawed, because fluorescein can disrupt the tear film.
See film, precorneal; lens, cobalt; mucin; test, non-invasive break-up time.
broad H t. A test to evaluate the integrity of the extraocular muscles and their innervation. The patient is asked to fixate a penlight while keeping the head still. The penlight is moved slowly horizontally to one side of the straight ahead position, then moved vertically, back down to the horizontal line, then below it and back up again to the horizontal line. The penlight is now moved along the horizontal line to the other side of the straight-ahead position and the same procedure is repeated thus completing the shape of the letter with a wide horizontal dimension. Overaction or underaction of one eye and the patient’s report of diplopia in any position of gaze are recorded to identify the paretic muscle/s.
Brock’s after-image t. See test, after-image transfer.
Brock’s string t. See Brock’s string.
Bruckner’s t. See method, Bruckner’s.
Cardiff acuity t. A test for measuring the visual acuity of young children. It is composed of a series of cards, each with a different picture (either a car, a dog, a duck, a fish, a house or a train) drawn with a white band, which is surrounded by a black line half the width of the white, on a neutral grey background. Thus the average luminance of the target is equal to that of the grey background. The picture is situated either in the top or bottom half of the card. The pictures remain of the same overall size on each card; only the width of the black and white bands decreases in size. There are 11 acuity levels ranging from 6/60 (20/200) to 6/6 (20/20) at a viewing distance of 1 metre, in 0.1 log steps. The acuity is given by the narrowest white band for which the picture is still recognizable, but the child’s eye movements are also noted to confirm or establish recognition. This test is best used with toddlers and children with intellectual impairment (Fig. T4).

See method, preferential looking.
City University colour vision t. A set of 10 pseudoisochromatic plates, each consisting of a central coloured spot surrounded by four differently coloured spots. The subject is asked to choose the spot that most closely matches the colour of the central spot in each plate viewed at a normal reading distance. For each plate there is a normal response and a response corresponding to each of the colour defects, deutan, protan and tritan.
See test, Farnsworth.
colour vision t . See Edridge–Green lantern; plates, pseudoisochromatic; test, City University colour vision; test, Farnsworth; test, lantern; test, wool.
confrontation t. A rough method of determining the approximate extent of the visual field. The patient, with one eye occluded, faces the examiner at a distance of about 60 cm and fixates the opposite eye of the examiner. The test object is moved in a plane midway between the examiner and the patient, starting far in the periphery and moving it towards the patient and in various meridians until it is seen.
contrast sensitivity t. See chart, contrast sensitivity; function, contrast sensitivity; sensitivity, contrast; test, Arden grating; Vistech.
corneal reflex t. See method, Hirschberg’s; method, Javal’s; method, Krimsky’s.
cortical vision screening t. (CORVIST) A test designed to detect visuoperceptual impairments caused by a cerebral disease (e.g. Alzheimer, stroke) or injury, in individuals who have normal or near-normal vision (with or without correction). It consists of an A4-size bound book containing a sequence of ten cards, each one assessing a different aspect of visual processing by cortical centres, and prefaced by a description of its aim, instructions and significance. The test includes symbol acuity, shape discrimination, size discrimination, shape detection, hue discrimination, scattered dot counting, fragmented numbers, word reading, crowding and face perception.
cotton thread t . See test, phenol red cotton thread.
cover t . (CT) A test for determining the presence and the type of heterophoria or strabismus. The subject fixates a small letter or any fine detail at a given distance. Strabismus is usually tested first. The opaque cover or occluder is placed over one eye and then removed, while the examiner observes the other eye and then the same operation is repeated on the other eye (this is called the unilateral cover test). If neither uncovered eye moves, the subject does not have strabismus. If the unoccluded eye moves when a cover is placed in front of the other, strabismus is present. In esotropia the unoccluded eye will move temporally to take up fixation, while in exotropia the unoccluded eye will move nasally, and an upward or downward movement indicates hypotropia or hypertropia, respectively. In alternating squint, in which either eye can take up fixation, the eye behind the cover will appear deviated when uncovered and will move as the cover is shifted to the other eye.
The type of heterophoria can be detected by observing the eye behind the cover. If there is no movement of the eye behind the cover, the subject is orthophoric. If the eye behind the cover moves inward, and outward when the cover is removed, the subject has esophoria. If the eye behind the cover moves outward, and inward when the cover is removed, the subject has exophoria. A similar procedure is used for hyperphoria and hypophoria. As it is difficult to view the eye behind the cover without allowing sufficient peripheral fusion to stop the eyes going to the phoria position, the observer usually watches for the recovery movement as the occluder is removed. By placing prisms of increasing power in front of one of the eyes until no movement is evoked, one can evaluate the approximate amount of the phoria. The cover test is the only objective method of measuring heterophoria. The determination of the magnitude of the deviation of the strabismus or heterophoria can also be done with the alternate (alternating) cover test (ACT). The subject fixates a target and the cover is successively placed in front of one eye and then the other while watching the eye that has just been uncovered to see the direction of the deviation. The amount of deviation can be estimated by using prisms of appropriate strength and base direction until the movement of the eye is neutralized when the cover is alternated from one eye to the other (prism cover test).
Although these tests are objective, they are sometimes used subjectively, i.e. the patient indicates the apparent movement of the fixation object. The alternate cover test is the most appropriate test for subjective testing. An apparent movement of the fixation object in the same direction as the cover indicates exophoria, while an apparent movement of the fixation object in the opposite direction to the cover indicates esophoria. An apparent downward movement of the fixation indicates hyperphoria of the eye from which the occluder is moved. Again prisms can be placed in front of the eyes until the apparent movement disappears, thus giving a measure of the heterophoria. This subjective perception of a movement of a stationary fixation object in people with heterophoria or strabismus is a particular example of the phi phenomenon. Syn. occlusion test; screen test.
cross-cylinder t. for astigmatism A subjective test for measuring the axis and the amount of astigmatism using a cross-cylinder lens. Having obtained the best visual acuity with a spherical lens, the cross-cylinder lens is placed before the eye being tested with its axes at 45° to the cylinder axis determined by retinoscopy. The patient looks at a single circular target, often a letter (O or C or Verhoeff’s circles), the cross-cylinder lens is then flipped and if one position provides a clearer image of the target, the axis of the correcting (minus) cylinder should be turned towards the minus axis of the cross-cylinder lens until vision is equally blurred in both positions of the cross-cylinder lens. That point indicates the correct axis of the correcting cylinder. The determination of the power of the correcting cylinder is carried out by placing the cross-cylinder lens with one of its axes parallel to the axis of the correcting cylinder. The cross-cylinder lens is flipped and the position that provides the clearer vision indicates whether to increase the cylinder power (when the minus axis of the cross-cylinder is parallel) or decrease cylinder power (when the plus axis is parallel). The proper amount of cylinder correction is obtained when the vision is equally blurred in both positions of the cross-cylinder lens. Syn. cross-cylinder method; cross-cylinder test; Jackson crossed cylinder test.
cross-cylinder t. at near A subjective test to determine the addition for near vision. It is performed (monocularly or binocularly) at a distance of usually 40 cm with the patient wearing his or her subjectively determined lenses and cross-cylinder lenses with axes horizontal and vertical and viewing a test chart composed of parallel, horizontal and vertical black lines. Beginning with sufficient fogging lens power, the plus lens power is reduced until the patient reports that the vertical and horizontal lines are equally distinct.
See addition; method, fogging.
dark filter t. See test, neutral density filter.
dark room t. See test, provocative.
dark wedge t. See test, Bielchowsky’s phenomenon.
Denver Developmental Screening t. See test, developmental and perceptual screening.
development and perceptual screening t. A test used to assess children’s perceptual and processing skills, such as gross motor coordination, directionality, laterality, visual form perception, visual memory and visualization, visual-motor integration and auditory and language development. There are many such tests, each evaluating one or several of the above skills. The most common ones are: (1) The Denver Developmental Screening Test (DDST), which is used for children up to about six years of age. It is easy to administer and covers a wide range of skills, which fall into four sectors: personal-social, fine motor-adaptive, language and gross motor. Treatment and/or referral will depend on the type of skills found to be abnormal. (2) The Test of Visual Analysis Skills (TVAS) assesses the child’s visual perceptual skills. It consists of 18 squares containing dots and lines, each forming a different pattern. The child is given a pencil and a special test form on which to reproduce the visual stimuli. The test comes with an expected score for each grade up to grade 3 and failure to reach that score may indicate that the child has a perceptual skills disorder. (3) The Gardner Reversal-Frequency Test in which the child is asked to mark those letters and numbers which are printed backward. This test assesses the directionality skill.
developmental eye movement t. (DEM) An indirect test for saccadic eye movements in which the subject reads numbers placed in four vertical columns (total of 80 numbers) and 16 horizontal rows (total of 80 numbers). The lengths of time taken to perform the horizontal and the vertical subtests are measured independently and assessed as a ratio, as well as the number of errors (omissions, additions, transpositions, or substitutions). All results are compared to test norms for the age of the subject. The vertical array mainly gives an indication of visual-verbal number skills (automaticity), whereas the horizontal array provides additional information on oculomotor function.
differential intraocular pressure t. A test for differentiating between a muscle paresis and a mechanical restriction of the eye. The intraocular pressure is measured in the primary position and then again with the patient turning his or her eyes in the direction of action of the suspected paretic muscle. An increase in intraocular pressure of 6 mmHg or more indicates a mechanical restriction (e.g. a fracture of the orbital floor), whereas no change in pressure suggests a muscle paresis. This test produces less discomfort to the patient than the forced duction test.
See test, forced duction.
diplopia t. 1. A test for measuring heterophoria in which the fusion reflex is prevented by displacing the retinal image of one eye with a prism as in the von Graefe’s test in which the magnitude of the phoria is estimated by the amount of prism necessary to align the two images. To measure lateral phorias the images are displaced vertically and aligned one above the other, whereas to measure vertical phorias the images are displaced horizontally and realigned horizontally (if a phoria is present). Syn. displacement test; prism dissociation test. 2. A test to investigate the integrity of the extraocular muscles in strabismus, in which the patient is required to view a light source in the dark with a red filter in front of one eye and a green filter in front of the other, to produce diplopia (prisms are sometimes necessary). The direction and extent of diplopia are evaluated relative to the size and direction of the angle measured with the cover test at the same distance.
See dissociation; test, red-glass.
displacement t. See test, diplopia.
dissociating t. Any test for measuring heterophoria in which fusion is dissociated.
See dissociation; Maddox rod; test, diplopia.
distortion t. A test for measuring heterophoria, in which the images presented to the two eyes are so unlike that they cannot be fused. The most common such test is the Maddox rod test.
doll’s head t. See phenomenon, doll’s head.
Dolman’s t. See test, hole in the card.
double-blind t . See study, double-blind.
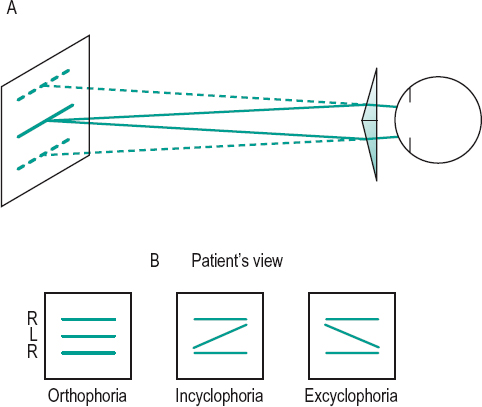
double prism t . A test for determining the presence of cyclophoria, in which a double prism (a pair of prisms set base to base) with the base line horizontal is placed before one eye. The patient is requested to fixate a horizontal line (or row of letters), which through the double prism appears as two lines (or two rows) vertically separated. On uncovering the other eye, the patient sees three lines (or rows). If there is no cyclophoria, all three lines (or rows) will appear parallel, but lack of parallelism indicates cyclophoria. The double prism used in this test consists of two weak prisms (about 4 or 5 Δ): this clinical type of double prism is commonly called a Maddox double prism (Fig. T5).
See bi-prism, Fresnel’s; test, Maddox rod.
Dunlop t. A test for determining motor ocular dominance. It consists in having the eyes fusing two slightly different targets in, for example, a synoptophore, and diverging the targets until diplopia appears. Just beforehand, fixation disparity occurs in one eye. That eye is called the non-dominant or non-reference eye. The other eye is the dominant or reference eye.
duochrome t. A subjective refraction test in which the subject compares the sharpness of black targets (e.g. Landolt rings) of similar sizes, on a red background on one side and on a green background on the other side (blue is sometimes used) of a chart. In undercorrected myopia or overcorrected hyperopia, the letters on the red background will appear more distinct, while in overcorrected myopia or undercorrected hyperopia the letters on the green background will appear more distinct, and in emmetropia or corrected ametropia the letters should appear equally distinct on both sides. The test makes use of the chromatic aberration of the eye and assumes that when the eye is looking at distant objects it is focused on the yellow part of the visible spectrum. Syn. bichrome test; duochrome method.
See lens, cobalt; Verhoeff’s circles.
dye dilution t. A test for detecting a blockage in the lacrimal (or drainage) system. It consists of instilling a few drops of fluorescein (or a mixture of rose bengal and fluorescein) into the conjunctival sac and observing how long it takes before it dilutes which is shown by the change in colour. No change in colour indicates a blockage or a lack of tear production.
See lacrimal apparatus; staining, fluorescein; test, Jones 1.
‘E’t. See ‘E’ game; chart, illiterate E.
equalization t. See test, balancing.
Esterman t. A method of quantifying visual field disability. It consists of a grid made up of rectangles of different sizes placed across the field, being smaller centrally, inferiorly and along the horizontal meridian than at other locations, as these areas are considered to be most important functionally. Each rectangle contains a dot in the centre. There is a grid for the monocular field with 100 rectangles and a grid for the binocular field with 120 rectangles. The grid is placed on top of the results of the field chart. A percentage score is calculated on the basis of the number of spots seen by the patient. The grids are incorporated into most automated perimeters.
fan and block t. A test for determining the axis and the amount of astigmatism of the eye. It consists of an astigmatic fan chart with an inner rotating central disc on which are printed an arrowhead forming an acute angle of typically 60° and two sets of mutually perpendicular lines or ‘blocks’. The test follows the subjective determination of the best vision sphere that places the circle of least confusion on the retina. A positive spherical lens, of a power equal to half the estimated amount of astigmatism, is placed in front of the eye to create simple myopic astigmatism. The patient is asked to indicate the clearest line(s) on the chart and the arrowhead is rotated until its two sides appear equally blurred. The axis of the correcting negative cylindrical lens is then read on the fan chart. The amount of astigmatism is found when that cylindrical lens is of a power such that the two blocks appear equally clear. Syn. fan and block method.
See chart, astigmatic fan; method, fogging.
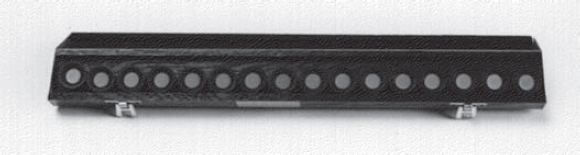
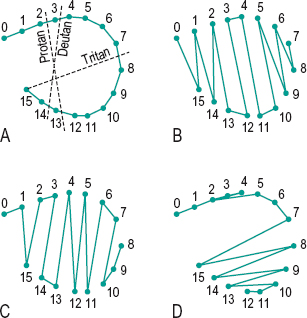
Farnsworth t. A colour vision test consisting of 85 small discs made up of Munsell colours of approximately equal chroma and value, but of different hue for normal observers. The examinee must place the discs so that they appear in a continuous and smooth series. Errors are scored and a diagnosis of the type and severity of the colour defect can be made. A smaller version of the Farnsworth test called the Farnsworth D-15 exists (Figs. T6 and T7). It consists of only 15 small discs and the procedure is the same, but it is a more rapid test, which does not give as much information as the large version. However, it has been found to be very valuable for detecting severe colour vision defects, including tritanopia. There exist also some versions of this test in which the colour samples are less saturated than the standard ones: (1) The Lanthony desaturated D-15 test in which the colour samples are less saturated by 2 units of Munsell chroma but also lighter by 3 units of Munsell value than the standard D-15 test, and (2) the Adams desaturated D-15 test in which only the saturation (or chroma) has been reduced by 2 units. These desaturated D-15 tests are more effective in detecting mild colour vision deficiencies than the standard D-15 test. Syn. Farnsworth–Munsell 100 Hue test (or FM 100 Hue test).
See colour vision, defective; lamp, Macbeth; Munsell colour system; test, City University colour vision.
Farnsworth–Munsell 100 Hue t. See test, Farnsworth.
fluorescein t . 1. A test to assess the fit of hard contact lenses. Fluorescein is instilled between the cornea and the contact lens and under ultraviolet illumination areas where the lens touches the cornea appear purple or blue, whereas areas where there is a space between the lens and the cornea appear yellowish green. This appearance is often referred to as fluorescein pattern. 2. Test using fluorescein and ultraviolet illumination to detect abrasions or other corneal epithelial defects, which stain yellowish green.
See bearing, apical; lamp, Burton; rose bengal; staining; test, Jones 1; test, Jones 1.
fogging t. See method, fogging.
forced duction t. A test for differentiating between a muscle paresis and a mechanical restriction of the eye. The eye in which the conjunctiva is anaesthetized is grasped with toothless forceps and passively rotated in the direction of action of the suspected paretic muscle. If the eye cannot be rotated further than the point where the patient can voluntarily rotate it, a mechanical restriction exists (e.g. a fracture of the orbital floor): if the examiner can passively rotate the eye to its full extent, the muscle is paretic. Syn. traction test.
See paralysis of the third nerve; strabismus fixus; syndrome, Brown’s superior oblique tendon sheath; test, Bielschowsky’s head tilt; test, three-step.
four dot t. See test, Worth’s four dot.
four prism dioptre base-out t . A test for the detection of microstrabismus (microtropia) and for the assessment of the suppression area. A 4 Δ BO is placed momentarily in front of the fixating eye (or the eye with the best acuity) and if the other eye moves outward but does not refixate inward it indicates suppression in that eye and a small angle strabismus. Microstrabismus is also indicated if, when the prism is placed BO in front of the eye that showed suppression, there is no movement of either eye. The extent of the suppression area can be assessed by momentarily placing prisms, of various powers and in various directions, in front of the affected eye until diplopia is noticed. The observation of the patient’s eye movements is difficult because of the small angle of deviation and because of the variation in size of the suppression area. Syn. Irvine’s prism displacement test.
See microtropia.
FRIEND t. A subjective test for simultaneous binocular vision in which the word FRIEND printed with the letters FIN in green and RED in red is viewed through red and green filters, one before each eye. People with simultaneous binocular vision see all the letters, whereas those with suppression see only some of the letters.
See test, Worth’s four dot.
Frisby stereo t. See stereotest, Frisby.
Gardner Reversal-Frequency t . See test, developmental and perceptual screening.
gradient t. See AC/A ratio.
von Graefe’s t. See test, diplopia.
Hering after-image t. See test, after-image.
Hess–Lancaster t. A test for measuring and classifying strabismus using the Hess screen.
Hirschberg’s t. See method, Hirschberg’s.
hole in the card t . A test for determining which eye is dominant. It consists of a card with a hole in it, through which the patient views a spotlight (or a letter) on a distant test chart while holding the card with both hands. The eye that the patient uses to view the letter is the dominant eye. This is easily detected by having the patient occlude each eye in turn and when the dominant eye is covered the spotlight can no longer be seen through the hole. Syn. Dolman’s test.
See dominance, ocular; manoptoscope.
hole in the hand t . A test for binocular vision in which a distant object is viewed through a tube with one eye while a hand is placed against the tube at a distance of some 20–30 cm before the other eye. Subjects who see the object through an apparent hole in the hand have binocular vision, whereas seeing either the object through the tube only or the hand only indicates an absence of binocular vision. Syn. hole in the hand illusion.
Holmgren’s t. See test, wool.
Howard–Dolman t . A test for measuring stereoscopic visual acuity consisting of two black vertical rods on a white background, viewed through an aperture from a distance of 6 m. By means of a double cord pulley arrangement, the subject manipulates one of the rods until it appears in the same plane as the fixed rod. The distance between the two rods is then measured, and calculations must be made to arrive at the acuity.
See test, three-needle; test, two-dimensional.
Humphriss immediate contrast t. See method, Humphriss.
infinity balance t. See test, Turville infinity balance.
Irvine’s prism displacement t. See test, four-prism dioptre base-out.
Ishihara t. See plates, pseudoisochromatic.
Jackson crossed cylinder t . See test for astigmatism, cross-cylinder.
Jones 1 t. A test to evaluate the tear drainage system. Fluorescein dye is instilled into the conjunctival sac. Over a period of five minutes at one-minute intervals, a cotton-tipped applicator is placed under the anaesthetized inferior nasal turbinate. Absence of dye suggests a blockage somewhere in the passage, the nasolacrimal duct being the most common site. Jones 2 test may then be performed. Syn. fluorescein instillation test; primary Jones test.
Jones 2 t. After Jones 1 test, fluorescein is washed out and physiological saline is injected into the anaesthetized lower canaliculus. If the fluid recovered from the nose is fluorescein-stained the test is positive indicating a partial obstruction in the nasolacrimal duct, otherwise there is a blockage in the punctum, canaliculus or common canaliculus or a defective pumping mechanism of the tears.
See lacrimal apparatus; test, dye dilution.
Krimsky’s t. See method, Krimsky’s.
Lang t . See stereotest, Lang.
lantern t. An occupational colour vision test used mainly to evaluate recognition of aviation and maritime signals. There are several such tests (e.g. Edridge–Green lantern, Giles–Archer lantern, Holmes–Wright lantern, Farnsworth lantern or Falant). The latter two show colours in pairs of which there are nine and the observer’s task is to name the colours.
light-stress t. See test, photostress.
log MAR crowded t. See Glasgow acuity cards.
Maddox rod t. 1. See Maddox rod. 2. A test for measuring cyclophoria in which a Maddox rod is placed in front of each eye, with axes parallel, while the subject views a spot light through a 10 to 15 Δ prism (to displace one image relative to the other). The subject will then see two streaks. If they appear parallel there is no cyclophoria. If not, one of the Maddox rods is rotated slowly until the subject reports that the two streaks are parallel. The angle of rotation as determined with a protractor scale indicates the amount of cyclophoria.
See test, double-prism.
Maddox wing t . See Maddox wing.
Mallett t. See Mallett fixation disparity unit.
manoptoscope t. See manoptoscope.
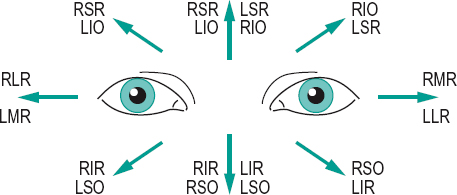
motility t. A test aimed at investigating the integrity of the extraocular muscles and their innervation. The most common method is to have the patient fixate a penlight, which is moved in eight meridians while keeping the head still: up, up and to the right, right, down and to the right, down, down and to the left, left, up and to the left, following a star pattern. The test can be done either binocularly or monocularly. Such movements will test the action of all six extraocular muscles of both eyes. If, for example, the penlight is moved up and to the right of the patient, any limitation in movement indicates a fault in either the right superior rectus or the left inferior oblique muscle (Fig. T8).
See movement, pursuit; muscles, yoke; pattern, A; pattern, V; positions of gaze, cardinal; positions of gaze, diagnostic; test, broad H; test, red-glass.
neutral density filter t. A test to differentiate between functional and organic amblyopia by measuring visual acuity, with or without a neutral density filter. If acuity is greatly reduced when looking through the filter, the amblyopia is organic (e.g. glaucoma, central retinal lesions), but if the acuity is unaffected or even slightly improved, the amblyopia is functional. The validity of this test has been questioned. Syn. Ammann’s test; dark filter test.
New Aniseikonia t. A test for measuring aniseikonia. It consists of a booklet with pairs of half-moons, one green, the other red, and of different sizes. The patient wears red and green filters and is asked to point to the set of half-moons that appear to have identical vertical diameters. If the sizes are actually equal the patient has no vertical aniseikonia; if the sizes are actually unequal the patient has vertical aniseikonia of a percentage amount indicated next to the target. The booklet is rotated to a horizontal position to measure the horizontal aniseikonia.
non-invasive break-up time t. (NIBUT) A test that does not require any interference with the eye used for assessing the stability of the precorneal tear film. The patient’s head rests on a chin rest at the centre of a hemispherical bowl of 20 cm radius, which is attached at the apex to a binocular microscope. A grid of white lines on a matt black background is inscribed on the inner surface of the bowl and the image of this grid pattern projected onto the open eye is observed. The subject fixates a hole in the centre of the grid pattern and refrains from blinking. The time taken for the appearance of the first randomly distributed distortion or discontinuity of some of the reflected grid lines is a measure of the precorneal tear film break-up. The values for normal subjects vary between 5 and 200 seconds with a mean of around 40 seconds. The instrument used to measure NIBUT is often referred to as a toposcope.
See Tearscope plus; test, break-up time.
Norn’s t . A test for assessing tear secretion. It consists of instilling one drop of a mixture of 1% fluorescein and 1% rose bengal into the lower conjunctival sac. After five minutes a slit-lamp examination is made of the colour of the stain in the central portion of the tear meniscus along the lower lid. The colour may be compared either with known dilutions of the mixture in capillary tubes or simply classified into five colours: intense red, pale red, intense orange, weak orange and yellow. In normal eyes the colour is yellow or weak orange whereas in a dry eye it is red. Syn. tear dilution test.
See eye, dry; keratoconjunctivitis sicca; test, break-up time; test, non-invasive break-up time; test, phenol red cotton thread; test, Schirmer’s.
t. object See test type.
ocular ferning t . A test for the assessment of ocular mucus. Conjunctival scraping are placed on a glass slide, left to dry and examined under the microscope for the presence or absence of arborization (fernlike pattern). Normal eyes show ferning whereas in patients with cicatrizing conjunctivitis, such as ocular pemphigoid or Stevens–Johnson syndrome, ferning of the mucus is reduced or absent.
See pemphigoid, cicatricial.
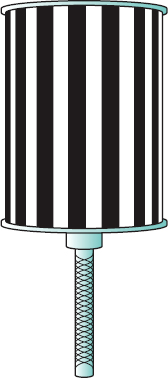
optokinetic nystagmus t. (OKN) A test for eliciting OKN. The subject sits in front of a rotating drum covered with uniform black and white vertical stripes parallel to the axis of rotation (this apparatus is called an optokinetoscope or optokinetic drum). When the eyes respond with a slow movement in the same direction as the drum lasting about 0.2 s, and a fast phase in the reverse direction of about 0.1 s, the OKN has been elicited and this fact provides evidence of vision. As finer and finer black and white stripes are used, this reflex response will cease to be elicited for a particular spatial frequency of the stripes corresponding to the objective visual acuity of the subject (Fig. T9).
See malingering; nystagmus.
Parks three-step t . See test, three-step.
Pepper t . A test for assessing reading performance in low vision patients. It emphasizes the visual rather than the cognitive component of reading. Thus, each chart consists of unrelated letters and words, rather than continuous text. Each row contains either separate letters (at the top of the chart) or separate words (of increasing length in the lower portion of the chart), all of the same size. Missing the first or last half of the word indicates the position of the scotoma relative to the fixation point. The rows at the top of the chart are triple line spaced, they are double line spaced in the middle and single line spaced at the bottom, thus requiring more and more exacting saccadic eye movements. There are five charts, each of different sized print. A reading rate, such as the number of correct units read per minute, can be determined with this test. Syn. Pepper Visual Skills for Reading Test (VSRT).
phenol red cotton thread t. A test for measuring tear secretion. It is accomplished by using a special cotton thread, impregnated with phenol red dye. The thread is inserted under the lower eyelid for 15 seconds, and both eyes are closed. The absorption of tears is determined by the length of thread that has turned from red to yellow (due to the pH of tears). The average length varies between 3 and 48 mm, and less than 9 mm is usually indicative of a dry eye. This test is much quicker and much less uncomfortable than Schirmer’s test and has good reliability. However, questions have been raised as to whether it is the actual secretion rate that is being measured. There exist several cotton thread tests to measure tear secretion, using different cottons of different lengths and diameters and some are used without phenol red dye.
See tear secretion; test, Norn’s; test, Schirmer’s.
phi phenomenon t. of Verhoeff See movement, phi.
photostress t. A test to differentiate the cause of a reduced visual acuity in one eye, between a lesion in the optic nerve and a disease in the fundus of the eye. A bright light is directed into the eye with the best acuity, for 10 seconds, while the defective eye is covered. The light is then removed and the patient is instructed to read the line just above the best visual acuity line for that eye. The time taken until the patient can just read that line is recorded. The same procedure is then repeated with the defective eye. If the recovery time is about the same in both eyes, the cause of the reduced visual acuity is an optic nerve lesion (e.g. retrobulbar optic neuritis); if the recovery time is much longer for the defective eye the cause is in the fundus (e.g. retinal oedema, retinopathy, age-related macular degeneration). The latter is attributed to a delay in the regeneration of visual pigments after being bleached with a bright light. Syn. light-stress test.
plus 1.00 D blur t . A check test used to verify a patient’s spherical correction or to determine whether a person is hyperopic. It consists of placing a +1.00 D lens in front of the eye: visual acuity should be reduced from 6/6 (20/20) to about 6/18 (20/60). If the patient can still read smaller letters than 6/18, the spherical prescription is incorrect or the patient is hyperopic. This result could also be due to a much smaller pupil than average. This test is most helpful with young children as it helps relax accommodation. Syn. blur back test.
See hyperopia, absolute; method, fogging.
prism adaptation t. A prognostic test in cases of esotropia (convergent strabismus), indicating whether surgical intervention is favourable or not. Prior to the intervention, the patient has to wear a BO prism, of an amount larger than the angle of deviation, for an hour or more. An increase in the angle of deviation is an unfavourable prognosis and no increase or a decrease is considered favourable.
prism cover t. See test, cover.
prism dissociation t. See test, diplopia.
prism reflex t. See method, Krimsky’s.
prone position t. See test, provocative.
provocative t. A test performed to reproduce signs of a suspected disease in order to help in the diagnosis of that disease. A common provocative test for open-angle glaucoma is the water-drinking test in which a fasting patient has to drink one quart of water (or about 1 litre in a 70 kg adult) within five minutes. The intraocular pressure (IOP) is measured before the water is taken and then at 15-minute intervals. An increase of 8 mmHg or more in 45 minutes is considered positive. Two common provocative tests for angle-closure glaucoma are: (1) The dark room test in which the patient is kept in a dark room for 1 hour and the IOP is measured before and after the test. An increase of 8 mmHg or more is generally considered positive. (2) The prone position test in which the patient lies in the prone position for 1 hour and if the IOP increases by 8 mmHg or more, compared with the value before the test, the result is considered positive. In open-angle glaucoma provocative tests have been found to be positive in less than half of the patients but that figure is higher in angle-closure glaucoma.
Purkinje tree t. See angioscotoma.
push-up t. 1. See method, push-up. 2. A procedure used to ensure adequate lens movement of a soft contact lens. The lens is gently pushed upward by pressing on the patient’s lower eyelid: it should move easily and return quickly to its original location.
random-dot E t. See stereogram, random-dot.
Raubitschek t. See chart, Raubitschek.
red glass t. A test for determining diplopia or suppression in which a bright target (e.g. a white light) is fixated while a red filter is held in front of one eye to interrupt fusion. The patient with diplopia will see a red light and a white light. The amount of deviation can be estimated by using a prism of an amount such that it eliminates the double image. The operation can be repeated in all the diagnostic positions of gaze to help identify a paretic extraocular muscle as the distance between the two images increases in the field of action of the paretic muscle. If only one light is seen it indicates suppression of one retinal image. Syn. red filter test.
See action, primary; test, diplopia; test, motility.
Scheiner’s t . A test for measuring the monocular near point of accommodation. It consists of using a Scheiner’s disc in front of the eye, which observes a small target such as a thin black line. The target is moved towards the eye until it is no longer seen single. That point represents the near point of accommodation.
See experiment, Scheiner’s.
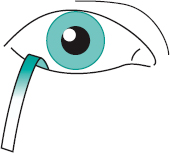
Schirmer’s t . A test for measuring tear secretion. It is accomplished by using a 35 × 5 mm strip of filter paper (e.g. Whatman No. 41). The filter strip is folded so that one end, about 5 mm long, is inserted at the mid-portion (or lateral portion) of the lower eyelid of a patient seated in a dimly lit room. Tear secretion is considered normal if 10 mm or more of the paper from the point of the fold becomes wet in a four-minute period. More than 25 mm of wetting would indicate excessive tear secretion. Without any additional stimulation of any kind the test, called Schirmer’s test 1, measures mainly the basal tear production, but because the filter paper tends to irritate the conjunctiva, some of the reflex tear secretion may be also be measured as well. Schirmer’s test 2 is aimed at measuring mainly reflex tear secretion. It is carried out with the filter paper inserted inside the lower lid of an eye with topical anaesthesia, while the contralateral half of the nasal mucosa is irritated by rubbing it with a dry cotton-tipped applicator. The amount of tear production is measured after two minutes. A value of more than 15 mm is considered to be normal and less than 15 mm may indicate a deficiency of reflex tear secretion (Fig. T10).
See alacrima; keratoconjunctivitis sicca; tear secretion; test, Norn’s; test, phenol red cotton thread.
sessile drop t. Measurement of the contact angle by observation of the formation of a drop of liquid on a solid surface. The image of the droplet may be photographed or projected.
shadow t. 1. A test that gives an approximate evaluation of the depth of the anterior chamber. It is carried out by placing a penlight on the temporal side of the eye at the level of the pupil and directing the beam of light horizontally towards the inner side of the eye. If the iris lies in a flat plane, which usually indicates a deep anterior chamber, the entire iris will be illuminated. If the iris is directed anteriorly, which usually indicates a narrow anterior chamber, the iris on the temporal side of the eye will be illuminated but the iris on the nasal side will be shadowed to varying degrees depending on the narrowness of the anterior chamber (Fig. T11). Syn. oblique illumination shadow test. 2. See retinoscopy. 3. A test for the homogeneity of a lens (both material and surface quality) in which the light from a small, intense source of light passes through the lens and falls on a screen. Any defects will show as shadows.
See angle of the anterior chamber; method, van Herick, Shaffer and Schwartz; method, Smith’s.
Sheridan–Gardiner t. A visual acuity test consisting of a large card (called the key card) which is held by the patient who is asked to point to the letter on that key card that is the same as the letter shown on the distance (or near) chart. The test consists of several cards with single letters of various sizes. It is most useful for testing children and illiterates.
Simultan t. See Simultantest.
stereotest t. See stereotest, Frisby; stereotest, Lang; vectogram.
swinging flashlight t . See pupil, Marcus Gunn.
t. target See test type.
tear t. See cytology, impression; rose bengal; test, basic secretion; test, break-up time; test, non-invasive break-up time; test, ocular ferning; test, phenol red cotton thread; test, Schirmer’s.
tear dilution t. See test, Norn’s.
Thorington t. A test for the measurement of heterophoria at near and at distance. It consists of a horizontal row of letters on one side of a light source and a horizontal row of numbers on the other side of that source. A Maddox rod, orientated horizontally, is placed in front of one eye and the patient who is fixating the light source is asked to report through which letter or number the vertical streak appears to pass, or to which it is closest. At 6 m the number of letters must be placed 6 cm apart to represent 1 Δ steps. If the Maddox rod is in front of the right eye, the numbers on the right side of the source and the letters on the left, each number represents 1 Δ of esophoria and each letter represents 1 Δ of exophoria. The Thorington test can also be used at near. At 40 cm, for example, the separation of the letters and numbers must be 0.4 cm to represent 1 Δ. It can also be placed vertically with the Maddox rod orientated vertically to measure vertical heterophoria.
three-dimensional t. See test, two-dimensional.
three-needle t. A test for measuring stereoscopic visual acuity consisting of three fine rods placed vertically, two of them being fixed in the same plane, while the third one is movable in between. The subject views them through an aperture. The centre rod is placed in various positions backward and forward until the subject judges whether it is nearer or farther than the others (Fig. T12).
See stereopsis; test, Howard–Dolman.
three-step t. An objective test for determining which extraocular muscle is paretic in a patient with hypertropia. A three-step procedure is used: (1) to determine the type of hypertropia (right or left); (2) to determine the magnitude of the hypertropia (e.g. with prisms and cover test) when the patient fixates to the right and to the left; (3) to determine the magnitude of the hypertropia when the head is tilted towards each shoulder. Each step in this procedure reduces the number of possible muscles involved until it points to only one muscle of one eye. Example: paresis of the left superior oblique. Step (1) a left hypertropia points to a paresis of one of the following four muscles: left superior oblique, left inferior rectus, right inferior oblique or right superior rectus. Step (2) a hypertropia of the left eye increases when fixating to the right points to a paresis of either the left superior oblique or the right superior rectus. Step (3) a hypertropia of the left eye which increases when the head tilts to the left, points to a paresis of the left superior oblique. Syn. Parks three-step test.
See test, Bielschowsky’s head tilt; test, forced duction.
Titmus stereo t. See vectogram.
Turville infinity balance t. (TIB) A test for balancing the accommodative state of the eyes. It can also be used for detecting suppression, vertical and horizontal associated phorias and (with a target composed of two horizontal lines) aniseikonia in the vertical meridian. It consists of a 3 cm-wide vertical septum placed in the centre of a mirror on which is reflected a reversed illuminated chart. Thus the patient can only see the right side of the chart with the right eye, and the left side with the left eye, which allows for simultaneous comparison of the chart seen by both eyes, while still retaining fusion for peripheral objects near the border of the chart. If the chart is projected onto a screen, the septum is placed halfway between patient and screen. The test is carried out after the conventional refractive procedures. Syn. infinity balance test.
See balance, binocular; heterophoria, associated; suppression; test, balancing.
two-dimensional t. A test for stereopsis consisting of two-dimensional objects as test material such as targets, cards, etc. as used in a stereoscope or a major amblyoscope (e.g. random-test stereogram; Titmus stereotest). Other tests for stereopsis are three-dimensional (3-D), the Howard–Dolman test being the most well known. Two-dimensional tests (2-D) are the most commonly used in clinical practice.
See stereogram, random-dot; stereoscope; stereo-test; test, Howard–Dolman; vectogram.
t. type Any letter, figure or character used for vision testing. The term test object (Syn. test target) is a more general term, which encompasses any pattern or object (e.g. checkerboard, grating).
See chart; grating; Jaeger test type; König bars; Landolt ring; optotype; pattern, checkerboard.
Verhoeff phi phenomenon t. See movement, phi.
t. of Visual Analysis Skills See test, developmental and perceptual screening.
water-drinking t. See test, provocative .
Welland’s t. See test, bar reading.
wool t. A test for assessing colour vision deficiencies. It consists of a set of wool strands, which are to be matched with loose wool strands of the same colour. The bestknown of these is the Holmgren’s test. Syn. colour wool test.
Worth’s four dot t. A test for determining the presence of binocular vision. It consists of four illuminated discs: two green, one red and one white on a black background. The test is viewed at any distance by a subject wearing red and green filters such that one eye sees the red and the white discs, while the other eye sees the two green discs and the white disc. Subjects are asked to report how many dots they see: four dots indicates normal binocular vision; two dots, both red, indicates suppression of the image in the eye wearing the green filter; three dots, all green, indicates suppression of the image in the eye wearing the red filter; and five dots, two red and three green, indicates diplopia. Syn. four-dot test.
See suppression; test, FRIEND; vision, Worth’s classification of binocular.
testing in parallel Clinical test performed in such a way that different parameters are examined simultaneously. The effect of one parameter on another can be noticed and the final results appropriately altered. Examples: Parallel-Testing Infinity Balance test; Parallel-Testing Near Balance test; Turville Infinity Balance test.
testing in series Clinical tests performed one after the other. Each parameter is measured and corrected and assumed to remain fixed afterward.
tetracaine hydrochloride (amethocaine hydrochloride) A topical corneal anaesthetic, commonly used in 0.25–1% solution. It may be used to carry out tonometry, to remove a foreign body, etc.
tetrachromatic theory See theory, Hering’s of colour vision.
tetracycline See antibiotic.
textural gradient One of the monocular cues of depth perception produced by the change in the appearance of the grain of the structure of a surface, giving the impression that the thin, small details must be further away than the thick, large ones (Fig. T13).
See perception, depth.
thalamus One of a pair of ovoid masses of grey substance that serves as a relay station for sensory stimuli to the cerebral cortex. It contains the lateral geniculate body, which is a continuation of the pulvinar and which is situated at the posterior end of the thalamus.
See geniculate bodies, lateral.
theory An explanation of the manner in which a phenomenon occurs, has occurred, or will occur.
Bielschowsky’s t. See theories of strabismus.
biological-statistical t. Theory of the development of refractive errors, based on the way in which the refractive components of the eye combine. It postulates a high correlation between the normally distributed refractive components to produce emmetropia. A breakdown of this correlation leads to ametropia. This theory depends essentially on hereditary factors.
See gene-environment interaction; myopia control; myopia, physiological; theory, emmetropization; theory, use-abuse.
Chavasse’s t . See theories of strabismus.
corpuscular t . See theory, Newton’s.
Donders’ t . See theories of strabismus.
Duane’s t . See theories of strabismus.
duplicity t. The theory that vision is mediated by two independent photoreceptor systems in the retina: diurnal or photopic vision through the cones when the eyes see details and colours; and nocturnal or scotopic vision through the rods when the eyes see at very low levels of luminance. It can be illustrated when establishing a dark adaptation curve (sensitivity as a function of time), which is preceded by a bright preadaptation stimulus. The curve typically has two branches: and initial increase in sensitivity (i.e. lower light threshold) followed by a plateau, due to cone adaptation; then another increase in sensitivity followed by a plateau due to rod adaptation.
See interval, photochromatic; Purkinje shift; theory, two visual systems; vision, photopic; vision, scotopic.
emission t. See theory, Newton’s.
emmetropization t. A theory that explains the phenomenon of emmetropization on a biofeedback mechanism, involving cortical and subcortical control of the various components of the eye that contribute to its refractive power.
empiricist t. Theory that certain aspects of behaviour, perception, development of ametropia, etc. depend on environmental experience and learning, and are not inherited.
See empiricism; theory, nativist.
Fincham’s t. Theory of accommodation which attributes the increased convexity of the front surface of the crystalline lens, when accommodating, to the elasticity of the capsule and to the fact that it is thinner in the pupillary area than near the periphery of the lens.
See capsule; theory, Helmholtz’s of accommodation.
first order t. See theory, gaussian.
gaussian t. The theory that for tracing paraxial rays through an optical system, that system can be considered as having six cardinal planes: two principal planes, two nodal planes and two focal planes. The mathematical analysis can be carried out by the paraxial equation. Syn. first order theory; paraxial theory.
See Newton’s formula; optics, paraxial; paraxial equation, fundamental; ray, paraxial.
von Graefe’s t. See theories of strabismus.
Helmholtz’s t. of accommodation The theory that in accommodation the ciliary muscle contracts, relaxing the tension on the zonule of Zinn while the shape of the crystalline lens changes, resulting in increased convexity, especially of the anterior surface. Fincham’s theory complements that of Helmholtz.
See accommodation; theory, Fincham’s; Zinn, zonule of.
Helmholtz’s t. of colour vision See theory, Young–Helmholtz.
Hering’s t. of colour vision Theory that colour vision results from the action of three independent mechanisms, each of which is made up of a mutually antagonistic pair of colour sensations: red-green, yellow-blue and white-black. The latter pair is supposed to be responsible for the brightness aspect of the sensation, whereas the former two would be responsible for the coloured aspect of the sensation. Syn. opponent-process theory; tetrachromatic theory.
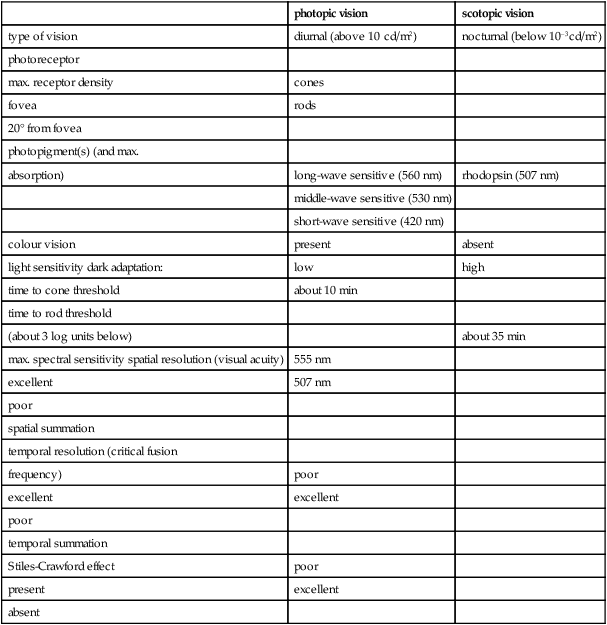
Table T1
Main characteristics of the photopic and scotopic visual system
| photopic vision | scotopic vision | |
| type of vision | diurnal (above 10 cd/m2) | nocturnal (below 10–3cd/m2) |
| photoreceptor | ||
| max. receptor density | cones | |
| fovea | rods | |
| 20° from fovea | ||
| photopigment(s) (and max. | ||
| absorption) | long-wave sensitive (560 nm) | rhodopsin (507 nm) |
| middle-wave sensitive (530 nm) | ||
| short-wave sensitive (420 nm) | ||
| colour vision | present | absent |
| light sensitivity dark adaptation: | low | high |
| time to cone threshold | about 10 min | |
| time to rod threshold | ||
| (about 3 log units below) | about 35 min | |
| max. spectral sensitivity spatial resolution (visual acuity) | 555 nm | |
| excellent | 507 nm | |
| poor | ||
| spatial summation | ||
| temporal resolution (critical fusion | ||
| frequency) | poor | |
| excellent | excellent | |
| poor | ||
| temporal summation | ||
| Stiles-Crawford effect | poor | |
| present | excellent | |
| absent |
See cells, colour-opponent; theory, Young–Helmholtz.
van der Hoeve’s t . See theories of strabismus.
Landolt’s t . See theories of strabismus.
lattice t . See theory, Maurice’s.
Luneburg’s t. A theory according to which the geometry of the visual space is described by a variable non-euclidean hyperbolic metric.
Mackenzie’s t. See theories of strabismus.
Maurice’s t. Theory that explains the transparency of the stroma of the cornea. It states that the stromal fibrils, which have a refractive index of about 1.55 in the dry state, are so arranged as to behave as a series of diffraction gratings permitting transmission through the liquid ground substance (refractive index 1.34). The fibrils are the grating elements that are arranged in a hexagonal lattice pattern of equal spacing and with the fibril interval being less than the wavelength of light. The diffraction gratings eliminate scattered light by destructive interference, except for the normally incident light rays. Light beams that are not normal to the cornea are also transmitted to the oblique lattice plane. However, recent work has demonstrated inconsistencies in lattice space and there is some modification to the original postulate of this theory. Syn. lattice theory.
nativist t. Theory that certain aspects of behaviour, perception, development of ametropia, etc. are inherited and independent of environmental experience.
See gene-environment interaction; nativism; theory, empiricist.
Newton’s t. The theory that light consists of minute particles radiated from a light source at a very high velocity. Syn. corpuscular theory; emission theory.
See theory, quantum; theory, wave.
Nordlow’s t. See theories of strabismus.
opponent-colour t. See theory, Hering’s of colour vision.
paraxial t. See theory, gaussian.
Parinaud’s t. See theories of strabismus.
Planck’s t. See theory, quantum.
quantum t . Theory that radiant energy consists of intermittent and spasmodic, minute indivisible amounts called quanta (or photons). This is a somewhat modern version of the theory originally proposed by Newton. Syn. Planck’s theory.
See photon; theory, Newton’s; theory, wave.
Scobee’s t. See theories of strabismus.
t. of strabismus See theories of strabismus.
three-component t. See theory, Young–Helmholtz.
trichromatic t. See theory, Young–Helmholtz.
two visual systems t. The theory that there are two distinct modes of processing visual information: one pertaining to the identification (or ‘what’ system) and the other to localization (or ‘where’ system) of visual stimuli. The identification mode is concerned with resolution and pattern vision, and is associated with the foveal and parafoveal regions of the retina. It is subserved by primary cortical mechanisms. The localization mode is concerned with motion and orientation and is subserved by midbrain visual structures.
See system, magnocellular visual; system, parvocellular visual; theory, duplicity.
use-abuse t. Theory that attributes the onset of myopia to an adaptation to the use or misuse of the eyes in prolonged close work with the concomitant lag of accommodation and hyperopic defocus. Environmental factors would be the main cause of myopia.
See myopia control; theory, biological-statistical.
wave t. Theory that light is propagated as continuous waves. This theory was quantified by the Maxwell equations. The wave theory of light can satisfactorily account for the observed facts of reflection, refraction, interference, diffraction and polarization. However, the interchange of energy between radiation and matter, absorption and the photoelectric effect are explained by the quantum theory. Both the wave and quantum theories of light were combined by the concept of quantum mechanics, and light is now considered to consist of quanta travelling in a manner that can be described by a waveform. Syn. Huygens’ theory.
See photon; theory, quantum; wavelength.
Worth’s t. See theories of strabismus.
Young–Helmholtz t. The theory that colour vision is due to a combination of the responses of three independent types of retinal receptors whose maximum sensitivities are situated in the blue, green and red regions of the visible spectrum. This theory has been shown to be correct, except that the pigment in the third receptor has a maximum sensitivity in the yellow and not in the red region of the spectrum. Hering’s theory of colour vision, which explains phenomena at a level higher than that of the cone receptors, complements this theory. Syn. Helmholtz’s theory of colour vision; three components theory; trichromatic theory.
See pigment, visual; theory, Hering’s of colour vision.
theoretical eye See eye, reduced; eye, schematic.
therapeutic soft contact lens See lens, therapeutic soft contact.
thimerosal See antiseptic.
third-degree fusion See stereopsis; vision, Worth’s classification of binocular.
third cranial nerve See nerve, oculomotor.
third nerve paralysis See paralysis of the third nerve.
Thorington test See test, Thorington.
Thorpe four-mirror fundus lens See slit-lamp.
three and nine o’clock staining See staining, 3 and 9 o’clock.
three-dimensional Pertaining to depth perception or the illusion of depth (e.g. a perspective drawing).
three-needle test See test, three-needle.
threshold The value of a stimulus that just produces a response. Syn. limen.
absolute t. The minimum luminance of a source that will produce a sensation of light. It varies with the state of dark adaptation, the retinal area stimulated, the wavelength of light, etc. Syn. light threshold.
See interval, photochromatic.
contrast t. See threshold, differential.
corneal touch t. See corneal touch threshold.
differential t. The smallest difference between two stimuli presented simultaneously that gives rise to a perceived difference in sensation. The difference may be related to brightness, but also to colour and specifically to either saturation (while hue is kept constant) or hue (while saturation is kept constant). The differential threshold of luminance is equal to about 1% in photopic vision. Syn. contrast threshold (if the difference is one of luminance); just noticeable difference (jnd).
See law, Weber’s; sensitivity, contrast.
light t. See threshold, absolute.
movement t. 1. The minimum motion of an object that can be perceived. 2. The speed at which an object moving between two points just appears to be moving.
See hyperacuity; movement, phi.
resolution t. See resolution, limit of.
stereo-t . See acuity, stereoscopic visual.
Thygeson’s superficial punctate keratitis See keratitis, Thygeson’s superficial punctate.
thymoxamine (moxisylyte) See alpha-adrenergic antagonist.
thyroid eye disease See disease, Graves’; ophthalmopathy, thyroid.
thyrotoxicosis See disease, Graves’.
tight junction Refers to cells in which their membranes are fused rather than separated by a small extracellular space. The movement of substances through that space is restricted. Syn. zonulae occludentes.
See blood-brain barrier.
tilt after-effect; See after-effect, tilt.
tilted optic disc See crescent, congenital scleral.
timolol maleate See adrenergic receptors; beta-blocker.
tissue A basic anatomical and physiological component of the living organism, consisting of a collection of similar cells and their intercellular substances. Examples: connective tissue, epithelial tissue, muscular tissue, nervous tissue.
Titmus stereo test See vectogram.
TNO test See stereogram, random-dot.
‘tobacco dust’ See sign, Shafer’s.
tobramycin See antibiotic.
tomograph, confocal scanning laser See glaucoma detection; ophthalmoscope, confocal scanning laser.
tomography A radiographic technique for making a detailed X-ray image of a selected plane section of the body while blurring out the images of other planes. The data can be manipulated to represent three-dimensional images of structures.
computed t. (CT) A radiographic method of viewing a three-dimensional image of a layer of body structures, which is constructed by a computer from a series of plane cross-sectional X-ray images made along an axis. The images indicate the X-ray absorption (called attenuation) of tissues (e.g. bones attenuate most, lungs attenuate least and blood vessels are in between). The X-rays are received by numerous gas or solid-state detectors and computers are used to store, process and manipulate the information received from these detectors. The method yields far better differentiation of tissues than conventional radiography thus providing more precise diagnostic information. Usage includes the detection of orbital fractures, orbital cellulitis, intraorbital calcification, cerebral haemorrhage and orbital tumours. Syn. computerized axial tomography (CAT); CAT scan; CT scan.
See glaucoma detection; magnetic resonance imaging; radiology.
confocal scanning laser t. See ophthalmoscope, confocal scanning laser.
optical coherence t. (OCT) A non-invasive, optical diagnostic imaging technique, which enables in vivo cross-sectional tomographic visualization of internal microstructure in biological systems. OCT is analogous to ultrasound imaging except that it uses light rather than sound, thus achieving approximately 1–100× higher image resolution. This is accomplished by using polychromatic (broad bandwidth) or tunable light sources in combination with interferometric techniques to detect depth resolved reflectivity profiles, due to subtle refractive index changes. Several adjacent onedimensional optical A-scans are combined into two- or three-dimensional tomograms for quantitative analysis of the optic nerve head topography, peripapillary fibre layer thickness, macular retinal thickness, as well as corneal visualization. Quantitative results are compared with an age-matched normative database. OCT can be used for early diagnosis of retinal diseases (e.g. cystoid macular oedema, central serous retinopathy, retinal detachments, macular hole), better understanding of retinal pathogenesis, monitoring of nerve fibre layer thickness and optic nerve head changes in glaucomatous eyes, as well as corneal thickness changes following refractive surgery. Most recent developments enable several 10 thousand measurements per second, allowing three-dimensional retinal images nearly free of motion artifact. In combination with improved resolution this technique has the potential to perform non-invasive optical biopsy of the human retina, i.e. visualization of intraretinal morphology in retinal pathologies approaching the level achieved with histopathology.
See glaucoma detection; interference.
positron emission t. (PET) A neuroimaging technique in which a positron-emitting isotope incorporated into a metabolically active molecule (e.g. fluorodeoxyglucose) is injected intravenously and used as radioactive tracers to generate images of regional cerebral blood flow and glucose consumption contained in the tracers and thus, indirectly brain function. The emitted positron collides with an electron, giving rise to two photons, which strike detectors placed around the head. Tomographic images can be used to construct a three-dimensional image of the relative concentration of the tracer within the brain. PET has been used to study normal and abnormal brain function and to assess tumours, stroke, cortical lesions and also mapping of the visual cortex.
See magnetic resonance imaging, fMRI; neuroimaging, functional.
tone, colour Term often used in colorimetry, photography and industry to indicate hue. See hue.
tone, muscle See tonus.
tonic accommodation See accommodation, resting state of.
tonic convergence See vergence, tonic.
tonic pupil See pupil, Adie’s.
tonic vergence See vergence, tonic.
tonicity See solution, hypertonic; solution, hypotonic; solution, isotonic.
tonography Technique for measuring the facility of outflow of aqueous humour from the eye under the continuous pressure exerted by the weight of a tonometer over a given period of time. The instrument usually employed for tonography is an electronically recording Schiötz tonometer. In this technique, the pressure is continuously recorded over a four-minute period and the outflow is deduced by utilizing a specifically designed diagram, called a nomogram (which is a graphical representation of one, or more, mathematical relationships whereby the desired value may be found without calculation by placing a straight edge across the diagram). The results of tonography can indicate the presence of established glaucoma, although the technique is not very reliable for borderline cases.
tonometer An instrument for estimating intraocular pressure. It measures either the degree of corneal deformation produced by a known force, or the force needed to produce a given degree of corneal deformation.
See glaucoma detection; manometer; pressure, intraocular; rigidity, ocular; Tonopen.
air-puff t . See tonometer, non-contact.
applanation t. A tonometer in which the intraocular pressure is estimated either by the force required to flatten a constant corneal area as, for example, in the Perkins (Fig. T14) and Goldmann (Fig. T15) tonometers, or by the area flattened by a constant force, as, for example, in the Maklakov and Tonomat tonometers. The Goldmann tonometer (Figs. T15 and T16) is used in conjunction with a slit-lamp and provides an accurate reading with which all other tonometers are usually compared. The Perkins tonometer is a handheld instrument.

See law, Imbert–Fick.
electronic t. Any tonometer with an electronic readout. These instruments act swiftly, the procedure usually being completed within a fraction of a second.
Goldmann t. See tonometer, applanation.
impression t. A tonometer in which the intraocular pressure is estimated by the degree of indentation of the cornea. The excursion of the plunger of the tonometer is read from a calibrated scale and converted into values of the intraocular pressure, often using appropriate tables. The most common such instrument is that of Schiötz. Syn. indentation tonometer.

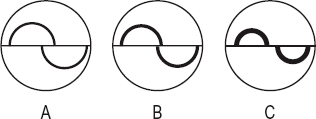
indentation t. See tonometer, impression.
Mackay-Marg t. An electronic tonometer in which a plunger in the centre of a flat footplate which applanates the cornea protrudes by a very small amount (5 mm). The intraocular pressure is related to the counter force required to resist displacement of this plunger when the cornea is flattened by the footplate. The result is read by interpretation of a graph on a strip chart.
Maklakov’s t. See tonometer, applanation.
non-contact t. (NCT) A tonometer that does not require any contact to be made between the tonometer and the eye. Hence no anaesthesia is required with this instrument. It consists of sending a puff of air towards the cornea of sufficient strength to flatten a predetermined area of cornea. The time taken from the onset of the puff of air to the applanation of the cornea (which is monitored optically) is recorded electronically and is proportional to the intraocular pressure. A digital readout of pressure, in mmHg, appears within about 15 ms after the measurement is initiated. The same principle is applied in the handheld Pulsair non-contact tonometer and in the Reichert Non-Contact tonometer. Syn. Air-puff tonometer; pneumatic tonometer.
Perkins t. See tonometer, applanation.
Pulsair non-contact t. See tonometer, non–contact.
rebound t. A handheld, compact, portable tonometer. It incorporates its own battery supply and digital readout. A pair of coils coaxial to a probe shaft is used: a solenoid coil propels a lightweight magnetized probe against the cornea and it bounces back. A sensing coil detects several motion parameters from the voltage that the moving probe induces. They are recorded and analyzed. The intraocular pressure is related to the duration of the corneal impact, the shorter the duration, the higher the pressure. The probe is disposable and its tip is covered with a round plastic cover to minimize corneal damage. The results correlate well with the Goldmann tonometer, although with slightly higher readings.
Reichert Non-Contact t . See tonometer, non-contact.
Schiötz t. See tonometer, impression.
Tonomat t. See tonometer, applanation.
tonometry Measurement of intraocular pressure with a tonometer.
See pressure, intraocular; tonometer.
Tonopen A handheld, compact, portable applanation tonometer based on the same principle as the Mackay–Marg tonometer. It is a very small instrument, 18 cm long by 2 cm in width weighing 56 g. It incorporates its own battery power supply and liquid crystal digital readout and provides both an intraocular pressure readout and an indicator of the reliability of the instrument. The results correlate well with the Goldmann tonometer, although it slightly overestimates low lOPs and underestimates high lOPs. It can take measurements in an eye with an irregular or oedematous cornea or through a soft contact lens and in a variety of clinical settings (Fig. T17).

See tonometer, applanation.
tonus A state of partial contraction present in a muscle in its passive state as, for example, when the eye is in the physiological position of rest. Syn. muscle tone.
See accommodation, resting state of; position of rest, physiological; vergence, tonic.
Topogometer A device attached to a keratometer that allows a measurement of the curvature of the cornea off the visual axis. It consists of an illuminated fixation light that can be moved along two axes, both of which are perpendicular to the axis of the keratometer. Scales are provided with the device to indicate, in millimetres, the amount of decentration of the visual axis from the optical axis of the keratometer at the corneal surface. This device helps in the fitting of contact lenses, by providing an estimation of the flattening of the peripheral cornea and of the position of the corneal apex. This instrument has been superseded by computerized instruments.
See corneal topography; videokeratoscope.
topography, corneal See corneal topography.
Toposcope 1 . An instrument for measuring the curvature of the surfaces of a contact lens, based on moiré fringes. A bar pattern is reflected from the lens surface and the reflected image is viewed with a microscope that has a second bar pattern in the eyepiece. The two bar patterns superimposing each other at slightly different orientations create the moiré patterns. The magnification of the microscope is changed until the fringes are parallel to the central index line seen in the field and a dial monitoring this change in magnification indicates the radius of curvature in millimetres. 2. See test, non-invasive break-up time.
See optic zone radius, back; radiuscope.
toroidal surface See lens, toric.
torsion Rotation of an eye about an anteroposterior axis. If the upper pole of the vertical meridian of the cornea appears to rotate inward, it is called intorsion, and outward, extorsion. If the eye rotates to the right it may be called dextrotorsion and if it rotates to the left it may be called laevotorsion. It may occur as a result of a head tilt, extraocular muscle weakness or rotation of the eye to a tertiary position. Syn. cycloduction; cyclorotation; torsional movement.
See law, Donder’s; position, tertiary; hemianopia, incongruous.
torticollis, ocular Head tilting usually accompanied by a twisting of the neck adopted to minimize the effect of a palsy of one or more of the vertically acting extraocular muscles (most often the superior oblique)
See spasmus nutans.
tortoiseshell Material used in the manufacture of spectacle frames. It is obtained from the shell plates of the hawksbill turtle.
See spectacle frame, plastic; spectacles.
total astigmatism; diameter; reflection See under the nouns.
toughened glass See glass, safety.
tourmaline See polarizer.
toxic amblyopia See amblyopia, toxic.
toxoplasmosis An infectious disease caused by the protozoan Toxoplasma gondii. It occurs either as a congenital or as an acquired type. The congenital type is characterized by bilateral retinochoroiditis in which the fovea is frequently destroyed, resulting in loss of central vision, hydrocephalus, convulsions and encephalomyelitis. The acquired type varies in severity and so does the ocular involvement, the more common lesion being a nonspecific intraocular inflammation involving either the anterior or posterior segment of the eye.
trabecular meshwork See meshwork, trabecular.
trabeculectomy A type of filtration surgery aimed at lowering the intraocular pressure by excising a small portion of the sclera and peripheral iris to create a passage allowing aqueous humour to flow from the anterior chamber out of the eye into the subconjunctival space. The hole is protected by a scleral flap, which is sutured back at the end of the procedure to reduce the risk of overfiltration and hypotony.
See cyclodialysis.
trabeculoplasty, laser A procedure aimed at improving the outflow of aqueous humour in open-angle glaucoma by producing a series of laser burns (usually with an argon laser) to the trabecular meshwork.
trabeculotomy A surgical procedure aimed at lowering intraocular pressure by unblocking the entry of Schlemm’s canal to ease the outflow of aqueous humour. This procedure is used principally in congenital glaucoma especially when goniotomy has failed.
trachoma A chronic, bilateral, contagious conjunctivitis caused by the serotypes A, Ba and C of Chlamydia trachomatis. The conjunctivitis results in conjunctival scarring (Arlt’s line) and may lead to entropion and trichiasis and dry eyes. Follicles at the limbus may leave some sharply defined depressions (Herbert’s pits). There is also keratitis with corneal infiltrates, pannus and vascularization. As the disease progresses there is corneal ulceration and opacification, which may result in blindness. Trachoma is one of the main causes of blindness in the world. It is a disease most commonly encountered in hot regions of the globe where hygienic conditions are poor. Treatment includes a course of tetracycline or erythromycin and surgical correction of entropion and trichiasis may be necessary. Syn. egyptian conjunctivitis; granular conjunctivitis.
tract 1. A bundle of nerve fibres (e.g. the optic tracts). 2. A system of organs serving the same function, e.g. the respiratory tract.
geniculocalcarine t. See radiations, optic.
optic t’s. Two cylindrical bands of nerve fibres carrying visual impulses. They run outward and backward from the posterolateral angle of the optic chiasma, then sweep laterally, encircling the hypothalamus posteriorly on their way to the lateral geniculate bodies. A few fibres end in the superior colliculi.
See hemianopia, incongruous; pathway, visual.
traction retinal detachment See retinal detachment.
training, visual Methods aimed at improving visual abilities, e.g. visual perception, spatial localization, heterophoria, hand/eye coordination, etc. to achieve optimal visual performance and comfort. These techniques represent an enlargement of the practice of orthoptics. Syn. vision therapy.
transcleral illumination See transillumination.
transduction Generally, the conversion of one form of energy into another. Example: the transformation of light energy into receptor potentials in the photoreceptors of the retina (also called phototransduction). The absorption of light by the pigments of the photoreceptors triggers a cascade of biochemical events that leads to a change in ionic fluxes across the plasma membrane and to a change in resting potential from around –40 mV in the dark, to around –70 mV in light, that is a hyperpolarization of the cells.
See depolarization; hyperpolarization; potential, receptor; pigment, visual.
transillumination 1 . The shining of light through a translucent membrane. This is principally used to better visualize ocular tumours, cysts or haemorrhages within the eye. It is accomplished by directing a narrow intense beam of light on the side of the eye. Example: If a tumour is present in the eye some light will not be reflected and the pupil will appear partially or completely black, instead of bright red as when the healthy eye is thus illuminated. Syn. transcleral illumination. 2. See illumination, retro-.
transition of a scleral contact lens The zone between the optic (corneal) and haptic (scleral) portions.
See blending; lens, scleral contact.
translocation See chromosome; mutation.
translucent Pertains to a medium or substance that transmits light but diffuses or scatters it on the way so that objects cannot be seen through it, e.g. paraffin wax, tracing paper, cloth, smoke, fog, ground glass, etc.
See transparent.
transmission Passage of radiations through a medium or a substance. Transmission can be either diffuse (light is scattered in all directions) or regular (i.e. without diffusion).
See absorption; translucent; transmittance; transparent.
transmission curve A graph in which the transmission of an optical medium is plotted against the wavelength.
transmittance A measure of transmission expressed as the ratio of the intensity of the transmitted light I’ to the intensity of the incident light I, for a specified wavelength, i.e. T = I’/I. It is usually given as a percentage, i.e. T = I’/I × 100. Syn. total transmittance.
See absorbance; density, optical.
transparent Pertains to a medium or a substance that transmits light without scattering and with little absorption, so that objects can be seen through it. Optical lenses, prisms, etc. are made of such material.
See opaque; translucent.
transplant, corneal See keratoplasty.
transport, active A process by which particles (e.g. ions, molecules) are transported across cell membranes, against, in almost all instances, the concentration gradient. It requires energy, which is provided by the metabolism of carbohydrates, proteins or lipids and cellular energy, which is obtained from splitting adenosine triphosphate (ATP). (Example: the sodium/potassium pump that keeps sodium ions out of a cell and potassium ions in). When this process results in a compound being released, it is termed ‘secretion’. This process is one of the mechanisms by which aqueous humour is produced in the ciliary body.
See potential, action; ultrafiltration.
transposition 1 . The act of converting the prescription of an ophthalmic lens from a sphere with minus cylinder form to a sphere with plus cylinder form or vice versa. Example: –3 D sphere –2 D cylinder axis 180° transposes to –5 D sphere +2 D cylinder axis 90°. 2. A surgical procedure used to correct muscle paralysis. In this procedure, adjacent muscles are transferred (transposed) to the paralysed muscle, allowing for partial movement in the field of action of the paretic muscle. There are various procedures: one in which parts of the recti muscles are sutured together (the superior and inferior recti are disinserted and joined to the lateral rectus) to correct lateral rectus palsy and improve abduction (Hummelsheim’s procedure or Jensen’s procedure): another in which the lateral and medial recti muscles are disinserted and attached adjacent to either the superior or inferior rectus, to improve elevation or depression, respectively (Knapp’s procedure).
See action, primary; focimeter; paralysis of the sixth nerve; paralysis of the third nerve; strabismus surgery.
Trantas’ dots See conjunctivitis, vernal.
travoprost See prostaglandin analogues.
Treacher Collins syndrome See syndrome, Treacher Collins.
tremors See movements, fixation.
trial case A case containing pairs of positive and negative spherical lenses, plano cylinders, thin prisms as well as discs, pinhole discs, etc. used in refraction with a trial frame. The contents of the case are referred to as a trial set.
trial frame Spectacle frame with variable adjustments for interpupillary distance, side length, etc. in which each lens rim is fitted with a number of cells into which trial lenses can be placed when testing vision (Fig. T18).
See phoropter; Simultantest.
trial lens clip See clipover.
trial, randomized controlled (RCT) An experimental design used for testing the effectiveness of a new medication or a new therapeutic procedure. Individuals are assigned randomly to a treatment group (experimental therapy) and a control group (placebo or standard therapy) and the outcomes are compared. The trial is strengthened by ‘blinding’ or masking (single-blind, double-blind or triple-blind study) and cross-over design. RCT is the most accepted scientific method of determining the benefit of a drug or a therapeutic procedure. It represents the best evidence available, which is integrated into the final decision about the management of a condition by healthcare practitioners in what is called evidence-based healthcare. Syn. randomized clinical trial.
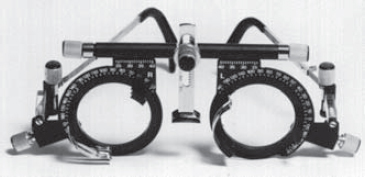
See sampling; significance; study.
trial set A number of objects used to measure the refraction of the eye. It includes a trial case with various lenses, prisms, pinhole discs, Maddox rod, etc. and a trial frame.
triamcinolone See antiinflammatory drug; chalazion; retinopathy, diabetic.
triangle, colour See chromaticity diagram.
triangulation, amplitude of See convergence, amplitude of.
triangulation, angle of See angle of convergence.
tricarboxylic acid cycle See cycle, Krebs.
trichiasis A condition in which the eyelashes due to entropion, blepharitis or injury, are directed towards the globe and cause irritation of the cornea and conjunctiva. Temporary relief may be achieved with epilation but permanent treatment consists of cryotherapy or laser ablation or in severe cases surgical excision and replacement with a mucous membrane (Fig. T19).
See distichiasis; epilation; lens, therapeutic soft contact.
trichromatic theory See theory, Young–Helmholtz.

trichromatism Colour vision characterized by the fact that any perceived hues can be matched by three independent primaries (e.g. red, green and blue). Syn. trichromacy; trichromatic vision.
trichromatism, anomalous A form of defective colour vision in which three primary colours are required for colour matching, but the proportion of each primary is not the same as those required by a normal trichromat. There are three types of anomalous trichromatism; deuteranomaly, protanomaly and tritanomaly. Syn. anomalous trichromacy; anomalous trichromatic vision.
See colours, primary; colour vision, defective.
trifluridine; trifluorothymidine See antiviral agents.
trigeminal ganglion See ganglion, gasserian.
trigeminal nerve See nerve, trigeminal.
trimethoprim See antibiotic.
triplet Lens system composed of three lenses as, for example, a convex crown glass lens cemented between two concave flint lenses. The aim of such a system is to minimize aberrations (Fig. T20).
See doublet; eyepiece, orthoscopic; lens, achromatizing.
triplopia Condition in which a subject sees three images of a single object. This condition may be the result of crystalline lens sclerosis, multiple pupils, etc.
trisomy See chromosome.
trisomy 18 syndrome See syndrome, Edwards’.
trisomy 21 syndrome See syndrome, Down’s.
tritan A person who has either tritanopia or tritanomaly.
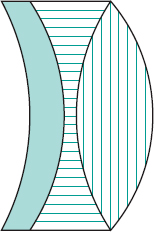
tritanomal A person who has tritanomaly.
tritanomaly A type of anomalous trichromatism in which an abnormally high proportion of blue is needed when mixing blue and green to match a standard blue-green stimulus. This condition is exceedingly rare: it is estimated at about one person in a million. Syn. tritanomalous trichromatism; tritanomalous vision.
See anomaloscope; colour vision, defective; plates, pseudoisochromatic.
tritanope A person who has tritanopia.
tritanopia A rare type of dichromatism in which blue and yellow are confused. The tritanope only sees two colours: reds on the long-wave side, and greens or bluish greens on the other side of his neutral point, which is situated around 570 nm. Tritanopia occurs more often as an acquired type as a result of retinal disease or detachment, glaucoma, diabetes, retinitis pigmentosa, etc. Congenital tritanopia is very rare: it is estimated at about five males and three females in 100 000. Syn. blue blindness; blue-yellow blindness.
See colour vision, defective; dichromatism; plates, pseudoisochromatic; test, Farnsworth.
trochlea See fossa, trochlear; muscle, superior oblique.
trochlear nerve See nerve, trochlear.
trochlear paralysis See paralysis of the fourth nerve.
troland Unit of retinal illuminance equal to that produced when the luminance of the observed object is one candela per square metre seen through a pupil having an area of one square millimetre. Syn. photon (obsolete).
See retinal illuminance.
tropia See strabismus.
tropicamide See acetylcholine; cycloplegia; mydriatic.
Troxler’s phenomenon See phenomenon, Troxler’s.
true negative See specificity.
true positive See sensitivity.
truncation Removal of the peripheral part of a contact lens. The truncation is often undertaken at the base of a prism ballast lens.
See ballast.
Tscherning ellipse See ellipse, Tscherning.
tubercle, lacrimal See lacrimal tubercle.
tubercle, lateral orbital A small elevation on the orbital surface of the zygomatic bone just behind and within the orbital margin, about 11 mm below the frontozy-gomatic suture. It serves as an attachment for the check ligament of the lateral rectus muscle, the lateral palpebral ligament, the suspensory ligament of Lockwood and the levator palpebrae superioris muscle. Syn. Whitnall’s tubercle.
See ligament of Lockwood; ligament, palpebral.
tuberculosis See disease, Eales’; uveitis.
tuck procedure See procedure, tuck.
tungsten-halogen lamp See lamp, halogen.
tunica vasculosa lentis See artery, hyaloid.
tunnel vision See vision, tunnel.
Turk’s disease See syndrome, Duane’s.
Turner’s syndrome See syndrome, Turner’s.
Turville infinity balance test See test, Turville infinity balance.
twitch, eyelid See myokymia.
twilight vision See vision, mesopic.
two visual systems theory See theory, two visual systems.
Tyndall effect See effect, Tyndall.
typoscope A reading shield made of black material in which there is a rectangular aperture allowing one or more lines of print to be seen. It reduces extraneous light reflected from the surface of the paper and assists in staying on the correct line (Fig. T21). It can be helpful for people with low vision who have, for example, media involvement. Recent models embody built-in lighting to provide even and controlled illumination. Syn. reading slit.






