71 Syringomyelia
Salient features
History
Examination
• Wasting and weakness of the small muscles of the hands and forearm (if fasciculation is seen, then the other diagnosis that comes to mind at this stage is motor neuron disease (Case 69))
• Rarely patients may have hypertrophy in limbs, hand and feet (Lancet 1996;347:1593–5)
• Tone and deep tendon reflexes are diminished
• Loss of pain and temperature sensation with intact vibration, light touch and joint position sense: this deficit is the underlying cause for any burns present
• Examine vibration sense over the fingers, lower end of radius, elbow and clavicles (note that vibration sense is impaired only at a later stage)
• Examine the neck posteriorly for scar of previous surgery
• Ask whether you may examine the following:
Questions
How do you explain the clinical features?
Advanced-level questions
What are the other causes of dissociated sensory loss?
What investigations would you do?
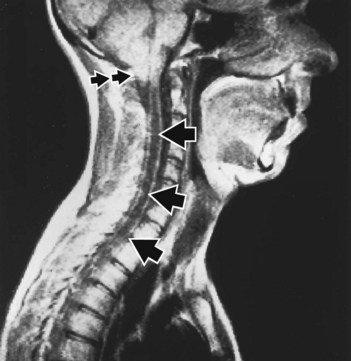
MRI scan (J Neurosurg 1988;68:726) (Fig. 71.1). In the past, myelography was performed to confirm the diagnosis but was associated with deterioration of the condition in a large number of patients.
What associated abnormalities may be present?
Arnold–Chiari malformation (Fig. 71.1), spina bifida, bony defects around the foramen magnum, hydrocephalus, spinal cord tumours.
What are the clinical features of syringobulbia?
• Dissociated sensory loss of the face in an ‘onion-skin’ pattern (extending from behind forwards, converging on the nose and upper lip)
• Wasting of the small muscles of the tongue (important physical sign)
• The process may be limited to the medullary region
• The main cranial nerve nuclei involved are those of the fifth, seventh, ninth and tenth cranial nerves.
What does the cavity of the syrinx contain?
It contains a fluid similar to CSF but with a higher protein content.
What treatment is available?
• Syringoperitoneal shunting (particularly in patients with basal arachnoiditis and without tonsillar descent)
• Direct drainage of the syrinx into the subarachnoid space (in post-traumatic cavitation)
• When there is an association with Arnold–Chiari malformation, the pressure is relieved by removing the lower central portion of the occipital bone and cervical laminectomy to restore normal CSF dynamics.
Mention some theories of formation of syringomyelia
Gardner’s hydrodynamic theory. This theory posits that syringomyelia is caused by a ‘water hammer’-like transmission of pulsatile CSF pressure via a communication between the fourth ventricle and the central canal of the spinal cord through the obex. A blockage of the foramen of Magendie initiates this process (J Neurol Neurosurg Psychiatry 1965;28:247–59.)
William’s theory. William’s theory posits that the development of the syrinx is caused by a differential between intracranial pressure and spinal pressure caused by a valve like action at the foramen magnum. The increase in subarachnoid fluid pressure from increased venous pressure during Valsalva maneuvers or coughing is localized to the intracranial compartment (Neurol Res 1986;8:130–45). This theory is particularly applicable to patients with Chiari malformation. The malformation of the hindbrain prevents the increased CSF pressure from dissipating caudally. During Valsalva maneuver or coughing, a progressive increase in cisterna magna pressure occurs simultaneously with a decrease in spinal subarachnoid pressure. This craniospinal pressure gradient draws CSF caudally into the syrinx.
Oldfield’s theory. During dynamic MRI, downward movement of the cerebellar tonsils during systole can be visualized. A piston effect, created by oscillations, in the spinal subarachnoid space that acts on the surface of the spinal cord and forces CSF through the perivascular and interstitial spaces into the syrinx raising intramedullary pressure. The resulting compression of long tracts, neurons and microcirculation are responsible for the signs and symptoms of neurological dysfunction that appear with distension of the syrinx. Decompression of the syrinx, therefore, potentially reverses the symptoms referable to increased intramedullary pressure (J Neurosurg 1994;80:3–15).
The intramedullary pulse pressure theory. The intramedullary pulse pressure theory posits that syringomyelia is caused by increased pulse pressure in the spinal cord and that the syrinx consists of extracellular fluid. The distending force in the production of syringomyelia is a relative increase in pulse pressure in the spinal cord compared with that in the nearby subarachnoid space. The syrinix is formed by the accumulation of extracellular fluid in the distended cord.
What do you know about the management of syringomyelia?
• Arnold-Chiari malformation associated syringomyelia: suboccipital craniectomy and upper cervical laminectomy to decompress the malformation at the foramen magnum
• Intramedullary tumour: surgery with or without radiation therapy
• Post-traumatic syringomyelia: surgery when the neurologic deficits or pain is intolerable
• The term syringomyelia (from syringx, a pipe or tube) was first used by Ollivier in 1824, in his monograph on diseases of the spinal cord, to denote cavity formation. It denotes the presence of a large fluid-filled cavity in the grey matter of the spinal cord that is in communication with the central canal and contains CSF.