CHAPTER 10 Symptoms of lower gastrointestinal disease
Introduction
Gastrointestinal symptoms are very common within the general population (Thompson et al., 2003). There is a high prevalence of rectal bleeding (Crossland and Jones, 1995; Thompson et al., 2000), change in bowel habit (Everhart et al., 1989) and abdominal pain (Sandler, 1990). Since any one of these symptoms alone can be due to benign, transient disease, symptom complexes are more useful for predicting serious pathology (Thompson et al., 2007). In the UK, this has led to the ‘two week wait guidelines’ for suspected cancer (Department of Health, 2000). This means that patients with symptoms most predictive of colorectal cancer (Table 10.1) must be seen within 2 weeks from the date of referral.
Table 10.1 Criteria for urgent referral for suspected colorectal cancer under the two-week rule
| Sign, symptom or combination | Age threshold |
|---|---|
| Rectal bleeding with a change in bowel habit to looser stools and/or increased frequency of defecation persistent for 6 weeks | Over 40 years |
| A definite right-sided abdominal mass | All ages |
| A definite palpable rectal (not pelvic) mass | All ages |
| Change of bowel habit to looser stools and/or increased frequency of defecation, without rectal bleeding and persistent for 6 weeks | Over 60 years |
| Rectal bleeding persistently without anal symptoms | Over 60 years |
| Iron deficiency anemia without an obvious cause (Hb<11 g/dl in men or <10 g/dl in postmenopausal women) | No age criterion |
Rectal bleeding
Bleeding from the gastrointestinal tract can be overt or occult. With overt rectal bleeding, the blood is recognized and is usually noticed on defecation. If this is the case, the origin of the bleeding is usually in the left colon or distal transverse colon. If the bleeding is occult, the blood loss is not recognized in the stool and the patient presents with anemia.
Bright red rectal bleeding with anal symptoms
Rectal bleeding with anal symptoms without a change in bowel habit is the lowest predictor of colorectal cancer (Thompson et al., 2007). It usually suggests hemorrhoids (associated with mucus, skin tags or prolapsing lumps) or an anal fissure (associated with anal pain on defecation). Distal proctitis (inflammation of the very distal rectum) may also be a cause. The exception to this is anal cancer that may present with these symptoms but is often associated with a lump or ulcer in the anal canal
Investigation: no radiological investigation may be necessary. This diagnosis can usually be made in the outpatient clinic on rigid sigmoidoscopy and/or proctoscopy. In the case of a fissure, examination may not be possible and a painful per rectum (PR) examination may be diagnostic.
Bright red rectal bleeding without anal symptoms
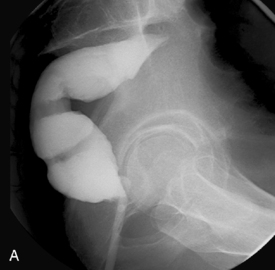
Investigation: radiological investigation may not be necessary for this symptom complex. It should be diagnosed on PR examination ± rigid sigmoidoscopy or proctoscopy. Flexible sigmoidoscopy would be appropriate in the over 40s to exclude malignancy. Should a stricture prevent the passage of the endoscope, a barium enema (Figure 10.1) or computed tomography (CT) should be considered.
Bright red rectal bleeding with change in bowel habit (CIBH) to looser stools
This carries the highest risk of bowel cancer (Thompson et al., 2007) but is also symptomatic of colitis, which may be infective, ischemic, ulcerative colitis (UC) or Crohn’s disease (Figures 10.2, 10.3 and 10.4).
Bright red rectal bleeding with constipation
Often the constipation has exacerbated bleeding from hemorrhoids or a fissure, rarely due to cancer.
Investigation: the clinician may request a barium enema or CT colonography to find a cause for the change in bowel habit. Constipation alone is a poor predictor of cancer. However, it is a predisposing factor for diverticular disease and so this is a common finding in patients with constipation. A coloproctological referral will still be needed to assess the distal bleeding. If the constipation is long standing and an underlying functional bowel disorder is being considered, a colonic transit study (Figure 10.5) may be requested.
Dark red rectal bleeding without a CIBH
Usually this presentation results from diverticular bleeding. This may present as a large bleed where dark blood and clots are passed with very little stool. The patient usually presents as an emergency or may give a history of a few large bleeds rather than continuing ongoing bleeding (see also Chapter 15).
Dark red rectal bleeding with a CIBH
This may mean a more proximal tumor in the sigmoid, descending colon (Figure 10.6) or transverse colon or more proximal colitis.
Change in bowel habit alone
While CIBH with rectal bleeding is often indicative of significant pathology, CIBH alone is less predictive. This is because many of the population experience a CIBH at some point (Everhart et al., 1989) and 10–20% (Longstreth et al., 2006) have irritable bowel syndrome. When asking about change in bowel habit, it is essential to ascertain what the patient means. For example, does diarrhea mean more frequent stools, looser stools or both? Some patients describe diarrhea as a slightly looser stool; others will only use the term if they are passing watery stools. It is the same with constipation. Some patients describe this as hard stools, some as less frequent stools and some mean they are not going at all. In fact, patients with an obstructing malignancy may describe ‘constipation’ and, although they may be hardly passing any stool, when they do so, it may be watery.
Irritable bowel syndrome (IBS)
It is worth mentioning this as a separate entity as it probably accounts for many of the patients with a negative barium enema who present with symptoms. It is not a diagnosis of exclusion and has very specific diagnostic criteria based on the Rome Criteria (Sandler, 1990). In 2008, the National Institute for Clinical Excellence (NICE) produced guidelines for the diagnosis and management of IBS.
The positive diagnostic criteria are:
Investigation: NICE has ruled that for patients who meet the positive diagnostic criteria for IBS, neither barium enema nor colonoscopy is necessary (NICE, 2008).
Iron deficiency anemia
Investigation: The British Society of Gastroenterology Guidelines (Goddard et al., 2005) recommend investigation of both the lower and upper GI tract in men and post-menopausal women. This can consist of a barium enema then esophagogastroduodenoscopy (OGD) or an OGD and colonoscopy at the same sitting. It is important that, if tests are done consecutively, that the lower GI tract is examined as anemia can be mistakenly attributed to mild gastritis. If the patient is frail or elderly and will not withstand bowel prep, a CT scan is a good first line test as it has good sensitivity for the diagnosis of right-sided colonic tumors (Figure 10.7) (Ng et al., 2002).
Melena
This is the passage of altered blood per rectum. Patients may describe black stools. True melena is very distinctive. It has an offensive smell and is described as black and tarry and is usually a reflection of a large bleed, most commonly due to an upper GI source such as a gastric or duodenal ulcer. It can be due to a right-sided colonic tumor.
Abdominal pain
Abdominal pain alone is rarely discriminatory for problems affecting the lower GI tract. In general, pain from the large bowel presents as lower abdominal pain, whereas pain from the small bowel presents as upper or central abdominal pain. Pain from an obstructing lesion is generally colicky and comes in waves, whereas pain from an inflammatory process, e.g. diverticulitis, is usually constant (see also Chapter 15). The features of the pain such as exacerbating and relieving factors, radiation (whether it spreads anywhere) and any associated symptoms also help determine the cause. In obstruction, (Figures 10.8, 10.9A and 10.9B), the pain may be exacerbated by eating and may be associated with vomiting and a change in bowel habit.
Investigation: if the pain is obviously related to the gut and associated with gastrointestinal symptoms, the investigations of the large bowel described above will be appropriate. If not obviously intestinal, an ultrasound scan or abdominal and pelvic CT with oral contrast is a good first line investigation, as it will identify common extracolonic causes of abdominal pain such as abscess formation or that originating from the gallbladder, pancreas or gynecological tract.
Rectal prolapse
Investigation: if the prolapse is extending beyond the anal canal the diagnosis is obvious, but if it is internal, radiological investigation may be necessary. In this case, a defecating proctogram will give information on the degree of prolapse if present and give information to help plan appropriate surgery (see Chapter 13).
Association of Coloproctology of Great Britain and Ireland. Guidelines for the management of colorectal cancer, third ed, 2007.
Crossland A., Jones R. Rectal bleeding; prevalence and consultation behaviour. Br. Med. J.. 1995;311:486-488.
Everhart J.E., Go V.L.W., Johannes R.S., et al. A longitudinal survey of self reported bowel habits in the United States. Dig. Dis. Sci.. 1989;34:1153-1162.
Department of Health. Referral guidelines for suspected cancer. 2000. Health service circular HSC 2000/013. Published 13 April 2000
Goddard A.F., James M.W., McIntyre M.S., et al. (On behalf of the British Society of Gastroenterology). In Guidelines for the management of iron deficiency anaemia. British Society of Gastroenterology Guidelines; 2005.
Longstreth G.F., Thompson W.G., Chey W.D., et al. Functional bowel disorders. Gastroenterology. 2006;130:1480-1491.
Ng C.S., Doyle T.C., Pinto E.M., et al. Caecal carcinomas in the elderly: useful signs in minimal preparation CT. Clin. Radiol.. 2002;57(5):359-364.
NICE. Clinical guideline 61. 2008 www.nice.org.
Sandler R.S. Epidemiology of irritable bowel syndrome in the United States. Gastroenterology. 1990;99:409-415.
Thompson J.A., Pond C.L., Ellis B.G., et al. Rectal bleeding in general and hospital practice ‘the tip of the iceberg. Colorectal Dis.. 2000;2:288-293.
Thompson M.R., Heath I., Ellis B.G., et al. Identifying and managing patients at low risk of bowel cancer in general practice. Br. Med. J.. 2003;327:263-265.
Thompson M.R., Perea R., Senapati A., et al. Predictive value of common symptom combinations in diagnosing colorectal cancer. Br. J. Surg.. 2007;94:1260-1265.