Chapter 10 Sympathetic Nerve Block and Neurolysis
Preoperative preparation
 The operator must have a full understanding of the relevant anatomy and the pathophysiology of the underlying condition, because the complications of sympathetic blocks can be very serious.
The operator must have a full understanding of the relevant anatomy and the pathophysiology of the underlying condition, because the complications of sympathetic blocks can be very serious.Instrumentation
For sympathetic nerve block, the following equipment is required:
Also, 99% alcohol is needed for chemical neurolysis.
The instrumentation required for radiofrequency lesioning is described in Chapter 8 (Figs. 8-14 to 8-16).
Contraindications
 Coagulopathy (International Normalized Ratio (INR) value > 1.5 or platelet count < 50,000/mm3) or prescribed anticoagulant therapy. There is significant risk of vessel injury in a patient with either condition, because the sympathetic trunks are deeply placed and close to major blood vessels. A large hematoma may be produced if the patient has a coagulation disorder. Aspirin or antiplatelet agents should be stopped 7 days, and warfarin 5 days, before injection is performed.
Coagulopathy (International Normalized Ratio (INR) value > 1.5 or platelet count < 50,000/mm3) or prescribed anticoagulant therapy. There is significant risk of vessel injury in a patient with either condition, because the sympathetic trunks are deeply placed and close to major blood vessels. A large hematoma may be produced if the patient has a coagulation disorder. Aspirin or antiplatelet agents should be stopped 7 days, and warfarin 5 days, before injection is performed. Local infection or neoplasm at the needle trajectory: There is a risk of spreading the infection to deeper structures.
Local infection or neoplasm at the needle trajectory: There is a risk of spreading the infection to deeper structures. Anatomical or vascular anomalies: Anatomical distortion, such as pressure from a neoplasm or spinal scoliosis, may make the block more difficult and reduce the chance of success. Anomalous vessels increase the risk of accidental needle puncture.
Anatomical or vascular anomalies: Anatomical distortion, such as pressure from a neoplasm or spinal scoliosis, may make the block more difficult and reduce the chance of success. Anomalous vessels increase the risk of accidental needle puncture.Procedures
Stellate Ganglion
Anatomy
The stellate ganglion, which is formed by the fusion of the inferior cervical and T1 sympathetic ganglia, lies anterior to the transverse processes of C7 and T1 and to the neck of the first rib (Fig. 10-1).
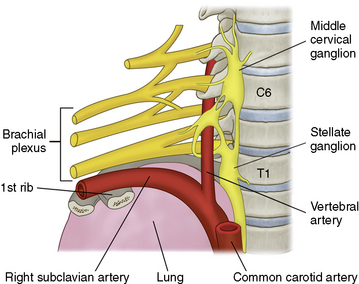
Figure 10–1 Position of the stellate ganglion. C6, sixth cervical vertebra; T1, first thoracic vertebra.
(Modified from Justins DM: Pain and autonomic nerve block. In Wildsmith JAW, Armitage EN, McClure JH [eds]: Principles and Practice of Regional Anaesthesia, 3rd ed. Edinburgh, Churchill Livingstone, 2002, pp 291-309.)
Temperature measurements in both hands (Fig. 10-2) are required to evaluate successful upper extremity block [1]. Digital infrared thermal imaging is helpful (refer to Fig. 15-29) [2]. Horner syndrome does not guarantee success of ipsilateral upper extremity sympathetic block.
Technique
Stellate ganglion block
Pulsed radiofrequency lesioning or radiofrequency thermocoagulation of the stellate ganglion
The stellate ganglion formed by the fusion of the inferior cervical and the first thoracic ganglion as they meet anterior to the vertebral levels of the C7 and T1 vertebra. The ganglion lies on the longus colli at the vertebral level covered by prevertebral fascia and is surrounded by important structures, such as common carotid artery, internal jugular vein, thyroid, vagus nerve, phrenic nerve, and brachial plexus. The distance from the junction of the transverse process and the vertebral body to the stellate ganglion may show individual differences according to the individual shape and volume of longus colli. We, therefore, cannot estimate where the ganglion is on the lateral image of C-arm. In addition, the location of the ganglion is also highly variable. We, also cannot estimate where the ganglion is on the AP image of C-arm. When we use the radiofrequency lesioning techniques (Fig. 8-16) we should remember how and where the lesion is made. If radiofrequency needle tip rests at the junction of the transverse process and the vertebral body, where the radiofrequency lesion is made? These are the reason why we do not perform the procedure under the guidance of fluoroscope.
Thoracic Sympathetic Ganglion
Anatomy
The upper thoracic sympathetic ganglia are located around the heads of the ribs and are covered by the pleura. The lower two or three ganglia are on the sides of the vertebral bodies. The thoracic sympathetic trunk runs between the ganglia and just in front of the somatic nerves (Fig. 10-4) [1].
Techniques
Thoracic sympathetic block
The following procedure is used for thoracic sympathetic block:
Splanchnic Nerve
Anatomy
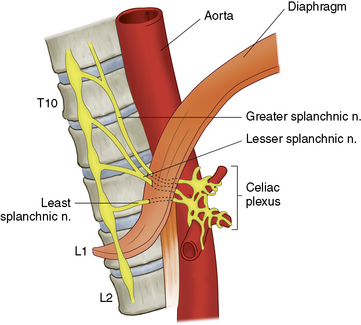
As shown in Figure 10-6, the greater (T5 through T10), lesser (T10 and T11), and least (T11 and T12) splanchnic nerves cross the lateral side of the body of T12 as they sweep forward to penetrate the diaphragm and form the celiac plexus. The pleura are attached posteriorly to the vertebral bodies and create a well-defined compartment.
Techniques
Splanchnic nerve block
The procedure for splanchnic nerve block is as follows:
Pulsed radiofrequency lesioning or radiofrequency thermocoagulation
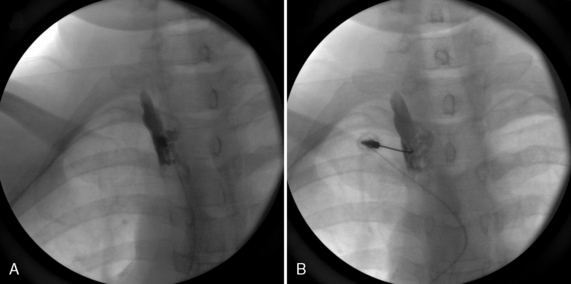
Figure 10-8 illustrates splanchnic nerve neuroablation. The following principles apply:
 As in the splanchnic nerve block at T11 or T12, PRFL or RFTC must be accomplished with fluoroscopic guidance and the use of a 22-gauge, 15-cm, curved-tipped cannula with a 15-mm active tip (Figs. 8-14 to 8-16).
As in the splanchnic nerve block at T11 or T12, PRFL or RFTC must be accomplished with fluoroscopic guidance and the use of a 22-gauge, 15-cm, curved-tipped cannula with a 15-mm active tip (Figs. 8-14 to 8-16).Radiofrequency Thermocoagulation
The following principles apply to RFTC of the splanchnic nerve:
 Impedance should be checked before lesioning. A reading of less than 500 ohms confirms placement of the probe; if the impedance is greater than 500 ohms, the probe should be removed, 0.5 mL of local anesthetics should be injected, and then the probe should be reinserted.
Impedance should be checked before lesioning. A reading of less than 500 ohms confirms placement of the probe; if the impedance is greater than 500 ohms, the probe should be removed, 0.5 mL of local anesthetics should be injected, and then the probe should be reinserted.Celiac Plexus
Anatomy
The celiac plexus is formed by the union of the greater (T5 through T10), lesser (T10 and T11), and least (T11 and T12) splanchnic nerves with the celiac branch of the right vagus (Fig. 10-6). It therefore contains both sympathetic and parasympathetic fibers. There are usually two ganglia at the level of the lower part of the T12 and the upper part of the L1. The ganglia lie in the retroperitoneal space, between the suprarenal glands, posterior to the stomach, pancreas, and the left renal vein, anterior to the crura of the diaphragm, and mainly anterolateral to the aorta. The kidneys are in close relationship.
Technique
Oblique approach
Celiac plexus block using the oblique approach is performed as follows:
A single-needle, transaortic approach
 The needle is inserted on the left side and positioned to ensure that its point is in the middle of the celiac plexus.
The needle is inserted on the left side and positioned to ensure that its point is in the middle of the celiac plexus.Lumbar Sympathetic Ganglion
Anatomy
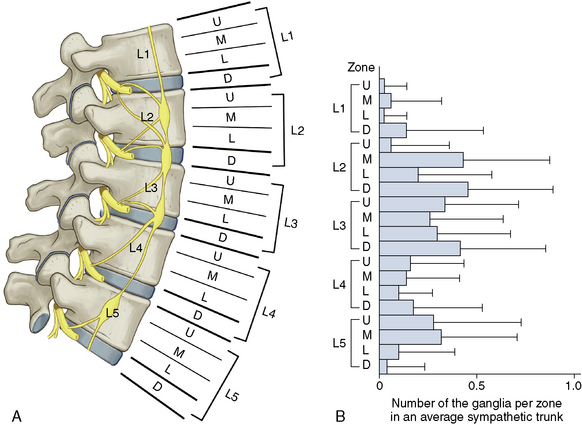
As shown in Figures 10-10 and 10-11, the lumbar sympathetic trunk is situated in the retroperitoneal connective tissue anterior to the vertebral bodies and the medial margin of psoas muscle. The aorta and the inferior vena cava are anterior relations, the genitofemoral nerve lies laterally on psoas, and the kidney and ureter are posterolateral in position.
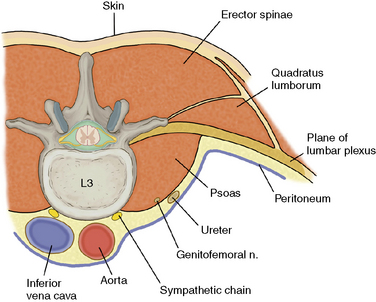
Figure 10–10 Transverse section through L3 to show the position and relationships of the lumbar sympathetic chain. n., nerve.
All the sympathetic fibers pass through or synapse at the L2 ganglion, so in theory, a block at the upper level of L3 should abolish all the sympathetic supply to the lower limb; opinions differ, however, over the number of levels that must be injected to produce optimal lower limb sympathectomy. Murata and colleagues [3] reported four lumbar sympathetic ganglia (on the L2 vertebra, the L2-L3 disc, the L3-L4 disc, and the L5 vertebra) and demonstrated that the sympathetic trunk runs on the anterior surface of the vertebral column from L1 to L4 levels and then passes to the lateral side.
Indications
Technique
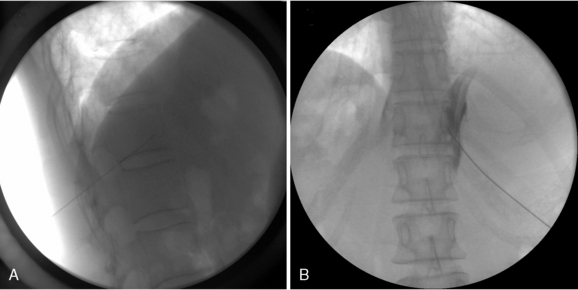
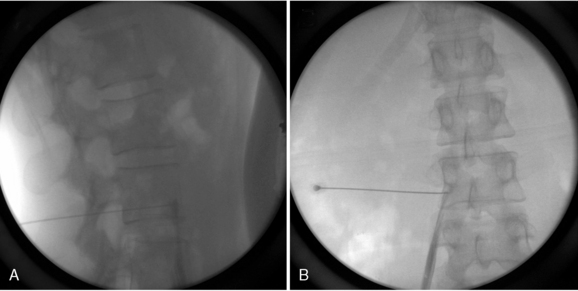
Lumbar sympathetic block
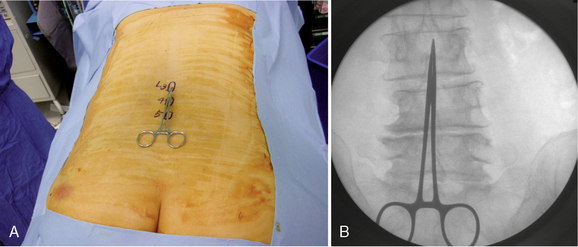
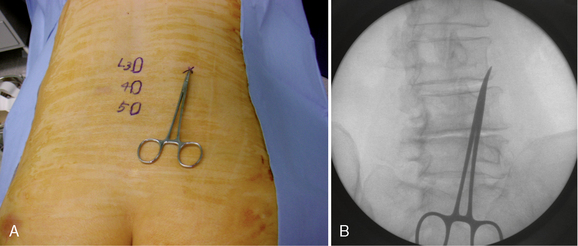
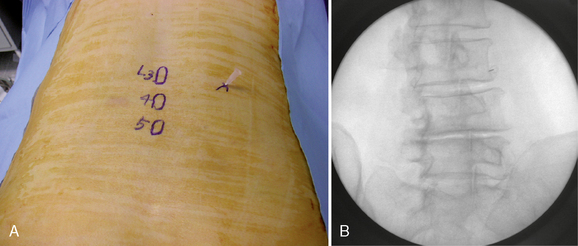
 The block is usually performed with the patient prone. However, the lateral position may be used in the patient who cannot lie prone.
The block is usually performed with the patient prone. However, the lateral position may be used in the patient who cannot lie prone. Blocks for the lower limb (e.g., for peripheral vascular disease or complex regional pain syndrome) usually target L3 and L4.
Blocks for the lower limb (e.g., for peripheral vascular disease or complex regional pain syndrome) usually target L3 and L4.Oblique Approach in the Prone Position
Radiofrequency lesioning
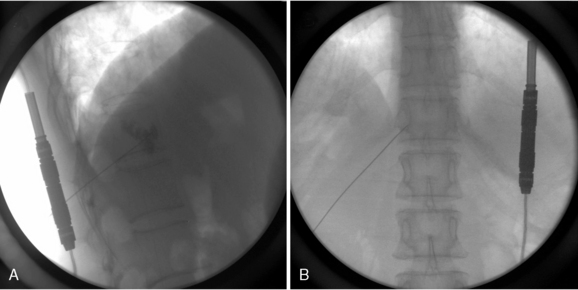
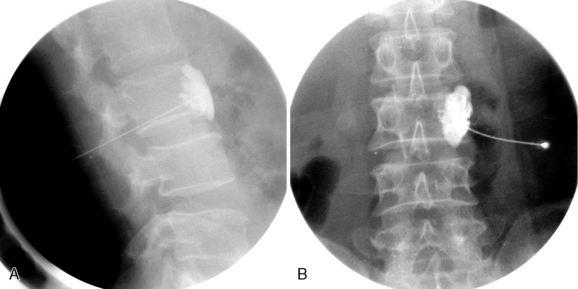
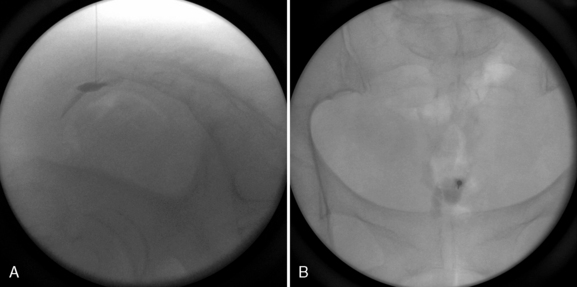
Figure 10-18 illustrates RFTC of the lumbar sympathetic nerve; the principles for radiofrequency lesioning are as follows:
 Radiofrequency lesioning must be performed under fluoroscopic guidance as for the lumbar sympathetic block at the inferior third of L2 and the upper third of L3, with use of a 22-gauge, curved-tipped, 15-cm long cannula with a10-mm active tip (Figs 8-14 to 8-16).
Radiofrequency lesioning must be performed under fluoroscopic guidance as for the lumbar sympathetic block at the inferior third of L2 and the upper third of L3, with use of a 22-gauge, curved-tipped, 15-cm long cannula with a10-mm active tip (Figs 8-14 to 8-16). Sensory and motor stimulation must be performed. During the sensory stimulation (50 Hz, 0.5-1.0 V), the patient may report feeling vague discomfort in the back. If paresthesia exists in the groin, the cannula must be repositioned because of its proximity to the genitofemoral nerve. If fasciculation in the lower extremity is observed during the motor stimulation (2 Hz, 2 V), the cannula must be repositioned owing to its proximity to the spinal nerves.
Sensory and motor stimulation must be performed. During the sensory stimulation (50 Hz, 0.5-1.0 V), the patient may report feeling vague discomfort in the back. If paresthesia exists in the groin, the cannula must be repositioned because of its proximity to the genitofemoral nerve. If fasciculation in the lower extremity is observed during the motor stimulation (2 Hz, 2 V), the cannula must be repositioned owing to its proximity to the spinal nerves.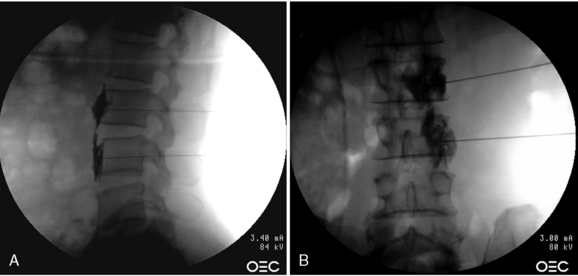
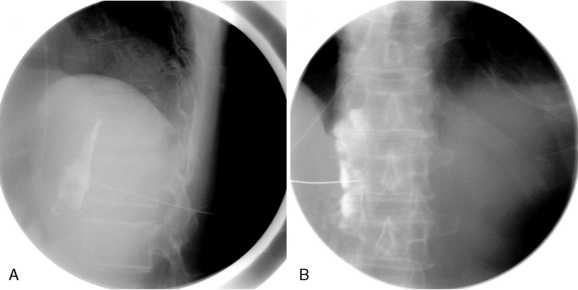
Figure 10–18 Lateral (A) and anteroposterior (B) fluoroscopic images of radiofrequency thermocoagulation at L2 and L3 levels.
Radiofrequency Thermocoagulation
The following principles apply to RFTC of the lumbar sympathetic nerve:
 Impedance should be checked before lesioning. Correct placement of the probe is confirmed by a reading of less than 500 ohms; if impedance is greater than 500 ohms, the probe must be removed, 0.5 mL of local anesthetics must be injected, and the probe must be reinserted.
Impedance should be checked before lesioning. Correct placement of the probe is confirmed by a reading of less than 500 ohms; if impedance is greater than 500 ohms, the probe must be removed, 0.5 mL of local anesthetics must be injected, and the probe must be reinserted.Pulsed Radiofrequency Lesioning
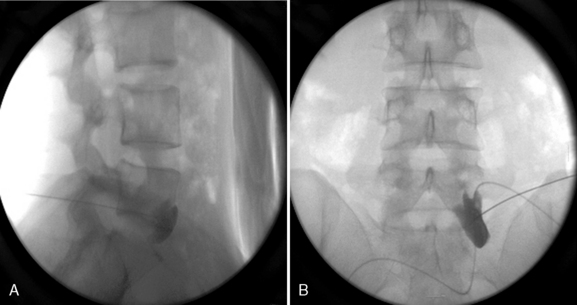
Chemical neurolysis
 Careful evaluation of the presence of anesthesia at the area innervated by the genitofemoral nerve (refer to Fig. 12-4) is essential before neurolytic injection.
Careful evaluation of the presence of anesthesia at the area innervated by the genitofemoral nerve (refer to Fig. 12-4) is essential before neurolytic injection. 1 to 1.5 mL of a neurolytic agent, such as 99% alcohol, should be injected on each level 20 to 30 minutes after the diagnostic block.
1 to 1.5 mL of a neurolytic agent, such as 99% alcohol, should be injected on each level 20 to 30 minutes after the diagnostic block.Complications
Complications of chemical neurolysis of the lumbar plexus include the following:
 Inadvertent injection of alcohol into the vertebral canal, the peritoneal cavity, or blood vessel, which is avoidable when the procedure is performed under C-arm guidance.
Inadvertent injection of alcohol into the vertebral canal, the peritoneal cavity, or blood vessel, which is avoidable when the procedure is performed under C-arm guidance. Damage by the needle or neurolytics to the kidney, renal pelvis, ureter or intervertebral discs, which is also avoidable when the procedure is performed under C-arm guidance.
Damage by the needle or neurolytics to the kidney, renal pelvis, ureter or intervertebral discs, which is also avoidable when the procedure is performed under C-arm guidance.Inferior Mesenteric Plexus
 The specific indication for inferior mesenteric plexus block or chemical neurolysis is unilateral or bilateral lower abdominal pain below the umbilicus and above the pelvis in patients with chronic diseases or cancer.
The specific indication for inferior mesenteric plexus block or chemical neurolysis is unilateral or bilateral lower abdominal pain below the umbilicus and above the pelvis in patients with chronic diseases or cancer. Celiac plexus block or chemical neurolysis is performed at the L1 vertebral level. Inferior mesenteric plexus block or chemical neurolysis is performed at L3.
Celiac plexus block or chemical neurolysis is performed at the L1 vertebral level. Inferior mesenteric plexus block or chemical neurolysis is performed at L3.Superior Hypogastric Plexus Block
Technique
The procedure for superior hypogastric plexus block is as follows:
Ganglion Impar Block
Coccygodynia (coccydynia, coccygalgia, or coccygeal pain) is a painful syndrome affecting the coccyx region, a bone that in primates corresponds to the tail but that in humans constitutes a mere vestigial structure without any function [5].
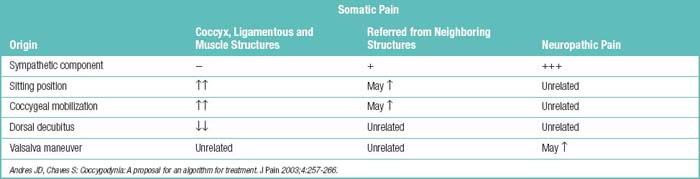
Causes of coccygodynia are listed in Table 10.1, and the differential diagnoses in Table 10.2.
| Somatic pain |
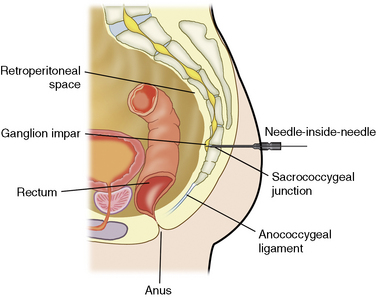
Anatomy
The injection is performed through the sacrococcygeal disc with use of a straight spinal needle.
Technique (Modified Needle-Inside-Needle Technique)
Ganglion impar block using the modified needle-inside-needle technique is performed as follows:
Postprocedure management
 Patients undergoing diagnostic or prognostic block or radiofrequency lesioning should be monitored for 30 to 60 minutes.
Patients undergoing diagnostic or prognostic block or radiofrequency lesioning should be monitored for 30 to 60 minutes.
 Patients undergoing neurolysis should be educated that absolute bed rest for 3 to 4 hours without position change is necessary to avoid unwanted spread of neurolytic agents to adjacent important structures. After a neurologic examination with normal findings, the patient should be discharged with an escort.
Patients undergoing neurolysis should be educated that absolute bed rest for 3 to 4 hours without position change is necessary to avoid unwanted spread of neurolytic agents to adjacent important structures. After a neurologic examination with normal findings, the patient should be discharged with an escort.1 Justins D.M. Pain and autonomic nerve block. In: Wildsmith J.A.W., Armitage E.N., McClure J.H., editors. Principles and Practice of Regional Anaesthesia. 3rd ed. Churchill Livingstone: Edinburgh; 2002:291-309.
2 Kim Y.C., Bahk J.H., Lee S.C., et al. Infrared thermographic imaging in the assessment of successful block on lumbar sympathetic ganglion. Yonsei Med J. 2003;44:119-124.
3 Murata Y., Takahashi K., Yamagata M., et al. Variations in the number and position of human lumbar sympathetic ganglia and rami communicantes. Clin Anat. 2003;16:108-113.
4 Lee C.J., Kim Y.C., Shin J.H., et al. Intravascular injection in lumbar medial branch block: A prospective evaluation of 1433 injections. Anesth Analg. 2008;106:1274-1278.
5 Andres J.D., Chaves S. Coccygodynia: A proposal for an algorithm for treatment. J Pain. 2003;4:257-266.