A, Admit to: Indicate ward where pt is being admitted and attending physician (e.g., coronary care unit, Dr. Smith’s service).
B, Because: Indicate admitting dx (e.g., chest pain).
C, Condition: Specify pt’s general condition (stable, fair, poor, critical).
Code status: Specify DNR, full code, CMO.
Consults:
D, Diet: Specify whether regular, clear liquids, NAS, ADA, low cholesterol, other.
DVT prophylaxis:
A, Allergies: Indicate medications (including OTC medications) and specific food products to which the pt has experienced an allergic reaction.
Activity: Specify bed rest, ad lib, bathroom privileges.
V, Vital signs: Specify frequency (e.g., qid, q4h); also indicate any special nursing orders (e.g., VS and neurologic signs q2h × 24h, then q4h if stable).
I, IV fluids: Specify any IV solutions and rate of infusion.
D, Diagnostic tests: Specify laboratory tests, x-rays, ECG, special tests.
Drugs: Indicate medication, dose, frequency, special restrictions (e.g., atenolol 50 mg PO qd; if HR <50 bpm, hold atenolol and notify house).
2. Lab Shorthand Notation
See Figure 1-1.
3. Dictating the H&P
1. VS: BP, pulse, respirations, temperature.
2. General description: The pt is a (age, sex) who looks her stated age, is pleasant, appears to be well nourished, and seems in a good state of health.
3. Skin: The skin is warm and dry; turgor is adequate; color is nl. No icterus, purpura, rash, or unusual pigmentation is noted. Hair is nl in appearance, distribution, and texture.
4. Lymph nodes: There is no cervical, supraclavicular, axillary, epitrochlear, or inguinal adenopathy.
5. HEENT:
a. Head: It is normocephalic and atraumatic; no lesions are noted.
b. Eyes: Cornea is without lesions, conjunctiva is clear, sclera is white. Pupils are equal, measuring approximately 3 mm in diameter, round, and reactive to light and accommodation. Extraocular movements are within nl limits without any nystagmus or strabismus. Fundi appear benign. Disks are well delineated. There are no hemorrhages or exudates. Visual acuity is 20/20 bilaterally, and visual fields are within nl limits.
c. Ears: Ears are nl in appearance. Auditory canal appears clean and without lesions. The tympanic membranes are intact. Hearing is adequate.
d. Nose: Septum appears to be within nl limits and without deviation. Nasal mucosa appears pink and without any abnl discharge. No nasal polyps or other lesions are noted. Frontal and maxillary sinuses are nontender.
e. Mouth and throat: Lips are without cyanosis or pallor. Buccal mucosa is nl in appearance. Teeth appear to be in good condition. Tongue shows no lesions or tremor. Pharyngeal mucosa is pink and does not reveal any lesions, exudates, erythema, or evidence of inflammation. Gag reflex is intact.
6. Neck: Neck is supple. Full range of motion is present. There is no evidence of tracheal deviation, JVD, or lymphadenopathy. Carotid pulses are 2+, equal bilaterally, and without bruits. Carotid upstroke is within nl limits. Thyroid gland is nl in size; its palpation does not reveal any nodules or masses.
7. Back: Spinal curvature is nl; no scoliosis, kyphosis, or tenderness is present. Full range of motion is present.
8. Chest: Thorax is symmetric. Full expansion is noted bilaterally. Anterior-posterior diameter is within nl limits.
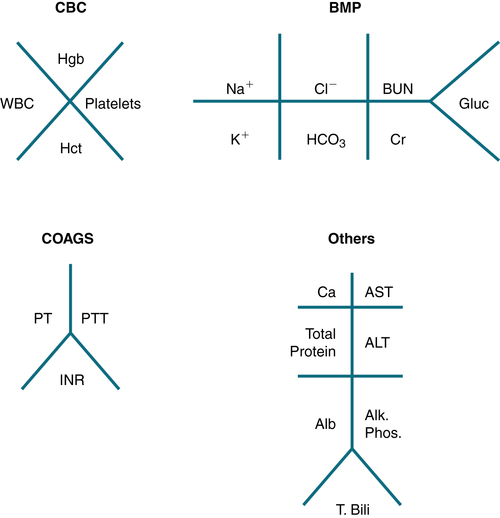
FIGURE 1-1 Lab shorthand notation.
9. Lungs: Fremitus is equal bilaterally. Lung fields are resonant throughout. Breath sounds and voice sounds are nl. There are no rales or rhonchi.
10. Heart: Palpation reveals no heaves or thrills. The PMI is medial to the midclavicular line, fourth intercostal space. Auscultation reveals S1, S2 of nl intensity. There are no S3, S4, rubs, clicks, or other abnl heart sounds. Heart rate is approximately 70 bpm and rhythm is regular.
11. Breasts (female pt): Breasts are symmetric and have a nl contour. Skin is of nl color and appearance; there is no edema, ulceration, or erythema. Nipples are of nl size and shape; there is no nipple retraction, ulceration, or discharge. Palpation does not reveal any tenderness or masses.
12. Abdomen: Abdomen is of nl size and contour. No capillary dilatations, skin lesions, or surgical scars are noted. Auscultation reveals normoactive bowel sounds and no abdominal bruits. Palpation reveals no abdominal tenderness, guarding, or masses. The liver edge is felt approximately 1 inch below the right costal margin; it is firm, sharp, and smooth. The liver percusses to approximately 8 to 10 cm in total span. The spleen is not palpable.
13. Rectal examination: Rectal examination reveals no external anal lesions. Sphincter tone is nl. There are no internal or external hemorrhoids. Rectal mucosa appears nl, and no nodules or masses are present. Stool is brown and (−) for occult blood. Male pt: Prostate is nl in size, no nodules.
14. Genitalia: Inspection reveals nl distribution of pubic hair. Female pt: Clitoris and labia are without lesions. Internal examination with speculum reveals nl vaginal wall. The cervical os is well visualized. No lesions or discharges are noted. A specimen was obtained for cervical cytology. Bimanual examination reveals no cervical tenderness or masses. Uterus and ovaries are nontender and of nl size.
15. Inguinal area: No lymphadenopathy is noted. Femoral pulses are 2+ and equal bilaterally. Auscultation reveals no femoral bruits.
16. Extremities: There is no clubbing, cyanosis, or edema. Brachial, radial, popliteal, dorsalis pedis, and posterior tibialis pulses are 2+ and equal bilaterally. Musculoskeletal examination reveals no joint deformities and full range of motion. No bone, joint, or muscle tenderness is noted.
17. Neurologic: Pt is alert and oriented to time, person, and place. Cranial nerves II to XII are within nl limits. Speech, memory, and expression are within nl limits. Muscle strength is 5/5 in both upper and lower extremities. No muscle atrophy or involuntary movement is noted. Testing of cerebellar function reveals nl gait, (−) Romberg test result, and good coordination in finger-to-nose, heel-to-shin, and alternate motion testing. Sensory is intact to light touch, pain, and vibratory stimuli. No focal motor or sensory deficits are present. Deep tendon reflexes are 2+ and equal bilaterally.
4. Progress (SOAP) Note
S, Subjective: observations, pt complaints.
O, Objective: description of physical findings and recording of laboratory, x-ray, or ECG data.
A, Assessment: analysis of data and tentative dx.
P, Plan: diagnostic studies and therapeutic regimen.
5. Consult Note
 Date/time
Date/time Reason for consult
Reason for consult HPI
HPI Current medications
Current medications Physical exam
Physical exam Impression
Impression Recommendations
Recommendations6. Discharge Summary
The discharge summary should contain only essential information about the investigation and Rx of the pt’s illness. It should briefly describe the following:
 Why the pt entered the hospital: a brief statement of the CC, admission dx, and HPI.
Why the pt entered the hospital: a brief statement of the CC, admission dx, and HPI. The pertinent laboratory, x-ray, and physical findings; (−) findings may be as pertinent as (+) findings.
The pertinent laboratory, x-ray, and physical findings; (−) findings may be as pertinent as (+) findings. The medical or surgical Rx, including the pt’s response, any complications, and consultations; a rationale for what was or was not done.
The medical or surgical Rx, including the pt’s response, any complications, and consultations; a rationale for what was or was not done. The pt’s condition when discharged (ambulation, self-care, ability to work).
The pt’s condition when discharged (ambulation, self-care, ability to work). Instructions given on continuing care, such as medication by name and specific dosage, diet, type and amount of physical activity, other therapeutic measures, referrals, and appointments.
Instructions given on continuing care, such as medication by name and specific dosage, diet, type and amount of physical activity, other therapeutic measures, referrals, and appointments.7. Pronouncing Death While on Call
The legal criteria of death fall within state jurisdiction. One should become familiar with the accepted definition of death in one’s own state. When called to pronounce a pt dead, the following steps should be followed:
1. Identify the pt (examine hospital ID tag on the pt’s wrist).
2. Examine pt for:
a. Response to verbal or tactile stimuli (none)
b. Spontaneous respiration (none)
c. Heart sounds and pulses (absent)
d. Pupillary response (pupils fixed and dilated)
3. Document the time the pt was pronounced dead (legal time of death).
4. Notify attending physician (if not already done by the nursing staff) and inquire whether family requests autopsy. Notify the organ bank for possible organ donation, if this is consistent with your hospital’s policy.
5. Document findings in pt’s chart (e.g., “Called by charge nurse to pronounce Mr. John Smith dead. Pt examined, unresponsive to verbal or tactile stimuli, no spontaneous respiration noted, heart sounds not audible, pulses absent, pupils fixed and dilated. Pt pronounced dead at 11:10 pm. Attending notified. Next of kin to be contacted by attending.”) The attending will often not be available, and you will be asked to notify the next of kin.
a. Familiarize yourself with the pt’s medical hx and mode of death.
b. Identify yourself to the family in a humble and caring manner and inform them that their next of kin has expired. Inform them of the time that the pt was pronounced dead, and always try to comfort them that their relative died peacefully.
c. If it is not clear from the pt’s records, inquire whether the family requests an autopsy.
d. Ask the next of kin whether the family will be coming to the hospital to view the body before it is transported to the hospital morgue. Notify the charge nurse of their decision.
8. Discharge Against Medical Advice (AMA)
1. Discharge AMA, in which a pt chooses to leave the hospital before the treating physician recommends discharge, occurs in 2% of medical admissions.
2. Risk factors are h/o substance or EtOH abuse, lack of insurance, younger age, and male sex.
3. Strategies for preventing AMA discharges include proactively addressing substance abuse issues and recognizing and treating psychological factors. Motivational interviewing, which relies on the principle of pt-centered interviewing and use of nonjudgmental empathetic questioning, is an effective modality in lowering the risk of discharge AMA.
4. If prevention of discharge AMA is not successful, informed consent is a crucial element in managing an AMA discharge. An informed decision means that the decision has been made by the pt in consultation with the physician without being coerced and with a full understanding of the risks, benefits, and alternatives of the decision.
5. The evaluation of the pt being discharged AMA should include the following:
a. Does the pt understand and appreciate the admission dx, prognosis, and risks and benefits of leaving the hospital? It is important to document that the pt understands the information, terminology, and language (has adequate health literacy).
b. Is the pt aware of alternative Rxs outside of the hospital and associated risks and benefits?
c. Is the pt able to make and communicate his/her choice?
d. Can the pt articulate a reason for the choice that is consistent with his/her choice?
6. If a pt is deemed to be without decision-making capacity and has no surrogate, consultation with a psychiatrist may be helpful to keep the pt in the hospital against his/her will.
7. Managing an AMA discharge also includes ensuring that the discharge is as safe as possible under the circumstances and helping the pt follow up after discharge.
Reference
“I’m going home”: Discharges against medical advice. Mayo Clin Proc. 2009;84:255–260.
B
Evaluating the Labs
This section covers >150 labs. Each test is approached with the following format:
1. Lab test.
2. Normal (nl) range in adult pts.
3. Common abnormalities (e.g., [+] test result, ↑ or ↓ value).
4. Causes of abnl result.
The nl ranges may differ slightly, depending on the laboratory. The reader should be aware of the “nl range” of the particular laboratory performing the test. Every attempt has been made to present current laboratory test data with emphasis on practical considerations. Lab tests do not make diagnoses, physicians do. As such, any lab results should be integrated with the complete clinical picture and radiographic studies (if needed) to make a dx.
ACE Level
Acetone (Serum or Plasma)
Nl: (−)
↑: DKA, starvation, isopropanol ingestion.
Acetylcholine Receptor (ACHR) Antibody
Nl: <0.03 nmol/L.
↑: myasthenia gravis. Changes in AChR concentration correlate w/the clinical severity of myasthenia gravis after Rx and during Rx w/prednisone and immunosuppressants. False-(+) AChR Ab results may be found in pts w/Eaton-Lambert syndrome.
Acid Phosphatase (Serum)
Nl range: enzymatic, prostatic, 0-5.5 U/L; enzymatic, total, 2-12 U/L.
Activated Clotting Time (ACT)
Nl: This test is used to determine the dose of protamine sulfate to reverse the effect of heparin as an anticoagulant during angioplasty, cardiac surgery, and hemodialysis. The accepted goal during cardiopulmonary bypass surgery is usually 400 to 500 seconds.
Activated Partial Thromboplastin Time (APTT)
Adrenocorticotropic Hormone (ACTH)
Nl: 9-52 pg/mL.
↑: Addison’s disease, ectopic ACTH-producing tumors, congenital adrenal hyperplasia, Nelson’s syndrome, pituitary-dependent Cushing’s disease.
↓: secondary adrenocortical insufficiency, hypopituitarism, adrenal adenoma or adrenal carcinoma.
Alanine Aminotransferase (ALT, SGPT)
Nl range: 8-35 U/L (female); 10-40 U/L (male).
↑: liver disease (e.g., hepatitis, cirrhosis, Reye’s syndrome), EtOH abuse, drugs (e.g., acetaminophen, statins, NSAIDs, abx, anabolic steroids, narcotics, heparin, labetalol, amiodarone, chlorpromazine, phenytoin), hepatic congestion, infectious mononucleosis, liver mets, MI, myocarditis, severe muscle trauma, dermatomyositis or polymyositis, muscular dystrophy, malignant neoplasms, renal and pulmonary infarction, convulsions, eclampsia, dehydration (relative ↑), Chinese herbs.
↓: azotemia, advanced malnutrition, chronic renal dialysis, chronic alcoholic liver disease, metronidazole therapy.
Albumin (Serum)
Nl range: 4-6 g/dL.
↑: dehydration (relative ), IV alb infusion.
↓: liver disease, nephrotic syndrome, poor nutritional status, rapid IV hydration, protein-losing enteropathies (IBD), severe burns, neoplasia, chronic inflammatory diseases, pregnancy, prolonged immobilization, lymphomas, hypervitaminosis A, chronic GN.
Aldosterone (Plasma)
Nl: 3-16 ng/dL (adult supine); 7-30 ng/dL (adult upright); 200-800 ng/dL (adrenal vein).
↑: aldosterone-secreting adenoma, bilateral adrenal hyperplasia, secondary aldosteronism (diuretics, CHF, laxatives, nephritic syndrome, cirrhosis w/ascites, Bartter’s syndrome, pregnancy, starvation).
↓: Addison’s disease, renin deficiency, Turner’s syndrome, DM, isolated aldosterone deficiency, post–acute EtOH intoxication (hangover phase).
Alkaline Phosphatase (Serum)
Nl range: 30-120 U/L.
↑: biliary obstruction, cirrhosis (particularly PBC), liver disease (hepatitis, infiltrative liver diseases, fatty metamorphosis), Paget’s disease of bone, osteitis deformans, rickets, osteomalacia, hypervitaminosis D, hyperparathyroidism, hyperthyroidism, UC, bowel perforation, bone mets, healing fxs, bone neoplasms, acromegaly, infectious mononucleosis, CMV infections, sepsis, pulmonary infarction, hypernephroma, leukemia, myelofibrosis, MM, drugs (estrogens, alb, erythromycin and other abx, cholestasis-producing drugs [phenothiazines]), pregnancy, puberty, postmenopausal women.
↓: hypothyroidism, pernicious anemia, hypophosphatemia, hypervitaminosis D, malnutrition.
Alpha1-Fetoprotein (Serum)
Nl range: 0-20 ng/mL.
↑: hepatocellular carcinoma (usually values >1000 ng/mL), germinal neoplasms (testis, ovary, mediastinum, retroperitoneum), liver disease (alcoholic cirrhosis, acute hepatitis, chronic active hepatitis), fetal anencephaly, spina bifida, basal cell carcinoma, breast carcinoma, pancreatic carcinoma, gastric carcinoma, retinoblastoma, esophageal atresia.
ALT
Aluminum (Serum)
Nl range: 0-6 ng/mL.
↑: chronic renal failure on dialysis, parenteral nutrition, industrial exposure.
AMA
Ammonia (Serum)
Nl range: 15-45 μm/dL (adults); 29-70 μm/dL (children).
↑: hepatic failure, hepatic encephalopathy, Reye’s syndrome, portacaval shunt, drugs (diuretics, polymyxin B, methicillin).
↓: drugs (neomycin, lactulose), renal failure.
Amylase (Serum)
Nl range: 0-130 U/L.
↑: acute pancreatitis, macroamylasemia, salivary gland inflammation, mumps; pancreatic neoplasm, abscess, pseudocyst, ascites; perforated peptic ulcer; intestinal obstruction, intestinal infarction; acute cholecystitis, appendicitis, ruptured ectopic pregnancy, peritonitis, burns, DKA, renal insufficiency; drugs (morphine); carcinomatosis of lung, esophagus, ovary; acute ethanol ingestion; prostate tumors; after ERCP; bulimia, anorexia nervosa.
↓: advanced chronic pancreatitis, hepatic necrosis, cystic fibrosis.
Amylase, Urine
See Urine Amylase
ANA
ANCA
Angiotensin II
Nl: 10-60 pg/mL.
↑: HTN, CHF, cirrhosis, renin-secreting renal tumor, volume depletion.
↓: ACEIs, ARB drugs, primary aldosteronism, Cushing’s syndrome.
Angiotensin-Converting Enzyme (ACE Level)
Nl range: <40 nmol/mL/min.
↑: sarcoidosis, PBC, alcoholic liver disease, hyperthyroidism, hyperparathyroidism, DM, amyloidosis, MM, lung disease (asbestosis, silicosis, berylliosis, allergic alveolitis, coccidioidomycosis), Gaucher’s disease, leprosy.
↓: ACEI Rx.
Anion Gap
Nl range: 9-14 mEq/L.
↑: lactic acidosis, ketoacidosis (DKA, alcoholic starvation), uremia (chronic renal failure), ingestion of toxins (paraldehyde, methanol, salicylates, ethylene glycol), hyperosmolar nonketotic coma, abx (carbenicillin).
↓: hypoalbuminemia, severe hypermagnesemia, IgG myeloma, lithium toxicity, laboratory error (falsely ↓ Na+ or overestimation of HCO3− or chloride), hypercalcemia of parathyroid origin, abx (e.g., polymyxin).
Anticardiolipin Antibody (ACA)
Nl range: (−) Test includes detection of IgG, IgM, and IgA Ab to phospholipid, cardiolipin.
Present in: antiphospholipid Ab syndrome, chronic HCV infection.
Anticoagulant
Antidiuretic Hormone (ADH)
Nl: 295-300 mOsm/kg; 4-12 pg/mL.
↑: SIADH, antipsychotic meds, ectopic ADH from systemic neoplasm, GBS, CNS infections, brain tumors, nephrogenic diabetes insipidus.
↓: central diabetes insipidus, nephritic syndrome, psychogenic polydipsia, demeclocycline, lithium, phenytoin, EtOH.
Anti-DNA
Nl range: absent.
Anti-DS DNA
Nl: <25 U.
↑: SLE.
Anti–Glomerular Basement Antibody
Anti-HCV
Antimitochondrial Antibody (AMA)
Nl range: <1:20 titer.
↑: PBC (85%-95%), chronic active hepatitis (25%-30%), cryptogenic cirrhosis (25%-30%).
Antineutrophil Cytoplasmic Antibody (ANCA)
(+) test result:
• Cytoplasmic pattern (cANCA): (+) in Wegener’s granulomatosis.
• Perinuclear pattern (pANCA): (+) in IBD, PBC, PSC, autoimmune chronic active hepatitis, crescentic GN.
Antinuclear Antibody (ANA)
Nl range: <1:20 titer.
(+) test: SLE (more significant if titer >1:160), drugs (phenytoin, ethosuximide, primidone, methyldopa, hydralazine, carbamazepine, PCN, procainamide, chlorpromazine, griseofulvin, thiazides), chronic active hepatitis, age >60 years (particularly age >80 years), RA, scleroderma, MCTD, necrotizing vasculitis, Sjögren’s syndrome.
Antiphospholipid Antibody
Anti-RNP Antibody
Anti–SCL-70
Nl: absent.
↑: scleroderma.
Anti-SM (Anti-Smith) Antibody
Anti–Smooth Muscle Antibody
Antithrombin III
Nl range: 81%-120% of nl activity; 17-30 mg/dL.
↓: hereditary deficiency of antithrombin III, DIC, PE, cirrhosis, thrombolytic Rx, chronic liver failure, postsurgery, third trimester of pregnancy, OCPs, nephrotic syndrome, IV heparin >3 days, sepsis, acute leukemia, carcinoma, thrombophlebitis.
↑: warfarin Rx, after MI.
Apolipoprotein A-1 (APO A-1)
Nl: recommended > 120 mg/dL.
↑: familial hyperalphalipoproteinemia, statins, niacin, estrogens, weight loss, familial CETP deficiency.
↓: familial hypoalphalipoproteinemia, Tangier disease, diuretics, androgens, cigarette smoking, hepatocellular disorders, chronic renal failure, nephritic syndrome, coronary heart disease, cholestasis.
Apolipoprotein B (APO B)
Nl: desirable <100 mg/dL; high risk >120 mg/dL.
↑: high–saturated fat diet, high-cholesterol diet, hyperapobetalipoproteinemia, familial combined hyperlipidemia, anabolic steroids, diuretics, β-blockers, corticosteroids, progestins, diabetes, hypothyroidism, chronic renal failure, liver disease, Cushing’s syndrome, coronary heart disease.
Arterial Blood Gases (ABGS)
Nl range:
• PO2: 75-100 mm Hg
• PCO2: 35-45 mm Hg
• HCO3−: 24-28 mEq/L
• pH: 7.35-7.45
Abnl values: Refer to individual acid-base disturbances in Chapter 9.
Aspartate Aminotransferase (AST, SGOT)
Nl range: 0-35 U/L.
↑: liver disease (hepatitis, hemochromatosis, cirrhosis, Reye’s syndrome, Wilson’s disease), EtOH abuse, drugs (acetaminophen, statins, NSAIDs, ACEIs, heparin, labetalol, phenytoin, amiodarone, chlorpromazine), hepatic congestion, infectious mononucleosis, MI, myocarditis, severe muscle trauma, dermatomyositis and polymyositis, muscular dystrophy, malignant neoplasia, renal and pulmonary infarction, convulsions, eclampsia.
↓: uremia, vitamin B6 deficiency.
Basophil Count
Nl range: 0.4%-1% of total WBCs; 40-100/mm3.
↑: inflammatory processes, leukemia, PV, Hodgkin’s lymphoma, hemolytic anemia, after splenectomy, myeloid metaplasia, myxedema.
↓: stress, hypersensitivity reaction, steroids, pregnancy, hyperthyroidism.
Bicarbonate
Nl: 21-28 mEq/L (arterial); 22-29 mEq/L (venous).
↑: metabolic alkalosis, compensated respiratory acidosis, diuretics, corticosteroids, laxative abuse.
↓: metabolic acidosis, compensated respiratory alkalosis; acetazolamide, cyclosporine, cholestyramine, methanol or ethylene glycol poisoning.
Bile Acid Breath Test
Nl: The test determines the radioactivity of 14CO2 in breath samples at 2 and 4 hr.
• 2 hr after dose: 0.11 ± 0.14
• 4 hr after dose: 0.52 ± 0.09
↑: GI bacterial overgrowth, cimetidine.
Bilirubin, Direct (Conjugated Bilirubin)
Nl range: 0-0.2 mg/dL.
↑: hepatocellular disease, biliary obstruction, drug-induced cholestasis, hereditary disorders (Dubin-Johnson syndrome, Rotor’s syndrome), advanced neoplastic states.
Bilirubin, Indirect (Unconjugated Bilirubin)
Nl range: 0-1.0 mg/dL.
↑: hemolysis, liver disease (hepatitis, cirrhosis, neoplasm), hepatic congestion caused by CHF, hereditary disorders (Gilbert’s disease, Crigler-Najjar syndrome).
Bilirubin, Total
Nl range: 0-1.0 mg/dL.
↑: liver disease (hepatitis, cirrhosis, cholangitis, neoplasm, biliary obstruction, infectious mononucleosis), hereditary disorders (Gilbert’s disease, Dubin-Johnson syndrome), drugs (steroids, diphenylhydantoin, phenothiazines, PCN, erythromycin, clindamycin, captopril, amphotericin B, sulfonamides, azathioprine, isoniazid, 5-aminosalicylic acid, allopurinol, methyldopa, indomethacin, halothane, OCPs, procainamide, tolbutamide, labetalol), hemolysis, pulmonary embolism or infarct, hepatic congestion resulting from CHF.
Bleeding Time (Modified IVY Method)
Nl range: 2-9.5 minutes.
↑: thrombocytopenia, capillary wall abnormalities, Plt abnormalities (Bernard-Soulier disease, Glanzmann’s disease), drugs (ASA, warfarin, anti-inflammatory medications, streptokinase, urokinase, dextran, β-lactam abx, moxalactam), DIC, cirrhosis, uremia, myeloproliferative disorders, vWD.
Comments: The bleeding time test as a method to evaluate suspected hemostatic incompetence has been replaced in many laboratories by Plt function analysis (PFA-100 assay). The bleeding time test’s ability to predict excessive bleeding in clinical situations, such as surgery or invasive diagnostic procedures, is poor. It may play a limited residual role in the evaluation of suspected hereditary disorders of hemostasis.
BNP
BRCA1, BRCA2
Test involves the detection of carriers of mutations in the genes characterized by predisposition to breast and ovarian cancers. These mutations occur in about 1 in 300 to 500 women in the general population and in about 2% of Ashkenazi Jewish women. Women found to carry the mutation should undergo earlier and more intensive surveillance for breast cancer. Pre-test counseling should be provided before genetic testing. The U.S. Preventive Services Task Force recommends screening in the following:
1. Non-Ashkenazi women:
a. Two first-degree relatives w/breast or ovarian cancer (including one diagnosed ≤50 years of age).
b. ≥3 first- or second-degree relatives w/breast cancer.
c. Both breast cancer and ovarian cancer among first- and second-degree relatives.
d. A first-degree relative w/bilateral breast cancer.
e. ≥2 first- or second-degree relatives w/ovarian cancer.
f. A first- or second-degree relative w/both breast and ovarian cancer.
g. A male relative w/breast cancer.
2. Ashkenazi women:
a. Any first-degree relative w/breast or ovarian cancer.
b. 2 second-degree relatives on the same side of the family w/breast or ovarian cancer.
Breath Hydrogen Test
Nl: This test is for bacterial overgrowth H2 excretion; fasting: 4.6 ± 5.1; after lactulose: early ↑ <12. Lactulose usually results in a colonic response >30 minutes after ingestion.
↑: a high fasting breath H2 level and an ↑ of at least 12 ppm within 30 minutes after lactulose challenge indicate bacterial overgrowth in the small intestine. The ↑ must precede the colonic response.
False (+): accelerated gastric emptying, laxative use.
False (−): use of abx and pts who are non–hydrogen producers.
B-Type Natriuretic Peptide (BNP)
Nl range: up to 100 μg/L. Natriuretic peptides are secreted to regulate fluid volume, BP, and electrolyte balance. They have activity in the central and peripheral nervous system. In humans, the main source of circulatory BNP is the heart ventricles.
↑: heart failure. This test is useful to differentiate heart failure from COPD manifesting w/dyspnea. Levels are also ↑ in asymptomatic left ventricular dysfunction, arterial and pulmonary HTN, cardiac hypertrophy, valvular heart disease, arrhythmia, and ACS.
BUN
See Urea Nitrogen
C3
See Complement C3
C4
See Complement C4
Calcitonin (Serum)
Nl range: <100 pg/mL.
↑: medullary carcinoma of the thyroid (particularly if level >1500 pg/mL), carcinoma of the breast, apudomas, carcinoids, renal failure, thyroiditis.
Calcium (Serum)
Nl range: 8.8-10.3 mg/dL.
Captopril Stimulation Test
Nl: The test is performed by giving 25 mg captopril PO after an overnight fast. The pt should be seated during the test. After captopril, aldosterone <15 ng/dL, renin >2 ng angiotensin I/mL/hr.
Interpretation: In pts w/primary aldosteronism, plasma aldosterone remains high and PRA remains low after captopril.
Carbon Dioxide, Partial Pressure
Carbon Monoxide
Carboxyhemoglobin
Nl range: saturation of Hgb <2%; smokers <9% (coma, 50%; death, 80%).
↑: smoking, exposure to smoking, exposure to automobile exhaust fumes, malfunctioning gas-burning appliances.
Carcinoembryonic Antigen (CEA)
Nl range: 0-2.5 ng/mL (nonsmokers); 0-5 ng/mL (smokers).
↑: colorectal carcinomas, pancreatic carcinomas, and metastatic disease usually produce higher elevations (>20 ng/mL); carcinomas of the esophagus, stomach, small intestine, liver, breast, ovary, lung, and thyroid usually produce lesser elevations; benign conditions (smoking, IBD, hypothyroidism, cirrhosis, pancreatitis, infections) usually produce levels <10 ng/mL.
Cardio CRP
Carotene (Serum)
Nl range: 50-250 μg/dL.
↑: carotenemia, chronic nephritis, DM, hypothyroidism, nephrotic syndrome, hyperlipidemia.
↓: fat malabsorption, steatorrhea, pancreatic insufficiency, lack of carotenoids in diet, high fever, liver disease.
CBC
CD4+ T-Lymphocyte Count (CD4+ T Cells)
Calculated as total WBC × % lymphocytes × % lymphocytes stained w/CD4.
This test is used primarily to evaluate immune dysfunction in HIV infection. It is useful as a prognostic indicator and as a criterion for initiation of prophylaxis for several opportunistic infections that are sequelae of HIV infection. Progressive depletion of CD4+ T lymphocytes is associated w/ ↑ likelihood of clinical complications. Adolescents and adults w/HIV infection are classified as having AIDS if their CD4+ lymphocyte count is <200/μL or if their CD4+ T-lymphocyte percentage is <14%. HIV-infected pts whose CD4+ count is <200/μL and who acquire certain infectious diseases or malignant neoplasms are also classified as having AIDS. Corticosteroids ↓ CD4+ T-cell % and absolute number.
CEA
Ceruloplasmin (Serum)
Nl range: 20-35 mg/dL.
↑: pregnancy, estrogens, OCPs, neoplastic diseases (leukemias, Hodgkin’s lymphoma, carcinomas), inflammatory states, SLE, PBC, RA.
↓: Wilson’s disease (values often <10 mg/dL), nephrotic syndrome, advanced liver disease, malabsorption, TPN, Menkes’ syndrome.
Chlamydia Group Antibody Serologic Test
Test description: Acute and convalescent serum samples are drawn 2 to 4 weeks apart. A fourfold ↑ in titer between acute and convalescent sera is necessary for confirmation. A single titer >1:64 is considered indicative of infection.
Chloride (Serum)
Nl range: 95-105 mEq/L.
↑: dehydration, Na+ loss > chloride loss, respiratory alkalosis, excessive infusion of NS solution, cystic fibrosis, hyperparathyroidism, renal tubular disease, metabolic acidosis, prolonged diarrhea, acetazolamide administration, diabetes insipidus, ureterosigmoidostomy.
↓: vomiting, gastric suction, primary aldosteronism, CHF, SIADH, Addison’s disease, salt-losing nephritis, continuous infusion of D5W, thiazide diuretic administration, diaphoresis, diarrhea, burns, DKA.
Chloride (Sweat)
Nl: 0-40 mmol/L.
Borderline/indeterminate: 41-60 mmol/L.
Consistent with cystic fibrosis: >60 mmol/L.
Cholesterol, Low-Density Lipoprotein
Cholesterol, High-Density Lipoprotein
Cholesterol, Total
Nl range: Generally <200 mg/dL.
↑: primary hypercholesterolemia, biliary obstruction, DM, nephrotic syndrome, hypothyroidism, PBC, diet high in cholesterol and total and saturated fat, third trimester of pregnancy, drugs (steroids, phenothiazines, OCPs).
↓: use of lipid-lowering agents (statins, niacin, ezetimibe, cholestyramine, colesevelam); starvation, malabsorption, abetalipoproteinemia, hyperthyroidism; hepatic failure, carcinoma, infection, inflammation.
Chorionic Gonadotropins, Human (Serum)
Nl range, serum: <0.8 IU/L (female, premenopausal); <3.3 IU/L (female, postmenopausal); <0.7 IU/L (male).
↑: pregnancy, choriocarcinoma, gestational trophoblastic neoplasia (including molar gestations), placental site trophoblastic tumors; human antimouse antibodies (HAMA) can produce false serum assay for hCG.
The principal use of this test is to diagnose pregnancy. The concentration of hCG ↑ significantly during the initial 6 weeks of pregnancy. Peak values approaching 100,000 IU/L occur 60 to 70 days after implantation.
hCG levels generally double every 1 to 3 days. In pts w/concentration <2000 IU/L, an ↑ of serum hCG <66% after 2 days suggests spontaneous abortion or ruptured ectopic gestation.
Chymotrypsin
Nl: <10 μg/L.
↑: acute pancreatitis, chronic renal failure, PO enzyme preparations, gastric cancer, pancreatic cancer.
↓: chronic pancreatitis, late cystic fibrosis.
Circulating Anticoagulant (Antiphospholipid Antibody, Lupus Anticoagulant)
Nl: (−)
Detected in: SLE, drug-induced lupus, long-term phenothiazine Rx, MM, UC, RA, post partum, hemophilia, neoplasms, chronic inflammatory states, AIDS, nephrotic syndrome.
Note: The name is a misnomer because these pts are prone to hypercoagulability and thrombosis.
CK
See Creatine Kinase
Clonidine Suppression Test
Interpretation: Clonidine inhibits neurogenic catecholamine release and will cause a ↓ in plasma norepinephrine into the reference interval in hypertensive subjects w/o pheochromocytoma. The test is performed by giving 4.3 μg clonidine/kg PO after an overnight fast. Norepinephrine is measured at 3 hr. The result should be within established reference range and ↓ to <50% of baseline concentration. Lack of ↓ in norepinephrine suggests pheochromocytoma.
Clostridium Difficile Toxin Assay (Stool)
Nl: (−)
Detected in: abx-associated diarrhea and pseudomembranous colitis.
CO
Coagulation Factors
Factor reference ranges:
• V: >10%
• VII: >10%
• VIII: 50%-170%
• IX: 60%-136%
• X: >10%
• XI: 50%-150%
• XII: >30%
Figure 1-2 illustrates the blood coagulation pathways.

FIGURE 1-2 Coagulation cascade. Fibrin clot formation results from the generation of thrombin, which depends on the sequential interaction of proenzymes and activated coagulation factors in the intrinsic, extrinsic, and common pathways of coagulation. (From Noble J [ed]: Primary Care Medicine, 3rd ed. St. Louis, Mosby, 2001.)
Cold Agglutinins Titer
Nl range: <1:32.
↑: primary atypical pneumonia (Mycoplasma pneumonia), infectious mononucleosis, CMV infection, others (hepatic cirrhosis, acquired hemolytic anemia, frostbite, MM, lymphoma, malaria).
Complement (C3, C4)
Nl range:
• C3: 70-160 mg/dL
• C4: 20-40 mg/dL
Abnl values:
• ↓ C3: active SLE, immune complex disease, AGN, inborn C3 deficiency, membranoproliferative GN, infective endocarditis, serum sickness, autoimmune-type chronic active hepatitis.
• ↓ C4: immune complex disease, active SLE, infective endocarditis, inborn C4 deficiency, hereditary angioedema, hypergammaglobulinemic states, cryoglobulinemic vasculitis.
Complete Blood Count (CBC)
WBCs: 3200-9800/mm3
RBCs: 4.3-5.9 106/mm3 (male); 3.5-5.0 106/mm3 (female)
Hgb: 13.6-17.7 g/dL (male); 12-15 g/dL (female)
Hct: 39%-49% (male); 33%-43% (female)
MCV: 76-100 μm3
MCH: 27-33 pg
MCHC: 33-37 g/dL
RDW: 11.5%-14.5%
Plt count: 130-400 × 103/mm3
Diff: 2-6 bands (early mature neutrophils); 60-70 segs (mature neutrophils); 1-4 eosinophils; 0-1 basophils; 2-8 monocytes; 25-40 lymphocytes
Conjugated Bilirubin
Coombs, Direct (Antiglobulin Test, Direct, DAT)
Nl: (−)
(+): AIHA, erythroblastosis fetalis, transfusion reactions, drugs (methyldopa, PCNs, tetracycline, sulfonamides, levodopa, cephalosporins, quinidine, insulin).
Coombs, Indirect
Nl: (−)
(+): acquired hemolytic anemia, incompatible crossmatched blood, anti-Rh antibodies, drugs (methyldopa, mefenamic acid, levodopa).
Copper (Serum)
Nl range: 70-140 μg/dL.
↓: Wilson’s disease, malabsorption, malnutrition, nephrosis, TPN, acute leukemia in remission.
↑: aplastic anemia, biliary cirrhosis, SLE, hemochromatosis, hyperthyroidism, hypothyroidism, infection, iron deficiency anemia, leukemia, lymphoma, OCPs, pernicious anemia, RA.
Corticotropin-Releasing Hormone (CRH) Stimulation Test
Nl: A dose of 0.5 mg of dexamethasone is given every 6 hr for 2 days; 2 hr after the last dose, 1 μg/kg CRH is given IV. Samples are drawn after 15 minutes. There is normally a twofold to fourfold ↑ in mean baseline concentration of ACTH or cortisol. Cortisol >1.4 μg/L is virtually 100% specific and 100% diagnostic.
Nl or exaggerated response: pituitary Cushing’s disease.
No response: ectopic ACTH-secreting tumor.
A (+) response to CRH or a suppressed response to high-dose dexamethasone has a 97% (+) predictive value for Cushing’s disease. However, a lack of response to either test excludes Cushing’s disease in only 64% to 78% of pts. When the tests are considered together, (−) responses from both have a 100% predictive value for ectopic ACTH secretion.
Cortisol (Plasma)
Nl range: varies w/time of collection (circadian variation):
• 8 am: 4-19 μg/dL
• 4 pm: 2-15 μg/dL
↑: ectopic ACTH production (i.e., oat cell carcinoma of lung), loss of nl diurnal variation, pregnancy, chronic renal failure, iatrogenic, stress, adrenal or pituitary hyperplasia or adenomas.
↓: primary adrenocortical insufficiency, anterior pituitary hypofunction, secondary adrenocortical insufficiency, adrenogenital syndromes.
C-Peptide
Nl range (serum): 0.51-2.70 ng/mL.
↑: insulinoma, sulfonylurea administration, type 2 DM, renal failure.
↓: type 1 DM, factitious insulin administration.
CPK
See Creatine Kinase
C-Reactive Protein (CRP)
Nl range: <1 mg/dL. CRP levels are valuable in the clinical assessment of chronic inflammatory disorders such as RA, SLE, vasculitis syndromes, and IBD.
↑: inflammatory and neoplastic diseases, MI, third trimester of pregnancy (acute-phase reactant), OCPs. Moderately high CRP concentrations (3-10 mg/L) predict ↑ risk of MI and stroke. Markedly high levels (>10 mg/L) have been shown to predict CV risk.
Note: High-sensitivity C-reactive protein (hs-CRP, Cardio CRP) is used as a cardiac risk marker. It is ↑ in pts w/silent atherosclerosis for a prolonged period before a CV event and is independent of cholesterol level and other lipoproteins. It can be used to help stratify cardiac risk.
Creatine Kinase (CK, CPK)
Nl range: 0-130 U/L.
↑: vigorous exercise, IM injections, MI, myocarditis, rhabdo, myositis, crush injury or trauma, polymyositis, dermatomyositis, muscular dystrophy, myxedema, seizures, malignant hyperthermia syndrome, CVA, pulmonary embolism and infarction, acute dissection of aorta.
Creatine Kinase Isoenzymes
CK-MB
↑: MI, myocarditis, pericarditis, muscular dystrophy, cardiac defibrillation, cardiac surgery, extensive rhabdo, strenuous exercise (e.g., marathon runners), MCTD, cardiomyopathy, hypothermia.
Note: CK-MB exists in the blood in two subforms. MB2 is released from cardiac cells and converted in the blood to MB1. Rapid assay of CK-MB subforms can detect MI (CK-MB2 ≥1.0 U/L, w/a ratio of CK-MB2/CK-MB1 ≥1.5) within the first 6 hr of onset of sx.
CK-MM
↑: crush injury, seizures, malignant hyperthermia syndrome, rhabdo, myositis, polymyositis, dermatomyositis, vigorous exercise, muscular dystrophy, IM injections, acute dissection of aorta.
CK-BB
↑: CVA, subarachnoid hemorrhage, neoplasms (prostate, GI tract, brain, ovary, breast, lung), severe shock, bowel infarction, hypothermia, meningitis.
Creatinine (Serum)
Nl range: 0.6-1.2 mg/dL.
↑: renal insufficiency (acute and chronic), ↓ renal perfusion (hypotension, dehydration, CHF), rhabdo, administration of contrast dyes, ketonemia, drugs (abx [AGs, cephalosporins], ACEIs [in pts w/RAS], diuretics).
Falsely ↑: DKA, administration of some cephalosporins (e.g., cefoxitin, cephalothin).
↓: ↓ muscle mass (including amputees and elderly), pregnancy, prolonged debilitation.
Creatinine Clearance
Nl range: 75-124 mL/min.
↑: pregnancy, exercise.
↓: renal insufficiency, drugs (e.g., cimetidine, procainamide, abx, quinidine), age.
Cryoglobulins (Serum)
Nl range: not detectable.
Present in: collagen-vascular diseases, chronic active hepatitis, CLL, hemolytic anemias, MM, Waldenström’s macroglobulinemia, Hodgkin’s disease.
Cystatin C
Nl: Cystatin C is a cysteine protease inhibitor that is produced at a constant rate by all nucleated cells. It is freely filtered by the glomerulus and reabsorbed (but not secreted) by the renal tubules w/no extrarenal excretion. Its concentration is not affected by diet, muscle mass, or acute inflammation. Nl range when measured by particle-enhanced nephelometric immunoassay (PENIA) is <0.28 mg/L.
↑: renal disorders; good predictor of the severity of ATN. Cystatin C ↑ more rapidly than Cr in the early stages of GFR impairment. The cystatin C concentration is an independent risk factor for heart failure in older adults and appears to provide a better measure of risk assessment than the serum Cr concentration.
D-Dimer
Nl range: <0.5 μg/mL.
↑: DVT, PE, high levels of RF, activation of coagulation and fibrinolytic systems from any cause.
D-dimer assay by ELISA assists in the dx of DVT and PE. This test has significant limitations because it can be ↑ whenever the coagulation and fibrinolytic systems are activated and can also be falsely ↑ w/high RF levels.
Dexamethasone Suppression Test, Overnight
Nl: Test performed by giving 1 mg dexamethasone PO at 11 pm and measuring serum cortisol at 8 am on the following morning; nl response is cortisol suppression to <3 g/dL. If dose of 4 mg dexamethasone is given, cortisol suppression will be to <50% of baseline.
Digoxin
Nl therapeutic range: 0.5-2 ng/mL.
↑: impaired renal function, excessive dosing; concomitant use of quinidine, amiodarone, verapamil, fluoxetine, nifedipine.
Dopamine
Nl range: 0-175 pg/mL.
↑: pheochromocytomas, neuroblastomas, stress, vigorous exercise, certain foods (bananas, chocolate, coffee, tea, vanilla).
Electrophoresis, Hemoglobin
Electrophoresis, Protein
ENA Complex
Endomysial Antibodies
Nl: not detected.
Present in: celiac disease, dermatitis herpetiformis.
Eosinophil Count
Nl range: 1%-4% eosinophils (0-440/mm3).
↑: allergy, parasitic infestations (trichinosis, aspergillosis, hydatidosis), angioneurotic edema, drug reactions, warfarin sensitivity, collagen-vascular diseases, acute hypereosinophilic syndrome, eosinophilic nonallergic rhinitis, myeloproliferative disorders, Hodgkin’s lymphoma, radiation Rx, NHL, L-tryptophan ingestion, urticaria, pernicious anemia, pemphigus, IBD, bronchial asthma.
Epinephrine (Plasma)
Nl range: 0-90 pg/mL.
↑: pheochromocytomas, neuroblastomas, stress, vigorous exercise, certain foods (bananas, chocolate, coffee, tea, vanilla), hypoglycemia.
Epstein-Barr Virus Serology
Nl range:
• IgG anti-VCA <1:10 or (−)
• IgM anti-VCA<1:10 or (−)
• Anti-EBNA <1.5 or (−)
Abn:
• IgG anti-VCA >1:10 or (+) indicates either current or previous infection.
• IgM anti-VCA >1:10 or (+) indicates current or recent infection.
• Anti-EBNA ≥1.5 or (+) indicates previous infection.
Erythrocyte Sedimentation Rate (ESR) (Westergren)
Nl range: 0-15 mm/hr (male); 0-20 mm/hr (female).
↑: inflammatory states (acute-phase reactant), collagen-vascular diseases, infections, MI, neoplasms, hyperthyroidism, hypothyroidism, rouleaux formation, elderly, pregnancy.
Note: Sedimentation rates >100 mm/hr are strongly associated w/serious underlying disease (collagen-vascular, infection, malignant disease). Some clinicians use ESR as a “sickness index”; high rates encountered w/o obvious reason should be repeated rather than pursuing extensive search for occult disease.
↓: sickle cell disease, polycythemia, corticosteroids, spherocytosis, anisocytosis, hypofibrinogenemia, serum viscosity, microcytosis.
Erythropoietin
Nl: 3.7-16.0 IU/L by radioimmunoassay. Erythropoietin is a glycoprotein secreted by the kidneys that stimulates RBC production by acting on erythroid committed stem cells.
↑:
• Extremely high: generally seen in pts w/severe anemia (Hct <25, Hgb <7), such as in cases of aplastic anemia, severe hemolytic anemia, hematologic cancers.
• Very high: pts w/mild to moderate anemia (Hct 25-35, Hgb 7-10).
• High: pts w/mild anemia (e.g., AIDS, myelodysplasia).
• Erythropoietin can be inappropriately ↑ in pts w/malignant neoplasms, renal cysts, after renal transplantation, and in meningioma, hemangioblastoma, and leiomyoma.
↓: renal failure, PV, autonomic neuropathy.
Ethanol (Blood)
Nl range: (−) (values <10 mg/dL are considered [−]). Ethanol is metabolized at 10-25 mg/dL/hr. Levels >80 mg/dL are considered evidence of impairment for driving. Fatal blood concentration is considered to be >400 mg/dL, although levels >400 mg/dL may be seen in pts w/chronic alcoholism.
Extractable Nuclear Antigen (ENA Complex, Anti-RNP Antibody, Anti-SM, Anti-Smith)
Nl: (−)
Present in: SLE, RA, Sjögren’s syndrome, MCTD.
Factor V Leiden
Test description: PCR test is performed on whole blood or tissue. This single mutation, found in 2% to 8% of the general white population, is the single most common cause of hereditary thrombophilia.
FBS
See Glucose, Fasting
FDP
Fecal Fat, Qualitative
See Sudan III Stain
Ferritin (Serum)
Nl range: 18-300 ng/mL.
↑: inflammatory states, liver disease (ferritin ↑ from necrotic hepatocytes), hyperthyroidism, neoplasms (neuroblastomas, lymphomas, leukemia, breast carcinoma), iron replacement Rx, hemochromatosis, hemosiderosis.
↓: iron deficiency anemia.
Fibrin Degradation Product (FDP)
Nl range: <10 μg/mL.
↑: DIC, primary fibrinolysis, PE, severe liver disease.
Note: The presence of RF may cause falsely ↑ FDP.
Fibrinogen
Nl range: 200-400 mg/dL.
↑: tissue inflammation or damage (acute-phase protein reactant), OCPs, pregnancy, acute infection, MI.
↓: DIC, hereditary afibrinogenemia, liver disease, primary or secondary fibrinolysis, cachexia.
Fluorescent Treponemal Antibody
See FTA-ABS (Serum)
Folate (Folic Acid)
Nl range:
• Plasma: <3.4 ng/mL (low); >5.4 ng/mL (nl)
• RBC: >280 ng/mL
↓: folic acid deficiency (inadequate intake, malabsorption), alcoholism, drugs (MTX, trimethoprim, phenytoin, OCPs, sulfasalazine), vitamin B12 deficiency (defective red cell folate absorption), hemolytic anemia.
↑: folic acid Rx.
Follicle-Stimulating Hormone (FSH)
Nl range:
• Female, adult: <40 IU/L (midcycle); <20 IU/L (non-midcycle); 40-160 IU/L (postmenopausal)
• Male, adult: <22 IU/L
↑: primary hypogonadism, gonadal failure, alcoholism, Klinefelter’s syndrome, testicular feminization, anorchia, castration.
Free Insulin
See Insulin, Free
Free T4
See T4, Free
Free Thyroxine Index
Nl range: 1.1-4.3.
Serum free T4 directly measures unbound thyroxine. Free T4 can be measured by equilibrium dialysis (gold standard of free T4 assays) or by immunometric techniques (influenced by serum levels of lipids, proteins, and certain drugs). The FTI can also be easily calculated by multiplying T4 times T3RU and dividing the result by 100; the FTI corrects for any abnl T4 values secondary to protein binding: FTI = T4 xT3RU/100.
FTA-ABS (Serum)
Nl: nonreactive.
Reactive in: syphilis, other treponemal diseases (yaws, pinta, bejel), SLE, pregnancy.
Furosemide Stimulation Test
Nl: The test is performed by giving 60 mg furosemide PO after overnight fast. Pt should be on a nl diet w/o medications the week before the test. Nl results: renin 1-6 ng angiotensin L/ml/hr.
↑: renovascular HTN, Bartter’s syndrome, high-renin essential HTN, pheochromocytoma.
No response in: primary aldosteronism, low-renin essential HTN, hyporeninemic hypoaldosteronism.
Gamma-Glutamyltransferase (GGT)
Nl range: 0-30 U/L.
↑: chronic alcoholic liver disease, neoplasms (hepatoma, metastatic disease to the liver, carcinoma of the pancreas), nephrotic syndrome, sepsis, cholestasis, drugs (phenytoin, barbiturates).
Gastrin (Serum)
Nl range: 0-180 pg/mL.
↑: Zollinger-Ellison syndrome (gastrinoma), use of PPIs, chronic renal failure, gastric ulcer, chronic atrophic gastritis, pyloric obstruction, malignant neoplasms of the stomach, H2 blockers, Ca Rx, UC, RA.
GGT
Glomerular Basement Membrane Antibody
Nl: (−)
Present in: Goodpasture’s syndrome.
Glomerular Filtration Rate
Nl:
• Age 20-29: 116 mL/min/1.73 m2
• Age 30-39: 107 mL/min/1.73 m2
• Age 40-49: 99 mL/min/1.73 m2
• Age 50-59: 93 mL/min/1.73 m2
• Age 60-69: 85 mL/min/1.73 m2
• Age >70: 75 mL/min/1.73 m2
↓: renal insufficiency, ↓ renal blood flow.
Glucagon
Nl: 20-100 pg/mL.
↑: glucagonoma (900-7800 pg/mL), chronic renal failure, DM, glucocorticoids, insulin, nifedipine, danazol, sympathomimetic amines.
↓: hyperlipoproteinemia (types III, IV), β-blockers, secretin.
Glucose, Fasting (Fasting Blood Sugar, FBS)
Nl range: 60-99 mg/dL.
↑: DM, stress, infections, MI, CVA, Cushing’s syndrome, acromegaly, acute pancreatitis, glucagonoma, hemochromatosis, drugs (glucocorticoids, diuretics [thiazides, loop diuretics]), impaired glucose tolerance.
Glucose, Postprandial
Nl range: <140 mg/dL.
↑: DM, impaired glucose tolerance.
↓: after administration of oral hypoglycemic agents or insulin, after extensive GI resection, in reactive hypoglycemia, hereditary fructose intolerance, galactosemia, leucine sensitivity.
Glucose Tolerance Test
Nl values above fasting:
• 30 minutes: 30-60 mg/dL
• 60 minutes: 20-50 mg/dL
• 120 minutes: 5-15 mg/dL
• 180 minutes: fasting level or below
Abnl in: impaired glucose tolerance, DM, Cushing’s syndrome, acromegaly, pheochromocytoma, gestational diabetes.
Glycohemoglobin (HbA1c, Glycated Hemoglobin, Glycosylated Hemoglobin)
Nl range: 4.0%-6.0%.
Diabetes: ≥6.5%
↑: uncontrolled DM (glycated Hgb levels reflect the level of glucose control during the preceding 120 days), lead toxicity, alcoholism, iron deficiency anemia, hypertriglyceridemia.
↓: hemolytic anemias, ↓ RBC survival, pregnancy, acute or chronic blood loss, chronic renal failure, insulinoma, congenital spherocytosis; HbS, HbC, HbD diseases.
Haptoglobin (Serum)
Nl range: 50-220 mg/dL.
↑: inflammation (acute-phase reactant), collagen-vascular diseases, infections (acute-phase reactant), drugs (androgens), obstructive liver disease.
↓: hemolysis (intravascular more than extravascular), megaloblastic anemia, severe liver disease, large tissue hematomas, infectious mononucleosis, drugs (oral contraceptives).
Helicobacter Pylori (Serology, Stool Antigen)
Nl range: not detected.
Detected in: H. pylori infection. (+) serology can indicate current or past infection. (+) stool antigen test result indicates acute infection (sensitivity and specificity >90%). Stool testing should be delayed at least 4 weeks after eradication Rx.
Hematocrit
Nl range: 39%-49% (male); 33%-43% (female).
↑: PV, smoking, COPD, high altitudes, dehydration, hypovolemia.
↓: blood loss (GI, GU), anemia, pregnancy.
Hemoglobin
Nl range: 13.6-17.7 g/dL (male); 12.0-15.0 g/dL (female).
↑: hemoconcentration, dehydration, PV, COPD, high altitudes, false elevations (hyperlipemic plasma, WBCs >50,000 mm3), stress.
↓: hemorrhage (GI, GU), anemia.
Hemoglobin Electrophoresis
Nl range:
• HbA1: 95%-98%
• HbA2: 1.5%-3.5%
• HbF: <2%
• HbC: absent
• HbS: absent
Heparin-Induced Thrombocytopenia Antibodies
Nl: antigen assay: (−), <0.45; weak, 0.45-1.0; strong, >1.0.
↑: HIT.
Hepatitis A Antibody
Nl: (−)
Hepatitis B Antigen and Antibody
Nl: (−) These tests are ordered together and should be used only in pts who are chronically HBsAg (+). The main utility of these tests is to assess response of hepatitis B infection to Rx.
Present in: Presence of HBeAg implies that infective HBV is present in serum. However, its absence on conversion to anti-HBe does not r/o infectivity, especially in persons infected w/genotypes other than A. Measurement of HBV DNA is useful in persons w/ ↑ ALT but (−) HBeAg.
Hepatitis B Core Antibody (HBcAb)
Nl: (−)
Present in: hepatitis B. Anti-HBc assay is the first Ab test to become (+) w/exposure to HBV and persists the longest after resolution of acute infection.
Hepatitis B DNA
Nl: (−)
Present in: active hepatitis B infection. It implies infectivity of the serum. Currently used to assess response of hepatitis B to Rx.
Hepatitis B Surface Antibody (HBsAb)
Nl: (−)
Present in: after vaccination for hepatitis B (a level >10 U/L for postvaccine testing is the accepted concentration that indicates protection), after infection w/hepatitis B (it generally appears several weeks after disappearance of HBsAg).
Hepatitis B Surface Antigen (HBsAg)
Nl: not detected.
Detected in: acute viral hepatitis type B, chronic hepatitis B.
Hepatitis C Antibody (Anti-HCV)
Nl: (−)
Present in: hepatitis C. CDC guidelines recommend confirmation w/RIBA before reporting of anti-HCV as (+). HCV RNA can also be obtained if there is a high clinical suspicion of HCV despite a (−) anti-HVC, especially in immunosuppressed individuals or in the setting of acute hepatitis. Anti-HCV and the RIBA often do not become (+) during an acute infection; thus, repeated testing several months later is required if HCV RNA is (−).
Hepatitis C RNA
Nl: (−)
↑: hepatitis C. Detection of hepatitis C RNA is used to confirm current infection and to monitor Rx. Quantitative assays (viral load) are needed before Rx to assess response (<2 log ↓ after 12-week Rx indicates lack of response).
Hepatitis Delta Antigen and Antibody
Nl: (−)
↑: hepatitis delta. Hepatitis delta is a replication-defective RNA virus that requires the surface coat of hepatitis B (HBsAg) to become an infectious virus. Testing for hepatitis delta is therefore done only in pts (+) for HBsAg. It is useful in pts w/chronic hepatitis B if there is an exacerbation of stable hepatitis.
Her-2/Neu
Nl: (−)
Present in: 25%-30% of primary breast cancers. It can also be found in other epithelial tumors, including lung, hepatocellular, pancreatic, colon, stomach, ovarian, cervical, and bladder cancer. Trastuzumab (Herceptin) is a humanized monoclonal Ab against Her-2/neu. The test is useful to identify pts w/metastatic, recurrent, or Rx-refractory unresectable locally advanced breast cancer for trastuzumab Rx.
HFE Screen For Hereditary Hemochromatosis
Test description: PCR test can be performed on whole blood or tissue. One mutation (C282Y) and two polymorphisms (H63D, S65C) account for the majority of alleles associated w/this disease.
High-Density Lipoprotein (HDL) Cholesterol
Nl range: 45-70 mg/dL (male); 50-90 mg/dL (female).
↑: use of fenofibrates, niacin, estrogens, regular aerobic exercise, mild to moderate (1-oz) daily EtOH intake.
↓: familial deficiency of apoproteins, liver disease, sedentary lifestyle, acute MI, CVA, starvation.
Note: A cholesterol/HDL ratio >4.5 is associated w/risk of CAD.
Homocysteine (Plasma)
Nl range:
• 0-30 years: 4.6-8.1 μmol/L
• 30-59 years: 6.3-11.2 μmol/L (males); 4-5-7.9 μmol/L (females)
• >59 years: 5.8-11.9 μmol/L
↑: thrombophilic states; B6, B12, folic acid, riboflavin deficiency; pregnancy; homocystinuria.
Note: An ↑ homocysteine level is an independent risk factor for atherosclerosis.
hs-CRP
Human Immunodeficiency Virus Antibody, Type 1 (HIV-1)
Nl range: not detected.
Abnl result: HIV antibodies usually appear in the blood 1 to 4 months after infection.
Testing sequence:
1. ELISA is the recommended initial screening test. Sensitivity and specificity are >99%. False-(+) ELISA results may occur w/autoimmune disorders, presence of RF, presence of DLA-DR antibodies in multigravida woman, administration of influenza vaccine within 3 months of testing, hemodialysis, (+) plasma reagin test response, and certain medical disorders (hemophilia, hypergammaglobulinemia, alcoholic hepatitis).
2. A (+) ELISA result is confirmed w/Western blot. False-(+) Western blot may be caused by connective tissue disorders, human leukocyte antigen antibodies, polyclonal gammopathies, hyperbilirubinemia, presence of Ab to another human retrovirus, cross-reaction w/other non–virus-derived proteins in healthy persons. Undetermined Western blot may occur in pts w/AIDS w/advanced immunodeficiency (from loss of antibodies) and in recent HIV infections.
3. PCR is used to confirm indeterminate Western blot results or (−) results in persons w/suspected HIV infection.
Immunoglobulins
Nl range:
• IgA: 50-350 mg/dL
• IgD: <6 mg/dL
• IgE: <25 μg/dL
• IgG: 800-1500 mg/dL
• IgM: 45-150 mg/dL
↑:
• IgA: lymphoproliferative disorders, Berger’s nephropathy, chronic infections, autoimmune disorders, liver disease.
• IgE: allergic disorders, parasitic infections, immunologic disorders, IgE myeloma, AIDS, pemphigoid.
• IgG: chronic granulomatous infections, infectious diseases, inflammation, myeloma, liver disease.
• IgM: PBC, infectious diseases (brucellosis, malaria), Waldenström’s macroglobulinemia, liver disease.
↓:
• IgA: nephrotic syndrome, protein-losing enteropathy, congenital deficiency, lymphocytic leukemia, ataxia-telangiectasia, chronic sinopulmonary disease.
• IgE: hypogammaglobulinemia, neoplasm (breast, bronchial, cervical), ataxia-telangiectasia.
• IgG: congenital or acquired deficiency, lymphocytic leukemia, phenytoin, methylprednisolone, nephrotic syndrome, protein-losing enteropathy.
• IgM: congenital deficiency, lymphocytic leukemia, nephrotic syndrome.
Insulin Autoantibodies
Nl: (−)
Insulin, Free
Nl: <17 μU/mL.
↑: insulin OD, insulin resistance syndromes, endogenous hyperinsulinemia.
↓: inadequately treated type 1 DM.
Insulin-Like Growth Factor 1 (IGF-1) (Serum)
Nl range:
• Age 16-24: 182-780 ng/mL
• Age 25-39: 114-492 ng/mL
• Age 40-54: 90-360 ng/mL
• Age >55: 71-290 ng/mL
↑: adolescence, acromegaly, pregnancy, precocious puberty, obesity.
↓: malnutrition, delayed puberty, DM, hypopituitarism, cirrhosis, old age.
Insulin-Like Growth Factor 2 (IGF-2)
Nl: 288-736 ng/mL.
↑: hypoglycemia associated w/non–islet cell tumors, hepatoma, and Wilms’ tumor.
↓: GH deficiency.
International Normalized Ratio (INR)
The INR is a comparative rating of PT ratios. The INR represents the observed PT ratio adjusted by the International Reference Sensitivity Index. INR = PT pt/PT mean. The INR provides a universal result indicative of what the pt’s PT result would have been if measured by use of the primary World Health Organization International Reference reagent. For proper interpretation of INR values, the pt should be on stable anticoagulant Rx.
Recommended therapeutic INR range: 2-3
Intrinsic Factor Antibodies
Nl: (−)
Present in: pernicious anemia (>50% of pts). Cyanocobalamin may give false-(+) results.
Iron (Serum)
Nl: 65-175 μg/dL (male); 50-1170 μg/dL (female).
↑: hemochromatosis, excessive iron Rx, repeated transfusions, lead poisoning, hemolytic anemia, aplastic anemia, pernicious anemia.
↓: iron deficiency anemia, hypothyroidism, chronic infection.
Iron-Binding Capacity (TIBC)
Nl range: 250-460 μg/dL.
↑: iron deficiency anemia, pregnancy, polycythemia, hepatitis, weight loss.
↓: anemia of chronic disease, hemochromatosis, chronic liver disease, hemolytic anemias, malnutrition (protein depletion).
Iron Saturation (% Transferrin Saturation)
Nl: 20%-50% (male); 15%-50% (female).
↑: hemochromatosis, excessive iron intake, aplastic anemia, thalassemia, vitamin B6 deficiency.
↓: hypochromic anemias, GI malignant disease.
Lactate (Blood)
Nl range: 0.5-2.0 mEq/L.
↑: tissue hypoxia (shock, respiratory failure, severe CHF, severe anemia, CO or cyanide poisoning), systemic disorders (liver or renal failure, seizures), abnl intestinal flora (D-lactic acidosis), drugs or toxins (salicylates, ethanol, methanol, ethylene glycol), G6PD deficiency.
Lactate Dehydrogenase (LDH)
Nl range: 50-150 U/L.
↑: infarction of myocardium, lung, kidney; diseases of cardiopulmonary system, liver, collagen, CNS; hemolytic anemias; megaloblastic anemias; transfusions; seizures; muscle trauma; muscular dystrophy; acute pancreatitis; hypotension; shock; infectious mononucleosis; inflammation; neoplasia; intestinal obstruction; hypothyroidism.
Lactate Dehydrogenase Isoenzymes
Nl range:
Nl range:
• LDH1 < LDH2
• LDH5 < LDH4
Abnl values:
• LDH1 > LDH2: MI (can also be seen w/hemolytic anemias, pernicious anemia, folate deficiency, renal infarct)
• LDH5 > LDH4: liver disease (cirrhosis, hepatitis, hepatic congestion)
Lactose Tolerance Test (Serum)
Nl: The test is performed by giving 2 g/kg BW lactose PO and drawing glucose level at 0, 30, 45, 60, and 90 minutes. Nl response is change in glucose from fasting value to >30 mg/dL. Inconclusive response is of 20 to 30 mg/dL; abnl response is ↑<20 mg/dL.
Abnl in: lactase deficiency.
LAP Score
LDH
Lead
Nl: <10 μg/dL (child); <25 μg/dL (adult); <50 μg/dL (acceptable for industrial exposure).
↑: lead exposure, lead poisoning.
Legionella Titer
Nl: (−)
(+) in: Legionnaires’ disease (presumptive, ≥1:256 titer; definitive, fourfold titer ↑ to ≥1:128).
Leukocyte Alkaline Phosphatase (LAP)
Nl range: 13-100.
↑: leukemoid reactions, neutrophilia resulting from infections (except in sickle cell crisis—no significant ↑ in LAP score), Hodgkin’s disease, PV, hairy cell leukemia, aplastic anemia, Down syndrome, myelofibrosis.
↓: acute and chronic granulocytic leukemia, thrombocytopenic purpura, PNH, hypophosphatemia, collagen disorders.
LH
Lipase
Nl range: 0-160 U/L.
↑: acute pancreatitis, perforated peptic ulcer, carcinoma of pancreas (early stage), pancreatic duct obstruction, bowel infarction, intestinal obstruction.
Lipoprotein(A)
Nl: 1.35-19.6 mg/dL (male); 1.24-20.1 mg/dL (female).
↑: CAD, uncontrolled diabetes, hypothyroidism, chronic renal failure, pregnancy, tobacco use, infections, nephritic syndrome.
↓: niacin, omega-3 fatty acids, estrogens, tamoxifen.
Lipoprotein Cholesterol, High Density
Lipoprotein Cholesterol, Low Density
Liver-Kidney Microsome Type 1 Antibodies (LKM1)
Nl: <20 U.
↑: autoimmune hepatitis type 2.
Low-Density Lipoprotein (LDL) Cholesterol
Nl range: <130 mg/dL (<70 mg/dL in diabetics and pts w/CV risk factors).
↑: diet high in saturated fat, familial hyperlipidemia, sedentary lifestyle, poorly controlled DM, nephritic syndrome, hypothyroidism.
↓: use of lipid-lowering agents (statins, niacin, ezetimibe, cholestyramine, colesevelam), starvation, malabsorption, abetalipoproteinemia, hyperthyroidism, hepatic failure, carcinoma, infection, inflammation.
Lupus Anticoagulant (LA) Test
Nl: (−)
Present in: antiphospholipid Ab syndrome. False-(+) results may occur w/oral anticoagulant Rx, factor deficiency, specific factor inhibitors.
Luteinizing Hormone (LH) (Blood)
Nl range:
• Female, adult: 1.0-18.0 IU/L (follicular phase); 20.0-80.0 IU/L (midcycle phase); 0.5-18.0 IU/L (luteal phase); postmenopausal: 12.0-55.0 IU/L
• Male, adult: 1.0-9.0 IU/L
↑: gonadal failure, anorchia, menopause, testicular feminization syndrome.
↓: primary pituitary or hypothalamic failure.
Lymphocytes
Nl range: 15%-40%.
• Total lymphocyte count: 800-2600/mm3
• Total T lymphocytes: 800-2200/mm3
• CD4 lymphocytes: ≥400/mm3
• CD8 lymphocytes: 200-800/mm3
• Nl CD4/CD8 ratio is 2.0.
↑: chronic infections, infectious mononucleosis and other viral infections, CLL, Hodgkin’s disease, UC, hypoadrenalism, ITP.
↓: HIV infection, bone marrow suppression from chemotherapeutic agents or chemoRx, aplastic anemia, neoplasms, steroids, adrenocortical hyperfunction, neurologic disorders (MS, myasthenia gravis, GBS).
CD4 lymphocytes are calculated as total WBCs × % lymphocytes × % lymphocytes stained w/CD4. They are ↓ in AIDS and other forms of immune dysfunction.
Magnesium (Serum)
Nl range: 1.8-3.0 mg/dL.
Abnl results: Refer to “Hypomagnesemia” and “Hypermagnesemia” in Chapter 9.
Mean Corpuscular Volume (MCV)
Nl range: 76-100 μm3.
↑: EtOH abuse, reticulocytosis, vitamin B12 deficiency, folic acid deficiency, liver disease, hypothyroidism, marrow aplasia, myelofibrosis.
↓: iron deficiency, anemia of chronic disease, thalassemia trait or syndrome, other hemoglobinopathies, sideroblastic anemia, chronic renal failure, lead poisoning.
Methylmalonic Acid (Serum)
Nl: <0.2 μmol/L.
↑: vitamin B12 deficiency, pregnancy, methylmalonic acidemia.
Mitochondrial Antibody (AMA Antimitochondrial Antibody)
Nl: (−)
Present in: PBC (>90% of pts).
Monocyte Count
Nl range: 2%-8%.
↑: viral diseases, parasites, infections, neoplasms, IBD, monocytic leukemia, lymphomas, myeloma, sarcoidosis.
↓: viral syndrome, glucocorticoid administration, aplastic anemia, lymphocytic leukemia.
Natriuretic Peptide
Neutrophil Count
Nl range: 50%-70%.
Subsets:
• Bands (early mature neutrophils): 2%-6%
• Segs (mature neutrophils): 60%-70%
↓: viral infections, aplastic anemias, immunosuppressive drugs, radiation Rx to bone marrow, agranulocytosis, drugs (abx, antithyroidals), lymphocytic and monocytic leukemias.
Norepinephrine
Nl range: 0-600 pg/mL.
↑: pheochromocytomas, neuroblastomas, stress, vigorous exercise, certain foods (bananas, chocolate, coffee, tea, vanilla).
5′-Nucleotidase
Nl range: 2-16 IU/L.
↑: biliary obstruction, metastatic neoplasms to liver, PBC, renal failure, pancreatic carcinoma, chronic active hepatitis.
Osmolality, Serum
Nl range: 280-300 mOsm/kg. It can also be estimated by the following formula: 2([Na] + [K]) + Glucose/18 + BUN/2.8.
↑: dehydration, hypernatremia, diabetes insipidus, uremia, hyperglycemia, mannitol Rx, ingestion of toxins (ethylene glycol, methanol, ethanol), hypercalcemia, diuretics.
↓: SIADH, hyponatremia, overhydration, Addison’s disease, hypothyroidism.
Osmotic Fragility Test
Nl: Hemolysis begins at 0.50, w/v [5.0 g/L] and is complete at 0.30, w/v [3.0 g/L] NaCl.
↑: hereditary spherocytosis, hereditary stomatocytosis, spherocytosis associated w/acquired immune hemolytic anemia.
↓: iron deficiency anemia, thalassemias, liver disease, leptocytosis associated w/asplenia.
Parathyroid Hormone
Nl: 10-65 pg/mL (serum, intact molecule); 1.0-5.0 pmol/L (plasma).
↑: hyperparathyroidism (primary or secondary), pseudohypoparathyroidism, anticonvulsants, corticosteroids, lithium, INH, rifampin, phosphates, Zollinger-Ellison syndrome, hereditary vit D def.
↓: hypoparathyroidism, sarcoidosis, cimetidine, β-blockers, hyperthyroidism, hypomagnesemia.
Parietal Cell Antibodies
Nl: (−)
Present in: pernicious anemia (>90%), atrophic gastritis (up to 50%), thyroiditis (30%), Addison’s disease, myasthenia gravis, Sjögren’s syndrome, type 1 DM.
Partial Thromboplastin Time (PTT), Activated Partial Thromboplastin Time (APTT)
Nl range: 25-41 seconds.
↑: heparin Rx, coagulation factor deficiency (I, II, V, VIII, IX, X, XI, XII), liver disease, vitamin K deficiency, DIC, circulating anticoagulant, warfarin Rx, specific factor inhibition (PCN reaction, RA), thrombolytic Rx, nephrotic syndrome.
Note: Useful to evaluate the intrinsic coagulation system.
pH, Blood
Nl values: 7.35-7.45 (arterial); 7.32-7.42 (venous).
PO4-3 (Serum)
Nl range: 2.5-5 mg/dL.
↑: refer to “Hyperphosphatemia” and “Hypophosphatemia” in Chapter 9.
Plasminogen
Nl: immunoassay (antigen), <20 mg/dL.
↑: infection, trauma, neoplasm, MI (acute-phase reactant), pregnancy, bilirubinemia.
↓: DIC, severe liver disease, thrombolytic Rx w/streptokinase or urokinase, alteplase.
Platelet Aggregation
Nl: full aggregation (generally >60%) in response to epinephrine, thrombin, ristocetin, ADP, collagen.
↑: heparin, hemolysis, lipemia, nicotine; hereditary and acquired disorders of Plt adhesion, activation, and aggregation.
↓: ASA, some PCNs, chloroquine, chlorpromazine, clofibrate, captopril, Glanzmann’s thrombasthenia, Bernard-Soulier syndrome, Wiskott-Aldrich syndrome, cyclooxygenase deficiency. In vWD, there is nl aggregation w/ADP, collagen, and epinephrine but abnl agglutination w/ristocetin.
Platelet Antibodies
Nl: absent.
Present in: ITP (>90% of pts w/chronic ITP). Pts w/nonimmune thrombocytopenias may have false-(+) results.
Platelet Count
Nl range: 130-400 × 103/mm3.
↑: iron deficiency, after hemorrhage, neoplasms (GI tract), CML, PV, myelofibrosis w/myeloid metaplasia, infections, after splenectomy, post partum, hemophilia, pancreatitis, cirrhosis.
Platelet Function Analysis (PFA-100 Assay)
Nl: Test is a two-component assay in which blood is aspirated through two capillary tubes, one of which is coated w/collagen and ADP (COL/ADP) and the other w/collagen and epinephrine (COL/EPI). The test measures the ability of Plts to occlude an aperture in a biologically active membrane treated with COL/ADP and COL/EPI. During the test, the Plts adhere to the surface of the tube and cause blood flow to cease. The closing time refers to the cessation of blood flow and is reported in conjunction w/the Hct and Plt count. Hct count must be >25% and Plt count >50 K/μL for the test to be performed.
• COL/ADP: 70-120 seconds
• COL/EPI: 75-120 seconds
↑: acquired Plt dysfunction, vWD, anemia, thrombocytopenia, use of ASA and NSAIDs.
Potassium (K+) (Serum)
Nl range: 3.5-5 mEq/L.
Progesterone (Serum)
Nl:
• Female: 15-70 ng/dL (follicular phase); 200-2500 ng/dL (luteal phase)
• Male: 15-70 ng/dL
↑: congenital adrenal hyperplasia, clomiphene, corticosterone, 11-deoxycortisol, dihydroprogesterone, molar pregnancy, lipoid ovarian tumor.
↓: primary or secondary hypogonadism, oral contraceptives, ampicillin, threatened abortion.
Prolactin
Nl range: <20 ng/mL.
↑: prolactinomas (level >200 highly suggestive), drugs (phenothiazines, cimetidine, tricyclic antidepressants, metoclopramide, estrogens, antihypertensives [methyldopa, verapamil], haloperidol), post partum, stress, hypoglycemia, hypothyroidism.
Prostate-Specific Antigen (PSA)
Nl range: 0-4 ng/mL. There is no PSA level below which prostate cancer can be ruled out and no level above which prostate cancer is certain. The individual’s PSA level is only part of the equation. Other risk factors need to be considered, such as age, race, FHx, findings on digital rectal examination, percentage free PSA ratio, and PSA velocity (rate of change from prior PSA measurement).
↑: BPH, carcinoma of prostate, after rectal examination, prostate trauma, androgens, prostatitis, urethral instrumentation.
Note: Measurement of free PSA is useful to assess the probability of prostate cancer in pts w/nl findings on digital rectal examination and total PSA level between 4 and 10 ng/mL. In these pts, the global risk of prostate cancer is 25% to 40%. However, if the free PSA is >25%, the risk of prostate cancer ↓ to 8%; whereas if the free PSA is <10%, the risk of cancer ↑ to 56%. Free PSA is also useful to evaluate the aggressiveness of prostate cancer. A low free PSA percentage generally indicates a high-grade cancer, whereas a high free PSA percentage is generally associated w/a slower growing tumor.
Prostatic Acid Phosphatase
Nl: 0-0.8 U/L.
↑: prostate cancer (especially in metastatic prostate cancer), BPH, prostatitis, after prostate surgery or manipulation, hemolysis, androgens, clofibrate.
↓: ketoconazole Rx.
Protein (Serum)
Nl range: 6-8 g/dL.
↑: dehydration, sarcoidosis, collagen-vascular diseases, MM, Waldenström’s macroglobulinemia.
↓: malnutrition, cirrhosis, nephrosis, low-protein diet, overhydration, malabsorption, pregnancy, severe burns, neoplasms, chronic diseases.
Protein C Assay
Nl: 70%-140%.
↑: oral contraceptives, stanozolol.
↓: congenital protein C deficiency, warfarin Rx, vitamin K deficiency, renal insufficiency, consumptive coagulopathies.
Protein Electrophoresis (Serum)
Nl range:
• Alb: 60%-75%; 3.6-5.2 g/dL
• α1: 1.7%-5%; 0.1-0.4 g/dL
• α2: 6.7%-12.5%; 0.4-1.0 g/dL
• β: 8.3%-16.3%; 0.5-1.2 g/dL
• Gamma: 10.7%-20%; 0.6-1.6 g/dL
↑:
• Alb: dehydration
• α1: neoplastic diseases, inflammation
• α2: neoplasms, inflammation, infection, nephrotic syndrome
• β: hypothyroidism, biliary cirrhosis, DM
• Gamma: see “Immunoglobulins,” earlier
↓:
• Alb: malnutrition, chronic liver disease, malabsorption, nephrotic syndrome, burns, SLE
• α1: emphysema (α1-antitrypsin deficiency), nephrosis
• α2: hemolytic anemias (↓ haptoglobin), severe hepatocellular damage
• β: hypocholesterolemia, nephrosis
• Gamma: see “Immunoglobulins,” earlier
Protein S Assay
Nl: 65%-140%.
↑: presence of lupus anticoagulant.
↓: hereditary deficiency, acute thrombotic events, DIC, surgery, oral contraceptives, pregnancy, hormone replacement Rx, L-asparaginase Rx.
Prothrombin Time (PT)
Nl range: 11-13.2 seconds.
Note: The PT is reported as absolute clotting time in seconds and also as a derivative number called the INR. This ratio is derived from the actual PT of the pt divided by the mean PT of a group of healthy subjects. INR should always be used in interpreting PT.
↑: liver disease, oral anticoagulants (warfarin), heparin, factor deficiency (I, II, V, VII, X), DIC, vitamin K deficiency, afibrinogenemia, dysfibrinogenemia, drugs (salicylate, chloral hydrate, diphenylhydantoin, estrogens, antacids, phenylbutazone, quinidine, abx, allopurinol, anabolic steroids).
↓: vitamin K supplementation, thrombophlebitis, drugs (glutethimide, estrogens, griseofulvin, diphenhydramine).
Protoporphyrin (Free Erythrocyte)
Nl range: 16-36 μg/dL of RBCs.
↑: iron deficiency, lead poisoning, sideroblastic anemias, anemia of chronic disease, hemolytic anemias, erythropoietic protoporphyria.
PSA
PT
Red Blood Cell Count
Nl range: 4.3-5.9 × 106/mm3 (male); 3.5-5.0 × 106/mm3 (female).
↑: hemoconcentration and dehydration, stress, PV, smokers, high altitude, CV disease, renal cell carcinoma and other erythropoietin-producing neoplasms.
↓: anemias, hemolysis, chronic renal failure, hemorrhage, failure of marrow production.
Red Blood Cell Distribution Width (RDW)
RDW measures variability of red cell size (anisocytosis)
Nl range: 11.5-14.5.
Nl RDW and:
• ↑ MCV: aplastic anemia, preleukemia.
• Nl MCV: nl, anemia of chronic disease, acute blood loss or hemolysis, CLL, CML, nonanemic enzymopathy or hemoglobinopathy.
• ↓ MCV: anemia of chronic disease, heterozygous thalassemia.
↑ RDW and:
• ↑ MCV: vitamin B12 deficiency, folate deficiency, immune hemolytic anemia, cold agglutinins, CLL w/high count, liver disease.
• Nl MCV: early iron deficiency, early vitamin B12 deficiency, early folate deficiency, anemic globinopathy.
• ↓ MCV: iron deficiency, RBC fragmentation, HbH disease, thalassemia intermedia.
Red Blood Cell Folate
See Folate
Red Blood Cell Mass (Volume)
Nl range:
• Male: 20-36 mL/kg of BW (1.15-1.21 L/m2 BSA)
• Female: 19-31 mL/kg of BW (0.95-1.00 L/m2 BSA)
↑: P vera, hypoxia (smokers, high altitude, CV disease), hemoglobinopathies w/↑O2 affinity, erythropoietin-producing tumors (renal cell carcinoma).
↓: hemorrhage, chronic disease, failure of marrow production, anemias, hemolysis.
Renin (Serum)
↑: renal HTN, reduced plasma volume, secondary aldosteronism, drugs (thiazides, estrogen, minoxidil), chronic renal failure, Bartter’s syndrome, pregnancy (nl), pheochromocytoma.
↓: primary aldosteronism, adrenocortical HTN, ↑ in plasma volume, drugs (propranolol, reserpine, clonidine).
Reticulocyte Count
Nl range: 0.5%-1.5%.
↑: hemolytic anemia (sickle cell crisis, thalassemia major, autoimmune hemolysis), hemorrhage, after anemia Rx (folic acid, ferrous sulfate, vitamin B12), chronic renal failure.
↓: aplastic anemia, marrow suppression (sepsis, chemotherapeutic agents, radiation), hepatic cirrhosis, blood transfusion, anemias of disordered maturation (iron deficiency anemia, megaloblastic anemia, sideroblastic anemia, anemia of chronic disease).
Rheumatoid Factor (RF)
Nl: (−)
Present in titer >1:20: RA, SLE, chronic inflammatory processes, old age, infections, liver disease, MM, sarcoidosis, pulmonary fibrosis, Sjögren’s syndrome.
RNP
Sedimentation Rate
Semen Analysis
Nl:
• Volume: 2-6 mL
• Sperm density: >20 million/mL
• Total number of spermatozoa: >80 million/ejaculate
• Progressive motility score evaluated 2-4 hr after ejaculate: 3-4
• Live spermatozoa: ≥50% of total
• Nl spermatozoa: ≥60% of total
• Immature forms: <4%
↓: cryptorchidism, testicular failure, obstruction of ejaculatory system, after vasectomy, medications (cimetidine, ketoconazole, nitrofurantoin, cancer chemoRx agents, sulfasalazine), testicular radiation.
SGPT
Sickle Cell Test
Nl: (−)
(+) in: sickle cell anemia, sickle cell trait; combination of Hgb S gene w/other disorders, such as thalassemias.
Smooth Muscle Antibody
Nl: (−)
Present in: chronic active hepatitis (≥1:80), PBC (≥1:80), infectious mononucleosis.
Na+ (Serum)
Sudan III Stain (Qualitative Screening For Fecal Fat)
Nl: (−) The test should be preceded by a diet containing 100 to 150 g of dietary fat/day for 1 week, avoidance of high-fiber diet, and avoidance of suppositories or oily material before specimen collection.
(+) in: steatorrhea, use of castor oil or mineral oil droplets.
T3 (Triiodothyronine)
Nl range: 75-220 ng/dL.
T3 Resin Uptake (T3RU)
Nl range: 25%-35%.
Abnl values: in hyperthyroidism. T3 resin uptake (T3RU or RT3U) measures the percentage of free T4 (not bound to protein); it does not measure serum T3 concentration. T3RU and other tests that reflect thyroid hormone binding to plasma protein are also known as THBR.
T4, Serum T4, And Free T4 (Free Thyroxine)
Nl range: 0.8-2.8 ng/dL.
Abnl values: see “Hyperthyroidism” in Chapter 5. Serum thyroxine test measures both circulating thyroxine bound to protein (represents >99% of circulating T4 and unbound [free] thyroxine). Values vary w/protein binding; changes in the concentration of T4 secondary to changes in TBG can be caused by the following:
• ↑ TBG ( ↑T4): pregnancy, estrogens, acute infectious hepatitis, oral contraceptives, familial, fluorouracil, clofibrate, heroin, methadone.
• ↓ TBG (↓ T4): androgens, glucocorticoids, nephrotic syndrome, cirrhosis, acromegaly, hypoproteinemia, familial, phenytoin, ASA and other NSAIDs, high-dose PCN, asparaginase, chronic debilitating illness.
To eliminate the suspected influence of protein binding on thyroxine values, two additional tests are available: T3 resin uptake and serum free thyroxine.
Serum free T4 directly measures unbound thyroxine. Free T4 can be measured by equilibrium dialysis (gold standard of free T4 assays) or by immunometric techniques (influenced by serum levels of lipids, proteins, and certain drugs).
The FTI can also be easily calculated by multiplying T4 times T3RU and dividing the result by 100; the FTI corrects for any abnl T4 values secondary to protein binding: FTI = T4 × T3RU/100. Nl values equal 1.1 to 4.3.
Testosterone
Nl range: variable with age and sex.
• Serum/plasma: 170-1000 ng/dL (males); 15-70 ng/dL (females)
• Urine: 50-135 μg/day (males); 2-12 μg/day (females)
↑: adrenogenital syndrome, polycystic ovary disease.
Thiamine
Nl: 275-675 ng/g.
↑: PV, leukemia, Hodgkin’s disease.
↓: alcoholism, dietary deficiency (beriberi), excessive consumption of tea (contains antithiamine factor) or raw fish (contains a microbial thiaminase), chronic illness, prolonged illness, barbiturates.
Thrombin Time (TT)
Nl range: 11.3-18.5 seconds.
↑: thrombolytic and heparin Rx, DIC, hypofibrinogenemia, dysfibrinogenemia.
Thyroglobulin
Nl: 3-40 ng/mL. Thyroglobulin is a tumor marker for monitoring the status of pts w/papillary or follicular thyroid cancer after resection.
↑: papillary or follicular thyroid cancer, Hashimoto’s thyroiditis, Graves’ disease, subacute thyroiditis.
Thyroid Microsomal Antibodies
Nl: undetectable. Low titers may be present in 5% to 10% of nl individuals.
↑: Hashimoto’s disease, thyroid carcinoma, early hypothyroidism, pernicious anemia.
Thyroid-Stimulating Hormone (TSH)
Nl: 2-6 U/mL.
Thyrotropin (TSH) Receptor Antibodies
Nl: <130 % of basal activity.
↑: values between 1.3 and 2.0 are found in 10% of pts w/thyroid disease other than Graves’ disease. Values >2.8 have been found only in pts w/Graves’ disease.
TIBC
Tissue Transglutaminase Antibody
Nl: (−)
Present in: celiac disease (specificity, 94%-97%; sensitivity, 90%-98%), dermatitis herpetiformis.
Transferrin
Nl range: 170-370 mg/dL.
↑: iron deficiency anemia, oral contraceptive administration, viral hepatitis, late pregnancy.
↓: nephrotic syndrome, liver disease, hereditary deficiency, protein malnutrition, neoplasms, chronic inflammatory states, chronic illness, thalassemia, hemochromatosis, hemolytic anemia.
Triglycerides
Nl range: <150 mg/dL.
↑: hyperlipoproteinemias (types I, IIb, III, IV, V), diet high in saturated fats, hypothyroidism, pregnancy, estrogens, pancreatitis, EtOH intake, nephrotic syndrome, poorly controlled DM, sedentary lifestyle, glycogen storage disease.
↓: malnutrition, vigorous exercise, congenital abetalipoproteinemias, drugs (e.g., gemfibrozil, fenofibrate, nicotinic acid, metformin, clofibrate).
Triiodothyronine
Troponins (Serum)
Nl range: 0-0.4 ng/mL ([−]). If there is clinical suspicion of evolving acute MI or ischemic episode, repeated testing in 5 to 6 hr is recommended.
Indeterminate: 0.05-0.49 ng/mL. Suggest further tests. In a pt w/unstable angina and this troponin I level, there is an ↑ in risk of a cardiac event in the near future.
High probability of acute MI: ≥0.50 ng/mL.
• cTnT is a highly sensitive marker for myocardial injury for the first 48 hr after MI and for up to 5 to 7 days. It may also be ↑ in renal failure, chronic muscle disease, and trauma.
• cTnI is highly sensitive and specific for myocardial injury (≥CK-MB) in the initial 8 hr, peaks within 24 hr, and lasts up to 7 days. With progressively higher levels of cTnI, the risk of mortality ↑ because the amount of necrosis ↑.
↑: in addition to ACS, many diseases such as sepsis, hypovolemia, AF, CHF, PE, myocarditis, myocardial contusion, and renal failure can be associated w/ an ↑ in troponin level.
TT
See Thrombin Time
Unconjugated Bilirubin
Urea Nitrogen
Nl range: 8-18 mg/dL.
↑: dehydration, renal disease (GN, pyelonephritis, diabetic nephropathy), urinary tract obstruction (prostatic hypertrophy), drugs (AGs and other abx, diuretics, lithium, corticosteroids), GI bleeding, ↓ renal blood flow (shock, CHF, MI).
↓: liver disease, malnutrition, third trimester of pregnancy.
Uric Acid (Serum)
Nl range: 2-7 mg/dL.
↑: hereditary enzyme deficiency (hypoxanthine-guanine phosphoribosyltransferase), renal failure, gout, excessive cell lysis (chemotherapeutic agents, radiation Rx, leukemia, lymphoma, hemolytic anemia), acidosis, myeloproliferative disorders, diet high in purines or protein, drugs (diuretics, low doses of ASA, ethambutol, nicotinic acid), lead poisoning, hypothyroidism.
↓: drugs (allopurinol, febuxostat, high doses of ASA, probenecid, warfarin, corticosteroid), deficiency of xanthine oxidase, SIADH, renal tubular deficits (Fanconi’s syndrome), alcoholism, liver disease, diet deficient in protein or purines, Wilson’s disease, hemochromatosis.
Urinalysis
Nl range:
• Color: light straw
• Appearance: clear
• pH: 4.5-8.0 (average, 6.0)
• Specific gravity: 1.005-1.030
• Protein: absent
• Ketones: absent
• Glucose: absent
• Occult blood: absent
Microscopic examination:
• RBC: 0-5 (high-power field)
• WBC: 0-5 (high-power field)
• Bacteria (spun specimen): absent
• Casts: 0-4 hyaline (low-power field)
Urine Amylase
Nl range: 35-260 U Somogyi/hr.
↑: pancreatitis, carcinoma of the pancreas.
Urine Bile
Nl: absent.
Abn:
• Urine bilirubin: hepatitis (viral, toxic, drug induced), biliary obstruction.
• Urine urobilinogen: hepatitis (viral, toxic, drug induced), hemolytic jaundice, liver cell dysfunction (cirrhosis, infection, mets).
Urine Calcium
Nl: 6.2 mmol/dL (CF, 0.02495; SMI, 0.1 mmol/dL).
↑: primary hyperparathyroidism, hypervitaminosis D, bone mets, MM, ↑ in Ca intake, steroids, prolonged immobilization, sarcoidosis, Paget’s disease, idiopathic hypercalciuria, renal tubular acidosis.
↓: hypoparathyroidism, pseudohypoparathyroidism, vitamin D deficiency, vitamin D–resistant rickets, diet low in Ca, drugs (thiazide diuretics, oral contraceptives), familial hypocalciuric hypercalcemia, renal osteodystrophy, K+ citrate Rx.
Urine cAMP
↑: hypercalciuria, familial hypocalciuric hypercalcemia, primary hyperparathyroidism, pseudohypoparathyroidism, rickets.
Urine Catecholamines
Nl range: <100 μg/24 hr (norepinephrine); <10 μg/24 hr (epinephrine).
↑: pheochromocytoma, neuroblastoma, severe stress.
Urine Chloride
Nl range: 110-250 mEq/day.
↑: corticosteroids, Bartter’s syndrome, diuretics, metabolic acidosis, severe hypokalemia.
↓: chloride depletion (vomiting), colonic villous adenoma, chronic renal failure, renal tubular acidosis.
Urine Creatinine (24-Hour)
Nl range: 0.8-1.8 g/day (male); 0.6-1.6 g/day (female).
Note: Useful test as an indicator of completeness of 24-hour urine collection.
Urine Crystals
Uric acid: acid urine, hyperuricosuria, uric acid nephropathy.
Sulfur: abx containing sulfa.
Calcium oxalate: ethylene glycol poisoning, acid urine, hyperoxaluria.
Calcium PO4-3: alkaline urine.
Cystine: cystinuria.
Urine Eosinophils
Nl: absent.
Present in: interstitial nephritis, ATN, UTI, kidney transplant rejection, HRS.
Urine Glucose (Qualitative)
Nl: absent.
Present in: DM, renal glycosuria (↓ renal threshold for glucose), glucose intolerance.
Urine Hemoglobin, Free
Nl: absent.
Present in: hemolysis (w/saturation of serum haptoglobin binding capacity and renal threshold for tubular absorption of Hgb).
Urine Hemosiderin
Nl: absent.
Present in: PNH, chronic hemolytic anemia, hemochromatosis, blood transfusion, thalassemias.
Urine 5-Hydroxyindoleacetic Acid (Urine 5-HIAA)
Nl range: 2-8 mg/24 hr.
↑: carcinoid tumors, after ingestion of certain foods (bananas, plums, tomatoes, avocados, pineapples, eggplant, walnuts), drugs (MAOIs, phenacetin, methyldopa, glycerol guaiacolate, acetaminophen, salicylates, phenothiazines, imipramine, methocarbamol, reserpine, methamphetamine).
Urine Indican
Nl: absent.
Present in: malabsorption resulting from intestinal bacterial overgrowth.
Urine Ketones (Semiquantitative)
Nl: absent.
Present in: DKA, alcoholic ketoacidosis, starvation, isopropanol ingestion.
Urine Metanephrines
Nl range: 0-2.0 mg/24 hr.
↑: pheochromocytoma, neuroblastoma, drugs (caffeine, phenothiazines, MAOIs), stress.
Urine Myoglobin
Nl: absent.
Present in: severe trauma, hyperthermia, polymyositis or dermatomyositis, CO poisoning, drugs (narcotic and amphetamine toxicity), hypothyroidism, muscle ischemia.
Urine Nitrite
Urine Occult Blood
Nl: (−)
(+) in: trauma to urinary tract, renal disease (GN, pyelonephritis), renal or ureteral calculi, bladder lesions (carcinoma, cystitis), prostatitis, prostatic carcinoma, menstrual contamination, hematopoietic disorders (hemophilia, thrombocytopenia), anticoagulants, ASA.
Note: Hematuria w/o erythrocyte casts or significant albuminuria suggests the possibility of renal or bladder cancers.
Urine Osmolality
Nl range: 50-1200 mOsm/kg.
↑: SIADH, dehydration, glycosuria, adrenal insufficiency, high-protein diet.
↓: diabetes insipidus, excessive water intake, IV hydration w/D5W, acute renal insufficiency, GN.
Urine pH
Nl range: 4.6-8.0 (average 6.0).
↑: bacteriuria, vegetarian diet, renal failure w/inability to form ammonia, drugs (abx, NaHCO3, acetazolamide).
↓: acidosis (metabolic, respiratory), drugs (ammonium chloride, methenamine mandelate), DM, starvation, diarrhea.
Urine PO4-3
Nl range: 0.8-2.0 g/24 hr.
↑: ATN (diuretic phase), chronic renal disease, uncontrolled DM, hyperparathyroidism, hypomagnesemia, metabolic acidosis, metabolic alkalosis, neurofibromatosis, adult-onset vitamin D–resistant hypophosphatemic osteomalacia.
↓: acromegaly, ARF, ↓ dietary intake, hypoparathyroidism, respiratory acidosis.
Urine K+
Nl range: 25-100 mEq/24 hr.
↑: aldosteronism (primary, secondary), glucocorticoids, alkalosis, renal tubular acidosis, excessive dietary K+ intake.
↓: ARF, K+-sparing diuretics, diarrhea, hypokalemia.
Urine Protein (Quantitative)
Nl range: <150 mg/24 hr.
↑: renal disease (glomerular, tubular, interstitial), CHF, HTN, neoplasms of renal pelvis and bladder, MM, Waldenström’s macroglobulinemia.
Urine Na+ (Quantitative)
Nl range: 40-220 mEq/day.
↑: diuretic administration, high Na+ intake, salt-losing nephritis, ATN, vomiting, Addison’s disease, SIADH, hypothyroidism, CHF, hepatic failure, chronic renal failure, Bartter’s syndrome, glucocorticoid deficiency, interstitial nephritis (caused by analgesic abuse, mannitol, dextran, or glycerol Rx), milk-alkali syndrome, ↓ renin secretion, postobstructive diuresis.
↓: ↑ in aldosterone, glucocorticoid excess, hyponatremia, prerenal azotemia, ↓ salt intake.
Urine Specific Gravity
Nl range: 1.005-1.03.
↑: dehydration, excessive fluid losses (vomiting, diarrhea, fever), x-ray contrast media, DM, CHF, SIADH, adrenal insufficiency, ↓ fluid intake.
↓: diabetes insipidus, renal disease (GN, pyelonephritis), excessive fluid intake or IV hydration.
Urine Vanillylmandelic Acid (VMA)
Nl range: <6.8 mg/24 hr.
↑: pheochromocytoma, neuroblastoma, ganglioblastoma, drugs (isoproterenol, methocarbamol, levodopa, sulfonamides, chlorpromazine), severe stress; after ingestion of bananas, chocolate, vanilla, tea, coffee.
↓: drugs (MAOIs, reserpine, guanethidine, methyldopa).
Vasoactive Intestinal Peptide (VIP)
Nl: <50 pg/mL.
Venereal Disease Research Laboratories (VDRL)
Nl range: (−)
(+) test: syphilis, other treponemal diseases (yaws, pinta, bejel).
Note: A false-(+) test result may be seen in pts w/SLE and other autoimmune diseases, infectious mononucleosis, HIV infection, atypical pneumonia, malaria, leprosy, typhus fever, rat-bite fever, and relapsing fever.
Viscosity (Serum)
Nl range: 1.4-1.8 relative to water (1.10-1.22 centipoise).
↑: monoclonal gammopathies (Waldenström’s macroglobulinemia, MM), hyperfibrinogenemia, SLE, RA, polycythemia, leukemia.
Vitamin B12
Nl range: 190-900 ng/mL.
↓: pernicious anemia, dietary (strict lacto-ovovegetarians, food faddists), malabsorption (achlorhydria, gastrectomy, ileal resection, Crohn’s disease of terminal ileum, pancreatic insufficiency, drugs [omeprazole and other PPIs, metformin, cholestyramine]), chronic alcoholism, H. pylori infection.
Vitamin D, 1,25-Dihydroxycholecalciferol
Nl: 32-65 pg/mL.
↑: tumor calcinosis, primary hyperparathyroidism, sarcoidosis, tuberculosis, idiopathic hypercalciuria.
↓: postmenopausal osteoporosis, chronic renal failure, hypoparathyroidism, tumor-induced osteomalacia, rickets, ↑ blood lead levels.
Vitamin K
Nl: 0.10-2.20 ng/mL.
↓: PBC, anticoagulants, abx, cholestyramine, GI disease, pancreatic disease, cystic fibrosis, obstructive jaundice, hypoprothrombinemia, hemorrhagic disease of the newborn.
