38 Surviving Financially
One important way to survive financially is to be paid appropriately for the procedures performed in the office. Coding and billing for skin procedures can be very complex. It is essential for the practitioner to understand the idiosyncrasies of the ICD-9 and CPT codes if billing is to be completed correctly.1–7 The objective is not to charge as much as possible, but rather, to optimize billing once the proper procedure has been performed. Oftentimes, the same procedure can be billed using three or four different codes. Without exception, one method will pay more. Knowing the proper application of billing rules can, and does, make a significant difference in the financial bottom line of the practice.
Unless a clinician is going to enter into the aesthetic field, the instruments used to perform dermatologic procedures are inexpensive. The most costly would be an electrosurgical unit and a liquid nitrogen gun (see Chapters 14 and 15). On the other hand, aesthetic equipment such as lasers can be very expensive, exceeding $150,000. However, when properly utilized on a frequent basis, lasers will offer the greatest revenue returns compared to other aesthetic procedures that require consumable products, such as botulinum toxin and dermal fillers. Cost versus fee charged for aesthetic laser treatments is more difficult to analyze due to the multiple variables involved such as methodology of acquiring the capital equipment, incidental disposable goods, cost of office space for storing the device, and maintenance contracts ($10,000 per year is common for aesthetic lasers).
A properly designed spreadsheet can be used to estimate whether major investments will provide an adequate financial return. Sales representatives will often paint a rosy picture and provide flow sheets which always conclude that there will be a significant return on investment. Major investments, however, require a careful independent study analysis of main factors.8
The purpose of this chapter is to help the reader become familiar with proper CPT coding for biopsies, destructions, and excisions of skin lesions. It will also help identify the pitfalls and common errors in coding and discuss financial considerations for aesthetic procedures. Tables 38-1 and 38-2 list common coding terminology and modifiers.
| Ablation | See “Destruction” |
| Balance billing | The process of charging a patient the difference between what the physician bills and what the insurance company pays. If a provider participates with an insurance carrier, only copays and deductibles may be charged to the patient. If there is no participation agreement, then the provider may bill the patient for any fees not paid by the insurance company. |
| Biopsy | The procedure used to obtain tissue for histologic examination. This can be done with shave, punch, excision, curettement, and incisional procedures. |
| Electrosurgery/fulgurate/desiccate/cauterize | The use of electrical current heat to treat/destroy an area. |
| CPT | Current Procedural Terminology, published and updated annually by the AMA. Every medical procedure has a CPT code number. The majority of billing is completed using CPT terminology.2 |
| Cryosurgery | The use of low temperatures to destroy (by freezing) a lesion (liquid nitrogen; nitrous oxide closed system; chemical spray canisters). |
| Debridement | Removal of devitalized tissue, dirt, and/or eschar from wounds or infected areas. |
| Destruction | Treatment of a lesion using cryosurgery, chemical application, injection of a chemical, curettement, or electrosurgery. Using a shave technique would also qualify, but in general, reimbursement would be higher using a shave or biopsy code than a destruction code for benign lesions. |
| Explanation of benefits (EOB) | A sheet provided by insurance companies that is enclosed with the payments for various procedures explaining what is allowed, what is the patient’s responsibility (copay, deductible, not covered), what is not allowed (must be “written off” by the provider), and the amount of the enclosed payment. |
| Excision | Removal of a lesion using sharp dissection or electrosurgical cutting. In a shave excision, a slicing technique is used to remove either all or a portion of the lesion. It does not require suturing. Elliptical or fusiform excision includes full-thickness (through the dermis) removal of the lesion and requires closure, usually with sutures (or glue or adhesive strips). |
| Global period | Certain procedures have global periods. During this time, additional services (relating to the original procedure) cannot be charged. For most skin surgical procedures, this period is 10 days (no global period for shaves and punches). |
| ICD-9 (International Classification of Diseases, 9th Revision) | Every diagnosis has a specific numbered code. A diagnostic code is required to justify the reason for a CPT (procedure) code.1 The ICD-10 codes are currently scheduled to be implemented October 1, 2013. |
| Incision and drainage (I&D) | Simple: Contents expressed after incision. |
| Complex: Multiple conditions would qualify for a complex I&D, including the removal of a sac, such as in a sebaceous cyst, or insertion of a drain, such as iodoform gauze. The size and depth of the abscess could also be a factor, as well as excessive time required to complete the procedure. If multiple I&Ds of different lesions are done at the same time, it would also be considered “complex.” | |
| J-codes | Nearly every injectable medication has a specific number assigned to it called the J-code. When administered, the physician charges for not only the administration itself (a CPT code), but also for the particular chemical delivered (identified by the J-code). |
| Modifiers | These are numbers appended to a CPT code while billing to indicate that more than just the usual services were provided for the particular CPT code. (See Table 38-2 for common modifiers). |
| Paring | Removal and/or decrease in the bulk of a lesion, by peeling or shaving it away using a scalpel or a sharp instrument. |
| -25 | Significantly separate E&M on the same day as a procedure. |
| Example: If a patient comes in for a mole removal and you have documentation that you also treated the patient for hypertension, osteoporosis, smoking, etc., use the -25 modifier with the office visit code. | |
| -50 | Bilateral procedures. |
| Example: If you perform sclerotherapy on both legs, you would use the -50 modifier with the sclerotherapy code. | |
| -51 | Multiple procedures. |
| Example: When multiple procedures, other than E&M, are performed at the same session by the same provider, the primary procedure or service may be reported as listed. The additional procedure(s) or service(s) may be identified by appending modifier -51 to the additional procedure or service code(s). Note: This modifier should not be appended to designated “add-on” codes. | |
| -59 | Distinct procedural service. |
| Example: If you performed a cyst excision and decided to also freeze some actinic keratoses, use the -59 modifier with the cryosurgery because it is a completely separate procedure from the excision. | |
| -79 | Unrelated procedure or service by the same physician during a postop period. |
| Example: If a patient comes in to have sutures removed during the postop period, and you perform cryosurgery on some actinic keratoses at the same visit when the sutures are removed, then -79 is used to clarify a separate procedure during a postop period. |
Essentials for Proper Coding and Billing
To code and bill properly, the following information is necessary:
ICD-9 Coding
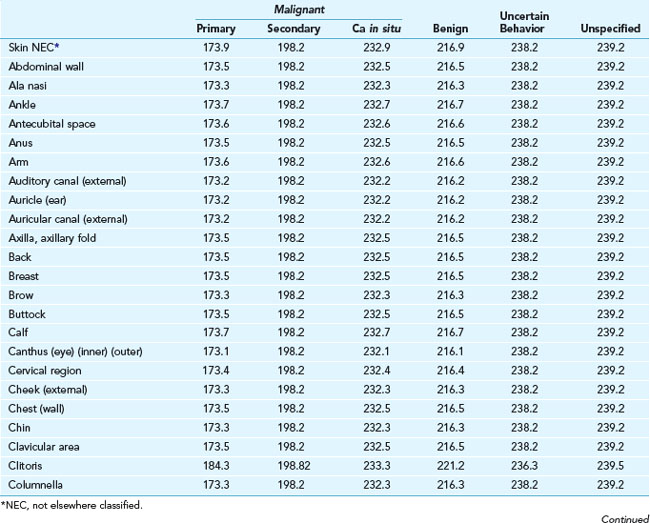
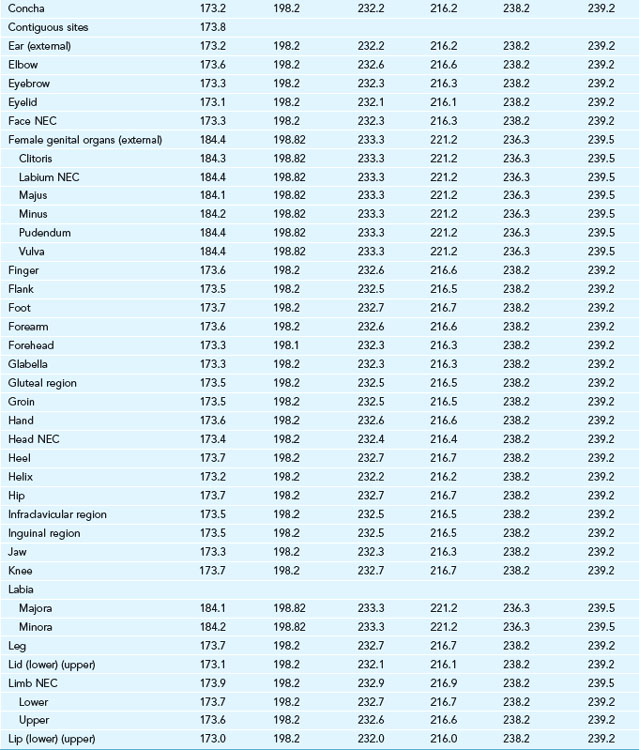
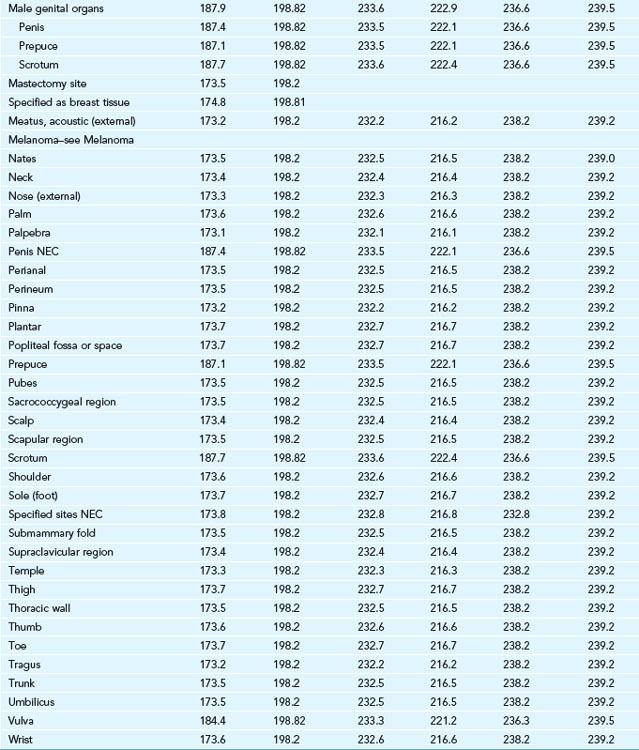
The majority of dermatologic procedures will involve an abnormal lesion. The diagnostic code (ICD-9) will vary depending on the location on the body and whether it is malignant (primary, secondary, or carcinoma in situ), benign, of uncertain behavior, or unspecified behavior (see Table 38-3). Specific conditions will have separate codes: abscesses, foreign bodies, cysts, etc.
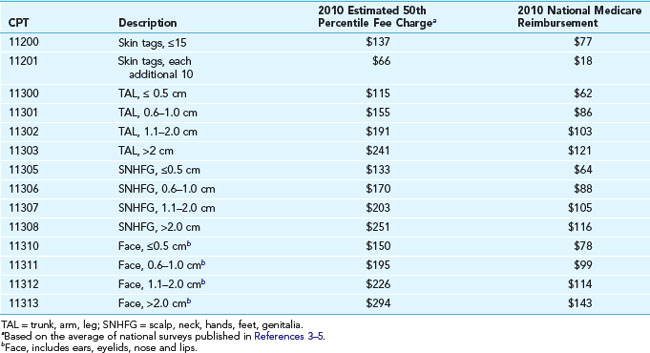
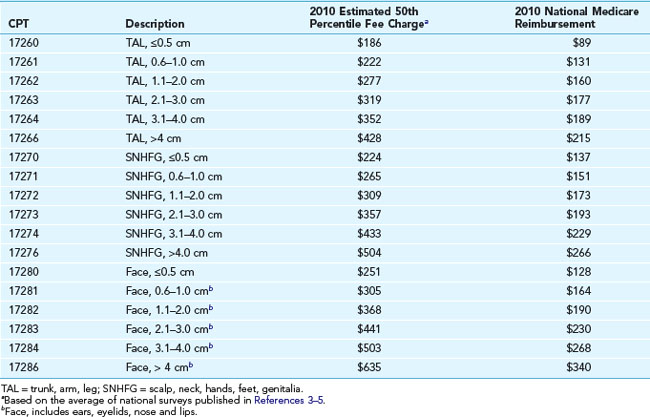
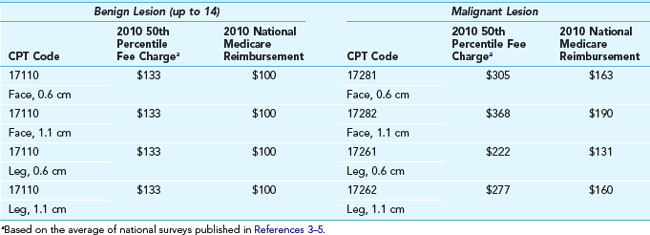
When the diagnosis is uncertain, several options are available. One can use the “uncertain behavior” code if the procedure is a biopsy. If a definitive treatment is performed, it sometimes helps to wait for the pathology to return before completing the billing process. It is best not to use the “unspecified” code because, for whatever reason, many insurance plans will reject that code. If a biopsy was performed, the reimbursement will be the same whether it is coded as “benign” or “malignant.” It makes little difference if the code is correct when only a biopsy was done. However, it is extremely important to know if the lesion was benign or malignant if a treatment is carried out. Note the differences in Table 38-4 for the 50th percentile charges and reimbursement for benign and malignant lesions. These lesions could have been treated with liquid nitrogen cryosurgery, electrosurgery, laser ablation, or other methods. The same time may have been required whether the lesion was benign or malignant, but the fees charged and eventually reimbursed vary markedly.
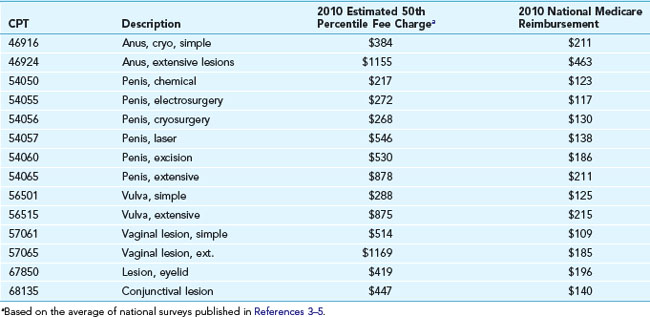
TABLE 38-4 50th Percentile Charges (National) for Destruction of Selected Skin Lesions and the Average Medicare Reimbursement (2010)
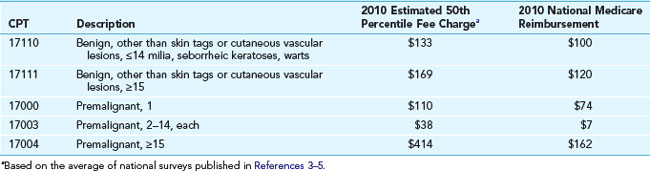
There is no specific code for premalignant lesions, such as actinic keratoses, on a particular body part. They can all be coded as 702.0 (actinic keratosis), regardless of location. However, reimbursement is higher for destruction of multiple premalignant lesions because each lesion (e.g., actinic keratosis) is charged individually (see Table 38-5).
The Importance of Size
Lesion size can be a major determinant in reimbursement. For some codes such as destruction for benign or premalignant lesions, size does not make a difference. However, if the lesion is malignant, the reimbursement varies widely (see Table 38-4). Similarly, size is very important in the repair of lacerations. For all excisions, size is best determined prior to the injection of any anesthetic.
The Importance of Location
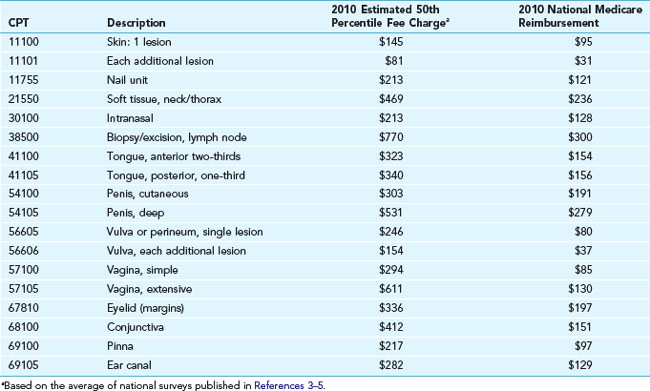
It is critical to know that the same procedure performed on different anatomic locations is reimbursed differently. Even for benign destructions, where size and location usually does not matter, there are some exceptions. For instance, treatment of benign lesions of the penis, vulva, vagina, perineum, anus, and the eyelids all have distinct CPT codes (see Table 38-6). Biopsy codes are also specific for similar sensitive areas (see Table 38-7).
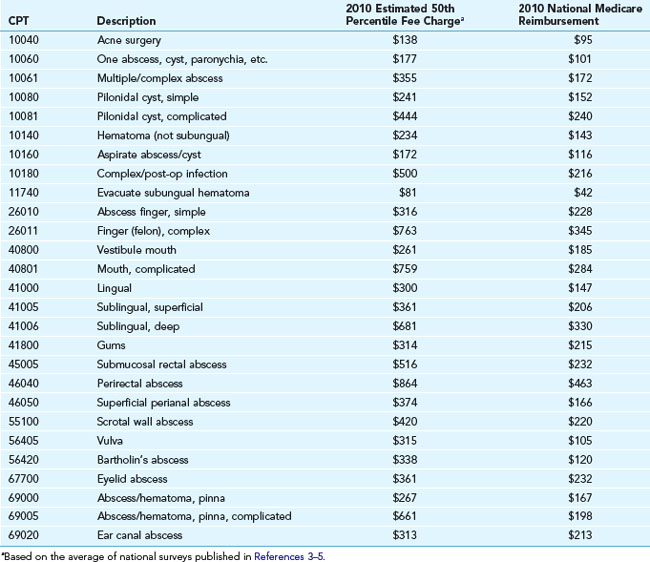
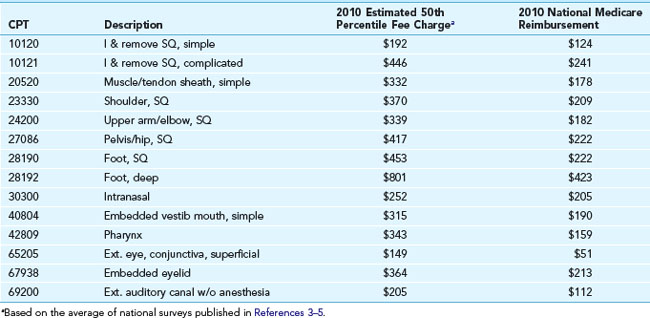
CPT codes and reimbursement numbers are provided in Table 38-8 for incision and drainage (I&D) procedures and in Table 38-9 for foreign body removal.
The Importance of Method
In general, the method of destruction does not change the coding. However, for the anus and genital areas, there are specific codes for the method used (see Table 38-6).
Shave excisions are distinctly different than full excisional procedures that require suture repair. Here, again, the “method” is important. Specific codes are used for shave excisions depending on size and location (see Table 38-10).
Specific CPT Codes: Office Visits
An E/M code can be charged in addition to a procedural code in specific, certain instances:
I&D Codes
A simple incision and drainage is billed with CPT code 10060; for complex or multiple lesions, the code is 10061. However, note that many locations have specific CPT codes (see Table 38-8). Those particular codes should be used rather than the generic ones since they often reimburse more.
Biopsies
The CPT code for a biopsy is method independent. In other words, shave, curettement, punch, incision, or excision could all be coded as a biopsy. If the biopsy codes are used, it does not really matter if the lesion is benign or malignant nor does the size matter, but location will make a difference. For most locations on the body, the first biopsy is coded as 11100 and there is a charge for each additional biopsy done (code 11101). Note that many of the specific biopsy CPT codes are dependent on the particular site biopsied (see Table 38-7). If a complete full-depth excision with a sutured repair is performed, it will most likely be compensated at a higher rate if billed as an excision and not as a biopsy (even when the diagnosis is not certain and the specimen is sent to pathology). For example, if an excision of a suspected BCC with margins is performed at the first visit, the reimbursement would be much higher for excision of a malignancy than biopsy of an unknown lesion.
Excisions and Lacerations
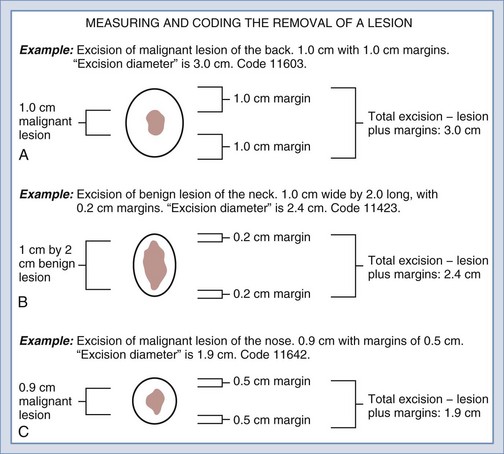
Coding for excisions can be straightforward. All of the previously identified factors need to be recorded: benign or malignant, location, and size. All measurements should be made before any anesthetic is administered. For the purpose of billing, the size of the lesion is determined by the “greatest clinical diameter of the apparent lesion plus that margin required for complete excision (lesion diameter plus the most narrow margins required equals the excised diameter)” (see Figure 38-1). If a lesion is long and narrow, the length plus the margins is actually the “diameter” size used for coding. So, in essence, it is the largest measurement of the lesion plus the margins that is used for proper coding:
Intermediate and Complex Repairs
A repair can be classified as intermediate or complex as follows:
|
CPT |
Description |
2010 Medicare National Nonfacility Price |
|---|---|---|
| 12031 | Scalp, axillae, trunk and/or extremities (excluding hands and feet), <2.6 cm | $226 |
| 12032 | 2.6–7.5 cm | $287 |
| 12034 | 7.6–12.5 cm | $286 |
| 12035 | 12.6–20.0 cm | $347 |
| 12041 | Neck, hands, feet and/or external genitalia, <2.6 cm | $236 |
| 12042 | 2.6–7.5 cm | $272 |
| 12044 | 7.6–12.5 cm | $318 |
| 12045 | 12.6–20.0 cm | $348 |
| 12051 | Face, ears, eyelids, nose, lips and/or mucous membranes, <2.6 cm | $251 |
| 12052 | 2.6–5.0 cm | $287 |
| 12053 | 5.1 cm–7.5 cm | $316 |
| 12054 | 7.6 cm–12.5 cm | $335 |
| 12055 | 12.6 cm–20.0 cm | $402 |
The CPT code for an intermediate repair is based on the length of the final closed wound (regardless of the size of a lesion or the mechanism of an injury). The codes for intermediate repairs encompass wide ranges of wound length as these are also used for laceration repairs (see Table 38-11). When it comes to laceration and wound repairs that are unrelated to a medical excision, intermediate repairs are billed instead of a simple repair and not in addition to the simple repair. Reasons to upgrade a simple repair to a complex repair beyond just a two-layer closure include the need for extensive wound cleaning and/or debridement before closure.
A complex repair can be billed if extensive undermining or debridement is required or if the time required for the procedure is excessive. If a flap, plasty, or graft is performed, other specific codes (14000 and 15000) apply. See Chapter 13 for further information on billing for flaps.
Destruction of Lesions
The number one determinant for the correct CPT code for a lesion destruction is whether the lesion is benign, premalignant, or malignant. If benign, destruction by any method of 1–14 lesions is the same code: 17110. If 15 or more are destroyed, then the code is 17111. The exceptions for various locations are noted in Table 38-6. If premalignant (e.g., actinic keratoses), the first lesion is coded as 17000. For lesions 2–14, 17003 is used, and a charge is made for each additional lesion. Use 17004 when 15 or more premalignant lesions are treated.
For malignant lesions, size becomes important as well as location (see Table 38-12).
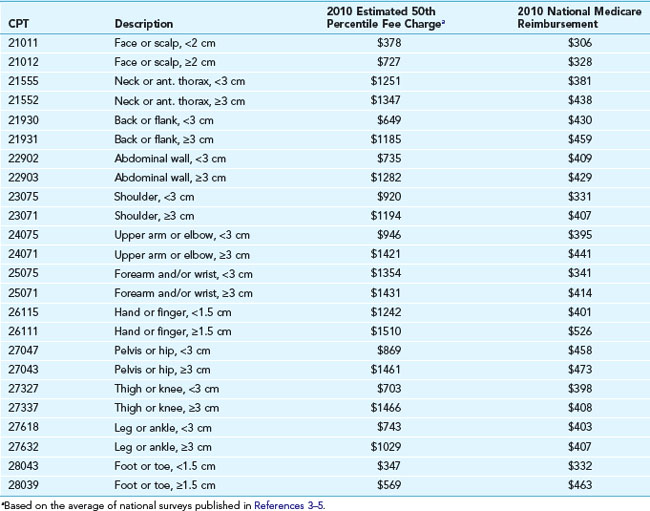
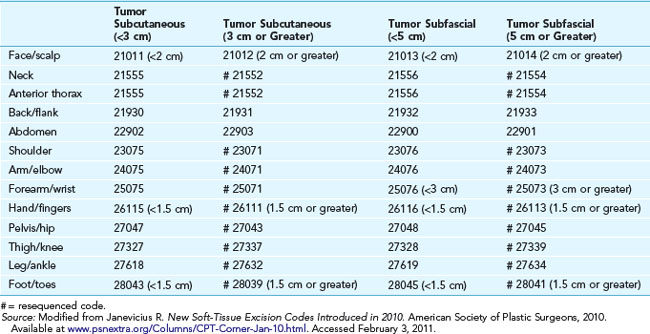
Tumors
The removal of subcutaneous tumors, such as lipomas, carries a specific diagnosis. These are not skin lesions. The CPT code was changed in 2010 and the proper code is determined based on whether the lesion is subcutaneous, subfascial, or whether it requires a radical excision. It does not matter if it is benign or malignant, but body site and depth of lesion do change the CPT code (Tables 38-13 and 38-14).
All subcutaneous tumors are reported by whether they are <3 cm or ≥3 cm, except:
All subfascial tumors are reported by whether they are <5 cm or ≥5 cm, except:
Also, the routine skin diagnostic ICD-9 codes are not used. Rather, ICD-9 provides specific codes for subcutaneous and deep tumors of the various body locations (see Table 38-15). It is important to be aware of these tumor removal codes, because the majority are much more highly reimbursed than those for skin lesion removal. A small subcutaneous 1-cm lipoma on the back that is removed with a simple incision and digital expression with a Steri-Strip closure (CPT 21555) can take a mere 5 to 10 minutes. The 50th percentile fee charged is $805. Medicare reimburses $205. For a more detailed discussion of lipoma coding see Chapter 12, Cysts and Lipomas, page 145.
|
CPT |
Description |
|---|---|
| Benign Soft Tissue Tumors | |
| (Do not use “Neoplasm–Skin” codes. These CPT codes are for deep soft tissue masses with their own distinct specific codes, both benign and malignant.) | |
| 210.4 | Benign neoplasm, gum |
| 214.0 | Lipoma, face, SQ |
| 214.1 | Lipoma, other SQ tissue |
| 215.0 | Benign neoplasm, face |
| 215.0 | Benign neoplasm, neck |
| 215.0 | Benign neoplasm, head |
| 215.2 | Benign neoplasm, shoulder |
| 215.2 | Benign neoplasm, upper extremity |
| 215.3 | Benign neoplasm, hip |
| 215.3 | Benign neoplasm, lower limb |
| 215.4 | Benign neoplasm, thorax |
| 215.5 | Benign neoplasm, abd. wall |
| 215.6 | Benign neoplasm, buttock |
| 215.7 | Benign |
| 215.7 | Benign neoplasm, trunk |
| 229.8 | Benign neoplasm, hand |
| Malignant Soft Tissue Tumors | |
| 171.0 | Cancer, head |
| 171.0 | Cancer, face |
| 171.0 | Cancer, neck |
| 171.2 | Cancer, upper limb |
| 171.2 | Cancer, shoulder |
| 171.3 | Cancer, hip |
| 171.3 | Cancer, lower limb |
| 171.5 | Cancer, abdominal wall |
| 171.7 | Cancer, back/flank |
Cosmetic Versus Medical Removals
Cosmetic procedure codes (Box 38-1) are primarily used for documentation purposes, because these procedures are not usually covered by insurance plans. As mentioned, some insurance carriers may cover chemical peels for conditions such as acne, but such coverage is not common. The 17000 code may be used for cosmetic laser treatments.
Purchasing Equipment
Aesthetic equipment can be very expensive, ranging from $10,000 for a microdermabrasion unit to more than $150,000 for various lasers for hair and tattoo removal, skin resurfacing, etc. Purchase of this equipment should be researched well. Company representatives are quick to show projected summaries with significant returns. However, the clinician must consider several factors, including true demand, time, insurance, personal property tax, maintenance contracts (up to $15,000 annually, per unit), incidental disposable materials, and additional office space and personnel. A successful aesthetics practice will generally require a website and advertising. The question to ask is “Will this all be cost effective in a busy practice?” The reader is strongly encouraged to review Needham and Katz’s work to better assess whether a major purchase “makes sense.”8
Cosmetic Procedure Financial Considerations
Practitioners entering the aesthetics field may choose to start with procedures that have lower start-up and overhead costs, such as chemical peels, botulinum toxin, dermal filler injection procedures, and microdermabrasion.9 Products may be purchased in small quantities as needed, which helps to keep the costs down. Fees charged for these procedures are at the discretion of the provider, and are typically determined using the following methods10:
Recommendations for aesthetic procedure fees can be found in the Financial Considerations and Coding sections of the chapters that cover the following procedures: botulinum toxin (Chapter 21), chemical peels (Chapter 22), microdermabrasion (Chapter 23), dermal fillers (Chapter 25), laser hair reduction (Chapter 26), laser photorejuvenation (Chapter 27), nonablative lasers for wrinkle reduction (Chapter 28), ablative lasers for skin resurfacing (Chapter 29), and laser tattoo removal (Chapter 30).
Cosmetic Practice Financial Pearls
Summary Tips
Resources
1. International Statistical Classification of Diseases, Clinical Modification, ICD-9-CM. Chicago: The American Medical Association, 2010.
2. Physicians Current Procedural Terminology 2010. Chicago: American Medical Association, 2010.
3. 2010 Physician’s Fee Reference. West Allis, WI: Yale Wasserman, DMD, Medical Publishers, 2010.
4. 2010 Physicians’ Fee & Coding Guide. Atlanta, GA: MAG Mutual HealthCare Solutions, 2010.
5. National Fee Analyzer. Eden Prairie, MN: Ingenix, 2010.
6. Pfenninger JL. The Reimbursement Manual for Office Procedures, 16th ed. Austin, TX: The National Procedures Institute; 2010.
7. Pfenninger JL. Coding for Dermatologic Procedures, 2004. [Videotape Creative Health Communications, Essexville, MI, 2004.
8. Needham M, Katz B. Buying office equipment (Appendix L). In Pfenninger JL, Fowler GC, editors: Pfenninger and Fowler’s Procedures for Primary Care, 3rd ed, Philadelphia: Mosby/Elsevier, 2011.
9. Small R. Botulinum toxin type A for facial rejuvenation. In: Mayeaux E, editor. The Essential Guide to Primary Care Procedures. Philadelphia: Lippincott Williams & Wilkins; 2009:200-213.
10. Werschler P. The costs of products and services. Cosm Dermatol. 2008;21(7):376-383.