Surgical Repair of Urethral Prolapse
Prolapse of edematous urethral mucosa may be of sufficient degree to require surgical excision (Figs. 82–1 and 82–2). It is important to differentiate urethral prolapse from a urethral caruncle. The former is circumferential in nature, is less common, and is treated surgically, whereas the latter is much more common, usually requires only topical estrogen therapy, and usually is isolated to the posterior urethral meatus.
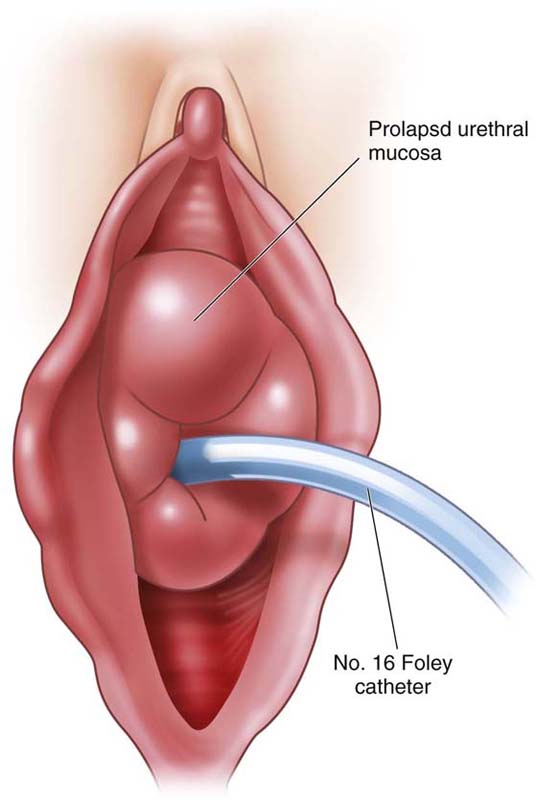
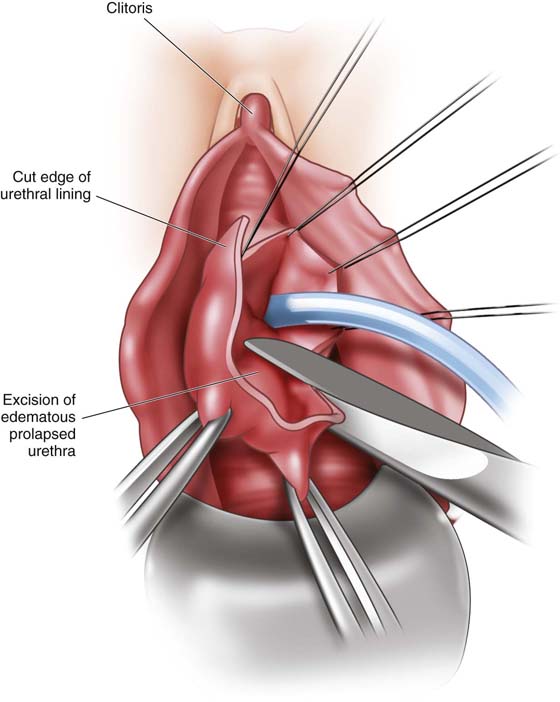
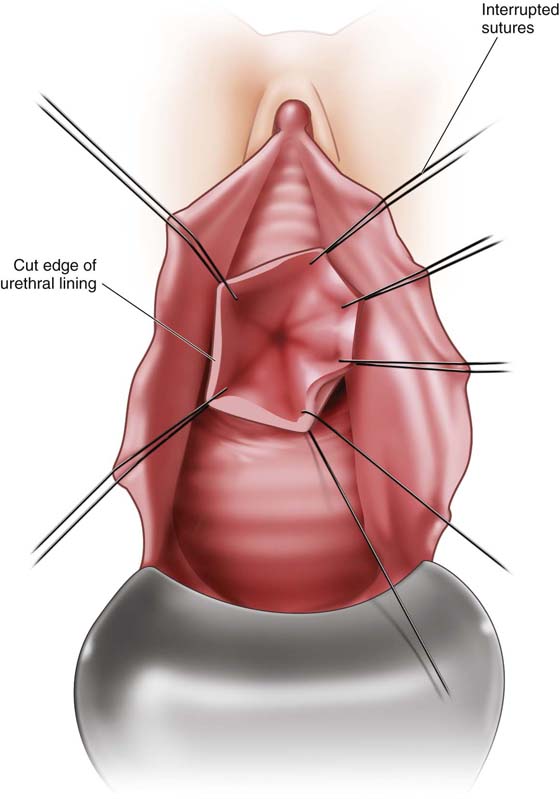
The procedure begins by identifying the urethral lumen (Fig. 82–3). Placement of a transurethral catheter is an option; however, it can be difficult to work around. The excision begins at the 12 o’clock position. A stay suture is placed to hold the tissue and provide traction. Working in a counterclockwise fashion, the redundant mucosa is trimmed with a scissors or is excised using needle-tip cautery (Fig. 82–4). During excision, each anchoring suture (usually 3-0 chromic or 4-0 Vicryl) is placed as the mucosa is freed (Fig. 82–5). This tissue is usually very edematous and friable. Failure to secure the mucosa with stay sutures as the mucosal prolapse is excised can result in retraction of the mucosa superiorly, making it much more difficult to reapproximate. A transurethral catheter may be left in place for a day if there is significant swelling.
FIGURE 82–1 Complete uterovaginal prolapse with urethral prolapse.
FIGURE 82–2 Close-up view of the urethral prolapse once the uterovaginal prolapse has been reduced.
FIGURE 82–3 Circumferential urethral prolapse with a transurethral catheter in place.
FIGURE 82–4 Anchor sutures are placed as the urethral prolapse is trimmed.
FIGURE 82–5 The urethral prolapse has been excised and the anchor sutures are now ready to be secured in place.