CHAPTER 9 Surgical Pearls for Fixed-Bearing Medial Unicompartmental Knee Arthroplasty
Skin Incision
The ACL can be visualized at the time of the arthrotomy, but visualization of an intact ACL is not always required. Certainly more important appears to be the stability of the knee. An examination under anesthesia can be performed and stability of the ACL assessed. A nonfunctioning ACL with an unstable knee increases the sliding forces that can eventually lead to early polyethylene wear and joint failure. Engh and Ammeen reported on the results of unicompartmental knee arthroplasty without an intact ACL, and good results can be obtained if functional instability is not present.1 This differs from the classic article by Goodfellow and O’Connor that showed a higher failure rate without an intact ACL. Therefore, the emphasis is on knee stability, not ACL integrity.2 Visualization at the ACL does not answer completely the status of the ACL. Cushner et al. not only described significant loss of the ACL at the time of indicated total knee arthroplasty, but pathologic changes in the “viable” ACL were also noted.3 Mullaji et al. recently evaluated tibial cartilage wear in patients undergoing total knee arthroplasty and found that the articular wear pattern can provide clues to the functional status of the ACL.4 Posterior-half involvement of the medial plateau was more commonly seen when a functional ACL was not present. This is a helpful pearl since studies from Trompeter et al. showed that the clinical appearance of the ACL was not a good predictor of severity on microscopic examination.5
Certainly, the size of the incision should not compromise results. Hamilton et al. reviewed 221 unicompartmental arthroplasties performed using the MIS technique.6 This cohort was compared to a cohort of 514 standard-incision unicompartmental knee arthroplasty patients. In the MIS group, 9 of 221 were revised for loosening. Of the remaining 212 patients, 16 patients required 18 nonrevision reoperations. In other words, 25 of 221 required at least one reoperation (11.3%). This compared to 8.6% for the standard-incision group, with a higher aseptic loosening rate also noted in the MIS group (3.7% vs. 1%).
Decreasing Blood Loss
Once a skin incision is made, a surgical pearl to decrease blood loss is to inject the knee arthrotomy site with a lidocaine (Marcaine)/epinephrine solution. Thirty milliliters injected along the arthrotomy site did result in a significant decrease in blood loss in our total knee arthroplasty patients.7 While this procedure was initially described in a total knee arthroplasty patient, it could be also performed in unicompartmental arthroplasty patients. We have extended the use of lidocaine with epinephrine to all arthrotomy patients with the goal of not only less bleeding and fewer transfusions but overall less hematoma in the joint postoperatively. Our thoughts are that less blood in the joint improves the patient’s function. Periarticular steroid injections can also be used to improve outcomes following unicondylar knee replacement. Pang et al. recently performed a prospective randomized study comparing 90 knees over a 2-year period where injection with triamcinolone acetonide, bupivacaine, and epinephrine was compared to a control group in which only bupivacaine and epinephrine injections were performed. Improvement was noted in midterm and short-term results with no increase in infection or tendon failures reported.8
Solid Repair of the Arthrotomy
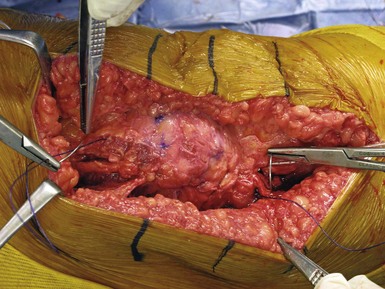
Another pearl utilized at our institution is a solid repair of the arthrotomy. If a solid repair is not performed, this can result in late patella instability and subluxation. We believe that a more watertight seal can not only improve knee appearance but also result in less wound drainage in the immediate postoperative period. We currently utilize a bidirectional barbed suture design to facilitate arthrotomy closure (Quill Suture; Angiotec, Vancouver, British Columbia). Our initial studies showed that not only did we achieve a shorter operating time secondary to a quicker closure of the arthrotomy, but a more watertight closure was also described in the laboratory setting9,10 (Fig. 9–1).
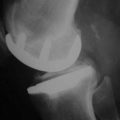
Tibial Bone Cuts
There are numerous pearls when it comes to completing the tibial bone cuts. As with all knee procedures, the accuracy of the tibial cut must be stressed. In several ways, a tibial cut for unicompartmental knee is a bit more difficult since mis-cuts or malaligned cuts can be less forgiving during the postoperative period. For example, Hernigou and Deschamps demonstrated that extreme tibial slope could increase failure rates and concluded that a slope of greater than 7° should be avoided.11 A pearl to avoid excessive slope is to use an angel wing or similar type of device and place it in the cutting guide before the osteotomy is performed. The amount of bone resected anteriorly should be similar to that resected posteriorly (Fig. 9–2). If this occurs, then the slope is well within the 7° limit. The depth of the resection also needs to be precise to avoid the complication of a posterior plateau fracture. These fractures are multifactorial and certainly can be minimized with a more conservative initial cut (2–3 mm), with the ability to cut more bone if needed.
Limiting of guide fixation pins may also play a role, because the more pins utilized, the higher the risk of fracture. Seon et al. reported two occasions of shear fracture as a result of number of guide pins utilized.12 Yang et al. showed similar results that appear to be associated with the technique related to the tibial osteotomy guide.13 Van Loon et al. reviewed peripheral tibial plateau fractures and, once again, they appeared to be related to surgical technique. This complication can be avoided by limiting the number of fixation pins, achieving the proper cutting depth, exercising caution when utilizing the operative mallet, and ensuring proper component sizing.14 Brumby et al. evaluated tibial stress fractures and noted that the use of three or more fixation pins did increase their occurrence.15 They felt that, if three or more pins were deemed necessary, the risk of stress fracture increases. Peripheral pins must not violate the medial cortex and should be avoided if at all possible.
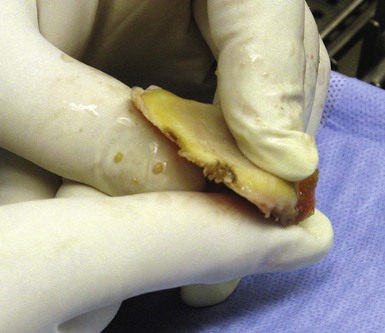
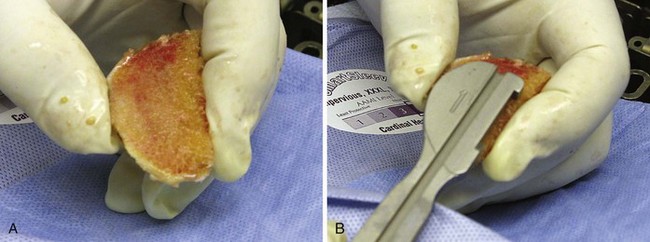
One means to avoid damage to the anterior cortex of the tibia is using caution on removing the osteotomy fragment. We like to remove it in one piece because the osteotomy fragment can serve as a good template for the proper-size tibial component (Fig. 9–3). To remove it in one piece without damage to the anterior cortex, we often use a tibial guide and place an ostium on leveling off the tibial guide, not the anterior cortex. By pushing up from the anterior guide and pulling the tibial fragment forward, the piece can be removed intact to be used for sizing purposes and the anterior rim of the cortex is not damaged (Fig. 9–4).
Simpson et al. evaluated bone strain and found that a 40% increase is noted after implantation.16 This increased stress reaction may be what contributes to the vague medial pain often seen in the initial 12 months following the unicompartmental procedure. Proper patient assurance is required if no fracture is found but medial pain exists. Unusually by the 12-month mark, these symptoms resolve as bone remodeling occurs.
1 Engh GA, Ammeen D. Is an intact anterior cruciate ligament needed in order to have a well-functioning unicondylar knee replacement? Clin Orthop Relat Res. 2004;428:170-173.
2 Goodfellow J, O’Connor J. The anterior cruciate ligament in knee arthroplasty. A risk-factor with unconstrained meniscal prostheses. Clin Orthop Relat Res. 1992;276:245-252.
3 Cushner FD, La Rosa DF, Vigorita VJ, et al. A quantitative histologic comparison: ACL degeneration in the osteoarthritic knee. J Arthroplasty. 2003;18:687-692.
4 Mullaji AB, Marawar SV, Luthra M. Tibial articular cartilage wear in varus osteoarthritic knees: correlation with anterior cruciate ligament integrity and severity of deformity. J Arthroplasty. 2008;23:128-135.
5 Trompeter AJ, Gill K, Appleton MA, Palmer SH. Predicting anterior cruciate ligament integrity in patients with osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2009;17:595-599.
6 Hamilton WG, Collier MB, Tarabee E, et al. Incidence and reasons for reoperation after minimally invasive uni-compartmental knee arthroplasty. J Arthroplasty. 2006;21(6 Suppl 2):98-107.
7 Kim RH, Scuderi GR, Cushner FD, et al. Use of lidocaine with epinephrine injections to minimize blood loss in total knee replacement. Paper presented at the annual meeting of the Knee Society.
8 Pang HN, Lo NN, Yank KY, et al. Peri-articular steroid injection improved the outcome after uni-condylar knee replacement: a prospective, randomized controlled trial with a two-year follow-up. J Bone Joint Surg [Br]. 2008;90:738-744.
9 Kissin YD, Cushner FD, Nett MP, Chadha P. Use of a novel suture to improve wound appearance and increase operating room efficiency. Paper presented at the annual meeting of the Eastern Orthopedic Association, Nassau, Bahamas, 2009.
10 Khanuja HS. Biomechanical comparison of medial parapatellar arthrotomy repair. Presentation at the annual. New Orleans, LA: AAOS Meeting; 2009.
11 Hernigou P, Deschamps G. Posterior slope of the tibial implant and the outcome of uni-compartmental knee arthroplasty. J Bone Joint Surg [Am]. 2004;86:506-511.
12 Seon JK, Song EK, Yoon TR, et al. Tibial plateau stress fracture after unicondylar knee arthroplasty using a navigation system: two case reports. Knee Surg Sports Traumatol Arthrosc. 2007;15:67-70.
13 Yang KY, Yeo SJ, Lo NN. Stress fracture of the medial tibial plateau after minimally invasive uni-compartmental knee arthroplasty: a report of 2 cases. J Arthroplasty. 2003;18:801-803.
14 Van Loon P, de Munnynck B, Bellemens J. Peri-prosthetic fracture of the tibial plateau after uni-compartmental knee arthroplasty. Acta Orthop Belg. 2006;72:369-374.
15 Brumby SA, Carrinton R, Zayontz S, et al. Tibial plateau stress fracture: a complication of uni-compartmental knee arthroplasty using 4 guide pinholes. J Arthroplasty. 2003;18:809-812.
16 Simpson DJ, Price AJ, Gulati A, et al. Elevated proximal tibial strains following uni-compartmental knee replacement—a possible cause of pain. Med Eng Phys. 2009;31:752-757.