Surgical Management of Ectopic Pregnancy
Linear Salpingostomy for Tubal Ectopic Pregnancy
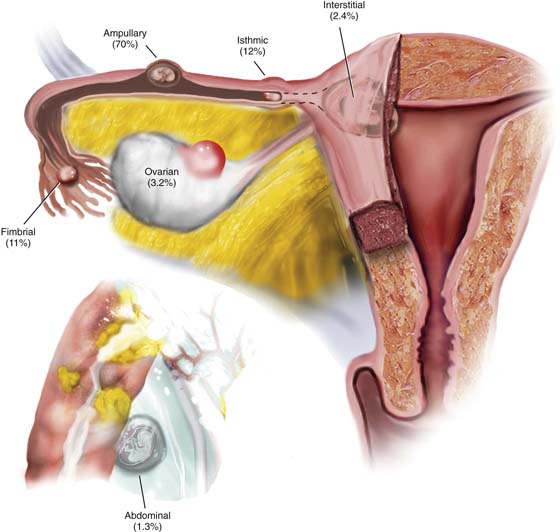
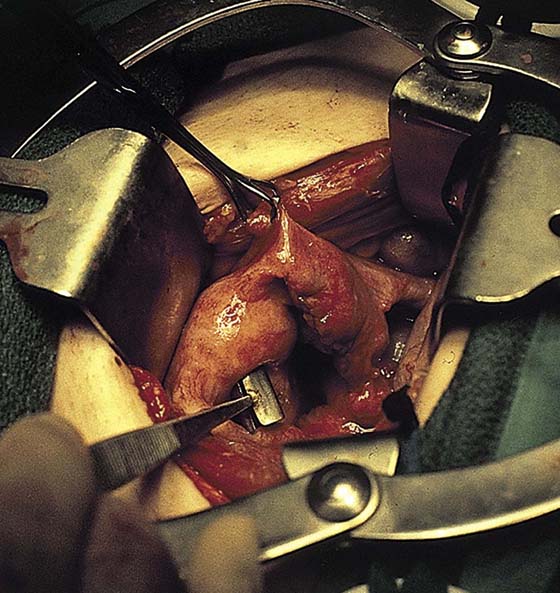
Ectopic pregnancy may occur in a variety of locations. A vast majority of these occur within some part of the oviduct (Fig. 26–1). The goal of early diagnosis and prompt therapy is prevention of rupture and severe internal hemorrhage (Fig. 26–2). Although most tubal ectopic pregnancies are managed laparoscopically, certain circumstances may require laparotomy. These include large tubal pregnancies, rupture with substantial hemorrhage and hypovolemia, and cornual pregnancies. The open procedure for treating a leaking or unruptured tubal pregnancy is identical to the laparoscopic procedure. A linear salpingostomy is performed as the operation of first choice. If the tube has been severely damaged or if bleeding cannot be controlled, then a salpingectomy should be done.
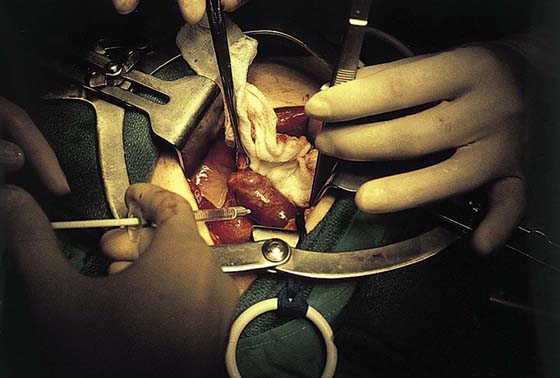
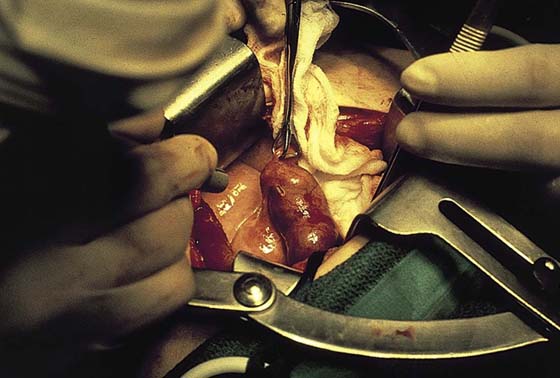
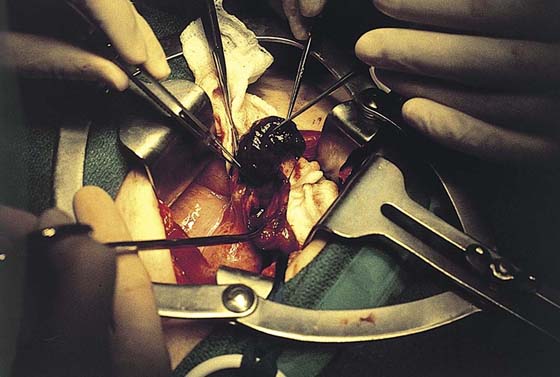
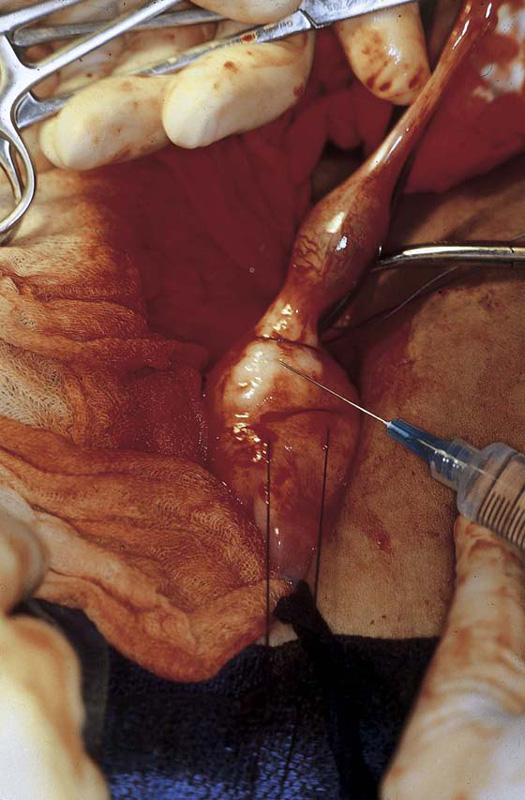
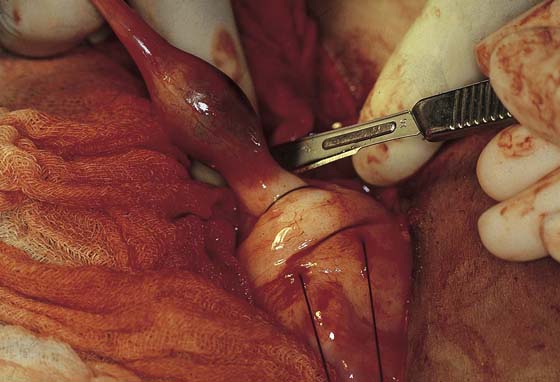
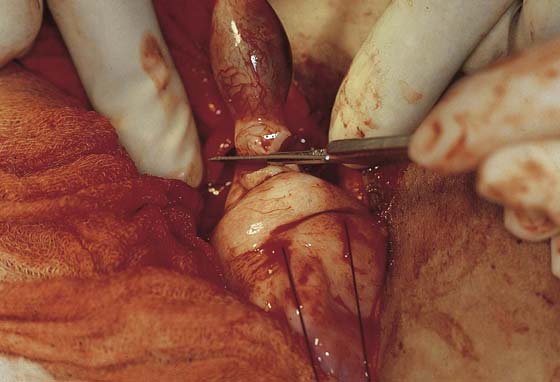
The affected tube is identified, as is the ipsilateral ovary (Fig. 26–3). Any blood in the abdominal cavity is evacuated. The contralateral tube and ovary are likewise examined for pathology. Next, the tube containing the tubal pregnancy is isolated via abdominal packs. A 1 : 100 vasopressin solution is injected (Fig. 26–4). It is wise to place traction (untied) stitches at either extreme of the bulging tube; alternatively, Babcock clamps may be applied. A trace incision is made on the antimesenteric edge of the tube with the use of an energy device (laser or electrosurgical) (Figs. 26–5 and 26–6). The incision is extended transmurally until the products of conception are contacted (Fig. 26–7).
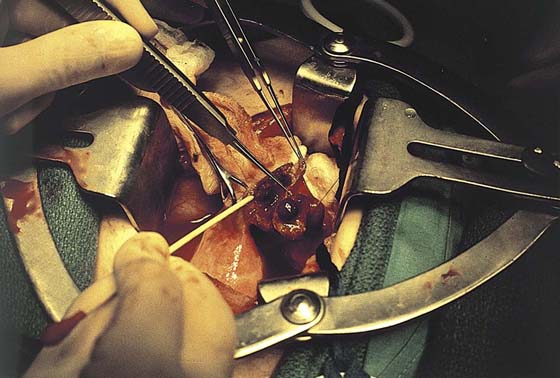
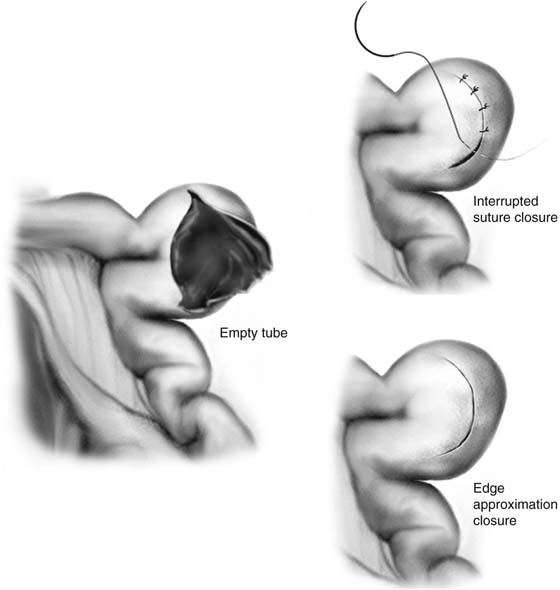
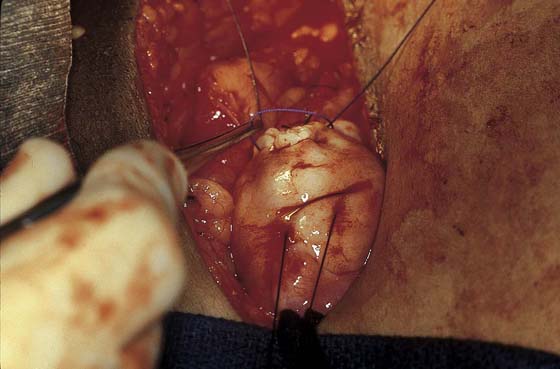
At this point, the pressure of the blood and clot expands the opening in the tube (Figs. 26–8 and 26–9). An irrigating probe is placed into the incision to facilitate separation of the products from the wall of the oviduct (Fig. 26–10). Traction is placed on the products, and the entire mass of blood, placenta, and embryo is removed (Fig. 26–11). The bed is irrigated (Fig. 26–12). The tube may be closed in one layer using 3-0 or 4-0 Vicryl, or the wound edges may be simply approximated and allowed to seal spontaneously (Figs. 26–13 through 26–17).
FIGURE 26–1 This schematic drawing illustrates the various intra-abdominal sites and their relative frequencies for ectopic pregnancy.
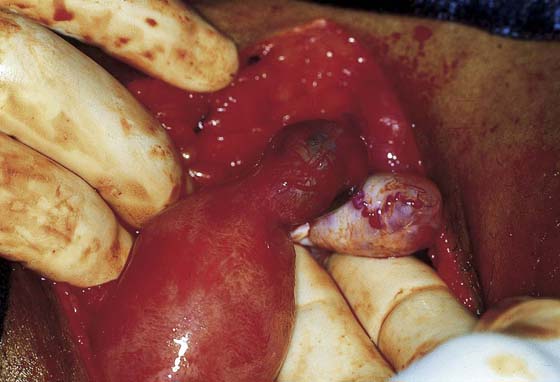
FIGURE 26–2 This ruptured ectopic pregnancy implanted on the mesentery of the ileum. When the abdominal pregnancy was diagnosed, the fetus had grown to 14 weeks’ gestational size.
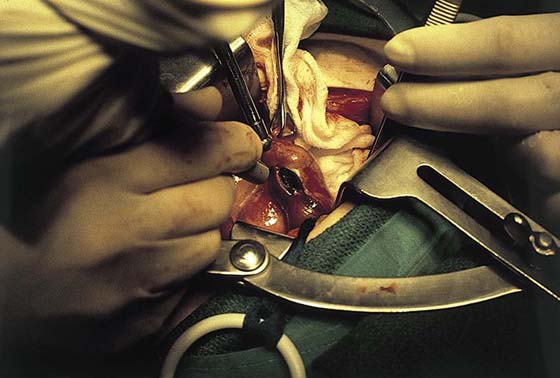
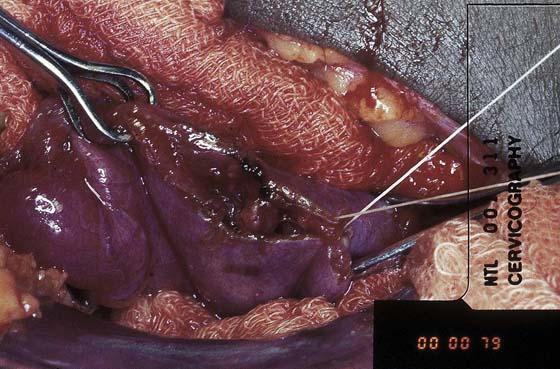
FIGURE 26–3 The right oviduct is grasped and elevated to reveal a swollen ampullary portion of the tube.
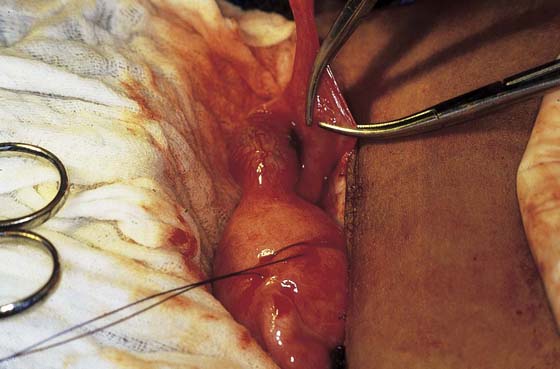
FIGURE 26–4 The oviduct is injected with 1 : 100 vasopressin solution. The surgical site is injected to induce vasoconstriction.
FIGURE 26–5 The antimesenteric surface is opened with an energy device (laser or electrosurgical) for purposes of hemostasis. In this case, a carbon dioxide (CO2) laser is used.
FIGURE 26–6 The incision is linear and measures between 1 and 2 cm in length.
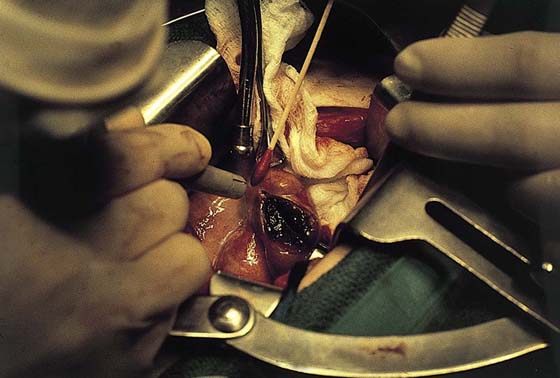
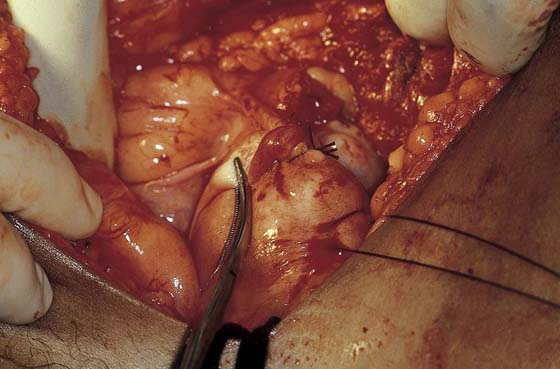
FIGURE 26–7 As the tubal lumen is encountered, the pressure of the blood spreads the incision.
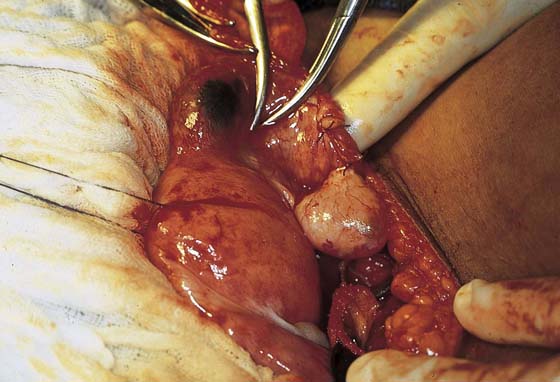
FIGURE 26–8 Alternatively, an electrosurgical handpiece equipped with a needle electrode may be used to perform the salpingostomy. The net effect is similar to that produced by the carbon dioxide (CO2) laser.
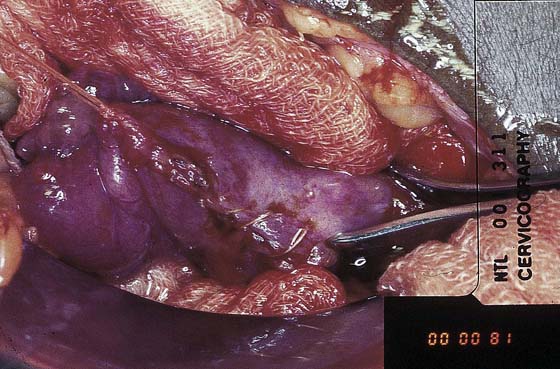
FIGURE 26–9 Typically, the tubal pregnancy presents as a large blood clot within the lumen.
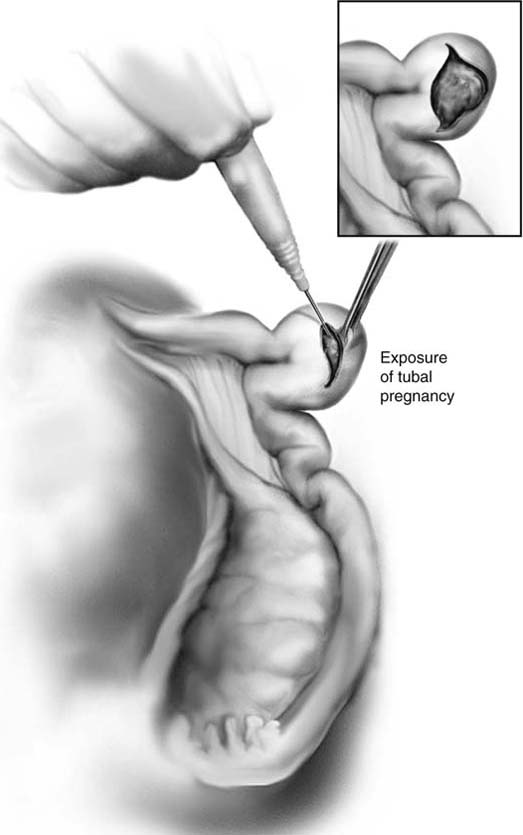
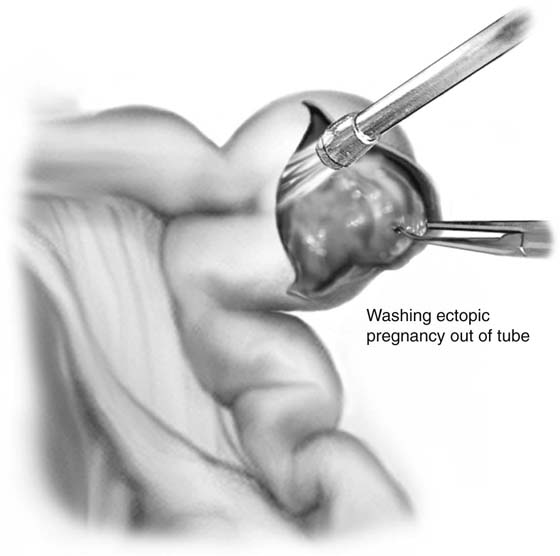
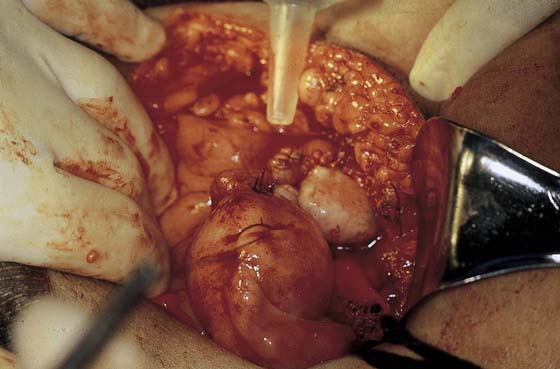
FIGURE 26–10 A small cannula is inserted into the incision, and the pressure of the irrigating solution dislodges the products of conception from the tube wall.
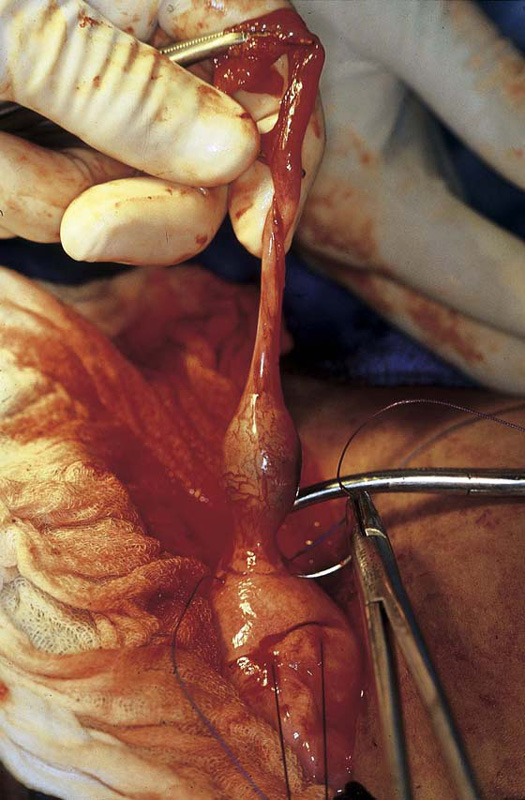
FIGURE 26–11 With the use of fine manipulating hooks or forceps, the entire ectopic pregnancy is removed en masse.
FIGURE 26–12 The tubal bed is typically dry but should be irrigated with saline to check for bleeding. The repair may be initiated.
FIGURE 26–13 The incision may be closed with 4-0 Vicryl, interrupted through-and-through, simple sutures, or the edges of the incision may be simply pulled together and allowed to seal spontaneously.
FIGURE 26–14 Unruptured ectopic pregnancy within the ampullary portion of the tube. Two Babcock clamps isolate the affected tubal segment.
FIGURE 26–15 A salpingostomy has been performed, and the products have been extracted. The tube and the ectopic bed are irrigated with warmed saline.
FIGURE 26–16 The linear incision in the oviduct will be closed, in this case with the use of 4-0 Vicryl.
FIGURE 26–17 The incision has been closed with simple interrupted stitches.
Cornual Excision and Salpingectomy for Cornual Ectopic Pregnancy
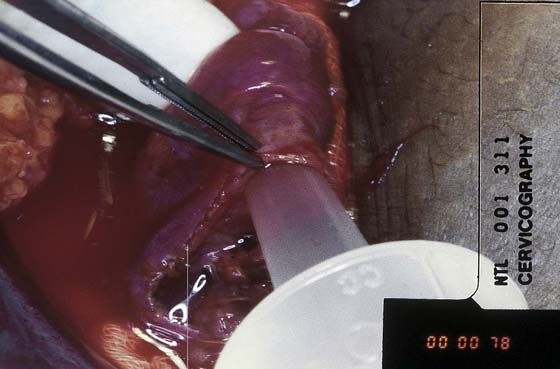
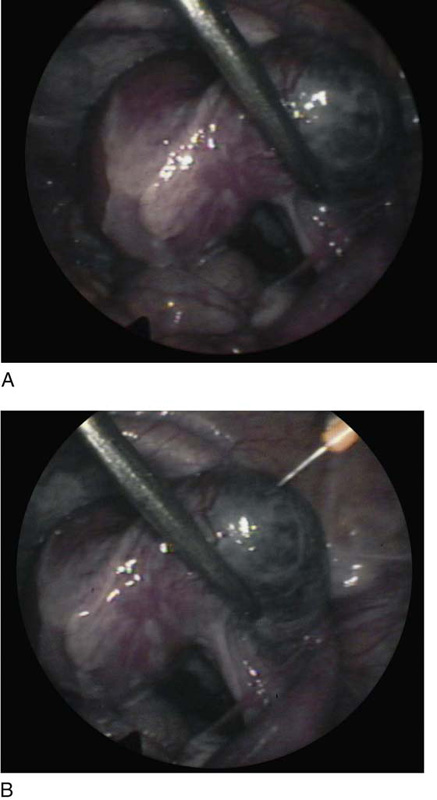
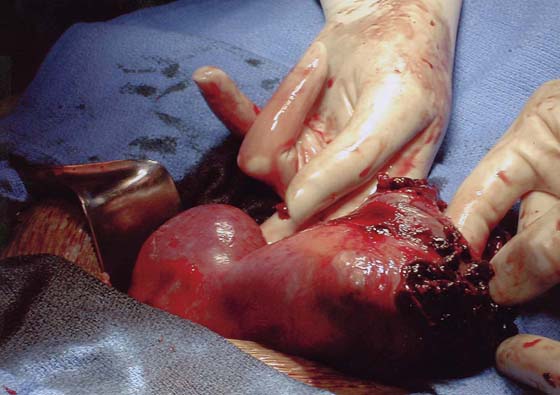
This abnormal implantation occurs in the interstitial portion of the oviduct and has a high potential for very serious hemorrhage related to the greater size of the ectopic pregnancy, the rich vascular network formed by the anastomosis of the uterine and ovarian arteries, and the later gestational age of the conceptus at the time of diagnosis (Fig. 26–18A, B). Cornual pregnancies account for 2.6% of all ectopic pregnancies and present a five times greater risk for fatality (i.e., 2.5% maternal mortality) (Fig. 26–19).
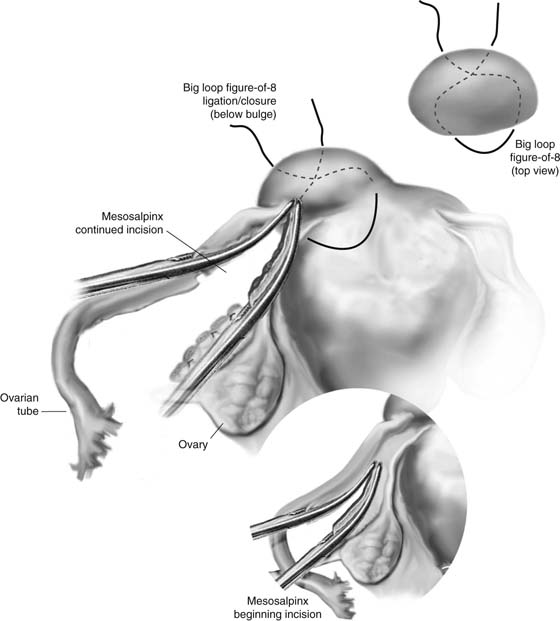
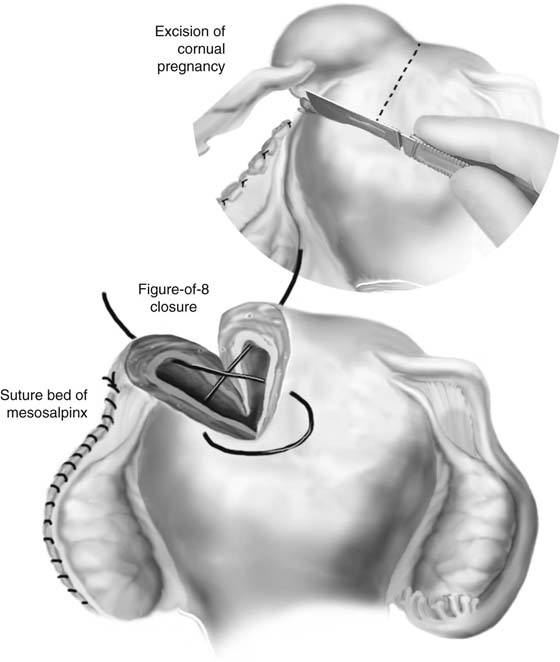
The affected tube is grasped with Babcock clamps. The mesosalpinx is doubly clamped and incised between the two clamps along its entire length. The clamped pedicles are suture-ligated on either side with 0 Vicryl. The ovary may be preserved by avoiding the infundibulopelvic and utero-ovarian ligaments (Fig. 26–20).
When the tubouterine junction is reached, a figure-of-8 suture of 1 Vicryl or polydioxanone (PDS) is placed so as to encompass the bulging mass of the cornual pregnancy.
A 1 : 200 vasopressin solution (10 to 15 mL) is injected into the cornua.
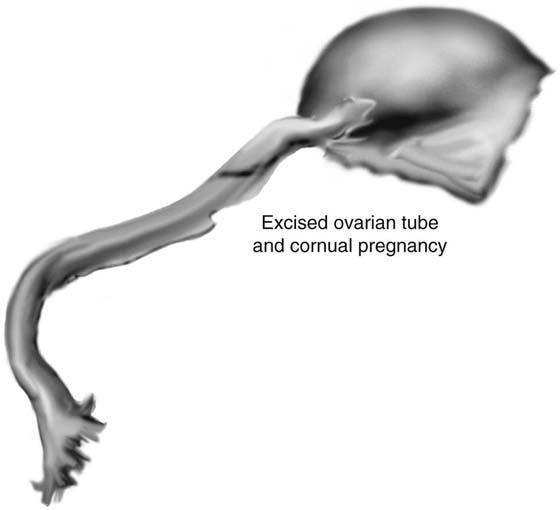
With a scalpel or energy device, the cornual pregnancy is wedged out of the uterus (Fig. 26–21). Simultaneously, the previously placed figure-of-8 suture is tightened to control bleeding. When the entire tubal mass has been excised, several pumping arterioles will have to be secured by clamping and suture ligatures. The large figure-of-8 suture is then tied (Fig. 26–22). The cornual portion of the uterus is further secured by placing three or four additional figure-of-8 sutures through the serosa and myometrium (Fig. 26–23).
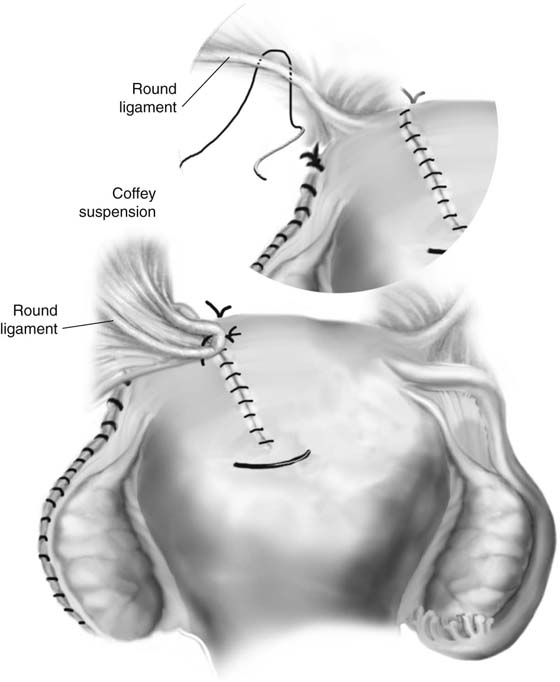
The uterus is peritonized and supported by placement of a U-shaped stitch from the cornual resection site through the ipsilateral round ligament. As the suture is tightened and tied into place, a knuckle of round ligament and peritoneum is pulled over to cover the operative site (see Fig. 26–23).
Rudimentary horn pregnancy occurs rarely, that is, in 1 of 100,000 pregnancies. This condition is attributed to pregnancy occurring in a noncommunicating horn of a bicornuate uterus. Rupture risk is high, and outcomes are similar to those for ruptured cornual pregnancy (Figs. 26–24 and 26–25).
FIGURE 26–18 A. An interstitial pregnancy presents as a bulge in the cornual region of the uterus. B. Laparoscopic view of an unruptured right cornual pregnancy.
FIGURE 26–19 This large cornual pregnancy clearly shows the site of rupture.
FIGURE 26–20 The mesosalpinx on the affected side is serially double-clamped with Kelly clamps and incised with Metzenbaum scissors. Each vascular pedicle is suture-ligated in transfixing fashion with 0 Vicryl. When the cornu is reached, a 0 or 1 Vicryl suture is placed deeply beneath the ectopic mass in figure-of-8 fashion. The suture is tagged with a mosquito clamp and left untied.
FIGURE 26–21 The cornual pregnancy is excised after injection with a 1 : 100 or 1 : 200 vasopressin solution. The previously placed figure-of-8 suture is triply tied, producing immediate hemostasis.
FIGURE 26–22 The en bloc excised cornual pregnancy is examined, then is handed off to the nurse.
FIGURE 26–23 Additional but shallower figure-of-8 sutures are placed linearly to gain additional hemostasis and to close the remainder of the incision. A U-shaped suture of 0 Vicryl is placed through the uterine wall at the cornual incision and is brought through the ipsilateral round ligament at its junction with the broad ligament. The net effect of this stitch when tied is to cover the incision with peritoneum and to suspend the uterus on that side.
FIGURE 26–24 Preoperative diagnosis of a ruptured or leaking cornual ectopic pregnancy was made. At laparotomy, a bicornuate uterus with a noncommunicating and ruptured unicornuate uterus was found.
FIGURE 26–25 This view shows the site of rupture to be in the thinned cornu of the unicornuate portion of the bicornuate uterus.
Salpingectomy for Isthmic Ectopic Pregnancy
Isthmic as well as ampullary ectopic pregnancy may be treated by linear salpingostomy, or alternatively by salpingectomy, or even by segmental resection.
Salpingectomy is performed by elevating the oviduct and ovary and serially clamping and suture-ligating the mesosalpinx. The tube can be clamped and cut off at the uterine terminus (Figs. 26–21 through 26–33). The decision to resect the interstitial remnant offers both advantages and disadvantages (Figs 26–34 through 26–36). Resection will eliminate the risk that a future cornual ectopic pregnancy may occur as the result of transmigration of a fertilized ovum but will greatly increase the risk of uterine rupture if a future intrauterine pregnancy should occur.
FIGURE 26–26 The tubal pregnancy site is isolated in the isthmus close to the cornual portion of the oviduct.
FIGURE 26–27 The mesosalpinx is grasped at the fimbrial end of the tube and is doubly clamped with Kelly clamps.
FIGURE 26–28 The maneuver shown in Figure 26-27 is repeated until the tubouterine junction is reached.
FIGURE 26–29 If the cornu is to be resected, a 0 Vicryl figure-of-8 stitch is placed widely and deeply into the area to be resected.
FIGURE 26–30 Vasopressin 1 : 100 solution is injected into the cornua via a 25-gauge needle.
FIGURE 26–31 The tube is cut by a wedging-type excision.
FIGURE 26–32 As the wedge is removed from the cornual portion of the uterus, the figure-of-8 stitch is tightened.
FIGURE 26–33 The figure-of-8 suture is tightened into place, and good hemostasis is seen.
FIGURE 26–34 Additional 0 Vicryl sutures may be placed if needed.
FIGURE 26–35 A knuckle of round ligament is pulled over the incision; it covers the suture line and suspends the operative side of the uterus.
FIGURE 26–36 On completion of the surgical site, ovary, ovarian vessels, ureter, and surrounding intestine are carefully examined while the field is irrigated with sterile saline.