Chapter 78 Surgical Management of Aneurysms of the Vertebral and Posterior Inferior Cerebellar Artery Complex
Aneurysms of the vertebral artery–posterior inferior cerebellar artery (VA-PICA) complex originate from any portion of the intradural VA up to the vertebrobasilar junction and from one of the five PICA segments. During the past decade, the treatment of these aneurysms became more sophisticated due to significant developments in diagnostic methods, improvements in microsurgical technique, further development of skull base surgery, better understanding of the microsurgical anatomy of the vertebrobasilar arterial territory, and dramatic advances in endovascular therapy. However, despite such continuous improvements, management of these complex lesions remains a challenging task. Several characteristic features distinguish VA and VA-PICA aneurysms from those of the anterior circulation: (1) they are relatively uncommon, occurring approximately one tenth as frequently as aneurysms in the anterior circulation1; (2) they show great variability in size, location, and morphology; the percentage of dissecting and fusiform aneurysms is much higher than in the other intracranial compartments; and (3) most of them are located deeply in the posterior fossa having a close relationship to the lower brain stem, the lower cranial nerves, and the cerebellum, making them difficult to access. The anatomic variability of the VA, the PICA, and the skull base around the jugular tubercle add further to the complexity of these lesions and increase the risk of their management. The infrequency of these lesions is the main reason why many neurosurgeons have only limited personal experience with the surgical treatment of VA-PICA aneurysms. With the advent of modern endovascular therapy, the number of lesions available for surgery, particularly the number of less complex VA and VA-PICA aneurysms, has further decreased, a situation that also raises problems in neurosurgical training. On the other hand, recent treatment strategies have gradually changed toward combined endovascular and surgical management, especially in the acute phase of severe subarachnoid hemorrhage (SAH) or in high-risk patients. It is obvious that only a limited number of specialized neurovascular centers can offer sufficient expertise for the safe management of this subgroup of vascular lesions.
Epidemiology
Aneurysms of the VA-PICA complex comprise 0.5% to 3% of all intracranial aneurysms.2–6 Approximately two thirds of these aneurysms are located at the bifurcation of the VAPICA junction, whereas distal PICA aneurysms account for approximately 0.3% to 1% of all aneurysms.6–8 In a recently published series of 24 patients, distal PICA aneurysms accounted for only 0.3% of all intracranial aneurysms and for 3.7% of the vertebrobasilar lesions; 74% were saccular, 7% were fusiform, and 19% were dissecting.7 Until 1992, only 140 patients harboring an aneurysm of the VA-PICA complex were reported in the literature9; of these, approximately 75% were VA or VA-PICA and 25% were distal PICA aneurysms. Multiple occurrence was occasionally reported.4,10–13 Although the incidence of aneurysms arising in association with arteriovenous malformations may be as high as 46%, the combination of a VA-PICA aneurysm and an arteriovenous malformation is rarely reported in the literature.14–16 With 85%, there is a clear predominance of female patients,4,5,17,18 even more notable in saccular aneurysms.19 Patients of virtually all ages may be affected, with an average age of 49.3 years.20
Aneurysm Characteristics
In contrast to intracranial aneurysms of other locations, only approximately 60% of VA-PICA aneurysms are saccular; approximately 30% are dissecting and 10% fusiform.9,21,22 In Yamaura’s18 series, there were 60% saccular, 27% dissecting, and 13% arteriosclerotic fusiform aneurysms; moreover, he found three giant lesions with a diameter exceeding 25 mm and two partially thrombosed saccular aneurysms. Drs. Drake and Peerless and colleagues have treated the world’s largest series of patients with vertebrobasilar aneurysms, comprising 1767 individual patients, of whom 217 (12.3%) harbored aneurysms of the VA-PICA complex.19,20,23 One hundred sixty-six lesions were saccular (76.5%), 25 were dissecting (11%), 18 were fusiform (8%), 4 were atherosclerotic (1.8%), 3 were associated with an arteriovenous malformation (1.3%), and 1 was traumatic (0.4%). The majority (70%) were small (<12 mm); 27 aneurysms (12%) were large (13 to 24 mm) and 40 (18%) were giant (>25 mm). Left-sided origin was more common (55%). Forty-three aneurysms (19%) were unruptured.19,23
Fusiform aneurysms appear as spindle-shaped dilatations, the vertebrobasilar trunk being the most frequent location for fusiform aneurysms.24 Due to a clear difference in natural history and optimal therapy, they must be clearly distinguished from dissecting aneurysms. More than two decades ago, nontraumatic dissecting aneurysms were considered to be extremely rare. However, improved neuroradiologic imaging techniques have demonstrated such lesions with increasing frequency, and during the past years, this type of aneurysm has received great attention in the pertinent literature.10,22,25 On arteriography, such aneurysms appear as a saccular or spindle-shaped vascular dilatation, occasionally combined with proximal stenosis. The classic arteriographic features of dissecting arteries include the double-lumen sign, retention of contrast medium, the pearl-and-string sign,26 and focal outpouching.22,27 Usually, they are not related to vascular branches of the VA. Such dissecting aneurysms of the VA may occur proximal as well as distal to the origin of the PICA, but occasionally they may involve the origin of the PICA as well.28 Yasui and colleagues29 believe that a fusiform VA aneurysm is one predisposing condition for a dissecting lesion. The sudden disruption of the internal elastic lamina is the primary mechanism underlying the development of dissecting aneurysms. The plane of dissection extends through the media, and most aneurysms have one entrance to this pseudolumen.30 Dissecting aneurysms of the VA often cause SAH by rupture of the adventitia and present a high risk of rebleeding.28,31,32 These lesions are not confined to the VA but may be observed on the distal PICA as well.7,33,34 Occasionally, a dissecting distal PICA aneurysm can develop as a traumatic lesion.35
Extreme dilations of the VA, termed “dolichoectasias,” occur less frequently and are usually difficult to treat. The involved artery is elongated and tortuous. On histologic examination, large defects within the muscular and elastic lamina can be detected and sometimes also extensive arteriosclerotic changes.30 Although dissecting aneurysms occur more frequently in male patients of younger age, dolichoectasias occur more frequently in the seventh decade.9,22,36,37
Historical Background
According to Hudgins and colleagues,4 the first case description of a saccular VA-PICA aneurysm was given by Cruveilhier in 1829. Rizzoli and Hayes38 were the first to surgically treat such an aneurysm in 1947 by interrupting the parent artery with two silver clips. Interestingly, the aneurysm was detected by these authors on a ventriculogram that showed a displaced fourth ventricle. Lewis and colleagues33 mentioned that the first case of an aneurysm arising from the distal segment of the PICA was reported in 1864 by Fernet and that the first surgical treatment of a peripheral PICA aneurysm is accredited to Olivecrona. In the 1950s and 1960s, vertebrobasilar aneurysms were associated with the highest mortality rate.39 Rizzoli and Hayes38 treated a peripheral PICA aneurysm with trapping in 1953. Uihlein and Hughes40 described in 1955 the nonsurgical treatment of 14 patients harboring a posterior fossa aneurysm; eight of these patients died after the aneurysm ruptured. After the introduction of routine vertebral angiography in patients with SAH, such aneurysms were detected with increasing frequency. In 1958, Desaussure and colleagues41 reported the successful surgical obliteration of two PICA aneurysms found on vertebral angiograms. Further improvements of neuroradiologic techniques after the introduction of transfemoral catheter and subtraction angiography as well as the routine use of microsurgical techniques in neurosurgery have dramatically improved the outcome of surgical procedures for treatment of vertebrobasilar aneurysms.42,43
Neuroradiologic Imaging
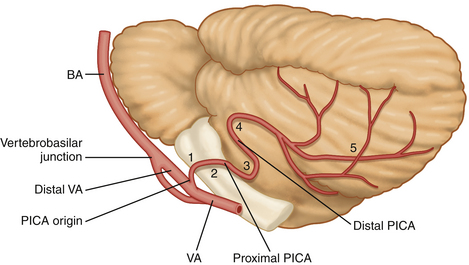
A meticulous preoperative neuroradiologic assessment is indispensable for successful treatment of VA and VA-PICA aneurysms. Neuroradiologic investigations should clarify the following features: (1) the exact location and origin of the aneurysm with respect to the VA and the various segments of the PICA (Fig. 78-1); (2) the size, shape, extent, and limits of the lesion to differentiate between saccular, fusiform, and dissecting aneurysms; (3) the orientation of the neck and the dome of the aneurysm; (4) the presence or absence of sufficient collateral circulation; (5) the patency of both VAs and the dominance of one of them, if present; (6) the presence or absence of multiple intracranial aneurysms or an associated arteriovenous malformation; (7) the precise relationship to the major surrounding anatomic structures as well as the degree of involvement of the brain stem and rootlets of the lower cranial nerves; and (8) the presence of hydrocephalus and/or intracerebellar/intraventricular hemorrhage.
Neuroradiologic studies include high-quality arterial digital angiography as well as various techniques of coronal, sagittal, and axial magnetic resonance imaging, and computed tomography (CT). Digital subtraction angiography may be complemented by rotational angiography with 3-dimensional rendering. Yonekawa and colleagues44 described three distances that can be measured on preoperative angiograms that are important predictors of the difficulty of operative access to VA-PICA aneurysms: the distance of the aneurysm from the midline, the distance from the most lateral point of the foramen magnum, and the distance from the clivus. According to these authors, optimal results are obtained when these distances are more than 5 to 10 mm, less than 10 to 21 mm, and less than 13 mm, respectively.
In a previous communication, we emphasized that high-resolution CT using a bone tissue algorithm is most useful to demonstrate the configuration of the skull base around the jugular foramen, in particular showing the size and shape of the jugular tubercle, the size of the posterior condylar canal, and the distance between the dural entrance of the vertebral artery and the hypoglossal canal or jugular tubercle.45 Special sections or 3-dimensional reconstructions may further add to the understanding of the individual skull base configuration or presence of bony anomalies. When performed with a bolus of contrast medium, this 3-dimensional CT image may demonstrate the relationship between the lesion, brain stem, and skull base, adding important information required for the planning of the procedure.45 Huynh-Le and colleagues46 have confirmed the utility of 3-dimensional CT angiography for the surgical management of VA-PICA aneurysms; this diagnostic technique was most valuable in demonstrating not only the exact site and shape of the aneurysm but also the relationships between parent vessel and malformation on the one side and the bony structures of the skull base on the other side. CT is important to demonstrate the SAH, the blood distribution within the basal cisterns, an associated hydrocephalus, and an intraventricular or intracerebellar hemorrhage. Intraventricular hemorrhage is present in as many as 82% of patients and associated hydrocephalus in approximately 75% of patients with ruptured aneurysms.5,47,48 Magnetic resonance imaging is particularly valuable in fusiform, dissecting, or partially thrombosed aneurysms.30,49 Magnetic resonance angiography can depict the aneurysm in relation to the brain stem, cerebellum, caudal cranial nerves, and skull base.
Clinical Presentation
The most frequent presenting symptom of patients with aneurysms of the VA-PICA complex is SAH. Rupture of these aneurysms occurs similarly to the rupture of aneurysms of the anterior circulation. However, the clinical consequences are far more disastrous. Although only a few patients experience intracerebellar hemorrhage or deficits of caudal cranial nerves, in some instances, prolonged coma, hemiparesis, or pulmonary embolism can occur.50,51 Aneurysm rupture occurs more frequently in lesions smaller than 12 mm. Large and giant aneurysms rarely rupture; they become symptomatic more frequently by their compressive effect on the lower brain stem or the caudal cranial nerves. Ischemic complications such as Wallenberg’s syndrome may occur in dissecting aneurysms due to occlusion of perforating arteries that supply the lateral aspect of the medulla. Patients with dolichoectatic VA and/or basilar artery may have ischemic stroke, brain stem compression, and occasionally hemifacial spasm or trigeminal neuralgia.52 In the series of Drake and Peerless53 of 221 patients, 178 had SAH (80.5%). Sixth nerve palsy, not lower cranial nerve paresis, was the most frequent preoperative cranial nerve dysfunction, as one might have expected. It was nearly always associated with SAH and recovered in 75% completely.
Management
The decision as to whether an aneurysm of the VA-PICA complex should be treated, as well as the timing and choice of treatment modality in case treatment appears indicated, depends on criteria such as the patient’s age, actual clinical condition, and neurologic status; progression or resolution of initial symptoms and signs; presence or absence of SAH; the interval between SAH and time of decision making; aneurysm characteristics; medical history; and the presence or absence of hydrocephalus and intraventricular or intracerebellar hemorrhage. Surgery, for instance, is preferable when a significant hematoma needs to be evacuated. For more than a decade, the concomitant availability of endovascular and microsurgical procedures has made possible a multimodal treatment of aneurysms of the VA-PICA complex.54–57 Particularly, the technologic achievements in neurovascular instrumentation (i.e., coil technology, intracranial stent technique) of the recent years led to a continuing challenge for interventional neuroradiologists, enabling them to treat even previously “untreatable” aneurysms with a high success rate.58–66 However, complications of the treatment such as brain stem infarction and hemorrhages are also reported for the interventional therapy of VA-PICA aneurysms.61,67,68 For some rare complex cases, a combined interventional and microsurgical therapy may constitute a reasonable solution.58
In some aneurysms such as proximal PICA lesions, even in cases in which endovascular coil occlusion of the aneurysms seems possible, the direct microsurgical inspection of the affected segment of the PICA and of perforating brain stem-supplying arteries may offer significant advantages compared with endovascular therapy.33 Considering the complexity and heterogeneity of VA and VA-PICA aneurysms, most lesions might require an individual case-by-case decision.
Surgical Approaches
To expose aneurysms of the VA-PICA complex surgically, a detailed analysis of aneurysm location, origin, extension, and orientation of the dome is necessary. Small saccular VA-PICA aneurysms may be exposed by a traditional suboccipital medial or lateral approach when they are located proximal to the rootlets of the lower cranial nerves. Aneurysms located more distally or even at the vertebrobasilar junction, as well as large or giant saccular or complex dissecting aneurysms, may require more extensive skull base approaches. Aneurysms of the third, fourth, and fifth PICA segments are best visualized via a suboccipital medial craniotomy. The patient is placed in either the sitting or prone position with the head flexed. The craniotomy includes the posterior rim of the foramen magnum. A number of lateral approaches are available to expose various aneurysms of the VA or the first two PICA segments.2,9,69–72 For exposure of some proximal VA aneurysms, a traditional retrosigmoid approach may be sufficient.73 However, several authors have underscored the necessity of extending the exposure more laterally.69 The retrolabyrinthine transsigmoidal approach was described by Giannotta and Maceri74 in 1988 and used to expose distal VA-PICA aneurysms or those of the vertebrobasilar junction.
It is a complex and more time-consuming skull base approach because large portions of the petrous bone must be drilled away and the ipsilateral sigmoid sinus is ligated, provided the contralateral sinus is intact. This approach, however, is rarely described in the literature for treatment of aneurysms of the VA-PICA complex. The transcondylar approach and several variations have been widely used by several authors in this context.33,75–79 A detailed description of the technique as we use it is given later in this chapter. Aneurysms that are not suitable for either surgical clipping or endovascular procedure may require other surgical techniques such as coating,5,80 external (surgical) trapping,4 or one of the various procedures of revascularization.
Saccular Aneurysms
Hernesniemi81 mentioned that most saccular nongiant aneurysms of the VA-PICA complex can be clipped. Today, most authors prefer an early treatment of these aneurysms after rupture, including distal PICA aneurysms,33 and also when they are associated with an arteriovenous malformation.15,82 The decision as to whether surgical clipping or endovascular coil occlusion is preferable should be made by an experienced neurovascular team. In the series of Horiuchi and colleagues7 comprising 27 PICA aneurysms in 24 patients, 22 lesions were clipped (81%), 2 (7%) were wrapped, 1 (4%) was proximally ligated with occipital artery-PICA bypass, and only 1 (4%) was occluded endovascularly with Guglielmi detachable (GD) coils.
Dissecting Aneurysms
With modern neuroimaging techniques, the diagnosis of dissecting aneurysms is now more precise than in the past.49,83 Although a benign course has occasionally been documented,84 the necessity of early treatment of dissecting aneurysms of the VA has been emphasized by many authors. An SAH from a dissecting aneurysm is considered a neurosurgical emergency because of a high incidence of rebleeding and a high mortality rate at the time of recurrent bleeding.22,30,31,55 Conversely, the natural history of non-SAH cases is relatively benign and therefore the treatment remains controversial.85–87 Despite early satisfactory results with a proximal occlusion of the VA,88 it is now well recognized that proximal occlusion of the affected VA by clip placement or endovascular procedure may not be sufficient.28 The primary goal of therapy is thus complete exclusion of the dissecting aneurysm from the circulation to avoid progression of the vascular dissection or a distal embolism with ischemic complications.28 In most cases, clip occlusion is impossible and wrapping alone may not be efficient.83 Test occlusion of the vertebral artery is performed, and thereafter either surgical or endovascular occlusion (internal trapping) is recommended.54 According to Hamada and colleagues,28 when occlusion of the VA is chosen as treatment option, patients should undergo a 20-minute occlusion tolerance test using a nondetachable balloon. Yoshimoto and Wakai87 have questioned the necessity of this balloon test because they doubt its reliability; these authors believe that definitive unilateral VA occlusion can be performed safely unless the contralateral VA is hypoplastic. Kitanaka and colleagues89 have mentioned that the choice of surgical technique depends on the location of the dissecting aneurysm in relation to the origin of the PICA. The VA can usually be occluded distal to the PICA origin, whereas a proximal occlusion of the VA may cause a secondary thrombosis of the PICA. A number of revascularization techniques have therefore been applied to occlude the VA with a consecutive reanastomosis of the PICA: PICA-PICA bypass at the level of the caudal loop,90–92 occipital artery-PICA,93–98 VA-PICA anastomosis with the superficial temporal artery or radial artery,99–101 and VA-PICA transposition.102
Giant Aneurysms
Despite the rare occurrence of giant aneurysms of the posterior circulation, these lesions have received much attention in the literature.11,103–106
The reasons for their frequent description are special characteristics of these lesions. The therapy of giant aneurysms is far more difficult that of those in the anterior circulation. Ausman and colleagues93 have recommended surgical clip occlusion in cooperation with cardiosurgeons under hypothermia and circulatory arrest.107 This method, however, has a specific morbidity and is associated with a certain mortality. The optimal therapy of giant aneurysms is the direct clip occlusion, which still bears a high risk for the patient. For this reason, the parent artery (VA) may be deliberately sacrificed or endovascularly occluded,108 the same technique as that used for dissecting or fusiform aneurysms. According to Inamasu and colleagues109 who treated six patients with giant VA and four patients with VA-PICA aneurysms surgically, more favorable results were obtained with surgical or endovascular rather than with conservative therapy.
The Authors’ Series
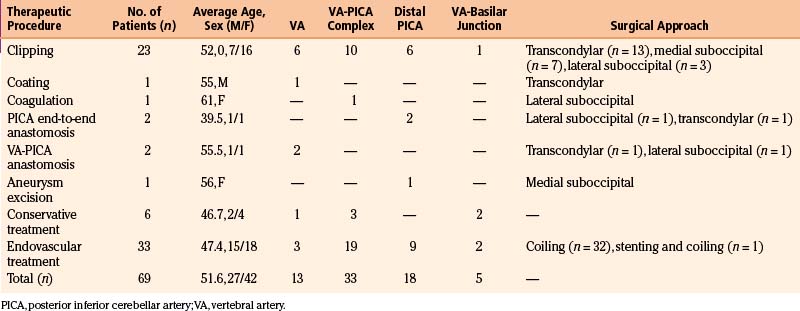
A total of 69 patients with aneurysms of the VA-PICA complex were treated in the period 1992 to 2004. Thirty patients were treated surgically, 33 endovascularly and 6 conservatively. Patient data are summarized in Table 78-1.
Surgical Anatomy
The origin of the PICA at the VA varies from extradurally, below the foramen magnum, to the vertebrobasilar junction. The PICA arises from the posterior or lateral surfaces of the VA more often than from the anterior or medial surfaces.110 The PICA is the artery with the most complex relationship to the cranial nerves of any artery.111 By definition, the PICA originates from the VA. Although rarely encountered (5%), one must bear in mind the possibility of an extradural origin of the PICA and of an extracranial (intradural) site of distal PICA aneurysms.110,112 In a few cases, the VA and the PICA are missing. If the PICA is present, it is the largest branch of the VA.110 Lister and colleagues113 have divided the artery into five segments based on its relationship to the medulla and the cerebellum. These five segments are the anterior medullary, the lateral medullary, the tonsillomedullary (includes the caudal loop), the telovelotonsillar (includes the cranial loop), and the cortical.113 Each segment sometimes includes more than one trunk. The PICA is closely related to the cerebellomedullary fissure, the inferior half of the ventricular roof, the inferior peduncle, and the suboccipital surface.110 The PICA supplies perforating branches to the medullar, choroidal arteries and cortical arteries. Perforating arteries arise from the medullary segment terminating into the brain stem.110 Recently, Marinkovic and colleagues114 gave a detailed description of the perforating branches of the VA providing valuable information for those performing aneurysm surgery in this region.
The upper portion of the sternocleidomastoid muscle and its posterior border indicate the region for the skin incision and further muscular opening. The most important muscles of the deep layer are the rectus capitis posterior major and minor muscles and the superior and inferior oblique muscles. The area between the medial rim of the superior oblique muscle, the upper rim of the inferior oblique muscle, and the lateral rim of the rectus capitis posterior major muscle, called the suboccipital triangle, contains the posterior rim of the atlantal arch, the horizontal portion of the vertebral artery, and the C1 root between these two structures. The posterior atlantal arch also serves as an important landmark for early localization of the VA during the stage of muscular dissection. Once this structure has been identified by palpation, the artery can readily be exposed in the sulcus dorsal and medial to the lateral atlantal mass. A C1 hemilaminectomy may not always be necessary but can be helpful when mobilization of the VA is required. The posterior edge of the occipital condyle is located just lateral to the dural entrance of the VA. To better expose the proximal intradural VA, this portion of the occipital condyle must be drilled away.
The diameter of the posterior condylar canal that contains the posterior condylar emissary vein varies widely. This canal is a very important landmark because it opens into the posteromedial margin of the jugular foramen and indicates the direction of bony drilling to expose the jugular tubercle. The jugular tubercle is a rounded prominence located at the junction between the basal part (clivus) and the condylar part of the occipital bone (jugular process). The jugular tubercle is one of the most important landmarks being surrounded by a number of vital neurovascular structures that must be exposed partially or totally.45,77 Medially and superiorly, the jugular tubercle is overcrossed by the cranial nerves IX, X, and XI intradurally. Laterally, the jugular tubercle has a close relationship with the jugular bulb, reaching the medial wall of the jugular foramen. Inferiorly, there is the hypoglossal canal containing the hypoglossal nerve surrounded by its venous plexus. Seeger115 was the first to document the necessity of resecting the jugular tubercle for an adequate visualization of near-midline aneurysms of the VA-PICA complex, later underscored by Perneczky.116
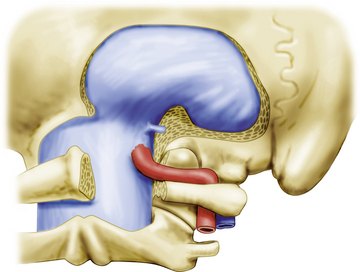
Exposure of the Deep Lateral Suboccipital Region
Basically, we have to deal with two muscular layers. The superficial muscle layer consists of the sternocleidomastoid and the splenius capitis muscles laterally, and the trapezius and the semispinalis capitis muscles medially. The occipital artery encountered either superficial or deep to the longissimus capitis and deep to the splenius capitis muscles is usually ligated and divided but may be preserved in case an occipital artery-PICA bypass is deemed necessary. From the deep muscle layer, the two oblique and the two rectus capitis posterior muscles deserve special attention. We start with freeing the attachment of the superficial and partially the deep muscles between the superior and inferior nuchal lines by using monopolar thermocautery. This instrument can be safely applied in this area when the tip of the instrument is permanently visualized and kept in contact with the occipital bone. The muscles are then divided in a craniocaudal direction layer by layer, as much as possible respecting the direction of the muscle fibers. Frequently, palpating the deep structures is helpful for avoiding injury to the VA, which sometimes may form a posterior loop that extends beyond the level of the atlantal arch. The surgeon should recognize this anatomic variation before surgery by carefully examining axial magnetic resonance imaging or CT slices taken at the C1 level. Instead of anatomically exposing the three suboccipital muscles that form the suboccipital triangle by extensive dissection, we prefer to identify the posterior arch of the atlas by palpation. The atlantal arch is then freed from its periosteal sheath using a sharp dissector, and the sulcus of the VA is thus exposed. The sulcus can easily be identified by observing the shape of the posterior rim of the atlantal arch. This structure is thick in its medial portion, changing into a thin and sharp osseous edge at the level of the sulcus more laterally. As the VA is surrounded by a venous plexus that may cause severe bleeding, it is advisable to identify the vessel at this stage by palpating its pulsations. Once the VA is identified, further detachment of the suboccipital muscles is continued and the posterior condylar fossa containing abundant fatty tissue is exposed together with the posterior aspect of the atlanto-occipital joint. It has proved favorable to perform this step under the operating microscope. The periarterial venous plexus may be coagulated or packed with collagen or Surgicel to control venous bleeding. Muscle and dural branches of the VA are coagulated and divided. Care is paid to the C1 root located beneath the horizontal portion of the VA. The fatty and connective tissue filling the condylar fossa is gradually removed and the posterior portion of the occipital condyle and lateral atlantal mass are exposed by subperiosteal dissection. When exposing the condylar fossa, the posterior condylar emissary vein is dissected free, coagulated, and then divided sharply. The remaining distal portion of the vein located within the posterior condylar canal is shrunk with bipolar forceps and serves as an important anatomic landmark, indicating the direction toward the posterior aspect of the jugular bulb (Fig. 78-2).
Suboccipital Craniectomy
Usually, we either perform a small bone flap or place several burr holes and preserve the bone dust for later wound closure. After placing the burr holes, the dura is gently detached from the bone. Craniectomy is continued step by step using a rongeur to preserve the bony fragments. The limits of the craniectomy are as follows: superiorly approximately 1 to 2 cm below the transverse sinus; medially and superiorly approximately 1 to 2 cm from the midline; medially and inferiorly the dorsolateral rim of the foramen magnum is completely opened from the midline to the dural entrance of the VA, thus reaching the posterior condylar fossa and posterior medial aspect of the jugular process; and laterally to the medial rim of the sigmoid sinus. This stage of the procedure is carried out without the aid of the operating microscope (see Fig. 78-2).
Partial Drilling of the Occipital Condyle and Jugular Tubercle
Because drilling around the jugular foramen is a highly demanding procedure, it is carried out extradurally with the aid of a high-speed drill and under magnification. Before drilling, however, we gently separate the bone from the adjacent dura mater and distal sigmoid sinus that may firmly adhere to the bone. In the early stage, a cutting burr is used that never touches the dura. Thereafter, we use diamond burrs of different sizes under continuous irrigation with saline solution. Drilling begins with removing the medial aspect of the posterior wall of the distal sigmoid sinus and continues to the medial aspect of the jugular process of the occipital bone. At this stage, the point where the VA pierces the dura serves as an important landmark. By measuring the distance from this point to the area of drilling in the depth, we can estimate the remaining distance to the hypoglossal canal and jugular tubercle as known from preoperative neuroradiologic studies. To expose the dura lateral to the point of entrance of the VA, the posteromedial aspect of the occipital condyle is gradually removed, leaving the vast majority of the articular surface intact. Venous bleeding from the marginal sinus at the level of the foramen magnum is controlled with bipolar coagulation and packing with Surgicel. While using the high speed drill in this region, the VA is protected from damage with the suction tube or a self-retaining brain retractor. Drilling is continued to expose the posterior aspect of the hypoglossal canal. Because the dural sheet of the hypoglossal nerve is surrounded by a venous plexus, the exposure may require packing with Surgicel to achieve hemostasis. Once the hypoglossal canal is exposed, the dura overlying the jugular tubercle is gently detached. In many instances, the jugular tubercle is a very high prominence. In such cases, this structure hampers visualization of the distal VA. To obtain a wide exposure, this bony structure is drilled partially or totally, depending on the specific anatomic situation and microsurgical requirements. Occasional bleeding from the jugular bulb or venous channels draining into the bulb is controlled by packing small amounts of Surgicel, and, if necessary, fibrin glue is applied as well. It has proved advantageous to drill the cancellous bone until a thin shallow of cortical bone remains in place. This shallow is then removed piece by piece with a small rongeur. Such a technique is crucial to avoid injury to the jugular bulb or cranial nerves that traverse the jugular foramen. The skull base surgeon working in this area must bear in mind that the wall of the jugular bulb and also the dura overlying the jugular tubercle are thin and very vulnerable structures. Damaging the dura around the jugular tubercle may cause injury to the cranial nerves IX, X, and XI located immediately above this bony prominence or even premature aneurysm rupture. To avoid by all means such damage at this stage, we use very cautiously a conventional drill at low speed.
To enlarge the exposure, in most cases only small amounts of the occipital condyle must be drilled away in the posteromedial portion of this structure. We have always been able to preserve the function of the atlanto-occipital joint (see Fig. 78-2).
Dural Incision
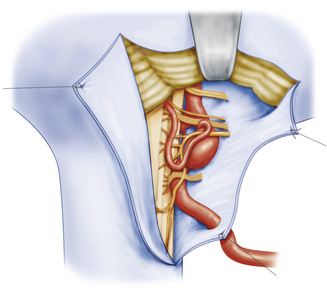
The dura is opened in a longitudinal or Y-shaped fashion, usually medial to the dural entrance of the VA. The dural ring around the VA is left intact save for the cases with proximal artery involvement. Opening the dura exposes the lobulus biventer of the cerebellum rostrally and the medulla oblongata caudally. The dural edges are sutured to the muscles in the vicinity so that the dural entrance of the VA is gently reflected laterally together with the dura. This becomes possible only after sufficient resection of bone lateral to the dural entrance of the VA (Fig. 78-3).
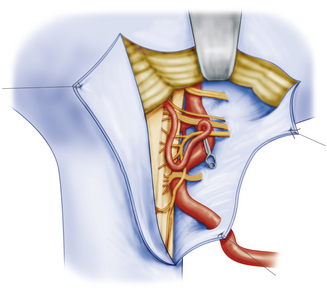
Intradural Stage
The intradural procedure begins with opening the arachnoid membrane of the great cistern. Gentle elevation of the cerebellum gradually exposes the spinal root of the accessory nerve, the proximal intradural portion of the VA, the proximal PICA, the first dentate ligament, and the C1 root. To further retract the cerebellum, the arachnoid around cranial nerves IX through XI must be divided using microscissors. The rootlets of the caudal cranial nerves are then dissected free up to their origin from the antero-olivary and retro-olivary grooves. Anterior to these rootlets, the distal portion of the VA is visualized. The artery and aneurysm may be covered by the rootlets of the hypoglossal nerve, which may cross the PICA anteriorly as well as posteriorly. Close to the midline, the sixth nerve and the junction of both VAs become visible. Superior to the glossopharyngeal nerve, the exit zone of the statoacoustic and more anteriorly of the facial nerve can be seen. However, these anatomic structures may be covered, distorted, or displaced by the underlying aneurysm (Fig. 78-4).
Aneurysms located at the level of the jugular tubercle, such as proximal aneurysms of the VA at the origin of the PICA or true PICA aneurysms located at the anterior or posterior medullary portion of this artery, were readily visualized with this technique. Apart from sufficient exposure of the vascular malformation, it was of great importance to obtain enough control of the VA distal to the aneurysm. Sufficient drilling of the jugular tubercle from extradurally was essential in these particular cases. Before applying an aneurysm clip, the rootlets of the lower cranial nerves including the 12th nerve were dissected free from the vascular malformation. After complete arachnoidal dissection, clipping was performed through a corridor between these rootlets. Only rarely, temporary clipping of the proximal and distal VA and/or PICA was necessary, usually to minimize the inner luminal pressure and shrink a larger aneurysm dome before definitive clipping. Dissecting aneurysms were wrapped or coated by either muscle or cottonoids. Before, during, and after aneurysm clipping, we routinely used a micro-Doppler probe for the control of vascular patency (see Fig. 78-4).
Clinical Outcome and Perioperative Morbidity and Mortality
Both intra- and peri-operative conditions might influence the long-term outcome of patients. Intraoperatively, aneurysm rupture, perforating vessel injury, inadvertent arterial occlusion, or an inadequate arterial hypotension might cause postoperative new deficits. Perioperatively, a postoperative hematoma, postoperative significant vasospasm, rebleeding from a treated aneurysm, septicemia, meningitis, and bleeding diathesis were observed as negative outcome predictors along with further intensive care-related complications such as respiratory insufficiency or pulmonary embolism. However, most patients can be managed without such problems and thus can expect a favorable outcome.45,71,117,118 Even for complex VA-PICA aneurysms, good or excellent clinical results predominate in the larger surgical series.33,34,45,71,78,117,118 One of the key issues for the management of these difficult lesions is the maintenance of cranial nerve function, which remains a challenging microsurgical problem during the treatment of VA-PICA aneurysms. In all major series, the most common postoperative neurologic deficit was a lower cranial nerve malfunction that can be observed in as many as 60% of the patients.4,5,9,45,51,78,118–120 D’Ambrosio and colleagues118 stated that the occurrence of lower cranial nerve dysfunction might be related to the extension of the approach. Our own data support this assumption.45,78
Severe morbidity or even mortality can be as high as 15% of the patients in the larger series, but is mostly related to a poor preoperative state of the patients.78,117
Illustrative Cases
Case Report 1
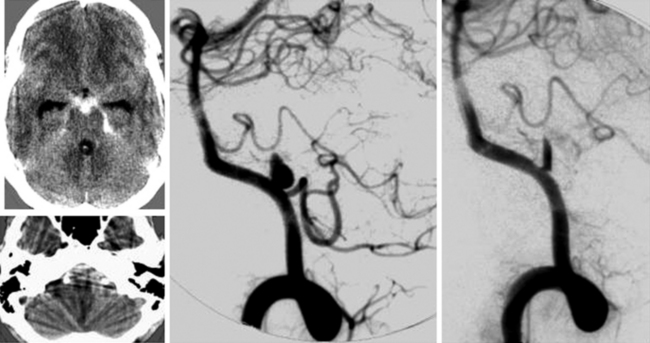
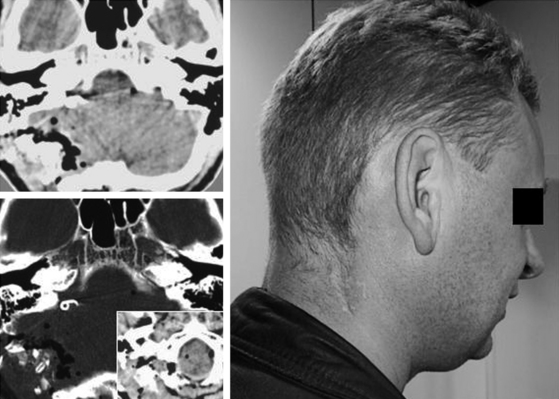
A 37-year-old woman with a history of SAH Hunt and Hess grade III from a left-sided VA-PICA aneurysm was admitted to our department from another hospital primarily for endovascular treatment. During the intervention with a GD coil, both the aneurysm and the anterior medullary segment of the PICA were spontaneously occluded by a thrombus. Local lysis was not attempted due to the risk of rebleeding from the recently ruptured aneurysm. Instead, emergency surgery was carried out, the thrombus was removed, and the aneurysm was successfully clipped with a restored patency of the PICA. Postoperatively, there was no additional morbidity (Figs. 78-5 to 78-7).
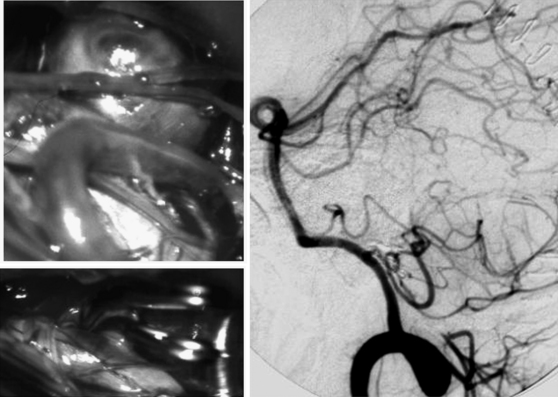
FIGURE 78-6 Intraoperative view and postoperative angiography of the same patient as shown in Fig. 78-5. Upper left: View of the thrombosed aneurysm and distal posterior inferior cerebellar artery (PICA) segment. Lower left: After thrombus removal from the aneurysm and the PICA, the aneurysm is clipped by two curved titanium clips. Right: Postoperative angiography reveals the patency of the PICA.
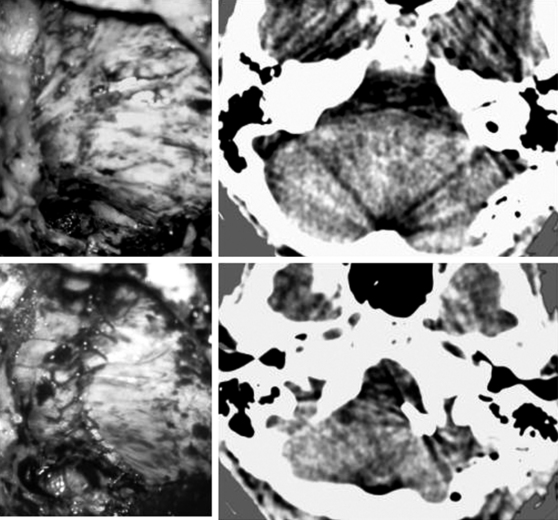
FIGURE 78-7 Intraoperative view and postoperative computed tomography (CT) of the same patient as shown in Figs. 85-5 and 85-6. Upper and lower left: Microscopic view before (upper) dural opening and after (lower) watertight dura closure. Upper and lower right: Postoperative CT shows the approach and clip artifacts (lower).
Case Report 2
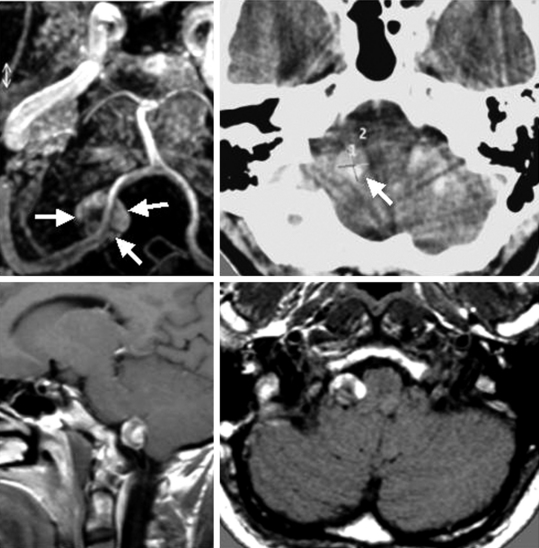
A 37-year-old man was admitted to our hospital with a recent history of occipital headache. Magnetic resonance imaging showed a right perimedullary hyperintense signal compatible with a partially thrombosed aneurysm of the PICA located slightly above the foramen magnum level. Angiography revealed a saccular aneurysm of the tonsillomedullary segment of the right PICA with the dome oriented downward. Endovascular treatment was judged inadequate by the endovascular interventionalist because of the reduced vessel diameter. The aneurysm was surgically exposed via the transcondylar approach and could be clipped successfully after endovascular thrombectomy. Temporary vocal cord paresis occurred postoperatively. No additional cranial nerve deficit was found. The patient returned to work (Figs. 78-8 to 78-11).
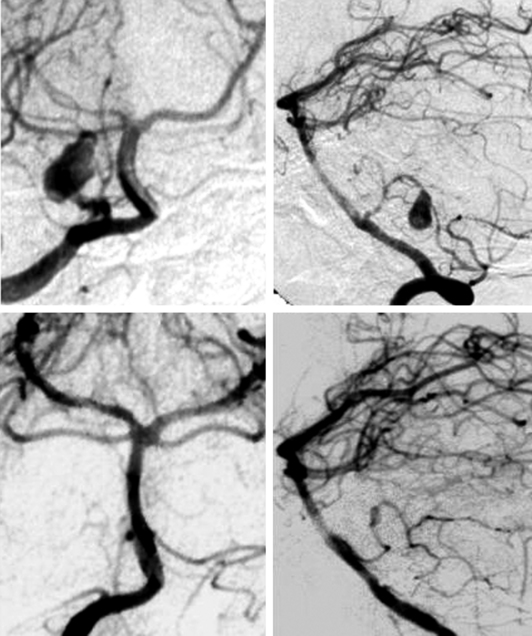
FIGURE 78-9 Pre- and post-operative angiography of the same patient as shown in Fig. 78-5. Angiography before (upper left and right) surgery reveals an aneurysm of the tonsillomedullary segment of the right posterior inferior cerebellar artery that could not be treated by coiling due to the small caliber of the parent vessel. Lower left and right: Postoperative angiography displays the complete clip occlusion of the aneurysm.
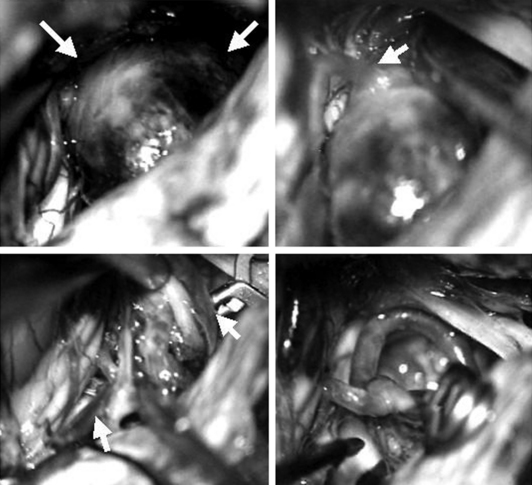
FIGURE 78-10 Intraoperative view of the same patient as shown in Figs. 78-8 and 78-9. The aneurysm was approached by the transcondylar route. Upper left: Aneurysm (arrows) after arachnoidal dissection. Upper right: Vision of the aneurysm neck (arrows). Note that the distal posterior inferior cerebellar artery cannot be observed during this state of dissection because it originates at the back of the aneurysm neck. Lower left: Proximal and distal clipping after (arrows) and removal of a thrombus inside the aneurysm. Lower right: Final clipping with parent vessel reconstruction.
Andoh T., Shirakami S., Nakashima T., et al. Clinical analysis of a series of vertebral aneurysm cases. Neurosurgery. 1992;31:987-993.
Beyerl B.D., Heros R.C. Multiple peripheral aneurysms of the posterior inferior cerebellar artery. Neurosurgery. 1986;19:285-289.
Dernbach P.D., Sila C.A., Little J.R. Giant and multiple aneurysms of the distal posterior inferior cerebellar artery. Neurosurgery. 1988;22:309-312.
Drake C.G. The treatment of aneurysms of the posterior circulation. Clin Neurosurg. 1979;26:96-144.
Drake C.G., Peerless S.J., Hernesniemi J.A. Surgery of Vertebrobasilar Aneurysms. London, Ontario, Experience on 1767 Patients. Vienna: Springer-Verlag; 1996.
Friedman A.H., Drake C.G. Subarachnoid hemorrhage from intracranial dissecting aneurysm. J Neurosurg. 1984;60:325-334.
Gacs G., Vinuela F., Fox A.J., et al. Peripheral aneurysms of the cerebellar arteries. Review of 16 cases. J Neurosurg. 1983;58:63-68.
Hernesniemi J. Clinical and radiographic outcome in the management of posterior circulation aneurysms by use of direct surgical or endovascular techniques. Neurosurgery. 2003;52:1505-1506.
Hernesniemi J. Distal PICA aneurysms. J Neurosurg. 2003;98:1144.
Hiscott P., Crockard A. Multiple aneurysms of the distal posterior inferior cerebellar artery. Neurosurgery. 1982;10:101-102.
Horiuchi T., Tanaka Y., Hongo K., et al. Characteristics of distal posteroinferior cerebellar artery aneurysms. Neurosurgery. 2003;53:589-595.
Hudgins R.J., Day A.L., Quisling R.G., et al. Aneurysms of the posterior inferior cerebellar artery. A clinical and anatomical analysis. J Neurosurg. 1983;58:381-387.
Kai Y., Hamada J.I., Morioka M., et al. Endovascular coil trapping for ruptured vertebral artery dissecting aneurysms by using double microcatheters technique in the acute stage. Acta Neurochir (Wien). 2003;145:447-451.
Kaptain G.J., Lanzino G., Do H.M., et al. Posterior inferior cerebellar artery aneurysms associated with posterior fossa arteriovenous malformation. Report of five cases and literature review. Surg Neurol. 1999;51:146-152.
Kassell N.F., Torner J.C. The International Cooperative Study on Timing of Aneurysm Surgery—an update. Stroke. 1984;15:566-570.
Lee K.S., Gower D.J., Branch C.L.Jr., et al. Surgical repair of aneurysms of the posterior inferior cerebellar artery—a clinical series. Surg Neurol. 1989;31:85-91.
Meisel H.J., Mansmann U., Alvarez H., et al. Cerebral arteriovenous malformations and associated aneurysms. Analysis of 305 cases from a series of 662 patients. Neurosurgery. 2000;46:793-800.
Peerless S.J., Drake C.G. Posterior circulation aneurysms. In: Wilkins R.H., Rengachary S.S. Neurosurgery. New York: McGraw-Hill; 1985:1422-1436.
Rothman S.L., zar-Kia B., Kier E.L., et al. The angiography of posterior inferior cerebellar artery aneurysms. Neuroradiology. 1973;6:1-7.
Shokunbi M.T., Vinters H.V., Kaufmann J.C. Fusiform intracranial aneurysms. Clinicopathologic features. Surg Neurol. 1988;29:263-270.
Tiyaworabun S., Wanis A., Schirmer M., et al. Aneurysms of the vertebrobasilar system. Clinical analysis and follow-up results. Acta Neurochir (Wien). 1982;63:221-229.
Westphal M., Grzyska U. Clinical significance of pedicle aneurysms on feeding vessels, especially those located in infratentorial arteriovenous malformations. J Neurosurg. 2000;92:995-1001.
Yamamoto I., Tsugane R., Ohya M., et al. Peripheral aneurysms of the posterior inferior cerebellar artery. Neurosurgery. 1984;15:839-845.
Yamaura A. Diagnosis and treatment of vertebral aneurysms. J Neurosurg. 1988;69:345-349.
Yamaura A., Watanabe Y., Saeki N. Dissecting aneurysms of the intracranial vertebral artery. J Neurosurg. 1990;72:183-188.
1. Kassell N.F., Torner J.C. The International Cooperative Study on Timing of Aneurysm Surgery—an update. Stroke. 1984;15:566-570.
2. Drake C.G. The treatment of aneurysms of the posterior circulation. Clin Neurosurg. 1979;26:96-144.
3. Friedman A.H., Drake C.G. Subarachnoid hemorrhage from intracranial dissecting aneurysm. J Neurosurg. 1984;60:325-334.
4. Hudgins R.J., Day A.L., Quisling R.G., et al. Aneurysms of the posterior inferior cerebellar artery. A clinical and anatomical analysis. J Neurosurg. 1983;58:381-387.
5. Lee K.S., Gower D.J., Branch C.L.Jr., et al. Surgical repair of aneurysms of the posterior inferior cerebellar artery—a clinical series. Surg Neurol. 1989;31:85-91.
6. Peerless S.J., Drake C.G. Posterior circulation aneurysms. In: Wilkins R.H., Rengachary S.S. Neurosurgery. New York: McGraw-Hill; 1985:1422-1436.
7. Horiuchi T., Tanaka Y., Hongo K., et al. Characteristics of distal posteroinferior cerebellar artery aneurysms. Neurosurgery. 2003;53:589-595.
8. Yamamoto I., Tsugane R., Ohya M., et al. Peripheral aneurysms of the posterior inferior cerebellar artery. Neurosurgery. 1984;15:839-845.
9. Andoh T., Shirakami S., Nakashima T., et al. Clinical analysis of a series of vertebral aneurysm cases. Neurosurgery. 1992;31:987-993.
10. Beyerl B.D., Heros R.C. Multiple peripheral aneurysms of the posterior inferior cerebellar artery. Neurosurgery. 1986;19:285-289.
11. Dernbach P.D., Sila C.A., Little J.R. Giant and multiple aneurysms of the distal posterior inferior cerebellar artery. Neurosurgery. 1988;22:309-312.
12. Gacs G., Vinuela F., Fox A.J., et al. Peripheral aneurysms of the cerebellar arteries. Review of 16 cases. J Neurosurg. 1983;58:63-68.
13. Hiscott P., Crockard A. Multiple aneurysms of the distal posterior inferior cerebellar artery. Neurosurgery. 1982;10:101-102.
14. Kaptain G.J., Lanzino G., Do H.M., et al. Posterior inferior cerebellar artery aneurysms associated with posterior fossa arteriovenous malformation. Report of five cases and literature review. Surg Neurol. 1999;51:146-152.
15. Meisel H.J., Mansmann U., Alvarez H., et al. Cerebral arteriovenous malformations and associated aneurysms. Analysis of 305 cases from a series of 662 patients. Neurosurgery. 2000;46:793-800.
16. Westphal M., Grzyska U. Clinical significance of pedicle aneurysms on feeding vessels, especially those located in infratentorial arteriovenous malformations. J Neurosurg. 2000;92:995-1001.
17. Rothman S.L., zar-Kia B., Kier E.L., et al. The angiography of posterior inferior cerebellar artery aneurysms. Neuroradiology. 1973;6:1-7.
18. Yamaura A. Diagnosis and treatment of vertebral aneurysms. J Neurosurg. 1988;69:345-349.
19. Hernesniemi J. Distal PICA aneurysms. J Neurosurg. 2003;98:1144.
20. Drake C.G., Peerless S.J., Hernesniemi J.A. Surgery of Vertebrobasilar Aneurysms. London, Ontario, Experience on 1767 Patients. Vienna: Springer-Verlag; 1996.
21. Tiyaworabun S., Wanis A., Schirmer M., et al. Aneurysms of the vertebrobasilar system. Clinical analysis and follow-up results. Acta Neurochir (Wien). 1982;63:221-229.
22. Yamaura A., Watanabe Y., Saeki N. Dissecting aneurysms of the intracranial vertebral artery. J Neurosurg. 1990;72:183-188.
23. Hernesniemi J. Clinical and radiographic outcome in the management of posterior circulation aneurysms by use of direct surgical or endovascular techniques. Neurosurgery. 2003;52:1505-1506.
24. Shokunbi M.T., Vinters H.V., Kaufmann J.C. Fusiform intracranial aneurysms. Clinicopathologic features. Surg Neurol. 1988;29:263-270.
25. Kai Y., Hamada J.I., Morioka M., et al. Endovascular coil trapping for ruptured vertebral artery dissecting aneurysms by using double microcatheters technique in the acute stage. Acta Neurochir (Wien). 2003;145:447-451.
26. Yonas H., Agamanolis D., Takaoka Y., et al. Dissecting intracranial aneurysms. Surg Neurol. 1977;8:407-415.
27. Waga S., Fujimoto K., Morooka Y. Dissecting aneurysm of the vertebral artery. Surg Neurol. 1978;10:237-239.
28. Hamada J., Kai Y., Morioka M., et al. Multimodal treatment of ruptured dissecting aneurysms of the vertebral artery during the acute stage. J Neurosurg. 2003;99:960-966.
29. Yasui T., Komiyama M., Nishikawa M., et al. Fusiform vertebral artery aneurysms as a cause of dissecting aneurysms. Report of two autopsy cases and a review of the literature. J Neurosurg. 1999;91:139-144.
30. Mizutani T., Aruga T., Kirino T., et al. Recurrent subarachnoid hemorrhage from untreated ruptured vertebrobasilar dissecting aneurysms. Neurosurgery. 1995;36:905-911.
31. Aoki N., Sakai T. Rebleeding from intracranial dissecting aneurysm in the vertebral artery. Stroke. 1990;21:1628-1631.
32. Wakhloo A.K., Lanzino G., Lieber B.B., et al. Stents for intracranial aneurysms. The beginning of a new endovascular era? Neurosurgery. 1998;43:377-379.
33. Lewis S.B., Chang D.J., Peace D.A., et al. Distal posterior inferior cerebellar artery aneurysms. Clinical features and management. J Neurosurg. 2002;97:756-766.
34. Kanou Y., Arita K., Kurisu K., et al. Dissecting aneurysm of the peripheral posterior inferior cerebellar artery. Acta Neurochir (Wien). 2000;142:1151-1156.
35. Schuster J.M., Santiago P., Elliott J.P., et al. Acute traumatic posteroinferior cerebellar artery aneurysms. Report of three cases. Neurosurgery. 1999;45:1465-1467.
36. Berger M.S., Wilson C.B. Intracranial dissecting aneurysms of the posterior circulation. Report of six cases and review of the literature. J Neurosurg. 1984;61:882-894.
37. Tanaka K., Waga S., Kojima T., et al. Non-traumatic dissecting aneurysms of the intracranial vertebral artery. Report of six cases. Acta Neurochir (Wien). 1989;100:62-66.
38. Rizzoli H.V., Hayes G.J. Congenital berry aneurysm of the posterior fossa. Case report with successful operative excision. J Neurosurg. 1953;10:550-551.
39. Richardson A.E. The natural history of patients with intracranial aneurysm after rupture. Prog Brain Res. 1968;30:269-273.
40. Uihlein A., Hughes R.A. The surgical treatment of intracranial vestigial aneurysms. Surg Clin North Am Mayo Clinic. 1955:1071-1083.
41. Desaussure R.L., Hunter S.E., Robertson J.T. Saccular aneurysms of the posterior fossa. J Neurosurg. 1958;15:385-391.
42. Drake C.G. The surgical treatment of vertebral-basilar aneurysms. Clin Neurosurg. 1969;16:114-169.
43. Rand R.W., Jannetta P.J. Micro-neurosurgery for aneurysms of the vertebral-basilar artery system. J Neurosurg. 1967;27:330-335.
44. Yonekawa Y., Kaku Y., Imhof H.G., et al. Posterior circulation aneurysms. Technical strategies based on angiographic anatomical findings and the results of 60 recent consecutive cases. Acta Neurochir Suppl. 1999;72:123-140.
45. Bertalanffy H., Gilsbach J.M., Mayfrank L., et al. Planning and surgical strategies for early management of vertebral artery and vertebrobasilar junction aneurysms. Acta Neurochir (Wien). 1995;134:60-65.
46. Huynh-Le P., Matsushima T., Miyazono M., et al. Three-dimensional CT angiography for the surgical management of the vertebral arteryposterior inferior cerebellar artery aneurysms. Acta Neurochir (Wien). 2004;146:329-335.
47. Kayama T., Sugawara T., Sakurai Y., et al. Early CT features of ruptured cerebral aneurysms of the posterior cranial fossa. Acta Neurochir (Wien). 1991;108:34-39.
48. Yeh H.S., Tomsick T.A., Tew J.M.Jr. Intraventricular hemorrhage due to aneurysms of the distal posterior inferior cerebellar artery. Report of three cases. J Neurosurg. 1985;62:772-775.
49. Iwama T., Andoh T., Sakai N., et al. Dissecting and fusiform aneurysms of vertebro-basilar systems. MR imaging. Neuroradiology. 1990;32:272-279.
50. Duvoisin R.C., Yahr M.D. Posterior fossa aneurysms. Neurology. 1965;15:231-241.
51. Salcman M., Rigamonti D., Numaguchi Y., et al. Aneurysms of the posterior inferior cerebellar artery-vertebral artery complex. Variations on a theme. Neurosurgery. 1990;27:12-20.
52. Day J.D., Giannotta S.L. Surgical Management of vertebro-PICA aneurysms. In: Schmidek H.H., Sweet W.H., et al. Operative Neurosurgical Techniques. Philadelphia: WB Saunders; 1994:1103-1111.
53. Drake C.G., Peerless S.J. Giant fusiform intracranial aneurysms. Review of 120 patients treated surgically from 1965 to 1992. J Neurosurg. 1997;87:141-162.
54. Halbach V.V., Higashida R.T., Dowd C.F., et al. Endovascular treatment of vertebral artery dissections and pseudoaneurysms. J Neurosurg. 1993;79:183-191.
55. Iihara K., Sakai N., Murao K., et al. Dissecting aneurysms of the vertebral artery. A management strategy. J Neurosurg. 2002;97:259-267.
56. Kurata A., Ohmomo T., Miyasaka Y., et al. Coil embolization for the treatment of ruptured dissecting vertebral aneurysms. AJNR Am J Neuroradiol. 2001;22:11-18.
57. Lylyk P., Cohen J.E., Ceratto R., et al. Combined endovascular treatment of dissecting vertebral artery aneurysms by using stents and coils. J Neurosurg. 2001;94:427-432.
58. Ponce F.A., Albuquerque F.C., McDougall C.G., et al. Combined endovascular and microsurgical management of giant and complex unruptured aneurysms. Neurosurg Focus. 2004;17:E11.
59. Rabinov J.D., Hellinger F.R., Morris P.P., et al. Endovascular management of vertebrobasilar dissecting aneurysms. AJNR Am J Neuroradiol. 2003;24:1421-1428.
60. Manabe H., Hatayama T., Hasegawa S., et al. Coil embolisation for ruptured vertebral artery dissection distal to the origin of the posterior inferior cerebellar artery. Neuroradiology. 2000;42:384-387.
61. Levy E.I., Horowitz M.B., Koebbe C.J., et al. Transluminal stent-assisted angioplasty of the intracranial vertebrobasilar system for medically refractory, posterior circulation ischemia. Early results. Neurosurgery. 2001;48:1215-1221.
62. Horowitz M.B., Levy E.I., Koebbe C.J., et al. Transluminal stent-assisted coil embolization of a vertebral confluence aneurysm. Technique report. Surg Neurol. 2001;55:291-296.
63. Barakate M.S., Snook K.L., Harrington T.J., et al. Angioplasty and stenting in the posterior cerebral circulation. J Endovasc Ther. 2001;8:558-565.
64. Rasmussen P.A. Transluminal stent-assisted angioplasty of the intracranial vertebrobasilar system for medically refractory, posterior circulation ischemia. Early results. Neurosurgery. 2001;49:1489-1490.
65. Kremer C., Groden C., Hansen H.C., et al. Outcome after endovascular treatment of Hunt and Hess grade IV or V aneurysms. Comparison of anterior versus posterior circulation. Stroke. 1999;30:2617-2622.
66. Lubicz B., Leclerc X., Gauvrit J.Y., et al. Giant vertebrobasilar aneurysms. Endovascular treatment and long-term follow-up. Neurosurgery. 2004;55:316-323.
67. Sugiu K., Takahashi K., Muneta K., et al. Rebleeding of a vertebral artery dissecting aneurysm during stent-assisted coil embolization. A pitfall of the “stent and coil” technique. Surg Neurol. 2004;61:365-370.
68. Nomura M., Kida S., Kita D., et al. Cerebellar hemorrhage after coil embolization for a ruptured vertebral dissecting aneurysm. Surg Neurol. 2000;53:239-242.
69. Heros R.C. Lateral suboccipital approach for vertebral and vertebrobasilar artery lesions. J Neurosurg. 1986;64:559-562.
70. Pritz M.B. Evaluation and treatment of aneurysms of the vertebral artery. Different strategies for different lesions. Neurosurgery. 1991;29:247-256.
71. Matsushima T., Matsukado K., Natori Y., et al. Surgery on a saccular vertebral artery-posterior inferior cerebellar artery aneurysm via the transcondylar fossa (supracondylar transjugular tubercle) approach or the transcondylar approach. Surgical results and indications for using two different lateral skull base approaches. J Neurosurg. 2001;95:268-274.
72. Matsushima T., Fukui M. Lateral approaches to the foramen magnum. with special reference to the transcondylar fossa approach and the transcondylar approach. No Shinkei Geka. 1996;24:119-124.
73. Pia H.W. Classification and treatment of aneurysms of the vertebrobasilar system. Neurol Med Chir (Tokyo). 1979;19:575-594.
74. Giannotta S.L., Maceri D.R. Retrolabyrinthine transsigmoid approach to basilar trunk and vertebrobasilar artery junction aneurysms. Technical note. J Neurosurg. 1988;69:461-466.
75. Day J.D., Fukushima T., Giannotta S.L. Cranial base approaches to posterior circulation aneurysms. J Neurosurg. 1997;87:544-554.
76. Todaka T., Hamada J., Yano S., et al. Successful clipping of a distal posterior inferior cerebellar artery aneurysm located on the anterior surface of the medulla oblongata—case report. Neurol Med Chir (Tokyo). 2002;42:158-161.
77. Bertalanffy H., Seeger W. The dorsolateral, suboccipital, transcondylar approach to the lower clivus and anterior portion of the craniocervical junction. Neurosurgery. 1991;29:815-821.
78. Bertalanffy H., Sure U., Petermeyer M., et al. Management of aneurysms of the vertebral artery-posterior inferior cerebellar artery complex. Neurol Med Chir (Tokyo). 1998;38(Suppl):93-103.
79. Kawase T., Bertalanffy H., Otani M., et al. Surgical approaches for vertebro-basilar trunk aneurysms located in the midline. Acta Neurochir (Wien). 1996;138:402-410.
80. Chou S.N., Ortiz-Suarez H.J. Surgical treatment of arterial aneurysms of the vertebrobasilar circulation. J Neurosurg. 1974;41:671-680.
81. Hernesniemi J., et alComment on Matsushima T. Surgery on a saccular vertebral artery-posterior inferior cerebellar artery aneurysm via the transcondylar fossa (supracondylar transjugular tubercle) approach or the transcondylar approach. Surgical results and indications for using two different lateral skull base approaches. J Neurosurg. 2001;95:638-640.
82. Perata H.J., Tomsick T.A., Tew J.M.Jr. Feeding artery pedicle aneurysms. Association with parenchymal hemorrhage and arteriovenous malformation in the brain. J Neurosurg. 1994;80:631-634.
83. Nagahiro S., Goto S., Yoshioka S., et al. Dissecting aneurysm of the posterior inferior cerebellar artery. Case report. Neurosurgery. 1993;33:739-741.
84. Pozzati E., Padovani R., Fabrizi A., et al. Benign arterial dissections of the posterior circulation. J Neurosurg. 1991;75:69-72.
85. Kitanaka C., Tanaka J., Kuwahara M., et al. Nonsurgical treatment of unruptured intracranial vertebral artery dissection with serial follow-up angiography. J Neurosurg. 1994;80:667-674.
86. Mokri B., Houser O.W., Sandok B.A., et al. Spontaneous dissections of the vertebral arteries. Neurology. 1988;38:880-885.
87. Yoshimoto Y., Wakai S. Unruptured intracranial vertebral artery dissection. Clinical course and serial radiographic imagings. Stroke. 1997;28:370-374.
88. Fujiwara S., Yokoyama N., Fujii K., et al. Repeat angiography and magnetic resonance imaging (MRI) of dissecting aneurysms of the intracranial vertebral artery. Report of four cases. Acta Neurochir (Wien). 1993;121:123-129.
89. Kitanaka C., Sasaki T., Eguchi T., et al. Intracranial vertebral artery dissections. Clinical, radiological features, and surgical considerations. Neurosurgery. 1994;34:620-626.
90. Lemole G.M.Jr., Henn J., Javedan S., et al. Cerebral revascularization performed using posterior inferior cerebellar artery-posterior inferior cerebellar artery bypass. Report of four cases and literature review. J Neurosurg. 2002;97:219-223.
91. Kakino S., Ogasawara K., Kubo Y., et al. Treatment of vertebral artery aneurysms with posterior inferior cerebellar artery-posterior inferior cerebellar artery anastomosis combined with parent artery occlusion. Surg Neurol. 2004;61:185-189.
92. Nussbaum E.S., Mendez A., Camarata P., et al. Surgical management of fusiform aneurysms of the peripheral posteroinferior cerebellar artery. Neurosurgery. 2003;53:831-834.
93. Ausman J.I., Lee M.C., Klassen A.C., et al. Stroke. What’s new? Cerebral revascularization. Minn Med. 1976;59:223-227.
94. Ausman J.I., Pearce J.E., Vacca D.F., et al. Tandem bypass: occipital artery to posterior inferior cerebellar artery side-to-side anastomosis and occipital artery to anterior inferior cerebellar artery end-to-side anastomosis—a case report. Neurosurgery. 1988;22:919-922.
95. Ausman J.I., Diaz F.G., Mullan S., et al. Posterior inferior to posterior inferior cerebellar artery anastomosis combined with trapping for vertebral artery aneurysm. Case report. J Neurosurg. 1990;73:462-465.
96. Lawton M.T., Hamilton M.G., Morcos J.J., et al. Revascularization and aneurysm surgery. Current techniques, indications, and outcome. Neurosurgery. 1996;38:83-92.
97. Yasui T., Komiyama M., Nishikawa M., et al. Subarachnoid hemorrhage from vertebral artery dissecting aneurysms involving the origin of the posteroinferior cerebellar artery. Report of two cases and review of the literature. Neurosurgery. 2000;46:196-200.
98. Ali M.J., Bendok B.R., Tawk R.G., et al. Trapping and revascularization for a dissecting aneurysm of the proximal posteroinferior cerebellar artery. Technical case report and review of the literature. Neurosurgery. 2002;51:258-262.
99. Ausman J.I., Nicoloff D.M., Chou S.N. Posterior fossa revascularization. Anastomosis of vertebral artery to PICA with interposed radial artery graft. Surg Neurol. 1978;9:281-286.
100. Hamada J., Nagahiro S., Mimata C., et al. Reconstruction of the posterior inferior cerebellar artery in the treatment of giant aneurysms. Report of two cases. J Neurosurg. 1996;85:496-499.
101. Hamada J., Todaka T., Yano S., et al. Vertebral artery-posterior inferior cerebellar artery bypass with a superficial temporal artery graft to treat aneurysms involving the posterior inferior cerebellar artery. J Neurosurg. 2002;96:867-871.
102. Durward Q.J. Treatment of vertebral artery dissecting aneurysm by aneurysm trapping and posterior inferior cerebellar artery reimplantation. Case report. J Neurosurg. 1995;82:137-139.
103. Kurokawa Y., Okamura T., Watanabe K. Transcerebellar thrombectomy for the successful clipping of thrombosed giant vertebral artery-posterior inferior cerebellar artery aneurysm. Case report. Surg Neurol. 1990;33:217-220.
104. Drake C.G. Giant intracranial aneurysms. experience with surgical treatment in 174 patients. Clin Neurosurg. 1979;26:12-95.
105. Sugita K. Microsurgical Atlas. New York: Springer-Verlag; 1985.
106. Sugita K., Kobayashi S., Takemae T., et al. Giant aneurysms of the vertebral artery. Report of five cases. J Neurosurg. 1988;68:960-966.
107. Ausman J.I., Malik G.M., Tomecek F.J., et al. Hypothermic circulatory arrest and the management of giant and large cerebral aneurysms. Surg Neurol. 1993;40:289-298.
108. Steinberg G.K., Drake C.G., Peerless S.J. Deliberate basilar or vertebral artery occlusion in the treatment of intracranial aneurysms. Immediate results and long-term outcome in 201 patients. J Neurosurg. 1993;79:161-173.
109. Inamasu J., Suga S., Sato S., et al. Long-term outcome of 17 cases of large-giant posterior fossa aneurysm. Clin Neurol Neurosurg. 2000;102:65-71.
110. Rhoton A.L.Jr. The cerebellar arteries. Neurosurgery. 2000;47:S29-S68.
111. Katsuta T., Rhoton A.L.Jr., Matsushima T. The jugular foramen. Microsurgical anatomy and operative approaches. Neurosurgery. 1997;41:149-201.
112. Ito K., Tanaka Y., Kakizawa Y., et al. Aneurysm at the posterior inferior cerebellar artery of extradural origin for preoperative evaluation of safe clipping. Case report and review of the literature. Surg Neurol. 2003;60:329-333.
113. Lister J.R., Rhoton A.L.Jr., Matsushima T., et al. Microsurgical anatomy of the posterior inferior cerebellar artery. Neurosurgery. 1982;10:170-199.
114. Marinkovic S., Milisavljevic M., Gibo H., et al. Microsurgical anatomy of the perforating branches of the vertebral artery. Surg Neurol. 2004;61:190-197.
115. Seeger W. Atlas of Topographical Anatomy of the Brain and Surrounding Structures. Wien: Springer-Verlag; 1978.
116. Perneczky A. The posterolateral approach to the foramen magnum. In: Samii M., editor. Surgery in and around the Brain Stem and the Third Ventricle. Berlin: Springer; 1986:460-466.
117. Hernesniemi J. Posterior fossa aneurysms. J Neurosurg. 2002;96:638-640.
118. D’Ambrosio A.L., Kreiter K.T., Bush C.A., et al. Far lateral suboccipital approach for the treatment of proximal posteroinferior cerebellar artery aneurysms. Surgical results and long-term outcome. Neurosurgery. 2004;55:39-50.
119. Horowitz M., Kopitnik T., Landreneau F., et al. Posteroinferior cerebellar artery aneurysms. Surgical results for 38 patients. Neurosurgery. 1998;43:1026-1032.
120. Peerless S.J., Hernesniemi J.A., Gutman F.B., et al. Early surgery for ruptured vertebrobasilar aneurysms. J Neurosurg. 1994;80:643-649.