CHAPTER 19 Surgical Approach and Handling of the Tuberosities
SURGICAL APPROACH
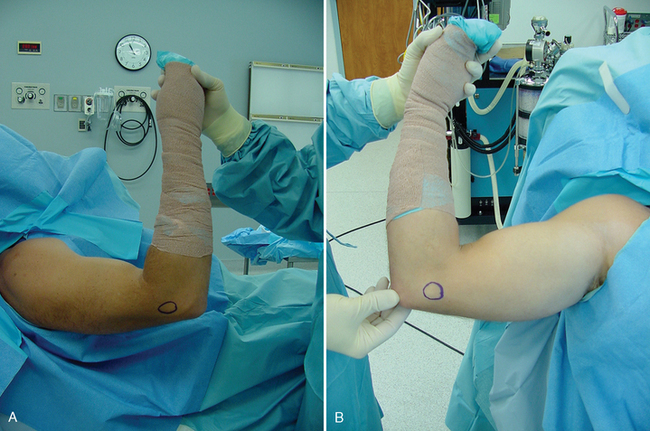
When performing shoulder arthroplasty for fracture, operating room setup, anesthesia, patient positioning, surgical site preparation, and sterile draping (Chapters 3 and 4) are essentially the same as for nonfracture cases, with a few exceptions. Draping of the patient differs slightly in fracture cases in which use of the fracture jig for prosthetic positioning is planned, in that the stockinet covers only the forearm so that the elbow and humeral epicondyles are easily accessible to use as reference points in judging prosthetic retroversion. When use of the fracture jig is planned, the epicondyles are palpated and marked with a surgical marking pen (Fig. 19-1).
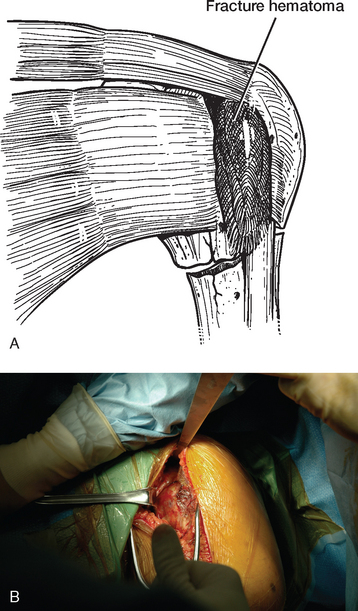
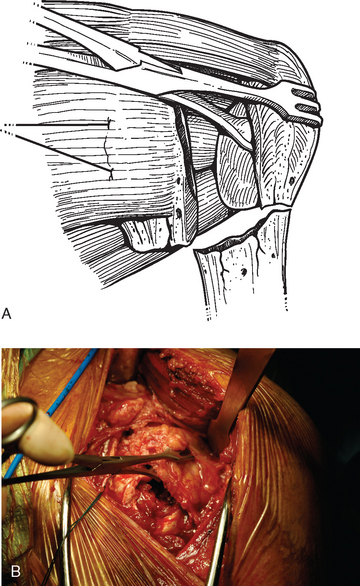
A standard deltopectoral approach is used for exposure just as in arthroplasty cases performed for chronic conditions. The skin incision starts at the tip of the coracoid process and extends distally and laterally approximately 10 to 15 cm, depending on the size of the patient. A needle tip electrocautery is used for deep dissection throughout the procedure to minimize hemorrhage. The interval between the deltoid and pectoralis major is identified by locating the cephalic vein. Once the cephalic vein is identified, it is retracted laterally with the deltoid muscle. The superior centimeter of the pectoralis major tendon is divided with the electrocautery to further enhance exposure. A self-retaining deltopectoral retractor is placed to maintain exposure during the procedure. The conjoined tendon is identified and traced to its insertion on the coracoid process. The tip of a Hohmann-type retractor is placed behind the base of the coracoid process to provide proximal retraction. With the arm abducted and externally rotated, the apex formed by the insertion of the coracoacromial ligament and the conjoined tendon onto the coracoid process is identified. The conjoined tendon is retracted medially to expose the proximal humeral fracture (Fig. 19-2).
IDENTIFICATION AND HANDLING OF THE TUBEROSITY
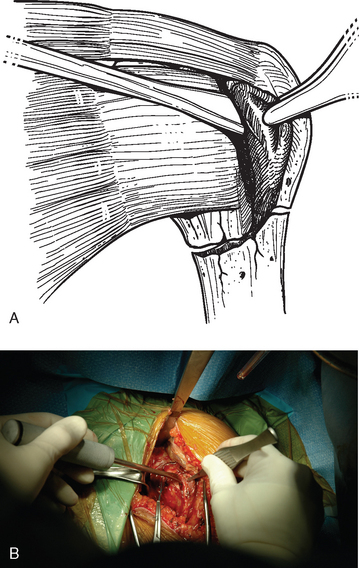
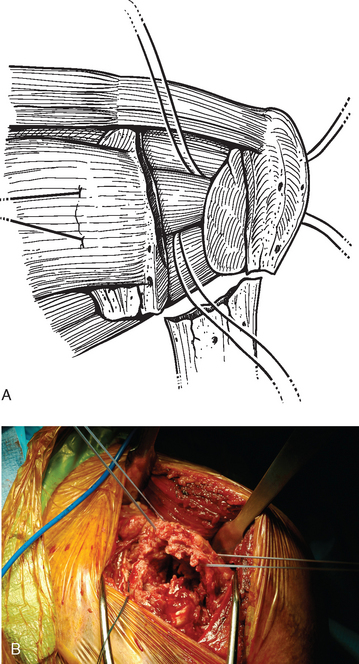
A Cobb elevator is used to perform blunt dissection and begin the process of identification of the tuberosities (Fig. 19-3). In the prototypical four-part fracture pattern, the lesser tuberosity with the attached subscapularis represents one fragment, the greater tuberosity with the attached posterior superior rotator cuff represents a second fragment, the humeral head represents a third fragment, and the humeral shaft represents the final fragment. A variety of combinations exist; however, the most common fracture pattern for which arthroplasty is indicated involves these major fracture fragments. Control of the lesser tuberosity is achieved by identifying the tuberosity and subscapularis tendon anteriorly in the shoulder just posterior to the conjoined tendon. Stay sutures of no. 1 polyester are placed through the subscapularis tendon just medial to its osseous insertion on the lesser tuberosity. One suture is placed superiorly and a second suture is placed inferiorly if necessary (Fig. 19-4). Sutures are not placed through the lesser tuberosity because it is usually osteopenic and does not support transosseous sutures sufficiently. These sutures will also aid in retracting the lesser tuberosity to gain access to the humeral head fragment. The humeral head fragment is identified and may be dislocated or split into two or more fragments. The humeral head is removed with locking forceps (Lahey type) and kept on the sterile field for later use as bone graft material (Fig. 19-5).
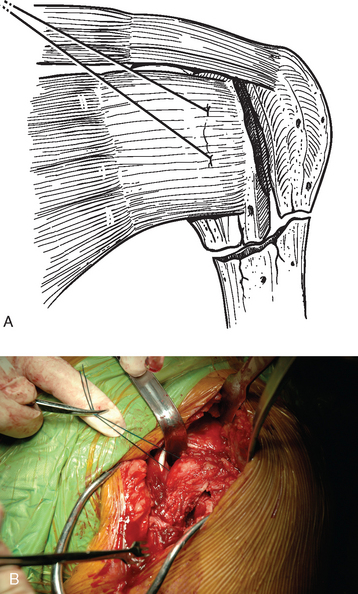
Figure 19-4 A and B, Control of the lesser tuberosity with stay sutures placed through the subscapularis tendon.
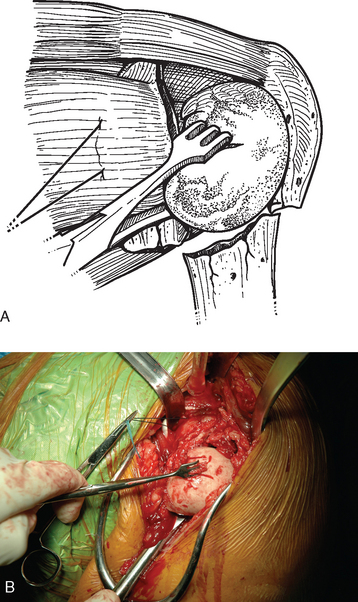
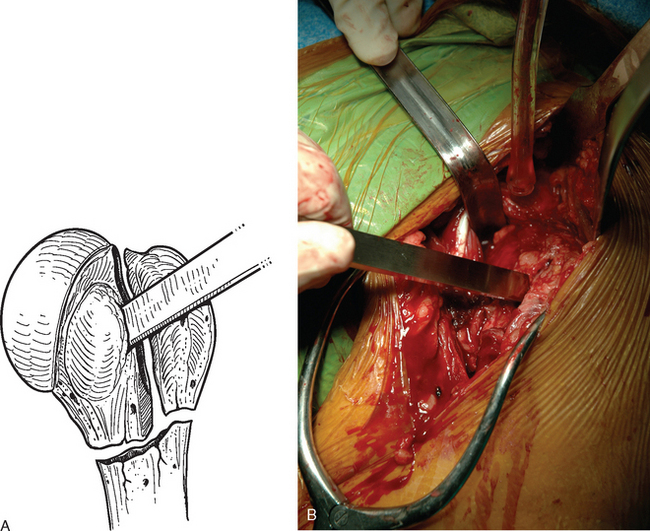
Removal of the humeral head facilitates identification of the greater tuberosity, which is located posteriorly in the shoulder. Frequently, especially in elderly patients in whom these fractures are most common, the greater tuberosity is a mere shell of thin cortical bone and must be handled with care to avoid further fracture (Fig. 19-6). Control of the greater tuberosity and attached posterior superior rotator cuff is obtained by passing no. 2 braided permanent suture through the rotator cuff tendons just medial to their insertion on the greater tuberosity. A large curved free needle is loaded with two strands of suture and passed through the rotator cuff at the junction of the supraspinatus and infraspinatus. A second free needle loaded with two strands of suture is passed through the rotator cuff at the junction of the infraspinatus and teres minor (Fig. 19-7). These sutures provide immediate control of the greater tuberosity and are used later for fixation of both the greater and lesser tuberosities. As with the lesser tuberosity, sutures are not placed through the greater tuberosity because it is usually osteopenic and does not support transosseous sutures sufficiently. Occasionally, it is necessary to temporarily grasp the greater tuberosity with Lahey forceps to provide traction and enable suture placement. This should always be done gently and with great care to avoid further fracture of the tuberosity.
Rarely, hemiarthroplasty is indicated in patients in whom the greater or lesser tuberosity remains attached to the humeral head (fracture-dislocation, head-splitting fracture). In these cases the tuberosity must be detached from the humeral head fragment. A 1-inch osteotome is used while leaving as much bone with the tuberosity fragment as possible (Fig. 19-8). The tuberosity is then handled as with a four-part fracture, as described earlier.