Chapter 39 Surgery for Trigeminal Neurinomas
Anatomy
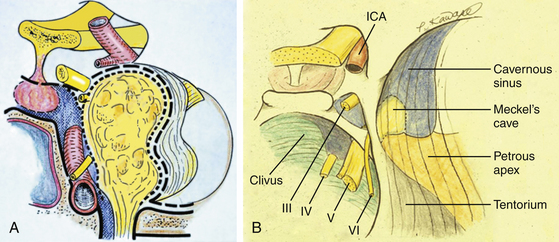
The trigeminal nerve courses in three compartments: middle cranial fossa, posterior fossa, and extracranial space. Therefore, tumors extending into multiple fossae are common (58%)1 (Table 39-1). The most common origin is around the Gasserian ganglion (GG), showing a dumbbell-shaped tumor extending both middle and posterior fossae (MP type, 38.6%) through Meckel’s cave (MC). MC is a subarachnoid space depressed from the posterior fossa, separated from the cavernous sinus by a thin meningeal dura (dura propria), and opened freely to the posterior fossa containing loose trigeminal nerve bundles without perineural covering.2 However, the trigeminal nerves peripheral to the GG course in the interdural space, are wrapped with a so-called inner reticular layer (perineurium), and are easily separated from the lateral wall of the cavernous sinus by a cleavage plane3 (Fig. 39-1A).
| Tumor Type | Patients |
|---|---|
| M | 8 (14.0%) |
| P | 12 (21.1%) |
| E | 4 (7.0%) |
| MP | 22 (38.6%) |
| ME | 7 (12.3%) |
| MPE | 4 (7.0%) |
| Total patients | 57 (100.0%) |
| Compartment | |
| Single | 24 (47.3%) |
| Multiple | 33 (57.9%) |
Therefore, the dumbbell-shaped tumor is spreading over the two anatomically different spaces: the interdural space anteriorly and the subarachnoid space posteriorly. The anterior part of the tumor can be removed through the interdural space by Dolenc’s approach.4 A small posterior fossa tumor can be removed through the orifice of MC; however, resection of the petrous apex, which obstructs the surgical field, is commonly necessary to observe the posterior fossa sufficiently. If the posterior fossa tumor is larger than 1 cm, the bone resection of the petrous apex plus detachment of the tentorium by the anterior petrosal approach (APA) is necessary.
Resection of the petrous apex may offer a surgical effect to widen the surgical space, as well as to decrease the tension of the trigeminal bundle bent by the petrous apex (Fig. 39-1B). The posterior fossa (P) type of tumor commonly attaches on the trigeminal nerve bundle alone, and it can be removed by the APA,5 even when the tumor is large.
Selection of Surgical Approaches
• The subtemporal interdural approach (SIA) without zygomatic osteotomy is indicated for tumors of the middle fossa (M) or middle fossa and extracranial (ME) type (with infratemporal extension).
• The APA is indicated for MP-type (dumbbell-shaped) and P-type tumors.
• The zygomatic petrosal approach (ZPA), combining SIA and APA is indicated for large MP-type tumors or extension into three middle, posterior, and infratemporal fossae (MPE)–type tumors.
SIA WITH OR without Zygomatic Osteomy
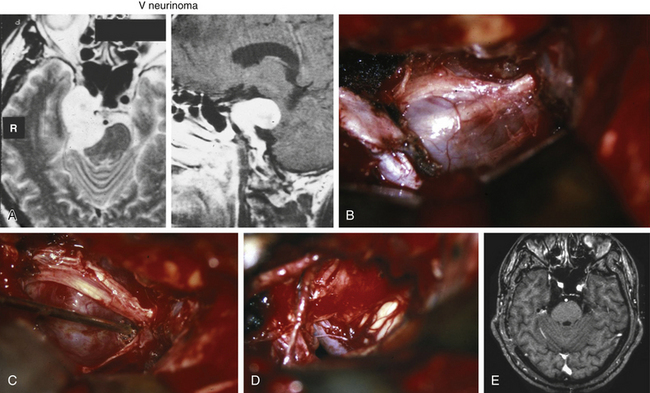
The SIA is indicated for an M-type tumor with or without extracranial extension (Fig. 39-2). The zygomatic osteotomy is not always necessary but is effective to spare retraction damage to the temporal lobe by turnover of the temporal muscle inferiorly, especially for a large tumor extending higher than the tentorial fold. In the supine position, the patient’s head is rotated 60 degrees with a downward axis. A curved hemicoronal incision along the auricle is followed by exposure of the zygomatic arch, which is cut in two points by a surgical saw. The craniotomy is created along the middle fossa base to expose the foramen rotundum and ovale epidurally. The middle meningeal artery is coagulated and cut at the foramen spinosum. The periosteal side of the dura mater is incised above the foramen rotundum, and the incision is extended above the foramen ovale and toward the superior orbital fissure.
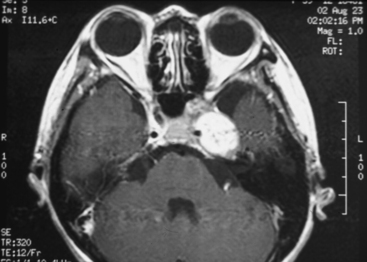
FIGURE 39-2 Parasellar type of trigeminal neurinoma. Note the compressed cavernous sinus medial to the tumor.
The lower part of the tumor appears by this point, and the upper part can be exposed by tacking the parasellar dura superiorly (Fig. 39-3). The tumor is commonly covered by a thin semitransparent membrane, the so-called inner reticular layer, showing the course of the trigeminal nerves through it (Fig. 39-3A and B).
The nerves are clearly identified and separated from the tumor by removal of the membrane (Fig. 39-3C). In large tumors, the nerve fascicule is lost and the tumor is commonly wrapped by numerous isolated trigeminal nerve fibers. The surgical windows for tumor removal are created by mobilizing the nerve fibers.
The cavernous sinus is separated from the tumor by the medial wall of the inner reticular layer, and it does not open by careful preservation of the membrane. After tumor removal, the widened orifice of MC can be confirmed by cerebrospinal fluid discharge. The anterolateral aspect of the pons can be seen through MC (Fig. 39-3C). The opened MC is packed by the fascial flap at closure. The zygomatic arch is replaced and fixed by titanium plates.
1. In the case of tumor extension into the infratemporal fossa (MPE type), the middle fossa base is drilled off until the penetrating tumor is exposed. Venous bleeding from pterygoid plexus must be cared for.
2. In the case of tumor extension into the orbit (ME type 1), the surgical method is the same as Dolenc’s approach.4 Orbital unroofing, removal of the anterior clinoid process, and interdural dissection on the superior orbital fissure offer a total view from the orbit to the parasellar space. The orbital wall is reconstructed by an inner layer of the cranial flap or by a titanium plate.
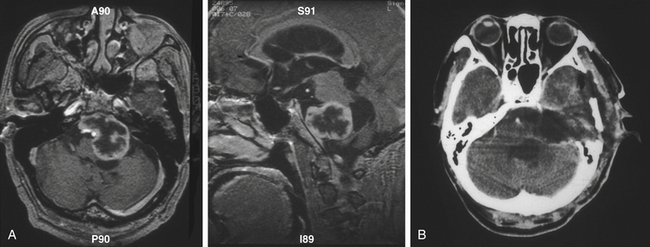
Anterior Petrosal Approach
The technical details of the APA were described earlier. This approach is indicated for dumbbell-shaped MP-type tumors (Fig. 39-4) or P-type tumors (Fig. 39-5). A fishhook-shaped scalp incision is followed by dissecting a fascial flap of the temporal muscle available for tight dural closure. The temporal muscle is reflected anteriorly without incision. The craniotomy size is almost the same as that of the squamous suture. After elevation of the middle fossa dura from the skull base, the middle meningeal artery is cauterized and cut. The petrous apex medial to the greater petrosal nerve is commonly eroded by the tumor; thus, the petrous resection is easier. In a P-type tumor, the petrous apex must be resected completely. The middle fossa dura is cut into a T shape along the superior petrosal sinus (SPS), which is ligated and cut with the tentorium thereafter.
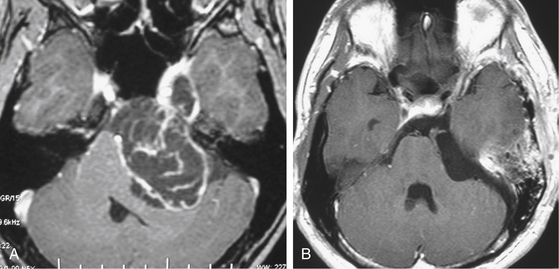
FIGURE 39-4 Large dumbbell-shaped (MP) neurinoma in a 26-year-old male before (A) and after (B) by the APA.
The complex can be confirmed by neuroendoscope after tumor removal. Also after tumor removal, the medial wall of MC, anterolateral aspect of the pons, and basilar artery complex are seen. For closure, a piece of abdominal fat is placed on the air cells of the petrous apex and rim of the craniotomy and is fixed with fibrin glue. Moreover, the cells are wrapped with a temporal fascia, which is sutured with dura thereafter. The double-layer closure seldom causes complication of cerebrospinal fluid leakage or subcutaneous cerebrospinal fluid accumulation.
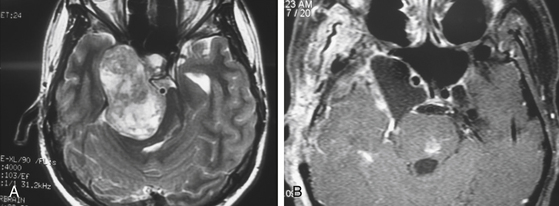
Zygomatic Petrosal Approach
The ZPA is a combination of SIA with zygomatic osteotomy and APA, indicated for a large MP-type tumor (Fig. 39-6) or a tumor extending into three fossae (middle, posterior, and infratemporal fossae); that is, a tumor of the MPE type. The operation has five steps. A question mark–shaped skin incision, zygomatic osteotomy, and basal craniotomy exposing the superior orbital fissure, foramen rotundum, foramen ovale, and petrous apex comprise the first step of operation. Skull base resection along the infratemporal tumor extension and resection of the petrous apex comprise the second step. The third step is removal of the tumor from the middle and infratemporal fossae. The fourth step consists of a dural incision along the SPS, a tentorial incision, and the opening of MC. The last step consists of removal of the posterior fossa tumor and closure. After tumor removal, the three fossae can be observed from a single craniotomy along the trigeminal nerve. Retraction damage to the temporal lobe is uncommon because exposure of the brain is minimal.
Surgical Results
Among 57 patients with trigeminal neurinoma at our university, 47 have undergone skull base surgery since 1990. The most common method was APA, performed in 29 patients (61.7%). Another 12 patients (21.3%) underwent SIA, and zygomatic osteotomy was combined in 6 of them. A further group of 7 patients (14.8%) underwent ZPA. One patient was treated by the supraorbital approach for the tumor location in the orbit. The tumor was gross totally resected in 43 patients (91.5%) and nearly totally resected in 3 patients (6.4%); partial resection was made only in 1 patient who had a history of surgery and gamma knife treatment (Table 39-2). Two patients with a small residue were treated by gamma knife, and a single patient underwent reoperation due to tumor regrowth. Patients did not present temporal lobe symptoms or long tract signs. No mortality occurred in this series. The major surgical complication was facial hypesthesia, which occurred in the territory of tumor origin. However, the patients’ symptoms did not significantly affect their daily life because branches were preserved when possible. Only 1 patient with an M-type tumor complained of paresthesia. Permanent abducens palsy occurred in 3 patients, and hearing disturbance occurred in a single patient with a large tumor. Incomplete facial palsy, which might have resulted from retraction of the greater superficial petrosal nerve, occurred in 2 patients; however, the incidence might be lower compared to another reports.6,7
| Extent | Patients |
|---|---|
| Total resection | 43 (91.5%) |
| Nearly total resection | 3 (6.4%) |
| Partial resection | 1 (2.1%) |
| Total patients | 47 (100.0%) |
Al-Mefty O., Ayoubi S., Gaber E. Trigeminal schwannomas: removal of dumbbell-shaped tumors through the expanded Meckel cave and outcome of cranial nerve function. J Neurosurg. 2002;96:453-463.
Dolenc V.V. Frontotemporal epidural approach to trigeminal neurinomas. Acta Neurochir (Wien). 1994;130:55-65.
Kawase T., Shiobara R., Toya S. Anterior transpetrosal–transtentorial approach for sphenopetroclival meningiomas: surgical method and results in 10 patients. Neurosurgery. 1991;28:869-875. discussion 875-876
Kawase T., van Loveren H., Kellar J.T., Tew J.M. Meningeal architecture of the cavernous sinus: clinical implications. Neurosurgery. 1996;39:527-534. discussion 534-536
Muto J., Kawase T., Yoshida K.. Meckel’s cave tumors, relation to meninges and minimally invasive approaches for surgery—anatomical and clinical studies. Neurosurgery, 2010 Sep;suppl operative 3:67 291-298; discussion 298-299
Sami M., Tatagiba M., Carvalho G.A. Retrosigmoid intradural suprameatal approach to Meckel’s cave and the middle fossa: surgical technique and outcome. J Neurosurg. 2000;92:235-241.
Yoshida K., Kawase T. Trigeminal neurinomas extending into multiple fossae; surgical methods and review of the literature. J Neurosurg. 1999;91:202-211.
1. Yoshida K., Kawase T. Trigeminal neurinomas extending into multiple fossae; surgical methods and review of the literature. J Neurosurg. 1999;91:202-211.
2. Muto J., Kawase T., Yoshida K.. Meckel’s cave tumors, relation to meninges and minimally invasive approaches for surgery—anatomical and clinical studies. Neurosurgery, 2010 Sep;suppl operative 3:67 291-298; discussion 298-299
3. Kawase T., van Loveren H., Kellar J.T., Tew J.M. Meningeal architecture of the cavernous sinus: clinical implications. Neurosurgery. 1996;39:527-534. discussion 534-536
4. Dolenc V.V. Frontotemporal epidural approach to trigeminal neurinomas. Acta Neurochir (Wien). 1994;130:55-65.
5. Kawase T., Shiobara R., Toya S. Anterior transpetrosal–transtentorial approach for sphenopetroclival meningiomas: surgical method and results in 10 patients. Neurosurgery. 1991;28:869-875. discussion 875-876
6. Sami M., Tatagiba M., Carvalho G.A. Retrosigmoid intradural suprameatal approach to Meckel’s cave and the middle fossa: surgical technique and outcome. J Neurosurg. 2000;92:235-241.
7. Al-Mefty O., Ayoubi S., Gaber E. Trigeminal schwannomas: removal of dumbbell-shaped tumors through the expanded Meckel cave and outcome of cranial nerve function. J Neurosurg. 2002;96:453-463.