Chapter 19 Sural Nerve
Anatomy
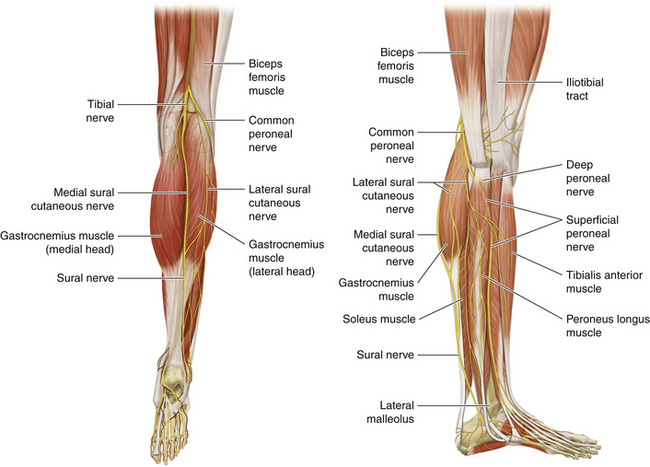
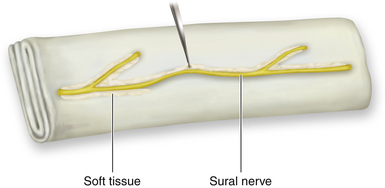
• The sural nerve is formed from two components derived from the tibial and peroneal nerves (Figure 19-1). The branching of the tibial and peroneal components and the main nerve is variable.
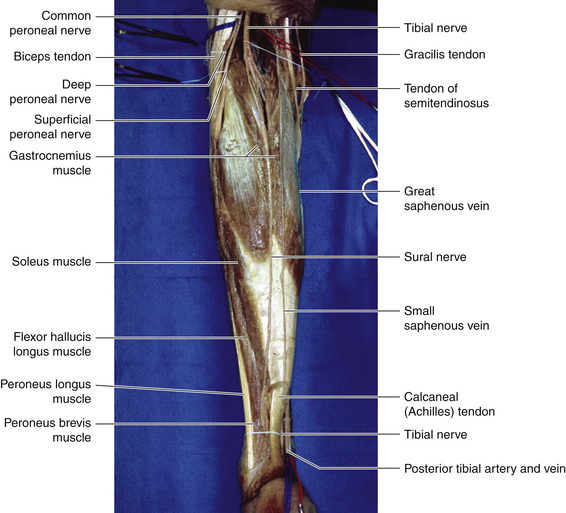
• The tibial nerve gives a single cutaneous branch—the sural nerve—at about the midline of the popliteal fossa. The sural nerve descends between the two heads of the gastrocnemius, deep to the investing fascia (Figure 19-2).
• Leaving the popliteal fossa at the inferior angle, the sural nerve descends in the groove between the two heads of the gastrocnemius and pierces the deep fascia proximally in the leg to join the lateral sural nerve.
• The level at which the various elements of the sural nerve pierce the investing fascia of the leg to run in the subcutaneous fat is variable.
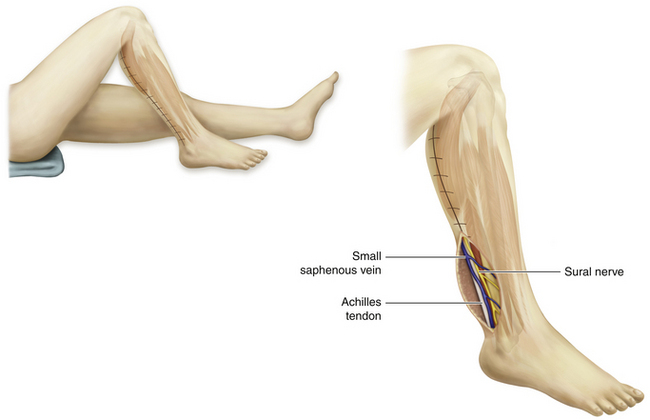
• Accompanied by the small saphenous vein, the sural nerve descends lateral to the Achilles tendon to the region located between the lateral malleolus and the area in front of the Achilles tendon (Figure 19-3). The point of junction of the two component nerves varies from immediately proximal to the lateral malleolus to the popliteal fossa. The specific pattern of a patient’s sural nerve cannot be forecast preoperatively.
• Distal to the lateral malleolus, the sural nerve runs along the lateral border of the foot and ends at the lateral side of the little toe. It supplies the posterior and lateral skin of the distal third of the leg and over the lateral border of the foot up to the tip of the little toe.
Surgery
Patient Positioning
• When the patient is prone, as for an approach to the sciatic nerve or a posterior approach to the radial or axillary nerves, sural nerve exposure is easily accomplished, because the calves are uppermost.
• With the patient supine, as is the case for many nerve dissections, sural exposure is more difficult.
• A folded towel is clipped to the surface of the operating table so that the knee can later be flexed and the hip internally rotated, with the foot braced against the folded towel.
• A folded sheet under the buttock helps the surgeon internally rotate the leg a bit to expose the calf.
• The plan to harvest sural grafts should be rehearsed before the main operative site and sural donor sites are prepared and draped. This is particularly important if an over-the-patient instrument table is used, or if the operating room nurse changes the site of command halfway through the procedure.
Skin Incision
• A vertical incision is made at the level of the lateral malleolus, using the small saphenous nerve as a guide.
• The nerve and vein are dissected and identified.
• A finger is passed beneath the nerve, and the nerve is very gently tented up. The fingertips of the surgeon’s other hand rest gently over a more proximal part of the nerve, and that structure can be palpated when the distal nerve is tented up.
• Using this technique, a series of stepladder incisions can be made up to the origins of the nerve. The nerve is divided at the malleolus and withdrawn at each subsequently placed horizontal incision.
• If gentle traction fails to produce the nerve, it is tethered by a branch. A vertical incision is placed over the nerve at that point, and the branch is divided.
• The ratio of horizontal to vertical incisions varies, according to the anatomy of each patient.
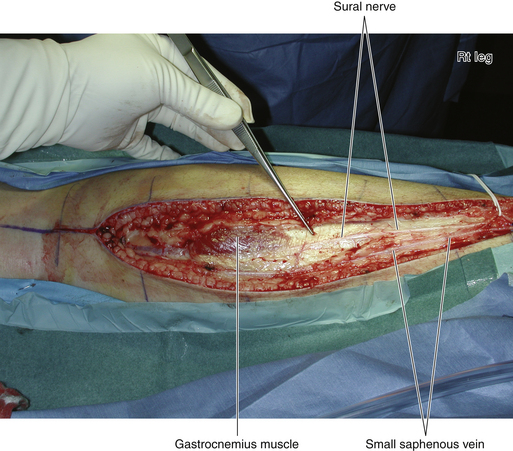
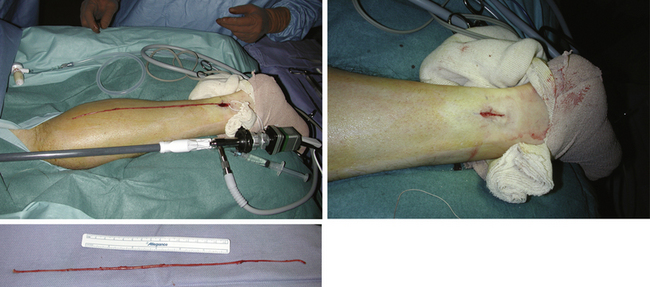
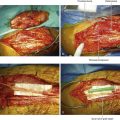
• In some circumstances a single long vertical incision is used (Figure 19-4)
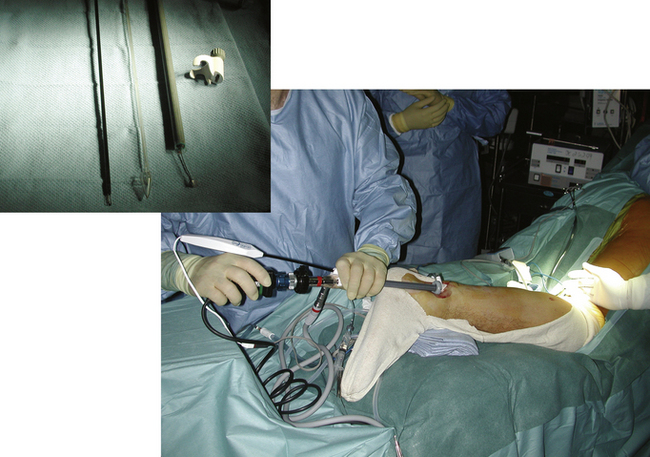
• A limited-access, closed system may be employed. For sural nerve endoscopic harvesting, all harvest procedures are performed under tourniquet control. A 2-cm incision is made behind the lateral malleolus, and the sural nerve and small saphenous vein are identified after open dissection. The retractor and endoscope unit (endoscopic cannula) are then inserted.
• A dissector is inserted along the relatively loose plane around the nerve and placed just beneath or above the tissue to be dissected. Tissue that is not fully dissected off the nerve by the dissector is dissected and transected with scissors, and the remaining vessels are electrocauterized. Fascial division may be necessary beyond the point where the nerve descends beneath the deep fascia of the calf to run on the belly of the gastrocnemius in close relation to the plantaris tendon. After enough of the sural nerve is harvested, the wound is closed (Figures 19-5 and 19-6).
Isolating the Nerve
• The nerve can be traced proximally by sharp dissection with a scalpel or scissors.
• The surgeon must understand that the exact fascicular anatomy of the sural nerve cannot be forecast because of normal variability. Technique must be adapted to the particular anatomy of each particular patient.
• Once identified, the nerve is surgically traced proximally.
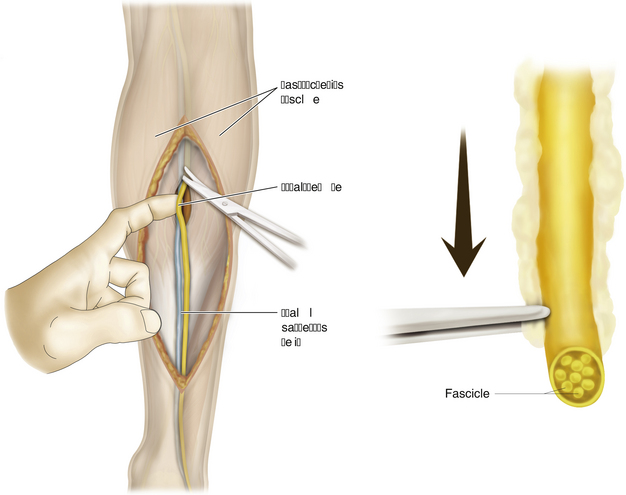
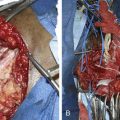
• Initially, the nerve is dissected in the subcutaneous fat, and subsequently, as the dissection moves more proximally, deep to the investing fascia. Overlying gastrocnemius fascia therefore must be incised in the proximal calf (Figure 19-7).
• Care must be taken proximally not to place too much traction on the lateral nerve, because it originates from the peroneal nerve, which can be damaged. It is, of course, paramount to manipulate the nerve as gently as possible, because it is to be used as a conduit for regenerating axons. Whatever technique is used, it is essential that stretch injuries not be created in the sural nerve, its branches, or the peroneal and tibial nerves.
• After the sural nerve and its branches are harvested, they are moved to the back operating table and are kept moist with sterile normal saline.
• By the use of fine forceps and scissors, excess soft tissues such as the fascia and fat are trimmed off the graft perineurium (Figure 19-8).
• In some instances, good lengths of large-fascicular-caliber donor nerve are obtained. In other circumstances, only miserable fine fascicles are found. Rarely, the material is of such poor quality that alternate donor sites have to be harvested.
• Defects to be bridged by grafts are measured, and the graft is divided into the required lengths for repair. Individual grafts need to be about 10% longer than the gaps to allow for retraction. It is important to keep the grafts and the graft sites moist, usually with sterile normal saline.