Chapter 35
Supraventricular Tachycardia
1. What does the term supraventricular tachycardia (SVT) mean?
2. What is the most common cause of paroxysmal SVT?
AVNRT accounts for 60% to 70% of paroxysmal SVTs, followed by AVRT.
3. What factors are part of the generic workup for supraventricular tachycardia?
 History, including type and duration of symptoms (palpitations, lightheadedness, chest pains, dyspnea, presyncope, precipitating factors)
History, including type and duration of symptoms (palpitations, lightheadedness, chest pains, dyspnea, presyncope, precipitating factors)
 Questions regarding the intake of alcohol, caffeine, and illicit drugs
Questions regarding the intake of alcohol, caffeine, and illicit drugs
 Cardiac history (myocardial infarction, valvular disease, cardiac surgery)
Cardiac history (myocardial infarction, valvular disease, cardiac surgery)
 Physical examination (although often unrevealing)
Physical examination (although often unrevealing)
 12-lead electrocardiogram (ECG) (looking for signs of chamber enlargement, preexcitation, etc.)
12-lead electrocardiogram (ECG) (looking for signs of chamber enlargement, preexcitation, etc.)
 Echocardiogram (often unrevealing because paroxysmal SVT can occur in the absence of structural heart disease, although atrial arrhythmias will often occur in the setting of dilated atria)
Echocardiogram (often unrevealing because paroxysmal SVT can occur in the absence of structural heart disease, although atrial arrhythmias will often occur in the setting of dilated atria)
 Laboratory tests (electrolyte abnormalities, hyperthyroidism)
Laboratory tests (electrolyte abnormalities, hyperthyroidism)
4. What are the causes of narrow complex regular tachycardias (regular referring to fixed R-R intervals—the time or distance between QRS complexes)?
ECGs of the more common SVTs that cause narrow complex regular tachycardias are shown in Figure 35-1.
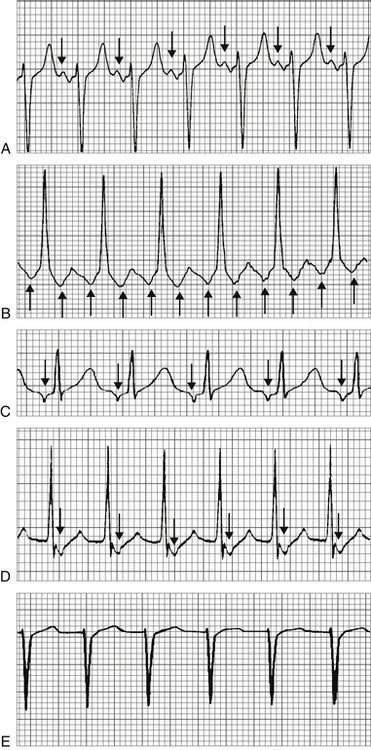
Figure 35-1 SVTs that cause a narrow complex regular tachycardia. A, Sinus tachycardia. Normal appearing P waves (arrows) are present before each QRS complex. B, Atrial tachycardia. Abnormal, inverted P waves (arrows) are present before each QRS complex. C, Atrial flutter. Flutter waves (arrows) are present. There is 2:1 conduction. D, Atrioventricular nodal reentrant tachycardia (AVNRT). No P waves are present before the QRS complexes. Retrograde, inverted P waves (arrows) are visible immediately after the QRS complexes. E, Atrioventricular reentrant tachycardia (AVRT). No P waves are present before the QRS complexes. Although retrograde P waves are sometimes seen in the ST-T segment with AVRT, none are visible in this particular rhythm strip.
 Sinus tachycardia (not really an arrhythmia, but still in the differential diagnosis)
Sinus tachycardia (not really an arrhythmia, but still in the differential diagnosis)
 Rare causes of narrow complex QRS, especially in adults, that are often difficult to diagnose and are more suited for discussion at the cardiology fellow or attending level, include sinoatrial (SA) nodal reentrant tachycardia and focal junctional tachycardia.
Rare causes of narrow complex QRS, especially in adults, that are often difficult to diagnose and are more suited for discussion at the cardiology fellow or attending level, include sinoatrial (SA) nodal reentrant tachycardia and focal junctional tachycardia.
5. What are the causes of narrow complex irregular tachycardias (tachycardias with irregular R-R intervals)?
ECGs of SVTs that cause narrow complex irregular tachycardias are shown in Figure 35-2.
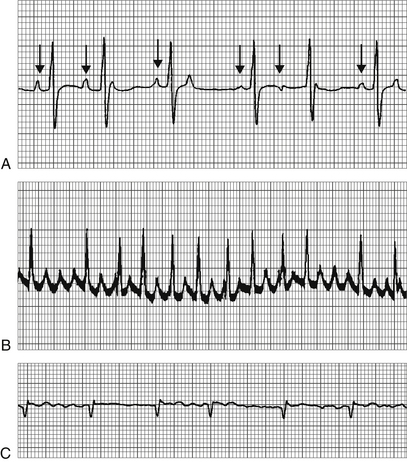
Figure 35-2 Supraventricular tachycardia (SVTs) that cause a narrow complex irregular tachycardia. A, Multifocal atrial tachycardia (MAT). P waves of differing morphologies (arrows) are present before the QRS complexes. B, Atrial flutter with variable block. Flutter waves are intermittently visible between the QRS complexes. C, Atrial fibrillation. No organized atrial activity is present.
6. How should one determine the correct diagnosis of a narrow complex tachycardia?
This can be done in two simple steps. First, decide if the rhythm is regular or irregular. Second, look for P waves or atrial activity. Figure 35-3 demonstrates how this simple two-step process will lead to the correct diagnosis.
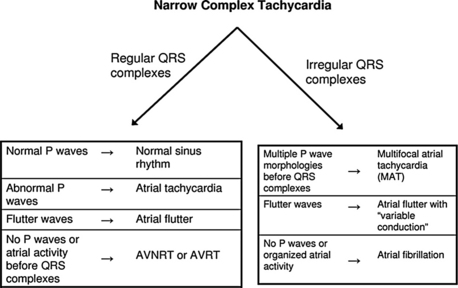
Figure 35-3 Simple algorithm for the diagnosis of narrow complex tachycardias. Step one is to decide if the rhythm is regular or irregular (are the QRS complexes occurring at regular or irregular intervals). Step two is to search for the presence of P waves or organized atrial activity.
7. What drug is most commonly implicated in cases of drug-induced atrial tachycardia?
Digoxin. Digoxin toxicity can cause many arrhythmias, including paroxysmal atrial tachycardia with block. In paroxysmal atrial tachycardia (PAT) with block, there is atrial tachycardia but also AV nodal block, leading to a slow ventricular response rate (Fig. 35-4). In cases of PAT with block, digoxin toxicity should be suspected.
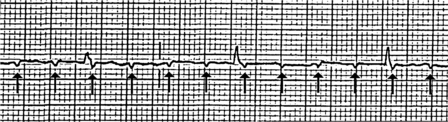
Figure 35-4 Atrial tachycardia with block. The arrows point to P waves generated by the atrial tachycardia. Most of these P waves are not conducted in to the ventricle. The finding of atrial tachycardia with significant atrioventricular (AV) node block is highly suggestive of digoxin toxicity.
8. What is the most common ventricular response rate in patients who develop atrial flutter?
Atrial flutter most commonly occurs at a rate of 300 beats/min, although the rate can be somewhat slower in patients on antiarrhythmic agents that slow ventricular conduction (such as amiodarone) or in cases of massively dilated atria. Most commonly, there is 2:1 AV block, meaning that only every other atrial impulse is conducted down to the ventricles. Thus, the most common ventricular response rate is 150 beats/min (see Fig. 35-1, C). The finding of a regular narrow complex tachycardia at exactly 150 beats/min should raise suspicion of atrial flutter as the causative arrhythmia.
9. Which is more common, AVNRT or AVRT?
AVNRT is more common in the general population. In patients with known preexcitation syndrome (Wolff-Parkinson-White [WPW] syndrome), AVRT, which requires an accessory circuit, is more common. Thus, statistically, the cause of a narrow complex regular tachycardia is more likely to be AVNRT than AVRT, unless the patient has known WPW (or evidence of it on a baseline ECG).
10. What is the most common cause of atrial tachycardia?
Atrial tachycardia (see Fig. 35-1, B) is most commonly caused by a discrete autonomic focus, although a microreentrant circuit causes a small percentage of atrial tachycardias. Precipitating factors and causes of atrial tachycardia include:
 Diseased atrial tissue (fibrosis, inflammation, etc.)
Diseased atrial tissue (fibrosis, inflammation, etc.)
 Increased sympathetic stimulation (hyperthyroidism, caffeine, etc.)
Increased sympathetic stimulation (hyperthyroidism, caffeine, etc.)
Although textbooks describe the rate of atrial tachycardia as anywhere between 100 and 220 beats/min, a rate of approximately 160 to 180 beats/min is most common. AV conduction is usually 1:1 unless the tachycardia is very rapid, in which case 2:1 conduction may occur. Because most cases of atrial tachycardia are due to an autonomic focus and not a reentrant pathway, the arrhythmia most commonly does not terminate with cardioversion. Adenosine usually (but not always) will not terminate the arrhythmia, but adenosine administration may be useful in cases in which the cause of regular SVT is unclear (see Question 12).
11. What is concealed conduction?
12. In cases of SVT in which the cause is not clear, what is generally considered first-line drug therapy?
13. For what arrhythmia should AV nodal blocking agents not be administered?
In rare cases of atrial fibrillation in the setting of an accessory bypass tract (WPW syndrome), some conduction of impulses will occur down the AV node and His-Purkinje system into the ventricle, and some conduction will occur down the bypass tract. In such cases, administration of AV nodal blocking agents (adenosine, digoxin, β-blockers, calcium channel blockers) may lead to increased conduction down the accessory bypass tract, producing an increased ventricular response rate and possibly precipitating ventricular fibrillation.
14. Do patients with atrial flutter require anticoagulation before cardioversion?
15. Can SVT cause a wide QRS complex tachycardia?
16. What is AVRT with antidromic conduction?
17. What factors make the diagnosis of a wide QRS complex more likely to be ventricular tachycardia (VT) than SVT?
 P-wave dissociation (also called AV dissociation): In P-wave dissociation, the QRS complexes occur at a greater rate than the P waves and there is no fixed relationship between the QRS complexes and the P waves. This finding is highly suggestive of VT. Unfortunately, P-wave dissociation can only be clearly discerned in 30% of cases of VT.
P-wave dissociation (also called AV dissociation): In P-wave dissociation, the QRS complexes occur at a greater rate than the P waves and there is no fixed relationship between the QRS complexes and the P waves. This finding is highly suggestive of VT. Unfortunately, P-wave dissociation can only be clearly discerned in 30% of cases of VT.
 QRS complex width: In the absence of antiarrhythmic agents or an accessory pathway, a QRS width of more than 140 ms with a right bundle branch block (RBBB) morphology or a QRS width of more than 160 ms with a left bundle branch block (LBBB) morphology favors the diagnosis of VT.
QRS complex width: In the absence of antiarrhythmic agents or an accessory pathway, a QRS width of more than 140 ms with a right bundle branch block (RBBB) morphology or a QRS width of more than 160 ms with a left bundle branch block (LBBB) morphology favors the diagnosis of VT.
 Negative concordance: Negative concordance is the finding of similar QRS morphologies in all the precordial leads, with QS complexes present. This finding is essentially diagnostic for VT.
Negative concordance: Negative concordance is the finding of similar QRS morphologies in all the precordial leads, with QS complexes present. This finding is essentially diagnostic for VT.
 Ventricular fusion beats: Fusion beats are QRS complexes that may be formed from the fusion of an impulse originating in the ventricle with an impulse originating in the atria and traveling down the AV node and His-Purkinje system. The finding of fusion beats indicates VT.
Ventricular fusion beats: Fusion beats are QRS complexes that may be formed from the fusion of an impulse originating in the ventricle with an impulse originating in the atria and traveling down the AV node and His-Purkinje system. The finding of fusion beats indicates VT.













